Abstract
Studies on the occurrence of homebound and the factors influencing it are available. However, the study of community homebound in China is still in its preliminary stage. No previous studies about this issue are available. This study aims to assess the occurrence of and factors influencing homebound elderly in Chinese communities and to provide a basis for effective intervention and prevention of homebound elderly people.
One sample community from three provinces was randomly selected. Investigations were performed on the selected communities and 2180 elderly people were chosen as the research subjects. Unified survey scales were used. Home visit and face-to-face interviews were performed to ensure that no single qualified survey respondent was missed.
The rate of morbidity in homebound elderly Chinese community was found to be 15.49% and it gradually increased with age, and also with a lower education or poorer Activities of Daily Living (ADL). Single factor analysis showed that general situation, living habits, physical condition, mental condition, society, social support, and other factors affected the occurrence of community homebound elderly. Women were more likely to be homebound than men (P < .05). Having a spouse or high income reduced the rate of morbidity in the homebound elderly (P < .05). Multifactor regression analysis revealed that poor ADL, depression, hearing impairment, being old, no exercise, and low social support are the main influencing factors.
Appropriate measures should be taken based on the specific influencing factor to prevent the occurrence of homebound.
Keywords: current status, homebound elderly people, influencing factors
1. Introduction
According to The National Economic and Social Development Statistics Announcement of the People's Republic of China, 2014, by the end of 2014, elderly people aged >60 years accounted for 15.5% of the total population of China. These elderly people and their health conditions have become the focus of the entire society.[1,2] China's problem of aging population has become serious. As the elderly people grow even older, their physiological functions and immunity gradually decline, which leads to increasingly serious health problems. At the same time, homebound results in the reduction of elderly people's physical and cognitive functions, weakens their self-maintenance ability in daily living, and intensifies their psychological stress. The lack of communication with the outside world eventually result in lying on bed or dementia, seriously impairing the elderly people's physical and mental health and life quality, and also placing huge pressure on their families, society, and social medical treatment.[3,4] Therefore, the concern on elderly homebound is essentially important in maintaining and improving the quality of life of elderly people, and also alleviating the burden on family and society, as well as preventing lying on bed and dementia.
Researchers have performed a number of studies on the occurrence of homebound and the factors influencing it and developed a variety of measures. However, the study of community homebound in China is still in its preliminary stage; so far the available investigation is confined only to an elderly homebound survey of a particular urban community, with limited scope. No studies on the occurrence of and factors influencing elderly homebound in Chinese urban community are available. Hence in this study, Chinese urban elderly people were chosen for investigating the occurrence of and the factors influencing elderly homebound in Chinese urban community, and provide a basis for community medical personnel to give individual intervention.
2. Subjects and methods
2.1. Subjects
The inclusion criteria were as follows: elderly people (aged ≥60 years) living in urban communities (having resided in the community for >1 year) in China were enrolled in this study.
The exclusion criteria were as follows: people who had serious speech impediment, hearing impairment, or visual impairment and those who were laid up.
Informed consent was obtained from all enrolled subjects. The study was approved by the Ethics Committee of the Local Disease Control and Prevention Center (2013150101).
The sample size was calculated as follows: Based on the related foreign studies, the rate of morbidity in community elderly homebound was 5.9% to 18.6%.[5,6] In a Chinese study, the reported rate of morbidity in elderly homebound of a particular urban community was 17.59% to 18.8%.[7] In the present study, the rate of morbidity of 18% was used, and the sample size was calculated using the formula N = Z2PQ/(0.1P)2 which is simplified as N = 400Q/P(Q = 1 − P), where Q = 1 − P, Z (=1.96 ≈ 2.00) represents the Chi-squared value.[8] Accordingly, the sample size calculated was N = 1822. Considering the possible loss of data and nonresponse, the sample size was increased by 10%. Hence, the sample size of this study should no more than 2004 subjects.
2.2. Sampling method
Random cluster sampling method was used in this study. At Stage 1, Anhui Province (South China) and Hebei Province (North China) were selected based on the geographical location. At Stage 2, the 11 cities of the Hebei Province were numbered and 2 cities, that is, Baoding City and Tangshan City, were randomly drawn; similarly, the 16 cities of Anhui Province were numbered and 1 city, that is, Bengbu City, was randomly drawn. At Stage 3, 1 sample community (Dajijia community) from the 159 communities of Baoding City, 1 sample (Diaoyutai community) from the 363 communities of Tangshan City, and another sample (Yan’an community) from the 204 communities of Bengbu City were randomly selected. From these communities, a total of 2180 qualified elderly people were enrolled. A total of 2133 questionnaires were handed out to the subjects and were retrieved. Among all the retrieved questionnaires, 28 were invalid. The remaining 2105 copies were regarded as valid. The percentage of valid questionnaires was 98.69%.
2.3. Survey
From July 2013 to December 2013, a survey was conducted among 2180 qualified elderly people from the selected communities. Unified survey scales were used including homemade general situation questionnaire, Activities of Daily Living (ADL) ability scale, Social Support Rating Scale (SSRS), Geriatric Depression Scale Short Form (GDS-15), and homebound condition assessment scale in Chinese version. Home visit and face-to-face interviews were performed among these research subjects to ensure that no single qualified survey respondent was missed. Questionnaires were retrieved and examined on the spot to ensure that there were no unfilled/missed items in the questionnaire.
2.4. Assessment
Twenty senior professors were selected from the Department of Health Statistics, Epidemiology, and Nursing, eventually an expert consultation group was constituted. All members of this group had the title of deputy senior or above and were engaged in professional teaching and research study for >10 years. The Delphi expert enquiry method was adopted to revise the content of the questionnaire.
2.4.1. General information
Subject's age, gender, height, weight, race, marital status, educational level, occupation, income, and health insurance.
2.4.2. Living habits
Physical exercise, hobbies, smoking, and drinking.
2.4.3. Physical condition
Subject's hearing ability, eyesight, chronic diseases, medications, and ADL ability. Among these indexes, the ADL was assessed using the ADL ability scale described by Lawton and Brody in 1969.[9] The ADL scale has 14 items and 4 grades. The studied subjects were assigned a score based on their ability or assistance needed to perform these activities, that is, 1, 2, 3, and 4 points, respectively, for “can do it by yourself,” “a bit difficult,” “need help,” and “cannot do.” Hence, the final score ranged from 14 to 56. A final score of 14 points means totally normal; a final score >14 points implies a certain level of dysfunction; and a score of >22 points indicates distinct dysfunction. The Cronbach α coefficient of the scale was set as 0.85 while the repeatability was 0.93. This scale was used to investigate the daily living of the studied subjects for the recent week.
2.4.4. Social conditions
Social support, participation in community or social activities, and networking with friends, relatives, and neighbors. Among these indexes, social support was assessed using the SSRS designed by Xiao.[10] This scale was designed and utilized first in 1986, and some minor changes were made in 1990 and further promoted. The scale contained 3 dimensions and 10 items, that is, objective support (3 items), subjective support (4 items), and utilization of support (3 items). The Cronbach α coefficient of the scale ranged from 0.89 to 0.94, while the repeatability was 0.92. The sum score of the 10 items was the final score of social support, which ranged from 8 to 66 points. A final score of ≤22 points was treated as low level; a final score of 23 to 44 points was treated as medium level; and a final score of 45 to 66 points was treated as high level. A higher score implies more social support can be obtained.
2.4.5. Psychological condition
Self-assessment of health condition, depression, and loneliness. GDS-15[11–13] was adopted to grade the level of depression in the elderly people. Out of 15 points, those who scored 0 to 5 points were considered as normal elderly people, while those who scored 6 points or higher were considered as depressed. A higher score indicates more serious depression.
2.4.6. Homebound status
People who go out of house less than once a week are considered as homebound.[14] (The going out record of the month before the survey was used as the reference data. If the going-out counts for each week of the month differ, the total counts for that 1 month averaged by the number of weeks was considered.)
2.5. Statistical analysis
All obtained data were statistically analyzed using SPSS 13.0 software. Measured data were expressed as  and analyzed using t test, while count data were analyzed using Chi-square test. The statistically significant results of single factor analysis were further processed through stepwise logistic regression analysis. The inclusion criteria for α was 0.05, while the exclusion criteria for α was 0.10. P < .05 was considered statistically significant.
and analyzed using t test, while count data were analyzed using Chi-square test. The statistically significant results of single factor analysis were further processed through stepwise logistic regression analysis. The inclusion criteria for α was 0.05, while the exclusion criteria for α was 0.10. P < .05 was considered statistically significant.
3. Results
3.1. General factors affect homebound
From the selected communities, 2180 qualified elderly people were initially enrolled. Among them 2133 people were investigated (response rate of 97.84%). Among all the retrieved questionnaires, 28 were invalid and hence the remaining 2105 were regarded as valid. The percentage of valid questionnaires was 98.69% (Fig. 1).
Figure 1.
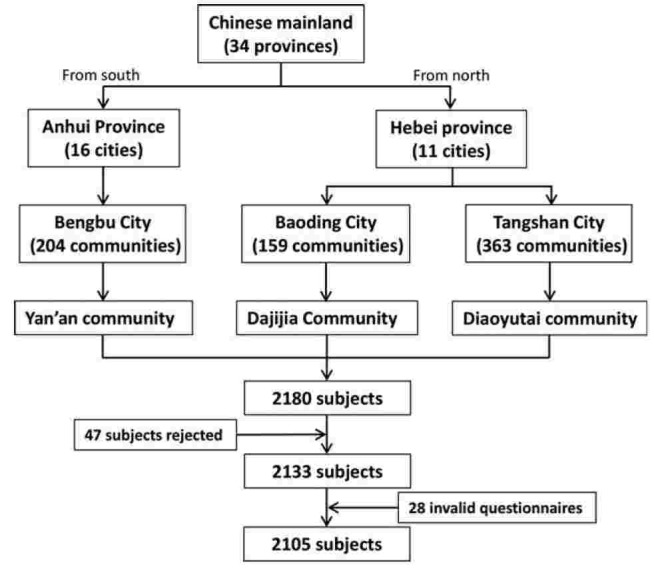
A flow diagram summarizes the selection of studies.
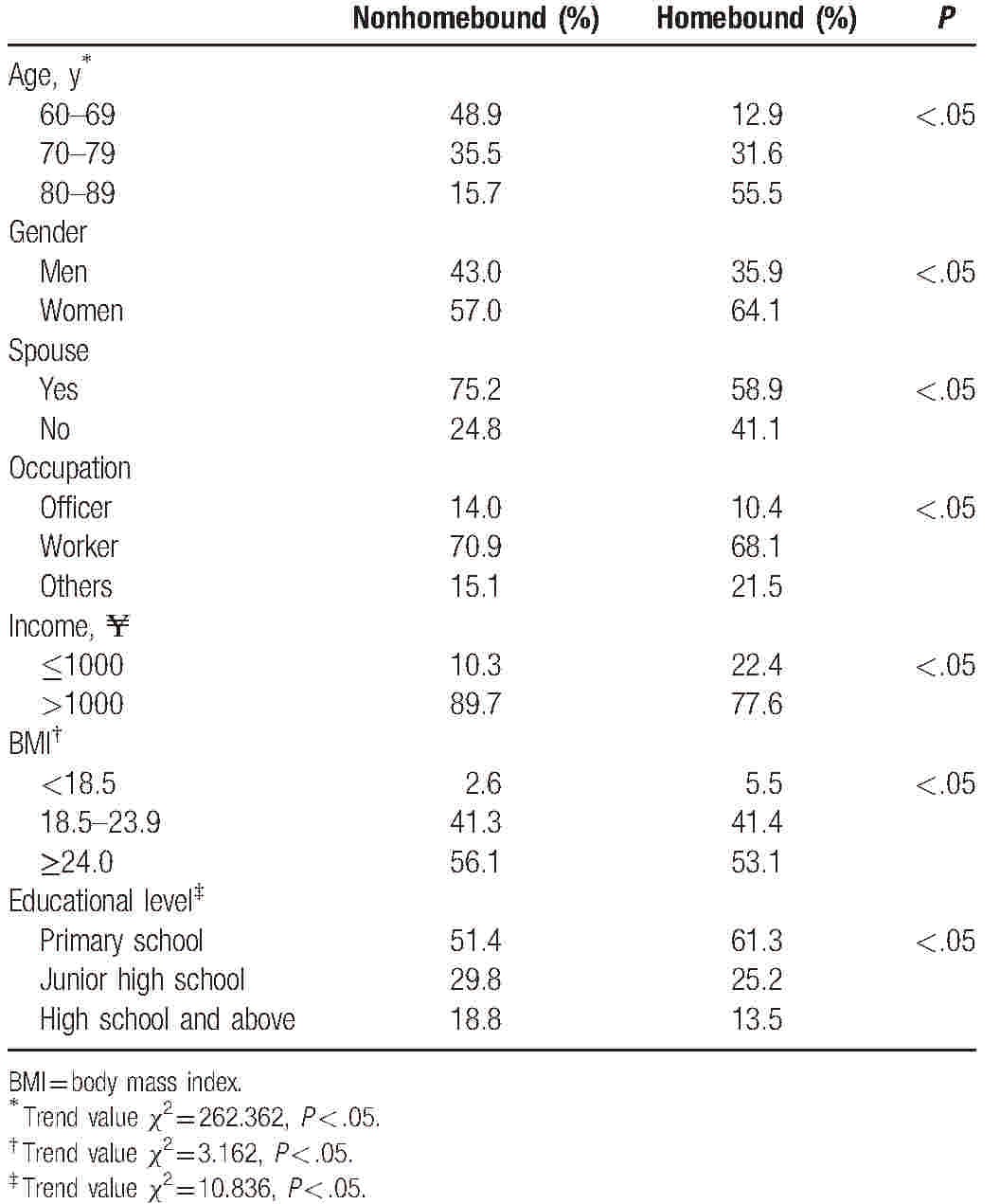
The ages of respondents ranged from 60 to 101 years including 882 (41.9%) men with a mean age of 71.74 ± 8.18 years and 1223 (58.1%) women with a mean age of 72.00 ± 8.61 years. Among these elderly people, 326 people (209 women and 117 men) were regarded as homebound, providing a rate of morbidity of homebound of 15.49%. It was found that older and less educated people were probably more homebound (P < .05) (Table 1). It was also found that women with low income and without a spouse showed a higher prevalence of homebound than men, high income group, and those with a spouse (P < .05).
Table 1.
General factors affect homebound (n = 2105).
3.2. Living habits affect homebound
Those elderly people who have hobbies, exercised regularly, and do not smoke or drink showed a lower prevalence of homebound than the other groups.
Compare with the nonhomebound, those homebound elderlies have high rate of no hobby (87.4% vs 81.3%) and low rate of hobby (12.6% vs 18.7%), The difference is statistically significant (P < .05). The homebound were doing less exercise (no exercise 48.8%, used to do, but not now 11.3%, sometimes 9.2%, often 30.7%), then the nonhomebound were doing more exercise (no exercise 14.3%, used to do, but not now 2.2%, sometimes 12.8%, often 70.7%), The difference is statistically significant (P < .05). The rates of smoking and drinking of the 2 groups (homebound vs nonhomebound) are 13.5% versus 18.7% and 7.1% versus 15.5%, respectively. The P values of the 2 indicators (smoking and drinking) between the 2 groups are both less than .05, which means the differences between the 2 groups are statistically significant at a confidence level of 95%.
3.3. Physical, social connection, and psychological condition affect homebound
3.3.1. Physical condition
With visual impairment, hearing impairment, chronic diseases, and medication, the prevalence of homebound elderly people was higher than the other groups. With ADL ability, the prevalence of homebound was higher, and the difference was statistically significant (P < .05) (Table 2).
Table 2.
Physical, social, and psychological condition affect homebound.
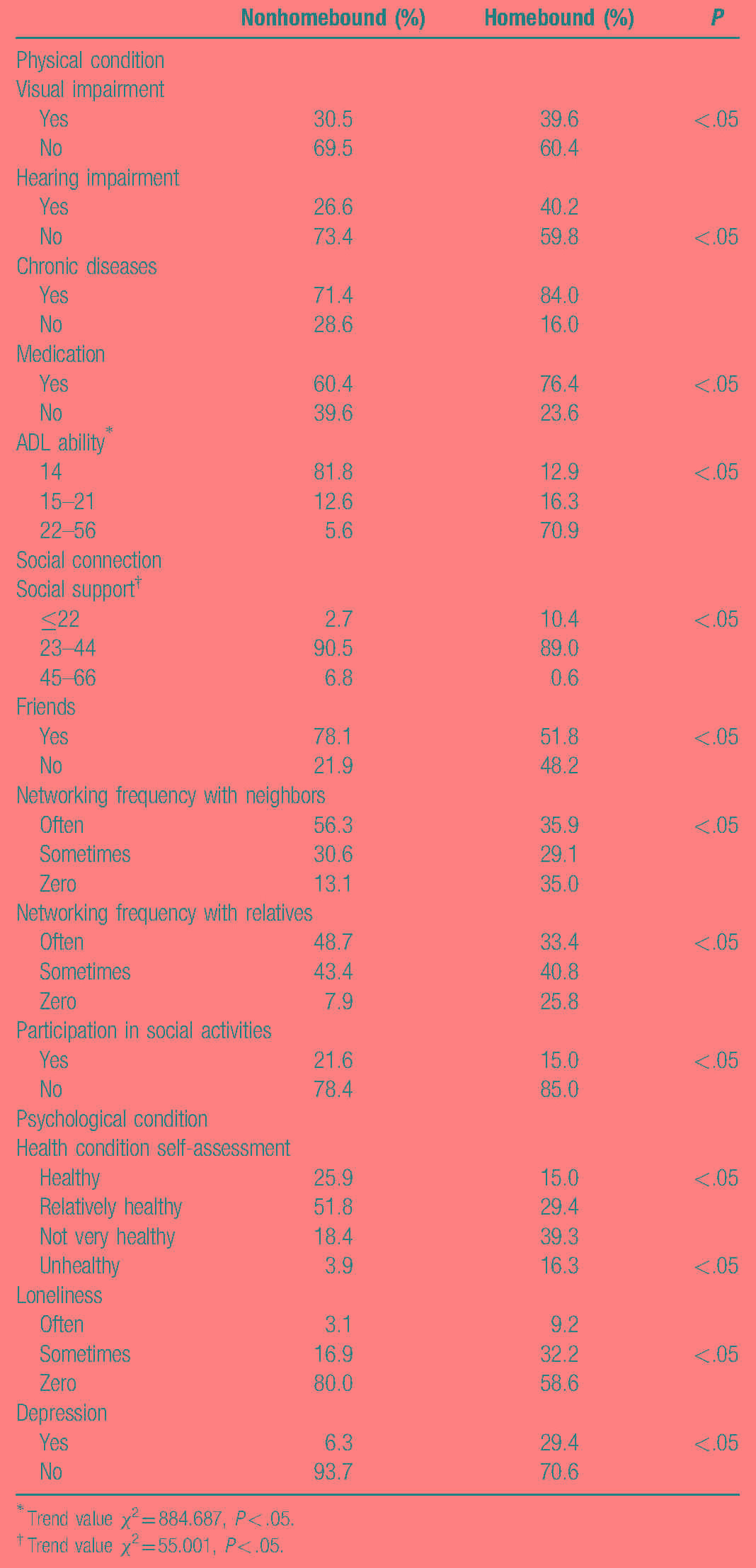
Those elderly people with visual impairment, hearing impairment, chronic diseases, and medication showed a higher prevalence of homebound than the other groups (P < .05). A poorer ADL ability resulted in a higher prevalence of homebound (P < .05), and the differences were statistically significant (Table 2).
3.3.2. Social connection
Less social support resulted in higher prevalence of elderly homebound, and the difference was statistically significant (P < .05). Those who have frequent contacts with friends, neighbors, and relatives, and frequently participated in social activities showed a lower prevalence of homebound than the other groups (P < .05), and the difference was statistically significant (Table 2).
3.3.3. Psychological condition
Those homebound elderly people who graded themselves as relatively healthy in self-assessment of health level showed the lowest rate of morbidity (P < .05). Those homebound elderly people who usually felt lonely showed a high rate of morbidity (P < .05). Those homebound elderly people who experienced depression showed a higher rate of morbidity than those have no symptoms of depression (P < .05) (Table 2).
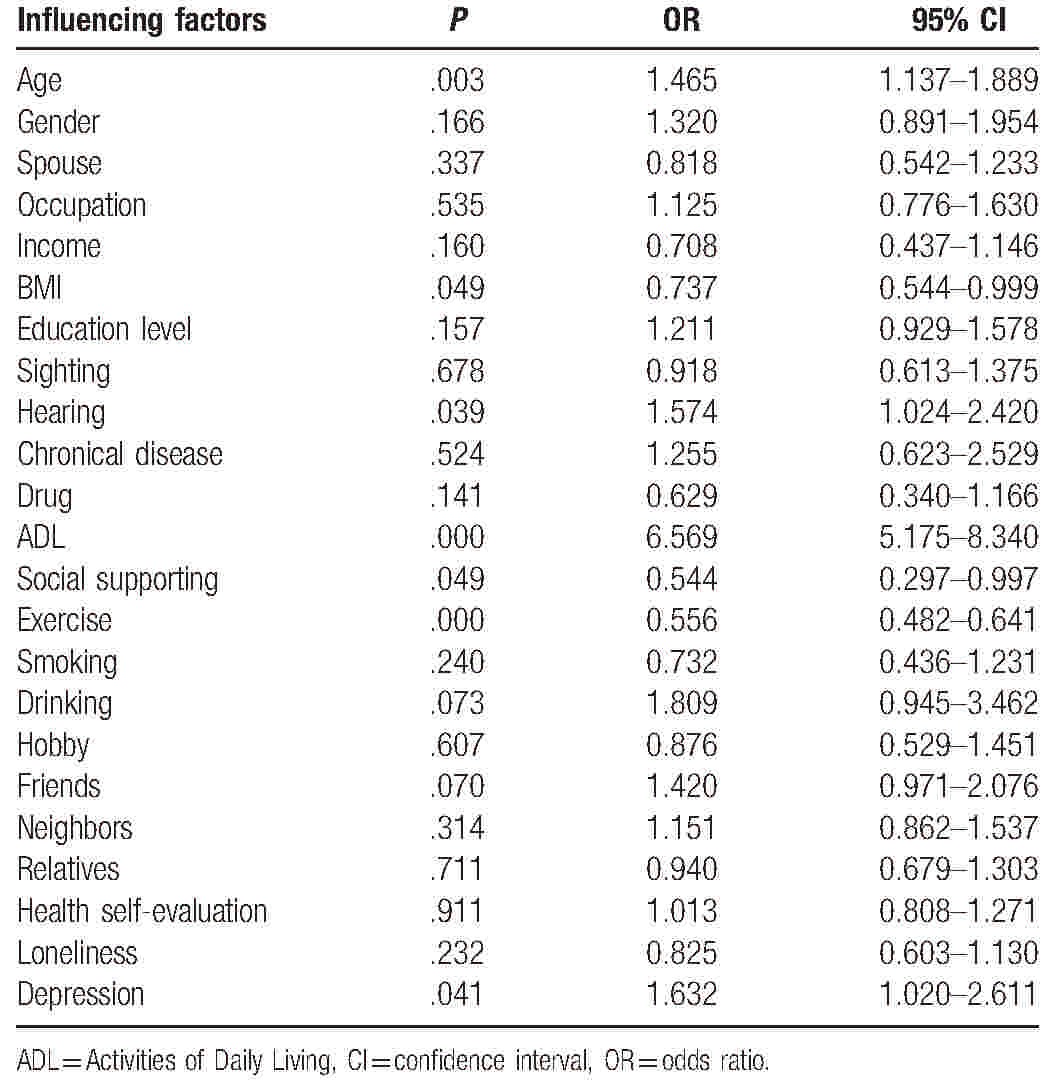
3.4. Logistic regression analysis of multiple factors influencing elderly homebound
The occurrence of homebound was taken as a dependent variable and those meaningful factors in the single factor analysis as the independent variables. Using the stepwise regression method, the multiple logistic regression analysis was performed, because the AIC value for this model is the smallest, which means the model is best fitted. Results proved that poor ADL, depressive symptoms, being old and hearing impairment are the risk factors for affecting the occurrence of community elderly homebound since the OR values for these variables are more than 1 while the BMI, low social support and lacking exercise are the protective factors since the OR values for these variables are less than 1 (Table 3).
Table 3.
Unconditional logistic regression analysis of factors influencing elderly homebound.
4. Discussion
The results of the study showed that the prevalence of Chinese community elderly homebound was 15.49%. In the United States, the results of a survey conducted in 2012[15] showed the prevalence of homebound elderly people to be 19.0%, while another survey conducted in 2015 showed that the prevalence rate was 5.9%.[6] The prevalence of urban homebound elderly people in Brazil was found to be 22.4%.[16] The prevalence in big cities of Japan is 14.4%.[17]
The results of the survey conducted in China and other countries, based on the same definition of homebound, on the prevalence of homebound urban community elderly people were different. The reasons could be first, the ages of selected study subjects were different; second, different sampling methods were used; third, regional differences, which meant the social environment, lifestyle, and economic levels of the Chinese elderly people were different from other countries, were found.
The results showed that the age of the elderly people affected the occurrence of homebound. With the increase in age, the prevalence of homebound increases gradually. Studies[18] have found that nearly 30% of the homebound people are aged ≥80 years. Physiological function and social activity ability weakened with the increase in age,[19,20] leading to a gradual increase in the occurrence of elderly homebound. Attention should be paid to the elderly, especially the health condition of the very old people.
The results of the study showed that the prevalence of homebound women was higher than men. Many overseas studies have found that the prevalence of homebound women is significantly higher than men. The reasons could be complex,[18,21] which may be due to diet habits, sexual hormone levels, work stress, and social pressure, and also due to the profound influence on their behaviors by the traditional role of a man and a woman in the family, that is, men are encouraged to work outside, while women are encouraged to work at home. Hence men preferred social activities outside the family, while women focused more on family and children and stayed at home.
The results of multifactor regression analysis showed that physical exercise is the main factor influencing homebound elderly people. Those elderly who exercised regularly had a low rate of morbidity among the homebound. Those elderly who exercise regularly tend to have a relatively correct health concept, pay attention to their physical condition, maintain a positive attitude and mindset every day, and have sufficient confidence in their life.[7] The results also showed that these elderly people had more friends and richer entertainment activities, hence these elderly would not stay at home every day.
The results showed that hearing impairment is also a main factor influencing the occurrence of homebound in elderly people. A number of elderly people choose to reduce their frequency of going out due to the impaired hearing, which seriously affects their communication with the outside world.[22] The results of multifactor regression analysis showed that the ADL is an independent risk factor that affected the occurrence of homebound, a higher score of ADL ability resulted in a lower prevalence of homebound, and 1 study also showed that ADL was an independent factor for the occurrence of homebound.[23] Studies[24] have showed that none of the elderly people who were able to take bus were homebound; 20.3% of the elderly people who can only walk 5 m were homebound; 75% of the elderly people who lost the ability to walk were homebound. A poor ADL ability of the elderly people makes their physical movement difficult, making it difficult to go out and hence more likely to result in homebound.
Results showed that social support affected the occurrence of homebound elderly people in Chinese community. A lower social support resulted in a higher prevalence of homebound. A number of overseas studies[25] have proven that elderly people with poor social support have a higher prevalence of homebound than those with strong social support. Social support can help the elderly people to cope with stress faced in daily living, alleviate the impact of negative events occurring in their lives, and protect their physical and mental health. Hence social support is an important factor that helps the elderly people in receiving treatment, overcoming disease, and maintaining a good psychological status, eventually improving their quality of life.[26] Social support to elderly people should be given attention, gradually complete the social support items, and reduce the prevalence of homebound.
The present study showed that those who often feel lonely scored their health condition to be poor and those who have depressive symptoms have a high rate of prevalence of homebound. The result of multifactor regression analysis showed that depression is a risk factor affecting the occurrence of homebound urban community elderly people in China. A number of overseas studies have also confirmed that depression leads to high prevalence of homebound elderly people. The incidence of depression in the homebound elderly people was higher than the nonhomebound elderly people.[27] With the presence of a depressive disorder, the elderly people are usually depressed, frustrated, low in emotion, self-abased, reluctant to communicate with people, with limited outdoor activities.[28] Studies have shown that[29] age is an important factor intensifying the feeling of loneliness in the elderly people. Older age leads to a stronger feeling of loneliness. A high self-rating on health can slow down the aging of physiology, while a poor subjective sense of health can worsen the self-maintenance ability. Hence the high incidence of homebound occurred among those who had a low self-rating of health.
5. Summary
The study used the multistage layered random cluster sampling method and investigated the current situation and factors influencing homebound elderly people in Chinese urban community. The results are as follows: The prevalence of homebound urban community elderly people in China is 15.49%. Poor ADL, depressive symptoms, hearing impairment, being old, no exercise, and low social support are the independent factors influencing the occurrence of homebound urban community Chinese elderly people.
The incidence of homebound urban community elderly people is relatively high in China and the factors influencing are complex. Hence attention should be paid to the problem of homebound elderly, conduct homebound-related health education events in the community, introduce elderly people, families, and the community medical staff to homebound-related knowledge and its harmful effects, and guide the elderly to maintain good living habits. The community should regularly organize activities that cater to elderly people, encourage the elderly people to walk out of their houses to join activities and do exercise, and also to interact with other people. Taking appropriate measures based on the specific influencing factor can effectively prevent the occurrence of homebound or becoming severe in elderly people, therefore effectively improving their quality of life and alleviate the endowment stress on their family and the society.
Acknowledgment
We would like to thank the staffs working in residents’ committee of Baoding and Bengbu cities.
Footnotes
Abbreviations: ADL =Activities of Daily Living, GDS-15 = Geriatric Depression Scale Short Form, SSRS = Social Support Rating Scale.
L-WJ and F-LW contributed equally to this work.
Author contributions: F-MX: study concept and design, revision of manuscript. L-WJ, F-LW, X-LZ and TY: acquisition of data, and preparation of manuscript. L-WJ: acquisition of data, analysis and interpretation of data, revision of manuscript.
Ethics approval and consent to participate: Informed consent was obtained from all enrolled subjects. The study was approved by the Ethics Committee of the Local Disease Control and Prevention Center (2013150101).
Funding: This study was supported by the National Social Science Foundation of China (2013BRK005).
The authors have no conflicts of interest to disclose.
References
- [1].China Information News, The National Bureau of Statistics of the People's Republic of China. The People's Republic of China National Economic and Social Development Statistical Bulletin in 2014. 2014. [Google Scholar]
- [2].Xie H, Wang Z, Hou X, et al. Present situation of pension service demand in our country and long-term care services strategy. Chin J Nurs 2012;9:14–6. [Google Scholar]
- [3].Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev 2012;33:137–52. [DOI] [PubMed] [Google Scholar]
- [4].Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc 2014;62:2243–51. [DOI] [PubMed] [Google Scholar]
- [5].Zeltzer BB, Kohn R. Mental health services for homebound elders from home health nursing agencies and home care agencies. Psychiatr Serv 2006;57:567–9. [DOI] [PubMed] [Google Scholar]
- [6].Musich S, Wang SS, Hawkins K, et al. Homebound older adults: prevalence, characteristics, health care utilization and quality of care. Geriatr Nurs 2015;36:445–50. [DOI] [PubMed] [Google Scholar]
- [7].Xing F, Yao S, Fan X, et al. Homebound status of older workers and influencing factors of the investigation and analysis. Chin J Gerontol 2008;28:796–9. [Google Scholar]
- [8].Gorstein J, Sullivan KM, Parvanta I, et al. Indicator and Methods for Cross-Sectional Surveys of Vitamin and Mineral Status of Populations. 2007;Ottawa: Micronutrient Initiative, Atlanta: Centers for Disease Control and Prevention. [Google Scholar]
- [9].Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86. [PubMed] [Google Scholar]
- [10].Xiao S. The theoretical foundation and applications of the social support rating scale. J Clin Psychiatry 1999;4:98–100. [Google Scholar]
- [11].Gallardo-Peralta LP, Sanchez-Moreno E, De Roda AB, et al. Ethnicity, social support, and depression among elderly Chilean people. J Psychol 2015;149:601–29. [DOI] [PubMed] [Google Scholar]
- [12].Albinski R, Kleszczewska-Albinska A, Bedynska S. [Geriatric Depression Scale (GDS). Validity and reliability of different versions of the scale—review]. Psychiatr Pol 2011;45:555–62. [PubMed] [Google Scholar]
- [13].Ishihara T, Terada S. [Geriatric Depression Scale (GDS)]. Nihon Rinsho 2011;69(suppl 8):455–8. [PubMed] [Google Scholar]
- [14].Herr M, Latouche A, Ankri J. Homebound status increases death risk within two years in the elderly: results from a national longitudinal survey. Arch Gerontol Geriatr 2013;56:258–64. [DOI] [PubMed] [Google Scholar]
- [15].Cohen-Mansfield J, Shmotkin D, Hazan H. Homebound older persons: prevalence, characteristics, and longitudinal predictors. Arch Gerontol Geriatr 2012;54:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ursine PG, Cordeiro Hde A, Moraes CL. Prevalence of homebound elderly people in the urban region of Belo Horizonte (Minas Gerais, Brazil). Cien Saude Colet 2011;16:2953–62. [DOI] [PubMed] [Google Scholar]
- [17].Umegaki H, Yanagawa M, Nakashima H, et al. The prevalence of homebound individuals in the elderly population: a survey in a city area in Japan. Nagoya J Med Sci 2015;77:439–46. [PMC free article] [PubMed] [Google Scholar]
- [18].Choi K, Park E, Lee IS. [Homebound status and related factors according to age in female elders in the community]. J Korean Acad Nurs 2012;42:291–301. [DOI] [PubMed] [Google Scholar]
- [19].Gilbert GH, Branch LG, Orav EJ. An operational definition of the homebound. Health Serv Res 1992;26:787–800. [PMC free article] [PubMed] [Google Scholar]
- [20].Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc 2010;58:2358–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Porter EJ, Lasiter S. Older homebound women's perceived risk of being unable to reach help quickly: influence of situations involving age-peers. Res Nurs Health 2012;35:624–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Imuta H, Yasumura S, Ahiko T, et al. [Predictors of functional status among independent and homebound community dwelling elderly: physical, psychological, and social parameters]. Nihon Koshu Eisei Zasshi 2002;49:483–96. [PubMed] [Google Scholar]
- [23].Yamagata E, Kimura M, Miyake M, et al. [Relationship between homebound status and physical fitness in the community-dwelling elderly population]. Nihon Koshu Eisei Zasshi 2014;61:671–8. [PubMed] [Google Scholar]
- [24].Qiu WQ, Dean M, Liu T, et al. Physical and mental health of homebound older adults: an overlooked population. J Am Geriatr Soc 2010;58:2423–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nour K, Laforest S, Gauvin L, et al. Behavior change following a self-management intervention for homebound older adults with arthritis: an experimental study. Int J Behav Nutr Phys Act 2006;3:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kim MT, Han HR, Shin HS, et al. Factors associated with depression experience of immigrant population: a study of Korean immigrants. Arch Psychiatr Nurs 2005;19:217–25. [DOI] [PubMed] [Google Scholar]
- [27].Gellis ZD. Assessment of a brief CES-D measure for depression in homebound medically ill older adults. J Gerontol Soc Work 2010;53:289–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Choi NG, McDougall GJ. Comparison of depressive symptoms between homebound older adults and ambulatory older adults. Aging Ment Health 2007;11:310–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Holmen K, Furukawa H. Loneliness, health and social network among elderly people—a follow-up study. Arch Gerontol Geriatr 2002;35:261–74. [DOI] [PubMed] [Google Scholar]


