Abstract
The aim of this study was to translate and cross-culturally adapt the swallowing quality-of-life questionnaire (SWAL-QOL) to Persian language and to determine validity and reliability of the Persian version of the swallow quality-of-life questionnaire (PSWAL-QOL) in the patients with oropharyngeal dysphagia.
The cross-sectional survey was designed to translate and cross-culturally adapt SWAL-QOL to Persian language following steps recommended in guideline. A total of 142 patients with dysphagia (mean age = 56.7 ± 12.22 years) were selected by non-probability consecutive sampling method to evaluate construct validity and internal consistency. Thirty patients with dysphagia were completed the PSWAL-QOL 2 weeks later for test–retest reliability.
The PSWAL-QOL was favorably accepted with no missing items. The floor effect was ranged 0% to 21% and ceiling effect was ranged 0% to 16%. The construct validity was established via exploratory factor analysis. Internal consistency was confirmed with Cronbach α >0.7 for all scales except eating duration (α = 0.68). The test–retest reliability was excellent with intraclass correlation coefficient (ICC) ≥0.75 for all scales.
The SWAL-QOL was cross-culturally adapted to Persian and demonstrated to be a valid and reliable self-report questionnaire to measure the impact of dysphagia on the quality-of-life in the Persian patients with oropharyngeal dysphagia.
Keywords: deglutition, deglutition disorders, dysphagia, quality-of-life, reliability, validity
1. Introduction
Normal swallowing is the complex cognitive, sensory motor act of moving bolus from the mouth to the stomach.[1] Dysphagia is a disturbance of the complex sensorimotor functions of swallowing.[2] Dysphagia caused by various diseases such as stroke, multiple sclerosis, Parkinson disease, head and neck cancer, dementia. Pneumonia, malnutrition, dehydration, and even death are complications of dysphagia.[3] Swallowing problems can be associated with psychosocial consequences such as anxiety, depression, shame, and fear. So, dysphagia have a negative impact on quality of life.[4,5]
Evaluation of dysphagia and its severity is performed using bedside clinical tests, videofluoroscopy (VFS) and flexible endoscopic evaluation of swallowing (FEES). The results of these examinations help to identify mechanical and physiological dysfunctions of swallowing.[4–6] The evaluation process should combined with a patient reported instrument for accurately measuring the impact of dysphagia on the various dimensions of quality of life (QOL).[6,7] There are various instruments that have been used to assess health related QOL in different patients with dysphagia. Most of them are related to general health issues without subsets of questions that specifically address dysphagia. Only a few instruments have been designed and validated to specifically address swallowing complaints and the effects of dysphagia on QOL.[8–11] The swallowing quality of life questionnaire (SWAL-QOL) as the first self report instrument specific to dysphagia was developed by McHorney et al[12–14] SWAL-QOL is a patient based questionnaire for assessing the impact of swallowing problems on QOL in patients with dysphagia caused by different diseases.[14–16] The original version of SWAL-QOL has shown good psychometric qualities.[14] It is widely used as a gold standard in dysphagia research and clinical situations.[17–19]
An instrument can be appropriate for use in international studies, if it was linguistically validated on translation and cross-cultural adaptation. The cross-cultural adaption and validation of SWAL-QOL has been confirmed in different languages such as Dutch,[20] French,[10] Chinese,[21] Swedish,[6] but to date there has not been the Persian version of it. Persian-speaking countries have great need for reliable and valid instruments such as SWAL-QOL questionnaire that provide patient perspective referring to swallowing problems. The purpose of this study was to cross-cultural adaption of the PSWAL-QOL and to determine its reliability and validity in patients with oropharyngeal dysphagia.
2. Materials and methods
This was a cross-sectional study. The protocol of this study was approved by the review board, MS Research Center, Tehran University of Medical Sciences (TUMS) and the Ethical Committee of TUMS. Written informed consent was obtained from all the patients for taking part in the study.
2.1. Participants
Patients were recruited based on non-probability consecutive sampling from outpatient neurology, cancer, speech, and swallowing clinics of Tehran University of Medical Sciences hospitals in Tehran, Iran. The inclusion criteria included: (1) oropharyngeal dysphagia diagnosed by a speech-language pathologist (SLP) using a clinical examination, (2) a stable dysphagia condition according to the patient and the SLP. The exclusion criteria included: (1) inability to provide informed consent, (2) inability to read and write Persian, (3) evidence of symptoms of esophageal dysphagia, and (4) evidence of cognitive disorders such as dementia in medical history. According to these criteria, a total of 142 patients were included in the study and completed the PSWAL-QOL to determine psychometrical properties. To measure test–retest reliability, 30 of the 142 patients completed the Persian version of SWAL-QOL again with an interval of 2 weeks.
2.2. Instrument
The SWAL-QOL is a 44-item quality-of-life questionnaire specific to dysphagia across 10 quality of life domains and an additional section on symptom frequency. The 10 domains are burden, eating duration, eating desire, food selection, communication, fear, mental health, social role, fatigue, and sleep. The symptom scale comprises 14 dysphagia symptoms including coughing, choking, gagging, and drooling. Each domain has at least 2 items in the form of a 5-point Likert scale. All scales are converted to a 0 to 100 metric, where a score of “0” represents the worst score and “100” the most optimal score. The psychometric properties of the SWAL-QOL have been found to be satisfactory.[12–14]
2.3. Translation and cross-cultural adaption procedure
The original version of the SWAL-QOL questionnaire was translated and cross-culturally adapted to Persian according to 5 steps described in guideline.[22] Step 1: Two Iranian translators, who were fluent in English, forward translated the original version of the SWAL-QOL questionnaire into Persian. Step 2: Two SLP who were involved in the study together with 2 translators discussed the translations to achieve a synthesized Persian SWAL-QOL. Step 3: A bilingual translator, whose mother tongue was English, back translated the synthesized Persian SWAL-QOL to English to highlight conceptual errors in the translations. Step 4: The expert panel (2 SLP, 1 methodologist, 1 neurologist) along with 3 translators reviewed all documents in terms of semantic, experiential, and conceptual equivalence. They reached a consensus about equivalence between original SWAL-QOL and Persian version of SWAL-QOL and pre-final PSWAL-QOL was approved. Step 5: A pilot study was conducted using 30 patients (age ranged from 30 to 85 years) with dysphagia to evaluate face and content validity. The patients understood each questionnaire items without any difficulty. This demonstrated the PSWAL-QOL items were clear, understandable, and relevant and consequently, the Persian version of the SWAL-QOL questionnaire was established.
2.4. Statistical analysis
Descriptive statistics was applied to assess the missing data, distribution of scores, floor effect, and ceiling effect. Floor and ceiling effects were considered to be present if more than 15% of the participants achieved the highest or lowest score, respectively.[14]
Construct validity was assessed by exploratory factor analysis (EFA). The Bartlett test of sphericity was used to assess whether the correlation matrix of sample was single identity and whether satisfactory factor analysis of the data could proceed. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was performed to determine whether the sample size was adequate to proceed factor analysis. The KMO >0.50 indicating the sample size is adequate.[23] The principal components analysis (PCA) as a factor extraction method was used to determine the construct of the PSWAL-QOL. Factors were extracted using varimax and promax methods. Decision about the number of prominent factors was taken based on the eigenvalue >1 and the scree plot methods.[23]
Internal consistency reliability of scales was analyzed by Cronbach α coefficient, which was considered statistically significant when between 0.70 and 0.95. The testretest reliability was evaluated using Pearson correlation coefficient and intraclass correlation coefficient (ICC). The ICC ≥0.75 was considered as excellent reliability.[24] Statistical analyses were performed using the SPSS 19.0 statistical software (SPSS, Inc., Chicago, IL). P values <.05 were considered to be statistically significant.
3. Results
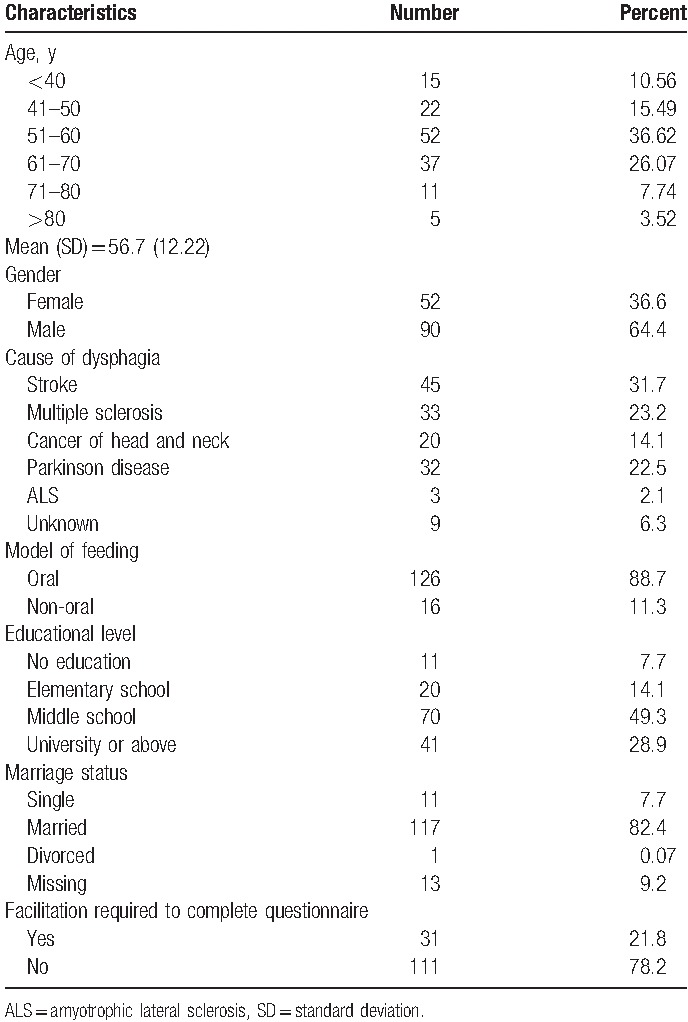
A total of 142 patients with oropharyngeal dysphagia were included to this study. Mean age of the patients was 56.7 years (range 35–85) and 64.4% of them were men. The 31/7% of participants (n = 45) had dysphagia post stroke and 2/1% of them (n = 3) had dysphagia due to amyotrophic lateral sclerosis. Most of the patients (88.7%) had oral feeding and 11.3% of them depend on tube-feeding. The patients’ characteristics are summarized in Table 1. The patients responded to all items of PSWAL-QOL questionnaire without any difficulties (response rate 100%). Translation of the questionnaire proceeded successfully and the backward translation was corresponded to the original version.
Table 1.
Demographic characteristics (n = 142).
3.1. Features of score distribution
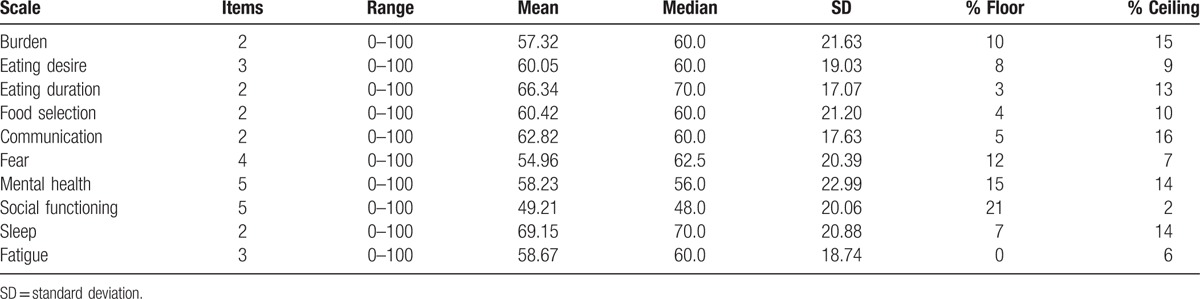
The features of the score distribution of the PSWAL-QOL scales obtained from 142 patients are given in Table 2. The full range of the 0 to 100 score distribution was observed for all scales. The mean score of all the scales ranged from 54.96 to 69.15. There were no missing data for individual items. The floor effects ranged from 0% (fatigue) to 21% (social functioning), and the ceiling effects ranged from 2% (social functioning) to 16% (communication).
Table 2.
Features of score distribution (n = 142).
3.2. Construct validity
Exploratory factor analysis was performed to explore the factor structure of the PSWAL-QOL. The result of Bartlett test of sphericity was significant (chi-square = 476.844, df = 45, P < .001) indicating that the correlation matrix was not a single identity. The result of the KMO measure was 0.837, which indicated that the sample size was sufficient to factor analysis. Principle component analysis gave 2 latent factors with eigenvalue greater than 1.00. The extraction of 2 factors was performed using varimax and promax rotations. The eigenvalue of the first factor was 6.49 (64.98% of total variance) and the eigenvalue of the second factor was 1.32 (13.23% of total variance). Furthermore, the scree plot curve confirmed that 2 factors could be extracted (Fig. 1).
Figure 1.
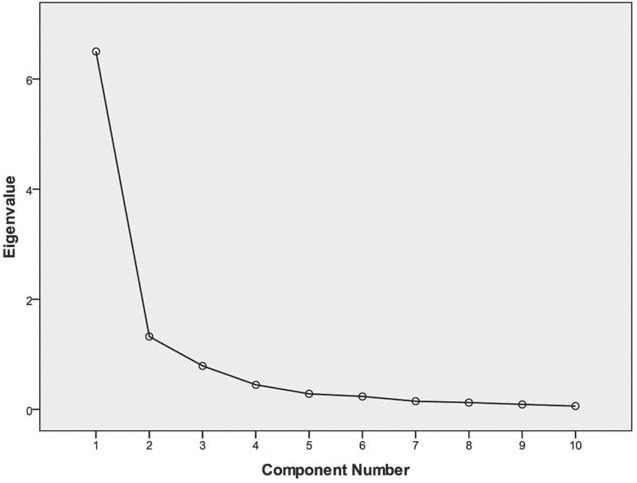
Scree plot of 44-item PSWAL-QOL. Two factors with eigenvalues greater than 1 are given. PSWAL-QOL = Persian version of the swallow quality-of-life questionnaire.
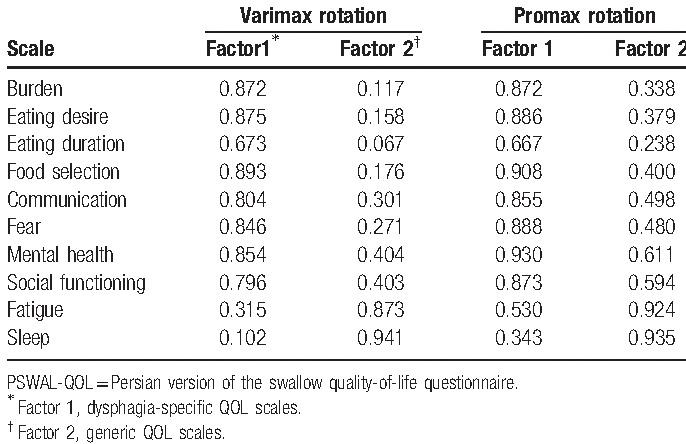
As shown in Table 3, 8 scales (burden, eating desire, eating duration, food selection, communication, fear, mental health, and social functioning) were loading on factor 1. The first factor was named “dysphagia-specific.” All scales except communication, social functioning, and eating duration were contributed equally to this factor. Two scales (sleep and fatigue) were loaded on factor 2. The second factor was named “generic,” which was not specific to dysphagia. Sleep (factor loading = 0.941) was the primary contributor to generic factor.
Table 3.
Factor loading of the PSWAL-QOL scales.
3.3. Reliability
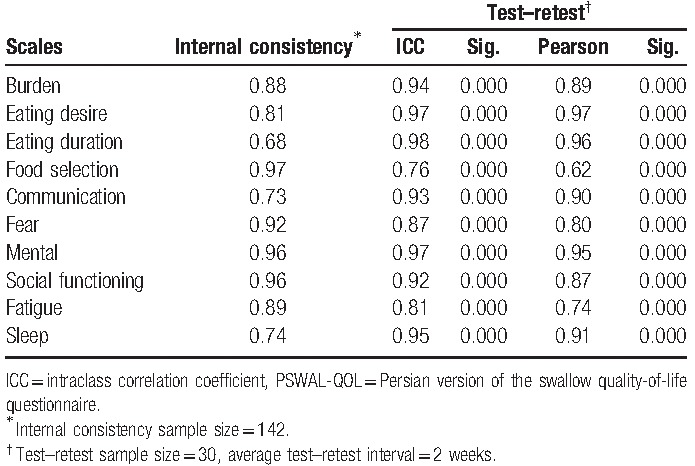
According to Table 4, all the scales except eating duration (α = 0.68) attained the reliability standard of 0.70 for group-level research. Cronbach α coefficients were ranged from 0.73 to 0.97 for the other 9 scales. The acceptable internal consistency indicated the homogeneity of the items in each of the 9 scales measuring the same construct. In the 2-week retest reliability, Pearson correlations ranged from 0.62 to 0.97 (P < .001) and ICC ranged from 0.76 to 0.98. Therefore, the PSWAL-QOL had excellent short-term stability.
Table 4.
Reliability of PSWAL-QOL.
4. Discussion
One of the main components of a comprehensive evaluation process of dysphagia is self-report instruments to represent the patient's perspective.[9,14] SWAL-QOL is a self-report questionnaire for evaluating the impact of swallowing problems on QOL.[6,14] The original version of SWAL-QOL has been translated to different languages and frequently used as a gold standard in dysphagia researches regarding QOL issues.[6,10,20,21] Therefore, in this study we made a cross-cultural adaption and investigation of the psychometrics properties of the PSWAL-QOL in the patients with oropharyngeal dysphagia.
The translation and cultural adaption of the SWAL-QOL to Persian language was performed without noticeable difficulties, and no changes were made in the translations. All the patients favorably accepted and understood questionnaire and scored all items of the PSWAL-QOL without missing responses, indicating its acceptability and feasibility. This is in agreement with the original and Swedish version studies.[6,14]
The full range of scores was observed, and the floor and ceiling effects were acceptable. These results were in agreement with results from the original and Swedish version of the SWAL-QOL.[6,14] The floor effects were more than 15% only for social functioning scale. These findings reflect that swallowing problems have serious impacts on the social functioning of the patients and can change the usual activities of social life of them. Responding to all items together with the well distribution of the scores, and acceptable floor or ceiling effects indicate the content validity of the Persian SWAL-QOL.
The exploratory factor analysis was performed to identify the underlying structure of the PSWAL-QOL. The factor analysis discovered 2 distinctive factors. The dysphagia-specific QOL factor was composed of burden, eating desire, eating duration, food selection, communication, fear, mental health, and social functioning scales. The generic QOL factor was composed of sleep and fatigue scales. These findings were in agreement with the results of the original and the Chinese versions of the SWAL-QOL studies.[14,21] This finding provides evidence for construct validity of the PSWAL-QOL.
The internal consistency reliability was evaluated. Nine scale scores of the PSWAL-QOL (burden, eating desire, food selection, communication, fear, mental health, social functioning, sleep, fatigue) except eating duration achieved an internal consistency with Cronbach α >0.7. It means that the items in each of those 9 scales are homogenous and examine various aspects of the same characteristics. These results were in agreement with the findings of the original[14] and Swedish versions[6] of SWAL-QOL. In line with Finizia et al[6] the internal consistency of the eating duration scale was lower than the standard cutoff. Since the number of items controls Cronbach α value, and eating duration scale consist of just 2 items therefore, each of the items could decrease the Cronbach α of eating duration scale.
Two-week retest reliability was confirmed by Pearson correlation coefficient and Intraclass correlation coefficient (ICC). The excellent test–retest reliability represented the stability of the PSWAL-QOL over time and consistency of the scores between 2 measurements. These findings were in line with the results of the original,[14] Swedish,[6] and Chinese[21] versions of SWAL-QOL.
The present study has some limitations. Convergent and divergent construct validity of the PSWAL-QOL was not determined due to time limitation and lack of convenient place for patients to complete other standard measures adapted into Persian language. However, the data on convergent validity for SWAL-QOL are available from the original,[14] Swedish,[6] and Chinese[21] versions. Future study is warranted to investigate convergent and divergent construct validity of the PSWAL-QOL.
5. Conclusions
The present study demonstrated that PSWAL-QOL questionnaire is a reliable and valid instrument to measure the impact of swallowing problems on quality of life in patients with oropharyngeal dysphagia. Therefore, PSWAL-QOL can be applied as a useful self-report questionnaire in the clinical settings and for research purposes in Persian-speaking population.
Footnotes
Abbreviations: EFA = exploratory factor analysis, FEES = flexible endoscopic evaluation of swallowing, ICC = intraclass correlation coefficient, KMO = Kaiser–Meyer–Olkin, PCA = principal components analysis, PSWAL-QOL = Persian version of the swallow quality-of-life questionnaire, QOL = quality of life, SLP = speech-language pathologist, SWAL-QOL = swallowing quality-of-life questionnaire, TUMS = Tehran University of Medical Sciences, VFS = videofluoroscopy.
This study was supported by MS Research Center, Neuroscience Institute of Tehran University of Medical Sciences.
The authors had no conflicts of interest to declare in relation to this article.
References
- [1].Miller AJ. Neurophysiological basis of swallowing. Dysphagia 1986;1:91–100. [Google Scholar]
- [2].Prosiegel M, Schelling A, Wagner-Sonntag E. Dysphagia and multiple sclerosis. Int MS J 2004;11:22–31. [PubMed] [Google Scholar]
- [3].Roden DF, Altman KW. Causes of dysphagia among different age groups: A systematic review of the Literature. Otolaryngol Clin N Am 2013;46:965–87. [DOI] [PubMed] [Google Scholar]
- [4].Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of lif—–a population-based study. Aliment Pharmacol Ther 2008;27:971–9. [DOI] [PubMed] [Google Scholar]
- [5].Jansson C, Wallander MA, Johansson S, et al. Stressful psychosocial factors and symptoms of gastroesophageal reflux disease: a population-based study in Norway. Scand J Gastroenterol 2010;45:21–9. [DOI] [PubMed] [Google Scholar]
- [6].Finizia C, Rudburg I, Bergqvist H, et al. A Cross-sectional Validation Study of the Swedish Version of SWAL-QOL. Dysphagia 2012;27:325–35. [DOI] [PubMed] [Google Scholar]
- [7].FDA. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 2008;117:919–24. [DOI] [PubMed] [Google Scholar]
- [9].Chen AY, Frankowski R, Bishop-Leone J, et al. The development and validation of a dysphagia specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg 2001;127:870–6. [PubMed] [Google Scholar]
- [10].Khaldoun E, Woisard V, Verin E. Validation in French of the SWAL-QOL scale in patients with oropharyngeal dysphagia. Gastroenterol Clin Biol 2009;33:167–71. [DOI] [PubMed] [Google Scholar]
- [11].Woisard V, Andrieux MP, Puech M. Validation of a selfassessment questionnaire for swallowing disorders (Deglutition Handicap Index). Rev Laryngol Otol Rhinol (Bord) 2006;127:315–25. [PubMed] [Google Scholar]
- [12].McHorney CA, Bricker DE, Kramer AE, et al. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: I. Conceptual foundation and item development. Dysphagia 2000;15:115–21. [DOI] [PubMed] [Google Scholar]
- [13].McHorney CA, Bricker DE, Robbins J, et al. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: II. Item reduction and preliminary scaling. Dysphagia 2000;15:122–33. [DOI] [PubMed] [Google Scholar]
- [14].McHorney CA, Robbins J, Lomax K, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 2002;17:97–114. [DOI] [PubMed] [Google Scholar]
- [15].Leow LP, Huckabee ML, Anderson T, et al. The impact of dysphagia on quality of life in ageing and Parkinson's disease as measured by the Swallowing Quality of Life (SWAL-QOL) Questionnaire. Dysphagia 2010;25:216–20. [DOI] [PubMed] [Google Scholar]
- [16].Rinkel RN, Verdonck-de Leeuw IM, Langendijk JA, et al. The psychometric and clinical validity of the SWAL-QOL questionnaire in evaluating swallowing problems experienced by patients with oral and oropharyngeal cancer. Oral Oncol 2009;45:e67–71. [DOI] [PubMed] [Google Scholar]
- [17].Lovell SJ, Wong HB, Loh KS, et al. Impact of dysphagia on quality-of-life in nasopharyngeal carcinoma. Head Neck 2005;27:864–72. [DOI] [PubMed] [Google Scholar]
- [18].Costa Bandeira AK, Azevedo EH, Vartanian JG, et al. Quality of life related to swallowing after tongue cancer treatment. Dysphagia 2008;23:183–92. [DOI] [PubMed] [Google Scholar]
- [19].Roe JW, Leslie P, Drinnan MJ. Oropharyngeal dysphagia: the experience of patients with non-head and neck cancers receiving specialist palliative care. Palliat Med 2007;21:567–74. [DOI] [PubMed] [Google Scholar]
- [20].Bogaardt HC, Speyer R, Baijens LW, et al. Cross-cultural adaptation and validation of the Dutch version of SWAL-QoL. Dysphagia 2009;24:66–70. [DOI] [PubMed] [Google Scholar]
- [21].Lam PM, Lai CK. The validation of the Chinese version of the Swallow Quality-of-Life questionnaire (SWAL-QOL) using exploratory and confirmatory factor analysis. Dysphagia 2011;26:117–24. [DOI] [PubMed] [Google Scholar]
- [22].Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000;25:3186–91. [DOI] [PubMed] [Google Scholar]
- [23].Dennis C. The Essentials of Factor Analysis. 3rd ed.London: Continuum; 2006. [Google Scholar]
- [24].Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. [DOI] [PubMed] [Google Scholar]


