Abstract
Background/Aims
Few obesity prevention trials have focused on young children and their families in the home environment, particularly in underserved communities. Healthy Children, Strong Families 2 (HCSF2) is a randomized controlled trial of a healthy lifestyle intervention for American Indian children and their families, a group at very high risk of obesity. The study design resulted from our long-standing engagement with American Indian communities, and few collaborations of this type resulting in the development and implementation of an RCT have been described.
Methods
HCSF2 is a lifestyle intervention targeting increased fruit and vegetable intake, decreased sugar intake, increased physical activity, decreased TV/screen time, and two lesser-studied risk factors: stress and sleep. Families with young children from five American Indian communities nationwide were randomly assigned to a healthy lifestyles intervention (Wellness Journey) augmented with social support (Facebook and text messaging) or a child safety control group (Safety Journey) for one year. After Year 1, families in the Safety Journey receive the Wellness Journey, and families in the Wellness Journey start the Safety Journey with continued wellness-focused social support based on communities’ request that all families receive the intervention. Primary (adult body mass index and child body mass index z-score) and secondary (health behaviors) outcomes are assessed after Year 1 with additional analyses planned after Year 2.
Results
To date, 450 adult/child dyads have been enrolled (100% target enrollment). Statistical analyses await trial completion in 2017.
Lessons Learned
Conducting a community-partnered randomized controlled trial requires significant formative work, relationship building, and ongoing flexibility. At the communities’ request, the study involved minimal exclusion criteria, focused on wellness rather than obesity, and included an active control group and a design allowing all families to receive the intervention. This collective effort took additional time but was critical to secure community engagement. Hiring and retaining qualified local site coordinators was a challenge but was strongly related to successful recruitment and retention of study families. Local infrastructure has also been critical to project success. Other challenges included geographic dispersion of study communities and providing appropriate incentives to retain families in a two-year study.
Conclusions
This multi-site intervention addresses key gaps regarding family/home-based approaches for obesity prevention in American Indian communities. HCSF2’s innovative aspects include substantial community input, inclusion of both traditional (diet/activity) and lesser-studied obesity risk factors (stress/sleep), measurement of both adult and child outcomes, social networking support for geographically dispersed households, and a community selected active control group. Our data will address a literature gap regarding multiple risk factors and their relationship to health outcomes in American Indian families.
Keywords: childhood obesity, diet, physical activity, stress, sleep, social support, community based participatory research
Background
Obesity disproportionately burdens American Indian populations compared to the general US population.1 Our previous research in Wisconsin American Indian communities showed 46% overweight/obesity in children ages 3–8 years2, 3 and even higher prevalence (>70%) in their primary caregivers.2 Once obesity is established in early childhood, it increases the likelihood of obesity in later life and greatly increases future chronic disease risk.4 However, few obesity prevention trials have focused on the vulnerable early childhood period or on families, particularly in underserved communities.5
For the past decade, we have worked in community based participatory research partnerships with four Wisconsin tribes on childhood obesity prevention.6–9 We collaboratively designed and pilot tested a randomized trial of a home-visiting vs. mailed-only healthy lifestyle toolkit for American Indian families with children ages 2–5 years, Healthy Children Strong Families (HCSF1)10, 11, which was funded as part of a collection of studies addressing the lack of randomized controlled trials in American Indian communities.12 In the first trial, HCSF1, both the mailed-only and home-visiting groups demonstrated improvements in child weight in overweight/obese children, adult and child screen time, added sugar and fruit/vegetable intake in children, and adult self-efficacy for diet and activity change.13 However, we found home-visiting was logistically difficult, expensive, and did not provide significant additional benefit.
Here we describe the collaborative development of the Healthy Children Strong Families 2 (HCSF2) randomized controlled trial, which was based on lessons learned from HCSF1. We discuss study design issues and the rationale for addressing these challenges in the context of community-engaged research. The trial is registered at clinicaltrials.gov (NCT01776255).
Research Design and Methods
Our previous work suggests American Indian caregivers have low recognition of overweight or disease risk in young children,14 often viewing heavier children as healthy or “the norm”. We also found high prevalence of overweight, obesity, and early cardiovascular disease risk factors in these children.3 Moreover, our work with community advisory boards suggested adults were far more willing to talk about their children’s health rather than their own health. Therefore, we chose to focus on young children and a primary caregiver, and the pilot communities chose the name “Healthy Children, Strong Families” to express the more holistic community views of health. This name notably avoids use of “overweight” or “obesity”, which are more stigmatizing and not appropriate given the low proportions of children perceived as overweight. These decisions were critical to facilitate recruitment and retention of families, which can be challenging in American Indian communities.
Study design
HCSF2 is a randomized controlled trial of an enhanced version of the HCSF1 toolkit (Wellness Journey) vs. an active control (Safety Journey) (Figure 1). Inclusion criteria included enrolling a child 2–5 years old and having a working cell phone. Exclusion criteria were minimal due to the communities’ value for inclusion in community projects. Dyads were randomized between starting in the Wellness or Safety Journeys, stratified by tribal site and child weight status (overweight vs. healthy weight).15 Randomization was conducted by the REDCap21 data management system (Research Electronic Data Capture data management system) using a permuted block strategy prepared by the study biostatistician.
Figure 1. Healthy Children, Strong Families 2 study design.
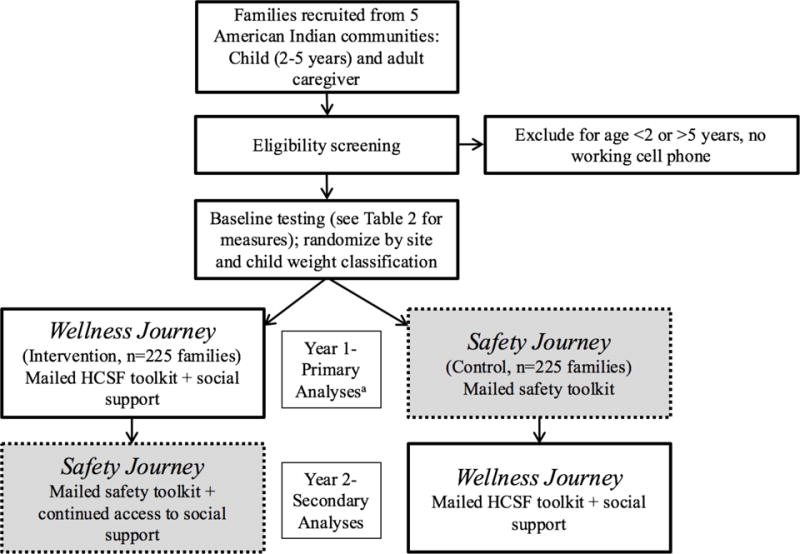
aAfter Year 1, families cross-over into the other Journey. Outcome measures are assessed at baseline, 6 months, 12 months (corresponding to the end of Year 1), 18 months, and 24 months (corresponding to the end of Year 2) as listed in Table 2. Families who randomize into the Wellness Journey first continue to receive the associated social support (cell phone text messaging and access to private Facebook group) after switching to the Safety Journey at the end of Year 1. Families who randomize into the Safety Journey first receive social support at the end of Year 1 when crossing into the Wellness Journey. Because of this design, the primary analyses of the effectiveness of the intervention will be comparison between groups of outcomes assessed at the end of Year 1.
A priority of participating communities was that all families receive the intervention, which has been previously described regarding community-engaged research in tribal communities and necessitates alternatives to the standard RCT.16 Most RCTs to date in American Indian communities have involved more discrete geographic regions, where differences in tribal-specific practices were not significant17. However, substantial differences in geography, language, culture, and traditions among our partner communities across the country suggested control communities would not be possible for HCSF2. A wait-list control group also was considered, but was deemed likely to result in high dropout, particularly in small American Indian communities where some family members may be receiving the intervention while others are waiting. Families who received the intervention also could easily pass on intervention materials to waiting families, resulting in study contamination. In HCSF1, we addressed the request for all families to receive the intervention by delivering an identical wellness toolkit but through different modalities.11 Seeking a more robust design for HCSF2, the research team designed an active control group, allowing for Year 1 to function as a traditional RCT. However, an additional year was included to allow all families to participate in both Journeys. After Year 1, families in the Safety Journey receive the Wellness Journey, while families who were first randomized to the Wellness Journey enter the Safety Journey but continue to receive social support via wellness-related text messages and Facebook content (Figure 1). To our knowledge, this design has not been reported in the literature. For this reason, primary outcomes will be assessed after Year 1, but additional analyses are planned after Year 2 to assess the effects of continued social support despite cessation of the wellness-related mailings (see ‘Statistical considerations’).
Site selection
In choosing American Indian communities to approach for the project, Drs. Adams and Parker selected communities with whom they were currently working or where they had close relationships with community members or wellness staff. Initially, six communities were selected as potential sites; due to changes in leadership, five communities enrolled participants. Each selected community vetted the final study design and provided input, and significant effort was made to take a broad American Indian value- and knowledge-based approach to expand its relevance across regions. Key stakeholders included administrators from tribal clinics, community health programs, schools, colleges, and early child development programs. The University of Wisconsin Health Sciences Institutional Review Board approved this study and serves as the IRB of record for four participating sites; one site approved this study through its own IRB.
Development of enhanced Wellness Journey toolkit
The original toolkit (from HCSF1) targeted four healthy lifestyle behavioral changes: 1) increasing fruit and vegetable intake, 2) decreasing added sugar intake, 3) increasing physical activity, and 4) decreasing TV/screen time. After pilot testing, we worked with our community partners (including tribal wellness staff and community advisory boards) to develop additional lessons targeting 5) stress and 6) sleep in recognition of these emerging obesity risk factors. Initial testing informed development of these lessons; for example, review of dietary records collected during pilot testing indicated high levels of late-night snacking for participating children, suggesting the need to address healthy sleep routines. Each Wellness Journey lesson includes a children’s book related to the topic and items to support behavior change (e.g., pedometers, apple corers, measuring cups, exercise DVDs). We chose the toolkit method because pilot testing showed high levels of acceptability and ease of toolkit use in American Indian families. Lesson topics are listed in Table 1 and are delivered monthly by mail starting with Lesson 1 (Starting the Journey).
Table 1.
Healthy Children Strong Families 2 monthly Wellness Journey mailed topics, including intervention target and associated book(s)/incentives
| Lesson | Book | Incentive |
|---|---|---|
| Starting the Journey (1–6)a | Through the Eyes of the Eagleb | Balloons, disposable camera |
| Naturally Sweet & Nutritiously Delicious (2) | The Very Hungry Caterpillar | Apple slicer, game, recipe cards |
| Fun Family Fitness (3) | Knees Lifted High, Little Running Deer Meets Robert | Pedometers, sidewalk chalk, magnifying glass, jump rope, game cards |
| Sleep Tight (6) | Little Beavers Go To Bed | Glow in the dark stickers, coloring book, stuffed animal |
| Maintaining Harmony (5) | Calm Down Time | Yoga Kids DVD, stress ball, relaxation cards |
| On Track Snacks (1,2,4) | Tricky Treats, Gregory the Terrible Eater | Game, recipe cards |
| Suspending Screen Time (3,4) | The Berenstain Bears and Too Much TV | Move Cube with activity cards |
| Juicing the Benefits (2) | Eating the Alphabet: Fruits & Vegetables from A to Z | Measuring spoons, game |
| Healthy Adventures (3,5) | Oh The Things You Can Do That Are Good For You | RezRobics DVD, stickers, beach ball |
| Gifts from the Land (1) | Plate Full of Color | Seed packets, recipe cards |
| Fruitful Foods (1) | I Will Never Not Ever Eat a Tomato | Dinner set (child sized divided plate, bowl, cup) |
| Fast Lane to Health (1,2,5) | The Berenstain Bears and Too Much Junk Food | Game, recipe cards |
| Maintaining a Healthy Balance (1–6) | HCSF Cookbook and Brag book |
Intervention targets: (1) Increase fruits and vegetables, (2) Decrease soda/sweetened drinks and added sugar intake, (3) Increase physical activity, (4) Decrease TV/screen time, (5) Manage stress, and (6) Develop healthy sleep habits.
Reference citations for books used in the lessons are provided as Supplementary Material (Little Running Deer Meets Robert, Little Beavers Go to Bed, and the HCSF Cookbook are self-published by the research team).
Creation of the Safety Journey curriculum
National data and feedback from community partners revealed American Indian children are disproportionately affected by unintentional injuries for a variety of reasons including poverty, substandard housing, limited access to emergency medical services, and low engagement with primary prevention strategies. Therefore, child safety was chosen as the focus for the active control group, particularly for its lack of relationship to the primary study outcomes. A similar approach was used by Walters et al., who used a family cohesiveness curriculum as a control condition to a cardiovascular prevention intervention in American Indian communities18. Academic and tribal researchers, tribal community members, tribal wellness staff, and national child safety experts collaborated to develop a comprehensive culturally-informed child safety curriculum. The Safety Journey addresses home safety, choking/suffocation, poison control, stranger danger, bike/pedestrian safety, weather safety, water safety, animal safety, car safety, Halloween safety, ATV use, fire safety, and cold weather safety. The Safety Journey curriculum is delivered through monthly mailings that also contain books and materials to support safe behaviors, such as bike reflectors and outlet covers. The development and content of this curriculum have been described in detail elsewhere (Berns et al., under review).
Hiring local community coordinator
The study partners decided employment of a local community member as the project coordinator at each site would best support community based participatory research principles.19 A standard job description was sent to each participating community to provide guidance regarding minimum qualifications and job duties. An initial problem encountered was that each tribe had a different hiring process, and the Memorandum of Understanding we adopted did not stipulate which party had the final say in applicant selection. At two sites, the tribe had a formal process and screened approximately 10–15 potential applicants. At other sites, the process was informal: a person identified as a good candidate was screened and interviewed, particularly for cases where a large applicant pool was not present. Most sites expressed the preference for a female coordinator because of the collection of sensitive measures (e.g., weight, waist circumference) from female participants, which further limited the applicant pool. Efforts were made to hire American Indian coordinators who were well known to the community to facilitate participant recruitment and enrollment. After hiring, local coordinators were trained in-person by the central study coordinator on all research protocols.
Social networking support
The benefits of cell phone messaging and social networking to support behavior change and improve health outcomes are being increasingly recognized.20–25 Our prior work revealed nearly all American Indian families use text messaging and regularly access the Internet for social networking, and the feasibility of technology-related health interventions in American Indian communities has been demonstrated previously.26–28 Therefore, the Wellness Journey is supported by both a text messaging campaign and community-specific Facebook pages for the adult participant to create a “virtual community” to enhance social support for lifestyle change. Several of the participating communities are small, and focus groups indicated Facebook is often used negatively such as for fighting or bullying. Our invitation-only, site-specific group pages were monitored by the central study coordinator to mitigate any potential misuse. The central coordinator posts information to all sites in support of lesson materials (e.g., healthy recipe ideas, sleep tips), and local site coordinators post community-specific information (e.g., announcement of local wellness events). Adult participant interaction with the Facebook page is tracked (e.g., number of “likes”) as a measure of engagement. Text messaging is managed by a mobile research and communications technology company, TargetMobi (Milwaukee, WI), and messages are sent twice weekly on relevant topics to one cell phone per study dyad.
Outcome measures
Measures are collected for both the enrolled child and adult by trained site coordinators at WIC visits, Head Start centers, tribal college/administration buildings, or clinics, depending on the site. All surveys are completed by the adult for themselves and the participating child. Measurement tools were selected to minimize participant burden (e.g., surveys rather than accelerometers to assess physical activity), to align with the qualifications of the survey administrator (e.g., generalized stress measures rather than depression surveys because the study coordinators were not qualified to refer for follow-up counseling or emergency services), and special consideration was made to use tools that had been validated for young children or in American Indian communities. Table 2 lists the included measures and the schedule for data collection.
Table 2.
Timeline for measurement of primary and secondary outcome variables
| Base | 6 m | 12 m | 18 m | 24 m | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| Adult BMI and child zBMI based on height and weight15 | A+C | C | A+C | C | A+C |
| Secondary Outcomes | |||||
| Medical history survey (developed by research team) | A+C | A+C | A+C | ||
| Waist circumference | A+C | C | A+C | C | A+C |
| Diet screeners: based on NHANES 2009–10 for adults35 and on the 2010 National Youth Physical Activity and Nutrition Survey for children36 | A+C | A+C | A+C | ||
| 24-hour dietary recall | A+C | A+C | A+C | ||
| Screen time survey (developed by research team) | A+C | A+C | A+C | ||
| Physical activity surveys: Godin Leisure-Time Exercise Questionnaire for adults37 and Netherlands Physical Activity Questionnaire for children38, 39 | A+C | A+C | A+C | ||
| Sleep survey based on Child Sleep Habits Questionnaire40, 41 and the Pittsburg Sleep Quality Index42 | A+C | A+C | A+C | ||
| Family activity and environment with Family Nutrition and Physical Activity Survey43 with 2 validated questions on food security from the USDA Household Food Security Survey44 | A | A | A | A | A |
| Psychosocial measures: Physical Activity and Nutrition Self-Efficacy Scale45, Perceived Stress Scale (PSS)46–48, SF-12 | A | A | A | ||
| Social network use (developed by research team) | A | A | A | ||
| Cultural Identity: A 6-item measure of acculturation49 | A | ||||
| Control Behaviors | |||||
| Safety survey (developed by the research team) | A | A | A |
A, adult; C, child; m, months.
Study management
Study management is primarily conducted through the coordinating center at the University of Wisconsin, Madison. Tracking of all participant data and schedule management for mailing intervention materials are performed through REDCap, and all intervention materials are mailed from Madison. This approach minimized the burden on local site coordinators, ensured consistency in mailing and tracking participants, and mitigated any potential disruptions if site coordinator turnover were to occur. The entire team meets bi-monthly via videoconferencing to facilitate relationship development among team members and to provide ongoing training/support for the local coordinators. Blinding of outcome assessors was not possible because measurements were taken by site coordinators, the only project employees available at our remote study sites. However, data entry was conducted by two blinded research staff, and an independent data oversight committee carefully monitors the analytical approach to ensure study ethics.
Statistical considerations
The effect of the HCSF2 intervention will be evaluated by comparing Year 1 outcomes for the Wellness Journey group against the Safety Journey group. A sample size of 450 adult/child pairs was based on changes in adult body mass index (BMI) observed in pilot testing to detect an effect size of 0.28 at a two-tailed 0.05 level with power 0.76–0.81 under the assumption of 10–20% Year 1 drop-out. The study has the same power to detect the effect size of 0.28 at a two-tailed 0.05 level for changes in child standardized BMI (zBMI). The effect size of 0.28 represents a mean change of 0.64 for adult BMI and 0.25 for child zBMI. Statistical analyses of outcome data await trial completion in 2017. Data will be analyzed with intention to treat by including all randomized dyads according to randomization, and missing data will be imputed using multiple imputation. The primary comparison will be supplemented by analysis of covariance (ACOVA) for BMI/zBMI at Year 1 with randomization and BMI/zBMI at baseline as model terms. Healthy behaviors and self-efficacy for behavior change from baseline to Year 1 will be analyzed as secondary outcomes using two-sample t-test or Wilcoxon rank sum test, supplemented by ANCOVA. We also will investigate the differential effectiveness of the intervention across different communities by developing exploratory regression models for outcome measures that include interaction terms between the intervention (Wellness Journey) and baseline family characteristics and study site. The secondary comparison of the Wellness vs. the Safety Journey will be based on a two-sample test of the change from baseline to Year 2 to test the effect of social networking under the assumption that the Journeys have the same effects regardless of the order in which they are applied. Finally, as a subgroup analysis, we intend to analyze participants by weight status at baseline to increase the clinical applicability of our findings and to determine if participants are crossing weight status group (e.g., normal weight to overweight).
Results
Recruitment was staggered by site from February 2013 to April 2015. Primary recruitment sites included Head Start centers, social service centers, and tribal clinics. Informational flyers also were distributed among community spaces. Community site coordinators collected 659 interest forms, and 527 participants were screened during the recruitment phase. Twenty-five participants failed screening (e.g., child not in targeted age range, moving out of area, no cell phone, or declined to participate), leaving 502 eligible participants. Of these participants, we were unable to collect baseline data on 52 families to enroll them in the study. To date, 450 adult/child (age 2–5 years) dyads have been enrolled from five communities (four rural and one urban site), representing 100% of our target enrollment. We anticipate project completion in March 2017 and will present study findings to each community along with dissemination to the wider academic community. As of October 2016, each community has received a summary of their participating families’ baseline data, each family has received portions of their individual baseline data, and each community will participate in the review and revision of any resulting study manuscripts in alignment with community based participatory research principles.
Lessons Learned
Here we describe lessons learned in the development and implementation of the trial. These and additional lessons related to community-based work are summarized in Table 3.
Table 3.
Lessons learned from community engagement using community-based participatory research approaches
| Component | Example |
|---|---|
| Study design |
|
| Wellness toolkit |
|
| Social support |
|
| Measures |
|
| American Indian cross-cultural considerations |
|
Incentives
Previous work in American Indian communities and ongoing feedback suggested incentives were an important component to increase retention. Community partners suggested Wal-Mart® gift cards would be desirable; one site did not have a local Wal-Mart®, and gift cards to a local grocery store are provided instead. All families receive a $50 gift card after completing testing at baseline, 12 months, and 24 months ($150 total). Families randomly selected to complete dietary recalls receive an additional $25 gift card at each time point (n=25 per community). Lesson-specific incentives, such as cooking utensils, balls, books, games, and pedometers, are included in each mailed lesson for the Wellness Journey. Safety-focused incentives, including bike reflectors, outlet covers, and books, are provided during the Safety Journey. Although small gifts for the child (<$10) are provided at the 6-month and 18-month visits, gift cards are not given because these visits are significantly shorter (compared to baseline, 12 months, and 24 months). We found that fewer participants showed up for these study visits or many who did were under the impression they were receiving a gift card, and other studies have cited misunderstanding of incentives as a barrier to retention.29
Social networking
An unexpected finding from the study has been the benefits of Facebook for promoting participant retention. The central and local site coordinators spend a large proportion of their time scheduling participant visits. We found that many participants screen phone calls and are difficult to reach by phone. Moreover, many participants in low-income communities have periodic disruptions of their cell phone service or change their number for a variety of reasons. However, we have been successful in reaching difficult-to-schedule participants through Facebook messaging, which would not have been possible without the creation of site-specific group pages. Participant feedback on the use of Facebook has been positive. Feedback on the weekly text messages has been mixed; with cell-phone number turnover and loss of service common in many rural communities, the challenges of phone-based intervention approaches should be considered in the future.
Site coordinators
We have discovered that the local site coordinators are crucial to the success of this project, as they are responsible for recruitment, retention, and data collection. For this study, the five coordinators were hired, housed, and managed in different ways. For example, one was hired through and housed in the tribal clinic, while another was hired through the early childhood education unit. Being associated with a unit that was already functional was critical for timely completion of job duties. For example, one coordinator was already working part-time in the tribal clinic and had access to office space, a phone, and a computer. At another site, it took months to secure these essentials for the study coordinator, making it very challenging to launch the project there. Another lesson was that some tribes required the site coordinator to be hired as tribal staff, which enhances tribal infrastructure. This approach was often slower, complicated by the distance between the research team and sites that would have allowed for in-person meetings. Some of the issues could be attributed to the lack of clarity in the Memorandum of Understanding regarding the hiring process. Future studies should articulate a defined protocol for hiring a site coordinator and the entity that has the ultimate authority in hiring and in local supervision.
Community based participatory research with American Indian communities
Maintaining an intervention for two years is difficult, especially in tribal communities where infrastructure may not exist to support the project. Moreover, the inclusion of diverse communities nationwide (5 states) strengthened the study but presented challenges associated with the large geographic spread. Other studies in American Indian communities have reported similar challenges that also resulted in changes to the study design, including a decrease in planned follow-up time after a lag in recruitment.26 We learned that conducting a multisite randomized trial using community-engaged approaches requires flexibility in several different areas. For example, it was important to engage in discussions with more potential sites than we needed because of likely dropout during the early stages of project planning. In addition, every site presented a different challenge that was associated with the study design. For example, a different number of care-giver child dyads were recruited at each site, two sites experienced coordinator turnover mid-project, and we had to be flexible with which sites started first due to lack of readiness in communities that were initially targeted with the staggered enrollment. Multiple studies conducted in American Indian communities have confirmed the importance of tribal support in ensuring project success30, 31, which can be challenging when tribal elections are held every 2 years. During a 5-year grant, this could potentially include 3 cycles of tribal council members from whom the researchers must earn trust and support.
Discussion
We have described the methods and study design issues of an innovative intervention to promote health in American Indian families with young children, Healthy Children, Strong Families 2, the first national family-based obesity prevention project in American Indian communities. HCSF2 has the following strengths:
Healthy Children, Strong Families 2 utlized a home-based approach. Other RCTs have been successfully implemented in American Indian communities in schools30, 32; another study focused on the health care setting but included home-focused elements.33 However, HCSF2 is the first to target both adults and children primarily within the home in recognition of the critical importance of family dynamics in promoting wellness. HCSF2 supports families in multiple ways by increasing internal resiliency to outside obesogenic forces and is unique in providing tools for change rather than just an educational lesson. Toolkits containing lessons, children’s books, and healthy lifestyle reinforcers (e.g., cooking supplies, exercise DVDs) are mailed monthly; participant feedback from previous focus group testing has indicated the excitement produced by a child receiving a monthly package in the mail has enhanced engagement and behavior change.13
Another strength is the focus on the early childhood period when health habits are developing. This focus addresses key gaps regarding family/home-based approaches for American Indian children, who are at particularly high risk for developing obesity and associated chronic diseases. Moreover, our approach considers traditional determinants of obesity risk, such as diet and activity, but also novel risk factors for obesity, namely stress and sleep. Data on these factors and their relationship to health outcomes are lacking for this population, and few interventions have addressed these important determinants of health risk.
HCSF2 is the first study, to our knowledge, to evaluate the use of social support for healthy lifestyle change in American Indian communities (text messaging and Facebook). These platforms allow for information exchange for both individual and community support, which is particularly relevant for geographically dispersed and economically limited households. Other aspects of the participating communities have been instrumental in this study: HCSF2 was designed and implemented with strong community engagement, which was critical to study success thus far. Initial testing of intervention materials in the HCSF1 trial indicated feasibility and community acceptance, and this successful pilot testing significantly informed the development of HCSF2. Finally, we feel this study was strengthened by the inclusion of a diverse sample of urban and rural families in 5 states across the county, representing a unique contribution to the literature.
Conclusion
We have addressed the HCSF2 study design and the challenges our research team encountered. We also describe the solutions we employed to overcome these problems during the implementation of this large randomized trial of a healthy lifestyles intervention in diverse American Indian communities across multiple states. A review of 165 studies in underserved populations found similar barriers and challenges, but very few randomized trials have been conducted in American Indian communities.34 The findings from this study may help future researchers understand the complexity and sensitivity needed when working with tribal or other underserved communities, including significant formative work, relationship- and trust-building, extensive planning, a high degree of flexibility, and respect for tribal or community-specific protocols. We are optimistic that data generated from this randomized controlled trial will significantly enhance our understanding of early child health in the context of American Indian families and strengthen the ability of researchers to effectively partner with tribal and other diverse communities to promote health and wellness.
Supplementary Material
Acknowledgments
We gratefully acknowledge all the communities and families who participated in the design, development, and implementation of the Healthy Children Strong Families intervention (the HCSF1 pilot and the expanded HCSF2 described here). Without their continued engagement, this project would not be possible. We also are indebted to the research coordinators at each site who have worked so hard to recruit and retain our participants. We also thank Dr. Jared B. Jobe for his valuable assistance during project development and his leadership of our Data Monitoring Board.
Footnotes
Clinical Trials Registration: NCT01776255, Healthy Children, Strong Families: American Indian Communities Preventing Obesity (HCSF2)
Declaration of Conflicting Interests
The authors declare that there are no conflicts of interest.
References
- 1.Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska Native populations. PloS one. 2014;9(1):e80973. doi: 10.1371/journal.pone.0080973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams AK, Quinn RA, Prince RJ. Low recognition of childhood overweight and disease risk among Native-American caregivers. Obes Res. 2005;13(1):146–52. doi: 10.1038/oby.2005.19. [DOI] [PubMed] [Google Scholar]
- 3.Adams A, Prince R, Webert H. The Wisconsin Nutrition and Growth Study (WINGS), a participatory research project with three Wisconsin tribes. The Great Lakes EpiCenter News. 2004;5:1–3. http://www.glitc.org/epicenter/publications. [Google Scholar]
- 4.Birch L, Parker L, Burns A, editors. Early childhood obesity prevention policies Institute of Medicine. Washington, D.C.: National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skouteris H, McCabe M, Swinburn B, Newgreen V, Sacher P, Chadwick P. Parental influence and obesity prevention in pre-schoolers: a systematic review of interventions. Obes Rev. 2010;12(5):315–28. doi: 10.1111/j.1467-789X.2010.00751.x. [DOI] [PubMed] [Google Scholar]
- 6.Adams A, Miller-Korth N, Brown D. Learning to work together: developing academic and community research partnerships. WMJ: official publication of the State Medical Society of Wisconsin. 2004;103(2):15–9. [PubMed] [Google Scholar]
- 7.Adams AK, Harvey H, Brown D. Constructs of health and environment inform child obesity prevention in American Indian communities. Obesity. 2008;16(2):311–7. doi: 10.1038/oby.2007.71. [DOI] [PubMed] [Google Scholar]
- 8.Adams A. Understanding community and family barriers and supports to physical activity in American Indian children. Journal of public health management and practice: JPHMP. 2010;16(5):401–3. doi: 10.1097/PHH.0b013e3181f51636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindberg SM, Adams AK, Prince RJ. Early predictors of obesity and cardiovascular risk among American Indian children. Maternal and child health journal. 2012;16(9):1879–86. doi: 10.1007/s10995-012-1024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaRowe TL, Wubben DP, Cronin KA, Vannatter SM, Adams AK. Development of a culturally appropriate, home-based nutrition and physical activity curriculum for Wisconsin American Indian families. Preventing chronic disease 4 United States. 2007:A109. [PMC free article] [PubMed] [Google Scholar]
- 11.Adams AK, LaRowe TL, Cronin KA, Prince RJ, Wubben DP, Parker T, et al. The Healthy Children, Strong Families intervention: design and community participation. J Prim Prev. 2012;33(4):175–85. doi: 10.1007/s10935-012-0275-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jobe JB, Adams AK, Henderson JA, Karanja N, Lee ET, Walters KL. Community-responsive interventions to reduce cardiovascular risk in American Indians. J Prim Prev. 2012;33(4):153–9. doi: 10.1007/s10935-012-0277-9. [DOI] [PubMed] [Google Scholar]
- 13.Adams AK, LaRowe TL, Cronin KA, Prince R, Jobe JB. Annual Scientific Meeting of The Obesity Society. Orlando, FL: 2011. Healthy Children, Strong Families: Results of a Randomized Trial of Obesity Prevention for Preschool American Indian Children and Their Families. 2011. [Google Scholar]
- 14.Adams AK, Quinn RA, Prince RJ. Low recognition of childhood overweight and disease risk among Native-American caregivers. Obesity research. 2005;13(1):146–52. doi: 10.1038/oby.2005.19. [DOI] [PubMed] [Google Scholar]
- 15.Kuczmarski RJ, Ogden CL, Grummer LM, et al. CDC growth charts: United States, Advance data from vital and health statistics. Health Statistics. 2000;314:2–27. [Google Scholar]
- 16.Henry D, Tolan P, Gorman-Smith D, Schoeny M. Alternatives to Randomized Control Trial Designs for Community-Based Prevention Evaluation. Prev Sci. 2016 doi: 10.1007/s11121-016-0706-8. [DOI] [PubMed] [Google Scholar]
- 17.Lee ET, Jobe JB, Yeh J, Ali T, Rhoades ER, Knehans AW, et al. A cardiovascular risk reduction program for American Indians with metabolic syndrome: the Balance Study. J Prim Prev. 2012;33(4):187–96. doi: 10.1007/s10935-012-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walters KL, LaMarr J, Levy RL, Pearson C, Maresca T, Mohammed SA, et al. Project həli?dx/Healthy Hearts Across Generations: development and evaluation design of a tribally based cardiovascular disease prevention intervention for American Indian families. J Prim Prev. 2012;33(4):197–207. doi: 10.1007/s10935-012-0274-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 20.Ackland R. Social Network Services as Data Sources and Platforms for e-Researching Social Networks. Soc Sci Comput Rev. 2009;27(4):481–92. [Google Scholar]
- 21.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2011 Sep 9; doi: 10.1016/j.jbi.2011.08.017. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connell RS. Academic libraries, Facebook and MySpace, and student outreach: a survey of student opinion portal. Libraries & the Academy. 2009;9:25–36. [Google Scholar]
- 23.Buffardi LE, Campbell WK. Narcissism and social networking Web sites. Pers Soc Psychol Bull. 2008;34:1303–14. doi: 10.1177/0146167208320061. [DOI] [PubMed] [Google Scholar]
- 24.Cain J, Scott DR, Akers P. Pharmacy students’ Facebook activity and opinions regarding accountability and e-professionalism. Am J Pharm Educ. 2009;73:104. doi: 10.5688/aj7306104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 26.Henderson JA, Chubak J, O’Connell J, Ramos MC, Jensen J, Jobe JB, et al. Design of a randomized controlled trial of a web-based intervention to reduce cardiovascular disease risk factors among remote reservation-dwelling American Indian adults with type 2 diabetes. J Prim Prev. 2012;33(4):209–22. doi: 10.1007/s10935-012-0276-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gorman JR, Clapp JD, Calac D, Kolander C, Nyquist C, Chambers CD. Creating a culturally appropriate web-based behavioral intervention for American Indian/Alaska Native women in Southern California: the healthy women healthy Native nation study. Am Indian Alsk Native Ment Health Res. 2013;20(1):1–15. doi: 10.5820/aian.2001.2013.1. [DOI] [PubMed] [Google Scholar]
- 28.Raghupathy S, Forth AL. The HAWK2 program: a computer-based drug prevention intervention for Native American youth. Am J Drug Alcohol Abuse. 2012;38(5):461–7. doi: 10.3109/00952990.2012.694531. [DOI] [PubMed] [Google Scholar]
- 29.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 30.Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harding A, Harper B, Stone D, O’Neill C, Berger P, Harris S, et al. Conducting research with tribal communities: sovereignty, ethics, and data-sharing issues. Environ Health Perspect. 2012;120(1):6–10. doi: 10.1289/ehp.1103904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stone EJ, Norman JE, Davis SM, Stewart D, Clay TE, Caballero B, et al. Design, implementation, and quality control in the Pathways American-Indian multicenter trial. Prev Med. 2003;37(6 Pt 2):S13–23. doi: 10.1016/j.ypmed.2003.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karanja N, Aickin M, Lutz T, Mist S, Jobe JB, Maupome G, et al. A community-based intervention to prevent obesity beginning at birth among American Indian children: study design and rationale for the PTOTS study. J Prim Prev. 2012;33(4):161–74. doi: 10.1007/s10935-012-0278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nicholson LM, Schwirian PM, Groner JA. Recruitment and retention strategies in clinical studies with low-income and minority populations: Progress from 2004–2014. Contemp Clin Trials. 2015;45(Pt A):34–40. doi: 10.1016/j.cct.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 35.Sugarman JR, Brenneman G, LaRoque W, Warren CW, Goldberg HI. The urban American Indian oversample in the 1988 National Maternal and Infant Health Survey. Public health reports. 1994;109(2):243–50. [PMC free article] [PubMed] [Google Scholar]
- 36.Eaton DK, Olsen EO, Brener ND, Scanlon KS, Kim SA, Demissie Z, et al. A comparison of fruit and vegetable intake estimates from three survey question sets to estimates from 24-hour dietary recall interviews. Journal of the Academy of Nutrition and Dietetics. 2013;113(9):1165–74. doi: 10.1016/j.jand.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amireault S, Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Perceptual and motor skills. 2015;120(2):604–22. doi: 10.2466/03.27.PMS.120v19x7. [DOI] [PubMed] [Google Scholar]
- 38.Chinapaw MJ, Mokkink LB, van Poppel MN, van Mechelen W, Terwee CB. Physical activity questionnaires for youth: a systematic review of measurement properties. Sports Med. 2010;40(7):539–63. doi: 10.2165/11530770-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39.Janz KF, Broffitt B, Levy SM. Validation evidence for the Netherlands physical activity questionnaire for young children: the Iowa bone development study. Res Q Exerc Sport. 2005;76(3):363–9. doi: 10.1080/02701367.2005.10599308. [DOI] [PubMed] [Google Scholar]
- 40.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. Journal of developmental and behavioral pediatrics: JDBP. 2008;29(2):82–8. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- 41.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–51. [PubMed] [Google Scholar]
- 42.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 43.Ihmels MA, Welk GJ, Eisenmann JC, Nusser SM. Development and preliminary validation of a Family Nutrition and Physical Activity (FNPA) screening tool. Int J Behav Nutr Phys Act. 2009;6:14. doi: 10.1186/1479-5868-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- 45.Latimer L, Walker LO, Kim S, Pasch KE, Sterling BS. Self-efficacy Scale for Weight Loss among Multi-ethnic Women of Lower Income: A Psychometric Evaluation. Journal of Nutrition Education and Behavior. 2011;43(4):279–83. doi: 10.1016/j.jneb.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 47.Cohen S, Williamson G, Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988. Perceived stress in a probability sample of the United States. [Google Scholar]
- 48.Korn L, Logsdon RG, Polissar NL, Gomez-Beloz A, Waters T, Ryser R. A randomized trial of a CAM therapy for stress reduction in American Indian and Alaskan Native family caregivers. Gerontologist. 2009;49(3):368–77. doi: 10.1093/geront/gnp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goins RT, Spencer SM, McGuire LC, Goldberg J, Wen Y, Henderson JA. Adult caregiving among American Indians: the role of cultural factors. The Gerontologist. 2011;51(3):310–20. doi: 10.1093/geront/gnq101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


