Abstract
Patient: Female, 38
Final Diagnosis: Ketoacidosis, part of Wolcott Rallison syndrome
Symptoms: Coma • dehydration
Medication: —
Clinical Procedure: —
Specialty: Endocrinology and Metabolic • Pediatrics
Objective:
Rare disease
Background:
Neonatal diabetes mellitus is a rare condition and it is important to differentiate it from other causes, such as hyperglycemia in infancy, for better outcomes. We report a case of an infant who presented to our neonatal intensive care unit in ketoacidosis and a comatose state.
Case Report:
Our case was an infant who presented to the neonatal intensive care unit at 38 days of age in ketoacidosis. The female infant, born to consanguineous parents (first cousins), weighing 2,300 grams at birth, presented with extreme dehydration and pale skin. The infant’s head was normocephalic and there were no obvious deformities on the rest of her body. Urine examination was positive for ketones and glucose was 4+. Her blood glucose level was 550 mg/dL (30.5 mmol/L). After taking care of electrolytes, insulin was initiated in the form of a continuous drip. After a few days, insulin glargine was initiated, given twice daily via subcutaneous route. A few days later, blood samples were sent from our hospital in India to the UK and genetic testing was performed free of charge by the Department of Molecular Genetics, University of Exeter Medical School, UK, and confirmed a genetic diagnosis of Wolcott-Rallison syndrome.
Conclusions:
Regardless of whether permanent neonatal diabetes mellitus is associated with Wolcott-Rallison syndrome or other genetic mutations, it is important to initially stabilize the infant and later do a genetic testing to see whether the infant can be given oral sulfonylureas or has to be given insulin therapy.
MeSH Keywords: Diabetic Coma; Diabetic Ketoacidosis; Mutation, Missense
Background
Neonatal diabetes mellitus is a rare condition and it is important to differentiate it from other causes, such as hyperglycemia in an infant, for better outcomes. The case presented here is of an infant who presented to our neonatal intensive care unit (NICU) in comatose state due to hyperglycemia. After controlling the infant’s blood sugar level, we performed several tests and ruled out several causes of hyperglycemia in infancy. We determined the diagnosis of neonatal diabetes mellitus after several weeks. This case report could be helpful to inform doctors around the world on how to deal with an infant with hyperglycemia.
Case Report
A 38-day-old female infant of East Indian ethnicity presented to the NICU in comatose state with shallow breathing and marked dehydration. The infant was normocephalic and had no obvious deformities. Her respiratory rate was 35 breathes per minute. Her pulse was 130 beats per minute, and her blood pressure was low. The infant was afebrile. Her birth weight was 2,300 grams; she was born to consanguineous parents (first cousins). The initial differential diagnoses were infections, cardiac conditions, kidney related issues, and endocrine conditions.
Investigations
Urine examination showed ketones at 4+, urine glucose also at 4+. The blood glucose level was 550 mg/dL. Her serum electrolytes were within normal limits. Liver and kidney function tests were normal. TSH was normal at 1.82 μIU/mL, cortisol (taken at 8 am) was normal at 5.37 μg/dL; IGF-1 was 59 ng/mL; C-peptide was low at 0.34 ng/mL; and antibodies for diabetes were negative.
Treatment
Actrapid was initiated with bolus of 4 units and then as a continuous infusion at around 1 unit/hour. In the first 24 hours a total of 26 units of Actrapid were given. The infant regained consciousness in a few hours. Between 24–48 hours after admission, a total of 24 units of Actrapid were given; and between 48–72 hours a total of 22 units of Actrapid were given. After 72 hours, we reduced the dose of Actrapid infusion by half and added insulin glargine at 3 units, twice daily. After 96 hours, we completely stopped Actrapid and continued with glargine at 7 units twice daily subcutaneous. Glargine was added after four days because when glargine is added to replace regular insulin, there can be spikes in blood glucose levels and we wanted to make sure that the infant was stable for a few days before adding glargine. When the switch was being done from Actrapid to the long-acting insulin glargine, there were occasional peaks and troughs in the blood glucose levels. After six days of admission, the blood glucose was well controlled between 110–180 mg/dL checked at multiple times during the day.
Genetic testing
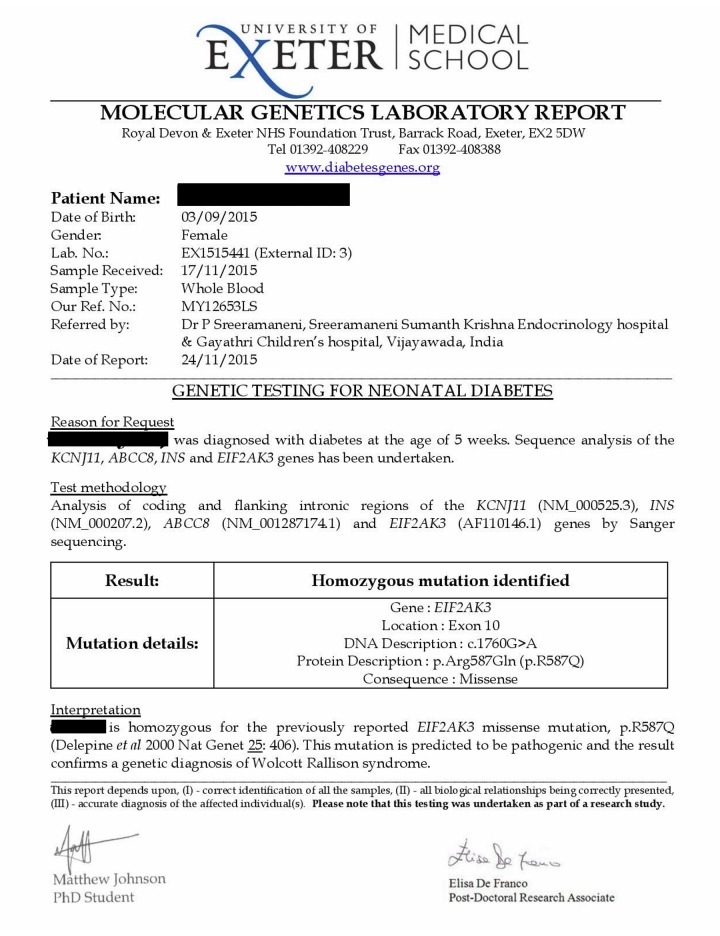
We contacted the Department of Molecular Genetics, University of Exeter Medical School, UK, and they did the genetic testing for free for this infant. We sent 5 mL blood samples from the infant, the mother, and the father for genetic testing. After a few days we got the diagnosis of Wolcott-Rallison syndrome (Figure 1).
Figure 1.
Molecular genetics laboratory report.
Follow-up
Since the day of the infant’s discharge, only once did her blood glucose level fall below 80 mg/dL and on two occasions it was more than 200 mg/dL (212 mg/dL and 220 mg/dL). On most occasions, the blood glucose has been maintained between 110–180 mg/dL. Liver function tests and kidney function tests have been normal.
Discussion
Hyperglycemia in infancy can be caused by infection, hepatic immaturity disorders, medications, etc. But if the serum blood glucose levels are inappropriately high then it is advisable to investigate whether the infant has neonatal diabetes mellitus. Neonatal diabetes mellitus is monogenic, very rare and occurs in between 200,000 to 500,000 births. Neonatal diabetes mellitus is either permanent or transient. The permanent form is most commonly due to a mutation in KCNJ11 gene [1]. Some cases of neonatal diabetes mellitus that are due to mutations in KCNJ11 and ABCC8 can be safely treated with sulfonylureas instead of insulin [1,2].
Wolcott-Rallison syndrome is rare with less than 60 cases identified worldwide. The diabetes mellitus that occurs in Wolcott-Rallison syndrome is permanent [3]. However, Wolcott-Rallison syndrome is now said to be the most common cause of neonatal diabetes mellitus in infants with parents who had consanguineous marriage [4]. Diabetes mellitus in these children is usually diagnosed by six months of age. Rarely, however, diabetes mellitus can present after infancy [4]. Exocrine pancreatic insufficiency, recurrent acute liver failure, renal failure, epiphyseal dysplasia, osteoporosis, growth retardation, hypothyroidism, neutropenia, recurrent infections, and cardiovascular issues might develop later [3]. The hepatic dysfunction is due to recurrent acute bouts of cytolysis, often with cholestasis. These episodes are usually recurrent with spontaneous remission with varying degree of severity [5]. These patients also have recurrent episodes of hypoglycemia likely due to impaired gluconeogenesis because of liver dysfunction [6].
Wolcott-Rallison syndrome is caused by mutations in the gene encoding eukaryotic translation initiation factor 2α kinase 3 (EIF2AK3) inherited in an autosomal recessive manner. EIF2AK3 is also known as PERK (PKR-like endoplasmic reticulum kinase). PERK is a trans membrane protein in endoplasmic reticulum (ER) [4]. EIF2AK3 is widely expressed in the early fetal pancreatic epithelial cells, and also present in adult pancreatic beta cells and exocrine tissue. It is also expressed in developing bone and kidney, which explains many symptoms of Wolcott-Rallison syndrome [6]. Wolcott-Rallison syndrome should be considered as a differential diagnosis in any child with neonatal diabetes mellitus and hepatic dysfunction or bone dysplasia [5]. Antibodies present in type-1 diabetes mellitus, like anti-tyrosine phosphatase (IA2) antibodies, anti-glutamic acid decarboxylase antibodies (GAD), anti-islet cell antibodies (ICA) and anti-insulin antibodies, are absent.
Conclusions
The glycemic targets for children younger than age six years are 100–180 mg/dL before meals, 110–200 mg/dL at bedtime/overnight, and hemoglobin A1c value should be between 7.5% and 8.5% [7]. Once an infant or a child is stable, short-acting insulin can be substituted with long-acting insulin, like glargine, twice a day [8]. Whether permanent neonatal diabetes mellitus is part of Wolcott-Rallison syndrome or another genetic mutation, it is important to initially stabilize the infant and later do genetic testing to see whether the infant can be given oral sulfonylureas or has to be given insulin therapy.
Acknowledgments
We would like to thank Dr. Sivaramakrishnaiah Sreeramaneni, Dr. Navya Sriramaneni and Dr. Havya Polavarapu for helping us in preparing this manuscript. Special thanks to Aishwarya Sreeramaneni, niece of Dr. Purna Sreeramaneni, who was the inspiration for giving free treatment to the child. We would like to thank the Department of Molecular Genetics, at Exeter University Medical School, for doing the genetic testing for free. We would like to specially thank Dr. Avivit Cohen, Dr. Benjamin Glaser and Dr. Rivka Polak from the Department of Endocrinology, at Hadassah Medical Center, Israel. Special thanks to Dr. David Gillis from the Department of Genetics, at Hadassah Medical Center, Israel.
Footnotes
Conflict of interest
None declared.
References:
- 1.De León DD, Stanley CA. Permanent neonatal diabetes mellitus. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [Internet] Seattle (WA): University of Washington, Seattle; pp. 1993–2017. [Google Scholar]
- 2.Hattersley A. Diabetes genes. Retrieved April 16, 2017 from http://www.diabetesgenes.org/content/transferring-patients-who-have-mutation-kcnj11-or-abcc8.
- 3.Delepine M, Nicolino M, Barrett T, et al. EIF2AK3, encoding translation ation factor 2-alpha kinase 3, is mutated in patients with Wolcott-Rallison syndrome. Nat Genet. 2000;25:406–9. doi: 10.1038/78085. [DOI] [PubMed] [Google Scholar]
- 4.Rubio-Cabezas O, Patch AM, Minton JA, et al. Wolcott-Rallison syndrome is the most common genetic cause of permanent neonatal diabetes in consanguineous families. J Clin Endocrinol Metab. 2009;94:4162–70. doi: 10.1210/jc.2009-1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Julier C, Nicolino M. Wolcott Rallison syndrome. Orphanet J Rare Dis. 2010;5:29. doi: 10.1186/1750-1172-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brickwood S, Bonthron DT, Al-Gazali LI, et al. Wolcott-Rallison syndrome: Pathogenic insights into neonatal diabetes from new mutation and expression studies of EIF2AK3. J Med Genet. 2003;40:685–89. doi: 10.1136/jmg.40.9.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 8.Barone JV, Tillman EM, Ferry RJ., Jr Treatment of transient neonatal diabetes mellitus with subcutaneous insulin glargine in an extremely low birth weight neonate. J Pediatr Pharmacol Ther. 2011;16:291–97. doi: 10.5863/1551-6776-16.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]