Abstract
Background & aims:
Nutritional interventions for malnutrition in cancer patients can be helpful. However, concise intervention recommendations remain controversial. Thus, the aim of this study was to report on a nutrition intervention conducted by a multidisciplinary team of specialist nurses and to explore the effect of nutritional intervention on cancer patients.
Methods:
This prospective clinical trial study enrolled 110 colorectal cancer patients undergoing chemotherapy. The patients were evaluated upon admission using the 2002 Nutritional Risk Screening system (NRS-2002). The patients were randomly divided into intervention and control groups including 55 patients each. Patients in the control group were administered a normal diet, while those in the intervention group received individual recipes developed by a team of professional nurses, clinical doctors, dietitian, family caregivers, and the patients themselves. Patient weight and serum albumin and prealbumin levels were compared between the 2 groups at different time points.
Results:
There was a significant difference in patient weight and serum albumin and prealbumin levels before and after nutrition intervention in the intervention group (P < .05). In the control group, weight did not change during ordinary diet guidance. Serum albumin level was slightly improved after 12 cycles of chemotherapy, similar to the prealbumin results. There were statistically significant differences in serum albumin and prealbumin levels between the intervention and control groups after nutrition intervention (P < .05). However, there was no statistically significant difference in weight between the groups after nutrition intervention (P > .05).
Conclusion:
A multidisciplinary team approach for nutrition intervention conducted by specialist nurses improved prealbumin levels in colorectal cancer patients undergoing chemotherapy, with no weight change.
Keywords: cancer, chemotherapy, multidisciplinary teamwork, nutrition intervention, specialist nurse
1. Introduction
Cancer is a leading cause of morbidity and mortality worldwide, with the number of new cases expected to rise significantly over the next decades. In China, 310 million people have been diagnosed with cancer.[1] Cancer patients are at risk of malnutrition, not only due to the physical and metabolic effects of the disease but also due to the effects of anticancer therapies, and malnutrition is associated with poorer prognosis.[2–5] Additionally, malnutrition has a negative effect on clinical outcome. These effects may be driven by inadequate food intake, decreased physical activity, and catabolic metabolic derangement.[6] Therefore, it is important to improve nutritional status in order to enhance immunity status and chemotherapy tolerance in cancer patients.
However, concise intervention recommendations remain under heated debate. The European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines recommend regular screening of all cancer patients for the risk or presence of malnutrition. Weight loss and nutrition screening tools such as the 2002 Nutrition Risk Screening system (NRS-2002) could be used for nutrition screening.[6] The Chinese version of NRS-2002 has been shown to function well in Chinese hospitalized patients.[7] However, the methods and efficacy of this strategy requires improvement. Our clinical oncology center has developed a multidisciplinary team of specialist nurses for patient nutritional interventions. This strategy has been widely accepted by cancer patients and shows promising effects on nutritional status improvement in our center. Thus, we conducted a clinical trial to systematically investigate this strategy.
This prospective study investigated the effect on patient weight and serum albumin and prealbumin levels of this multidisciplinary team approach for nutritional interventions in colorectal cancer patients undergoing chemotherapy.
2. Methods
2.1. Participants
We performed a prospective, observational study to evaluate consecutive adult patients with colorectal cancer undergoing chemotherapy in the general ward of the Department of Medical Oncology of the Third Affiliated Hospital of Sun Yat-Sen University between January 1, 2014, and June 31, 2015. A total of 110 participants voluntarily joined the study and provided written informed consent. This study used the NRS-2002[8] to evaluate the nutritional status of patients upon their admission. Several results of clinical studies of NRS-2002 showed that nutritional support was invalid for NRS scores less than 3. Thus, patients with NRS scores of 3 points or less were excluded.
The inclusion criteria included conscious patients 18 years or older who had pathologically diagnosed cancer and were undergoing chemotherapy, with NRS-2002 scores greater than or equal to 3 points. Patients who were rejected participation in the study included those meeting the exclusion criteria, including those unable to eat normally, with severe organ failure, with a diagnosis of another cancer, with apparent infection or fever, and those with pulmonary tuberculosis or peptic ulcer.
2.2. Nutrition interventions
The patients were randomly divided into intervention and control groups of 55 patients each. Patients in the control group received nutrition screening, nutritional guidance, diet mission, and arranged meal times. Furthermore, nurses provided individual nutrition education, encouraged patients to eat more, and administered nutrition treatments according to patient biochemical indicators. Patients in the intervention group received individual recipes developed by a team including specialist nurses, clinical doctors, dietitian, family caregivers, and patients themselves. Two specialist nurses with 5 years of experience assessed in patient nutritional status within 48 hours according to NRS-2002. A dietitian calculated the patients’ total energy requirement according to the formula[9]: (total energy demand = base energy expenditure [BEE] × activity coefficient × stress coefficient × temperature coefficient; BEE: male weight (kg) ×24, female weight (kg) ×22.8; activity coefficients: bedridden (1.2), bed activities (1.25), normal light activity (1.3); stress coefficients: no postoperative complications (1.0–1.05), cancer (1.1–1.45), peritonitis (1.05–1.25), serious infection or multiple trauma (1.3–1.55); temperature coefficients: normal temperature (1.0), 10% increase for every degree Celsius rise in consumption). The dietitian informed the doctors and professional nurses of this result. Afterward, doctors administered parenteral or enteral nutrition at 70% to 80% of the total energy supply in order to avoid refeeding syndrome. After a full assessment of the patients’ custom, diet nutrition, chemotherapy, gastrointestinal reaction duration, and changes in serum prealbumin levels, the patients and family care takers received individual nutrition education from the professional nurses. The patient diets were continually adjusted according to their nutritional status. The specific contents are shown in Table 1.
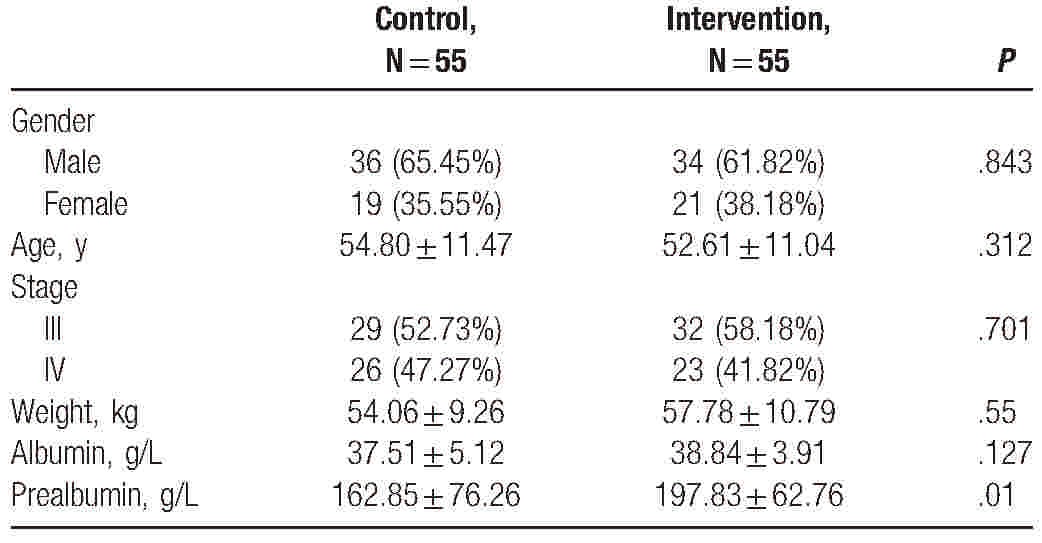
Table 1.
Baseline demographic and clinical characteristics of patients.
2.3. Data collection
The nutritional risks of all hospitalized cancer patients were evaluated on the day of admission by the 2 professional nurses using NRS-2002, which includes the following contents: nutritional status, body weight changes in the past 1 to 3 months, and variations in food intake in the past week; disease severity; and age ≥70 years. Total scores ≥3 indicated nutritional risk.[8] The weight of every participant was measured weekly by the same person. The serum albumin and prealbumin levels were evaluated monthly along with another clinical assessment. The basic data of all patients were obtained from the hospital information system (HIS).
2.4. Endpoints and statistical analysis
Patient weight and serum albumin and prealbumin levels were the main endpoints. We compared variables in different groups by Chi-square analysis. The criterion for statistical significance was set at an α of 0.05 and all P values were based on 2-sided tests. IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY) was used for all statistical analyses.
3. Results
3.1. Patient characteristics
All 110 patients included in this study were ethnic Chinese. Of these, 61.82% and 65.45% of patients in the control and intervention groups male. The ages were similar, with medians of 52.61 and 54.80 years in the control and intervention groups, respectively. Patient weight (57.78 vs 54.06 kg) and serum albumin levels (38.84 g/L vs 37.51 g/L) were also similar between groups. However, the serum prealbumin level in the control group was higher than that in the intervention group (197.83 g/L vs 162.85 g/L, P = .01) (Table 2).
Table 2.
Comparison of end points with baseline level in intervention group (n = 55) after 6 and 12 cycle of chemotherapy.
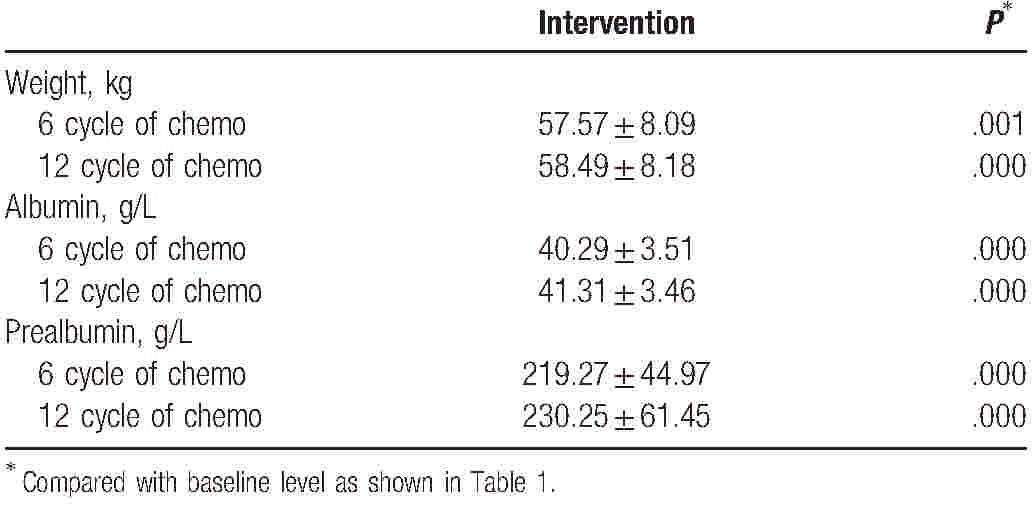
3.2. Improved nutritional status in the intervention group
There was a statistically significant difference before and after nutritional intervention in patient weight and serum albumin and prealbumin levels in the intervention group (P < .05). The improvement first occurred after 6 cycles of chemotherapy and was maintained after 12 cycles (Table 3).
Table 3.
Comparison of end points with baseline level in control group (n = 55) after 6 and 12 cycle of chemotherapy.
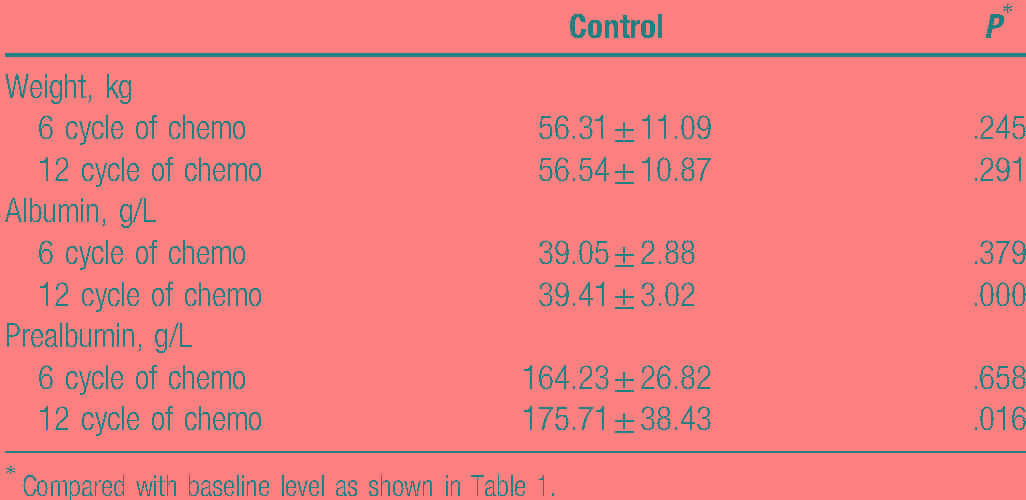
3.3. Improved nutritional status in the control group
Patient weight did not change significantly during ordinary diet guidance in the control group. Serum albumin level improved slightly after 12 cycles of chemotherapy, with similar results observed for prealbumin levels (Table 4).
Table 4.
The efficacy of intervention on nutrition status compared with control group.
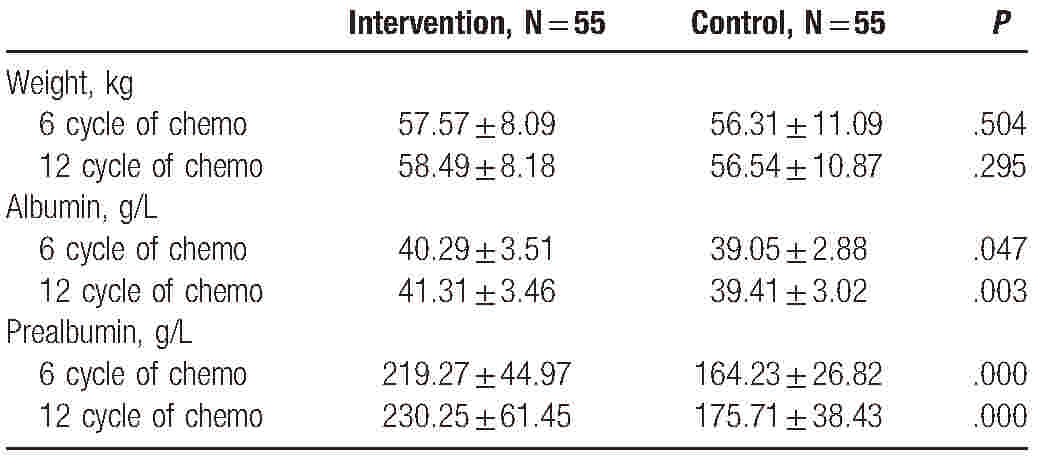
3.4. The efficacy of intervention on nutritional status compared to the control group
The differences in serum albumin and prealbumin levels between the intervention and control groups after nutritional intervention were statistically significant (P < .05). However, the weight difference between the 2 groups was not statistically significant after nutritional intervention (P > .05).
4. Discussion
Weight loss is common in patients with progressive cancer and has a major impact on both morbidity and mortality.[10] In addition, malnutrition is a common complication in patients undergoing chemotherapy, radiation, or surgery for cancer.[2,6] This common problem in cancer patients has been recognized as a significant contributor to morbidity and mortality in cancer.[5] Malnutrition is associated with a decreased quality of life in cancer patients, and significant weight loss is a biomarker of poor prognosis in these patients.[5] Nutritional interventions can help cancer patients to maintain body weight and nutritional stores, offering relief from symptoms and improved quality of life.[11] Several clinical studies have shown that patients receiving nutritional intervention survive longer.[12,13] Poor nutritional practices, which can lead to under-nutrition, can contribute to the incidence and severity of treatment side effects and increase the risk of infection and mortality in cancer patients.[2] Advanced colorectal cancer patients, especially those with malnutrition, experience poor general health and cannot adapt to project implementation. Therefore, it is important to accurately and early identify nutritional risk in patients.
In this study, a multidisciplinary team approach for nutritional interventions conducted by specialist nurses improved prealbumin levels in colorectal cancer patients undergoing chemotherapy, with no weight change. Moreover, 12 of 55 patients in the intervention group received nutritional intervention 1 week before chemotherapy. No treatment was interrupted by nutrition-related complications. Among the 55 cases in the intervention group, no patient required force-feeding. However, treatment in eight cases in the control group was interrupted by nutrition-related complications, including 5 cases of force-fed syndrome. A previous study[14] conducted a similar “individualized nutrition intervention,” in cancer patients undergoing radiotherapy. They found that the intervention decreased nutritional deterioration, similar to our results. These findings revealed that nutrition interventions should be based on the combination of specialist nurses and the full patient cooperation.[15]
Patient weight[13] and serum albumin and prealbumin levels[6,9,16] reflect the nutritional status of cancer patients and have been identified as critical prognostic factors for multiple cancers. Serum albumin and prealbumin levels increase immediately with improved nutritional status. The ESPEN guidelines recommend that weight, serum albumin level, and body mass index (BMI) could be used for nutritional screening.[6] In this study, the serum albumin and prealbumin levels in the intervention group were statistically significantly different from those in the control group. These 2 indicators immediately increase with improved nutritional status. However, weight was not easy to improve.
A multidisciplinary team[17] dominated by professional nurses could effectively improve nutrition in patients with advanced cancer. In this study, the multidisciplinary team included a dietitian, clinic doctor, professional nurse, family caretaker, and the patients themselves. The professional nurse screened and identified early malnutrition in the cancer patients.[8] Clinic doctors should balance malnutrition and anticancer therapy in order to avoid the further aggravation of malnutrition by complications. Additionally, a specialist dietitian should be part of the multidisciplinary team for cancer patients throughout the continuum of care, as frequent dietetic contact has been shown to enhance outcomes.
This study has several limitations. First, patients were aware of the study and would discuss their anticancer experiences with one other, so some nutritional interventions administered to the intervention group may have been imitated by the patients in other groups. Second, the sample size was limited. Third, all patients were from a single center; multicenter-based studies are needed to prove the efficacy of this strategy. Finally, it is necessary to collect data and continue follow-ups to explore the relationship between nutrition and patient survival.
In conclusion, a multidisciplinary team approach for nutritional interventions conducted by specialist nurses improved prealbumin levels in colorectal cancer patients undergoing chemotherapy with weight changes. Therefore, such multidisciplinary teams could provide the appropriate nutritional support essential for chemotherapy.
Footnotes
Abbreviations: BEE = base energy expenditure, ESPEN = European Society for Clinical Nutrition and Metabolism, NRS-2002 = 2002 Nutrition Risk Screening system.
J-XL, X-WC, and Z-HC contributed equally to this work.
Funding: This study was supported by the National Natural Science Foundation (31600710 and 81372374), Natural Science Foundation of Guangdong (No. 2014A030313146 and 2016A030313302), Scientific research project of Guangzhou Municipal University (1201630019), and Research project of Guangzhou Medical University (2016A09) and Guangzhou Science and Technology Plan (2015Y2000007).
The authors have no conflicts of interest to disclose.
References
- [1].Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115–32. [DOI] [PubMed] [Google Scholar]
- [2].Aapro M, Arends J, Bozzetti F, et al. Early recognition of malnutrition and cachexia in the cancer patient: a position paper of a European School of Oncology Task Force. Ann Oncol 2014;25:1492–9. [DOI] [PubMed] [Google Scholar]
- [3].Bilici A, Sonkaya A, Ercan S, et al. The changing of serum vitamin B12 and homocysteine levels after gastrectomy in patients with gastric cancer: do they associate with clinicopathological factors? Tumour Biol 2015;36:823–8. [DOI] [PubMed] [Google Scholar]
- [4].Liu Z, Sun Y, Tan S, et al. Nutrient deprivation-related OXPHOS/glycolysis interconversion via HIF-1alpha/C-MYC pathway in U251 cells. Tumour Biol 2016;37:6661–71. [DOI] [PubMed] [Google Scholar]
- [5].Nsengimana J, Laye J, Filia A, et al. Independent replication of a melanoma subtype gene signature and evaluation of its prognostic value and biological correlates in a population cohort. Oncotarget 2015;6:11683–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr 2017;36:11–48. [DOI] [PubMed] [Google Scholar]
- [7].Liu P, Zhang ZF, Cai JJ, et al. NRS2002 assesses nutritional status of leukemia patients undergoing hematopoietic stem cell transplantation. Chin J Cancer Res 2012;24:299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Davies M. Nutritional screening and assessment in cancer-associated malnutrition. Eur J Oncol Nurs 2005;9(suppl 2):S64–73. [DOI] [PubMed] [Google Scholar]
- [9].Han WX, Chen ZM, Wei ZJ, et al. Preoperative pre-albumin predicts prognosis of patients after gastrectomy for adenocarcinoma of esophagogastric junction. World J Surg Oncol 2016;14:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Balstad TR, Solheim TS, Strasser F, et al. Dietary treatment of weight loss in patients with advanced cancer and cachexia: a systematic literature review. Crit Rev Oncol Hematol 2014;91:210–21. [DOI] [PubMed] [Google Scholar]
- [11].Heber D, Li Z. Nutrition intervention in cancer. Med Clin North Am 2016;100:1329–40. [DOI] [PubMed] [Google Scholar]
- [12].Li G, Gao J, Liu ZG, et al. Influence of pretreatment ideal body weight percentile and albumin on prognosis of nasopharyngeal carcinoma: long-term outcomes of 512 patients from a single institution. Head Neck 2014;36:660–6. [DOI] [PubMed] [Google Scholar]
- [13].Omlin A, Blum D, Wierecky J, et al. Nutrition impact symptoms in advanced cancer patients: frequency and specific interventions, a case-control study. J Cachexia Sarcopenia Muscle 2013;4:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ravasco P, Monteiro-Grillo I, Camilo M. Individualized nutrition intervention is of major benefit to colorectal cancer patients: long-term follow-up of a randomized controlled trial of nutritional therapy. Am J Clin Nutr 2012;96:1346–53. [DOI] [PubMed] [Google Scholar]
- [15].Gangadharan A, Choi SE, Hassan A, et al. Protein calorie malnutrition, nutritional intervention and personalized cancer care. Oncotarget 2017;8:24009–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Huang J, Wang Y, Yuan Y, et al. Preoperative serum pre-albumin as an independent prognostic indicator in patients with localized upper tract urothelial carcinoma after radical nephroureterectomy. Oncotarget 2017;8:36772–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].English R, Metcalfe C, Day J, et al. A prospective analysis of implementation of multi-disciplinary team decisions in breast cancer. Breast J 2012;18:459–63. [DOI] [PubMed] [Google Scholar]


