Abstract
Background
CD4+ cell counts reflect immunologic status of human immunodeficiency virus (HIV) patients. Recommended CD4+ cell counts for the initiation of highly active antiretroviral therapy (HAART) has increased over the past several years in various HIV treatment guidelines. We investigated the trend of CD4+ cell counts at diagnosis and treatment start using data from the Korea HIV/acquired immune deficiency syndrome (AIDS) Cohort Study.
Materials and Methods
The Korea HIV/AIDS Cohort Study started in 2006 and enrolled HIV patients from 21 tertiary and secondary hospitals in South Korea. The data for CD4+ cell counts at diagnosis and HAART initiation from these HIV patients were analyzed by three-year time intervals and presented by number of CD4+ cells (≤100, 101-200, 201-350, 351-500 and >500 cells/mm3). The HIV-RNA titer at diagnosis and HAART initiation were presented by 3-year intervals by groups ≤50,000, 50,001-100,000, 100,001-200,000, 200,001-1,000,000, and >1,000,000 copies/mL.
Results
Median values of CD4+ cell count and HIV-RNA titer at initial HIV diagnosis were 247 cells/mm3 and 394,955 copies/mL, respectively. At time of initiating HAART, median values of CD4+ cell count and HIV-RNA were 181 cells/mm3 and 83,500 copies/mL, respectively. Patients with low CD4+ cell count (CD4+ cell count ≤200 cells/mm3) at diagnosis (31-51%) and initiation of HAART accounted for the largest proportion (30-65%) over the three-year time intervals. This proportion increased until 2010-2012.
Conclusion
CD4+ cell count at initiation of HAART was found to be very low, and the increase in late initiation of HAART in recent years is of concern. We think that this increase is primarily due to an increasing proportion of late presenters. We recommend early detection of HIV patients and earlier start of HAART in order to treat and prevent spread of HIV infection.
Keywords: Human immunodeficiency virus, Cohort Study, CD4+ Lymphocyte Count
Introduction
Due to developments of highly active antiretroviral therapy (HARRT), morbidity and mortality related to human immunodeficiency virus (HIV) infected patients has reduced markedly [1,2]. In 2014, the number of HIV-infected patients globally was about 36.9 million (34.3 - 41.4 million), and 2 million people were newly diagnosed with HIV [3]. At this time, 15 million HIV patients were receiving ART [3]. Previous studies have found that starting HAART when the CD4+ cell count is high is recommended for improved virologic and immunologic recovery and prevents disease progression [4,5,6]. Starting ART when CD4+ cell counts are already low results in acquired immunodeficiency syndrome (AIDS) defining disease for many patients [7]; HIV-infected patients who started HAART with a CD4+ cell count <200 cells/mm3 may not reach a normal CD4+ cell count [6]. In addition, early treatment of ART prevents sexual transmission among serodiscordant couples [8]. Considering these clinical findings, many HIV/AIDS expert groups have updated their clinical guidelines regarding the recommended time point for initiating ART. The European AIDS Clinical Society (EACS) recommends that patients whose CD4+ cell counts are <350 cells/mm3 initiate ART [9]. However, the Department of Health and Human Services (DHHS) guidelines strongly recommend that HIV-positive patients with CD4+ cell count ≤500 cells/mm3 should initiate ART [10]. The World Health Organization (WHO) also recently updated their treatment guidelines to advise that ART should be initiated for all HIV-positive adult patients, regardless of WHO clinical stage and CD4+ cell count [11]. Consistent with these other recommendations, the Korean Society for AIDS revised their guidelines in 2013 to recommend that all HIV-infected patients, regardless of CD4+ cell count, initiate ART. The guidelines also favor treatment of HIV-positive patients whose infection status is acute or who were recently infected [12]. Although previous clinical data and guidelines recommend early initiation of ART, most HIV-infected patients initiate ART when they are diagnosed with low CD4+ cell counts [2,13,14]. In Korea, the total number of patients infected with HIV in 2015 was 10,502 and there were 1,052 newly infected patients; incidence has been observed to be increasing steadily. In addition, with the support of the national HIV/AIDS policy, the proportion of patients treated with ART has increased. It is necessary to know the real status of CD4+ cell count and HIV-RNA at the HIV diagnosis and ART initiation. Therefore, we researched CD4+ cell count and HIV-RNA of Korean HIV- infected patients at the time points of diagnosis and initiation of treatment, using Korea HIV/AIDS Cohort Study data.
Materials and Methods
The Korea HIV/AIDS Cohort Study was a prospective observational cohort study with patients from 21 tertiary or secondary hospitals in South Korea, initiated in 2006. The Korea HIV/AIDS Cohort Study collected data on HIV-infected individuals, including socioeconomic status, route of infection, ART, conventional laboratory data, immunological and viral laboratory data, and information on opportunistic infections. The institutional review board approval was obtained from all participating hospitals.
Within the cohort study population, patients who had CD4+ cell count and HIV-RNA titer data at the time of diagnosis and HAART initiation were included in this study. Data were stratified on the basis of CD4+ cell count (≤100, 101-200, 201-350, 351-500, and >500 cells/mm3) and HIV-RNA titer (≤50,000, 50,001-100,000, 100,001-200,000, 200,001-1,000,000, and >1,000,000 copies/mL), and analyzed by 3-year time intervals. The stratified data are presented with percentages, average values, mean values, and quartile values.
Additionally, we investigated age, sex, transmission route, and the past medical history of patients with a CD4+ cell count at the time of diagnosis. We compared these factors based on the CD4+ cell count at diagnosis (cutoff point: CD4+ cell count 200 cells/mm3 or 350 cells/mm3). The Student-t test or the Wilcoxon Rank-Sum test was used to analyze continuous variables, and the chi-square test or the Fisher exact test was used for categorical variables. Statistical analyses were performed using R statistics version 3.2.1 (R Foundation for Statistical Computing, Vienna, Austria), and P <0.05 was considered statistically significant.
Result
1. Trend of CD4+ cell count and HIV-RNA titer at the time of diagnosis
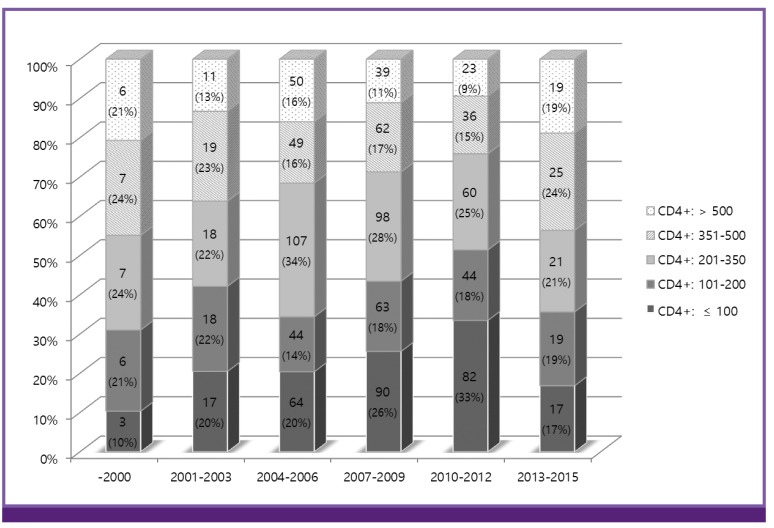
As of August 2015, 1,356 HIV-infected patients were enrolled in the Korea HIV/AIDS Cohort Study. Among the Cohort Study population, 1,124 HIV-infected patients were suitable for analysis of CD4+ cell count at time of diagnosis. Mean and median values of CD4+ cell counts were 271 cells/mm3 and 247 cells/mm3 (interquartile range [IQR] 104 - 390 cells/mm3), respectively. Table 1 shows mean and median values of CD4+ cell count at HIV diagnosis, according to three-year intervals. The patients suitable for analysis comprised between 1% and 15% of new patients with HIV/AIDS in each period (Table 1). The median age at diagnosis was 40 years (overall; IQR 31-48 years); 33 years (IQR 30-41) before 2000; 42 years (IQR 35-46) between 2001 and 2003; 40 years (IQR 31-47) between 2004 and 2006; 41 years (IQR 33-50) between 2007 and 2009; 39 years (IQR 30-51) between 2010 and 2012, and; 34 years (IQR 26-44) between 2013 and 2015. The patients with CD4+ cell counts lower than 100 cells/mm3 increased until 2012 (Fig. 1). However, in the three most recent years (2013-2015), the proportion of patients with lower initial CD4+ cell counts decreased. Additionally, the number of patients with CD4+ cell counts of more than 350 cells/mm3 at the time of diagnosis has increased (Fig. 1). However, patients with CD4+ cell counts lower than 100 cells/mm3 at diagnosis were still a substantial portion (10-33%) of the cohort study population (Fig. 1). CD4+ cell counts lower than 200 cells/mm3 at diagnosis increased over time (31-51%, maximum at 2010-2012 period). CD4+ cell counts lower than 350 cells/mm3 at diagnosis increased over time as well (55-75%, maximum at 2010-2012 period).
Table 1. CD4+ cell count and HIV-RNA titer at the time of HIV diagnosis, by 3-year intervals.
| Year | CD4+ cell count at the time of HIV diagnosis | HIV-RNA titer at the time of HIV diagnosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| -2000 | 2001-2003 | 2004-2006 | 2007-2009 | 2010-2012 | 2013-2015 | -2000 | 2001-2003 | 2004-2006 | 2007-2009 | 2010-2012 | 2013-2015 | ||
| Number of patientsa | 29 (2.2) | 83 (6.6) | 314 (15.4) | 352 (15.3) | 245 (9.7) | 101 (3.2) | 19 (1.5) | 87 (6.9) | 290 (14.2) | 338 (14.7) | 248 (9.8) | 97 (3.1) | |
| Mean value | 334 | 274 | 292 | 261 | 236 | 308 | 59,564 | 121,600 | 317,717 | 453,701 | 615,233 | 168,859 | |
| Median value | 326 | 252 | 269 | 233 | 195 | 295 | 24,724 | 38,000 | 24,000 | 43,250 | 76,651 | 36,800 | |
| Quartile | 25 | 146 | 123 | 126 | 95 | 58 | 148 | 7,521 | 3,430 | 3,155 | 5,785 | 18,700 | 11,150 |
| 75 | 471 | 444 | 417 | 375 | 348 | 441 | 107,304 | 140,000 | 120,000 | 137,750 | 213,759 | 115,900 | |
Values are presented as cells/mm3 in CD4+ cell count and copies/mL in HIV-RNA titer.
aValues in parentheses are the percentage of study population among new patients in Korea.
HIV, human immunodeficiency virus.
Figure 1.
The trend of CD4+ cell count at the time of diagnosis by 3-year intervals. As of 2015, a total of 1,124 HIV-infected patients were included. Each period was stratified by grade of CD4+ cell count: ≤100, 101-200, 201-350, 351-500, and >500 cells/mm3. Values are presented as number (percentage).
When the subjects were classified by a CD4+ cell count of 200 cells/mm3, 467 patients were included in the CD4+ cell count ≤200 cells/mm3 group. The median age at diagnosis was higher in the group with a CD4+ cell count ≤200 cells/mm3 (41 years, interquartile range [IQR] 33-49.5) (P = 0.001). With respect to their past medical history, syphilis was observed more frequently in patients with a CD4+ cell count >200 cells/mm3 (203 patients, P = 0.029). Tuberculosis was observed more frequently in patients with a CD4+ cell count ≤200 cells/mm3 (109 patients, P <0.0001) (Table 2).
Table 2. Factors associated with low CD4+ cell count in patients with HIV infection at the time of diagnosis.
| CD4+ >200 (n=657) | CD4+ ≤200 (n=467) | P-value | |
|---|---|---|---|
| Gender | 0.550 | ||
| Female | 48 (7.3) | 29 (6.2) | |
| Male | 609 (92.7) | 438 (93.8) | |
| Median age at diagnosis in years | 39 (30-48) | 41 (33-49.5) | 0.001 |
| Age at diagnosis | 0.002 | ||
| ≤29 | 150 (22.8) | 69 (14.8) | |
| 30-39 | 199 (30.3) | 130 (27.8) | |
| 40-49 | 166 (25.3) | 151 (32.3) | |
| 50-59 | 95 (14.5) | 72 (15.4) | |
| ≥60 | 47 (7.2) | 45 (9.6) | |
| Estimated transmission route | |||
| Sexual intercourse | 572 (87.1) | 404 (86.5) | 0.628 |
| - MSMa | 287 (43.7) | 166 (35.5) | 0.007 |
| - Heterosexual | 230 (35.0) | 202 (43.3) | 0.003 |
| - Unknown | 55 (8.4) | 36 (7.7) | |
| IVDU | 0 (0) | 5 (1.1) | 0.024 |
| Transfusion | 9 (1.4) | 15 (3.2) | 0.045 |
| Injection of coagulation factor | 2 (0.3) | 2 (0.4) | 1.000 |
| Unknown | 74 (11.3) | 41 (8.8) | |
| Past medical history | |||
| HBV infection | 34 (5.2) | 19 (4.1) | 0.464 |
| HCV infection | 6 (0.9) | 5 (1.1) | 1.000 |
| Syphilis | 203 (30.9) | 119 (25.5) | 0.029 |
| Gonorrhea | 43 (6.5) | 30 (6.4) | 1.000 |
| Non-gonococcal urethritis | 38 (5.8) | 24 (5.1) | 0.754 |
| Tuberculosis | 72 (11.0) | 109 (23.3) | <0.0001 |
Values are presented as median (interquartile range) or number (%).
aMSM included homosexual or bisexual.
HIV, human immunodeficiency virus; MSM, men who have sex with men; IVDU, intravenous drug user; HBV, hepatitis B virus; HCV, hepatitis C virus.
When the subjects were classified by a CD4+ cell count of 350 cells/mm3, 778 patients were included in the CD4+ cell count ≤350 cells/mm3 group (low CD4+ group) and 346 patients were included in the CD4+ cell count >350 cells/mm3 group (high CD4+ group). The median age at diagnosis was 41 years in the low CD4+ group (IQR 32-49), which was higher than that of the high CD4+ group (38.5 years, IQR 31-48) (P = 0.038). Syphilis was observed in 213 patients in the low CD4+ group and in 109 patients in the high CD4+ group, which was not statistically significant (P = 0.169). Tuberculosis was observed more frequently in the low CD4+ group (148/778) [19%] than in the high CD4+ group (33/346) [9.5%] (P <0.0001).
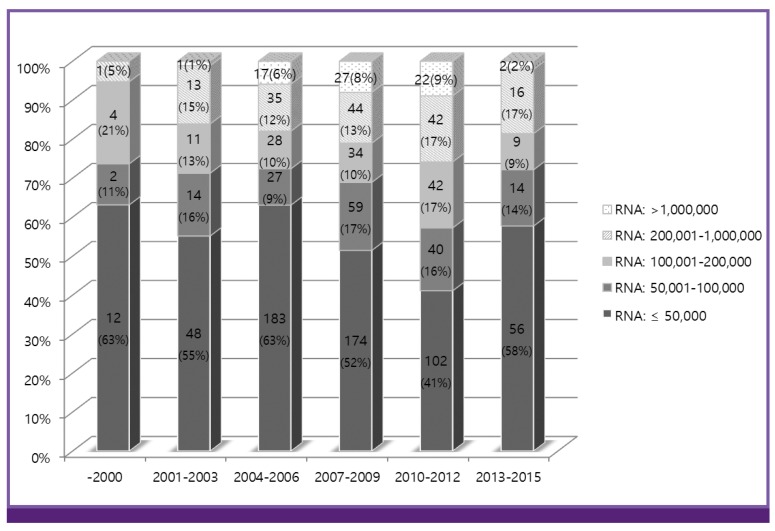
A total of 1,079 HIV-infected patients met the criteria for analysis of HIV-RNA titer at the time of diagnosis. Mean and median values of HIV-RNA titer were 394,955 copies/mL and 39,436 copies/mL (IQR, 7,150-151,000 copies/mL), respectively. Until the 2010-2012 period, the proportion of patients with HIV-RNA <50,000 copies/mL decreased (Fig. 2).
Figure 2.
The trend of HIV-RNA titer at the time of diagnosis by 3-year intervals. As of 2015, a total of 1,079 HIV-infected patients were included. Each period was stratified by the level of HIV-RNA titer: ≤50,000, 500,001-100,000, 100,001-200,000, 200,001-1,000,000, and >1,000,000 copies/mL. Values are presented as number (percentage).
2. Trend of CD4+ cell count and HIV-RNA titer at the time of initiating HAART
A total of 376 HIV-infected patients met the criteria for analysis of CD4+ cell count at time of initiating HAART. Mean and median values of CD4+ cell counts were 194 cells/mm3 and 181 cells/mm3 (IQR, 63-270 cells/mm3), respectively. Median value of CD4+ cell count was lowest in 2010-2012 period, and those values showed a decrease pattern until 2010-2012 period (Table 3).
Table 3. CD4+ cell count and HIV-RNA titer at the time of initiating highly active antiretroviral therapy, by 3-year intervals.
| Year | CD4+ cell count at the time of initiating HAART | HIV-RNA titer at the time of initiating HAART | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| -2000 | 2001-2003 | 2004-2006 | 2007-2009 | 2010-2012 | 2013-2015 | -2000 | 2001-2003 | 2004-2006 | 2007-2009 | 2010-2012 | 2013-2015 | ||
| Number of patients | 12 | 48 | 127 | 110 | 69 | 10 | 3 | 38 | 104 | 102 | 66 | 9 | |
| Mean value | 229 | 212 | 213 | 172 | 156 | 320 | 11,103 | 179,463 | 696,943 | 419,355 | 603,373 | 343,503 | |
| Median value | 232 | 192 | 195 | 153 | 120 | 246 | 8,021 | 93,400 | 94,500 | 65,972 | 119,500 | 110,000 | |
| Quartile | 25 | 135 | 116 | 77 | 60 | 38 | 179 | 289 | 18,105 | 16,167 | 10,300 | 35,025 | 18,665 |
| 75 | 341 | 307 | 284 | 258 | 237 | 453 | 25,000 | 213,500 | 498,500 | 260,000 | 315,250 | 705,501 | |
Values are presented as cells/mm3 in CD4+ cell count and copies/mL in HIV-RNA titer.
HIV, human immunodeficiency virus; HAART, highly active antiretroviral therapy.
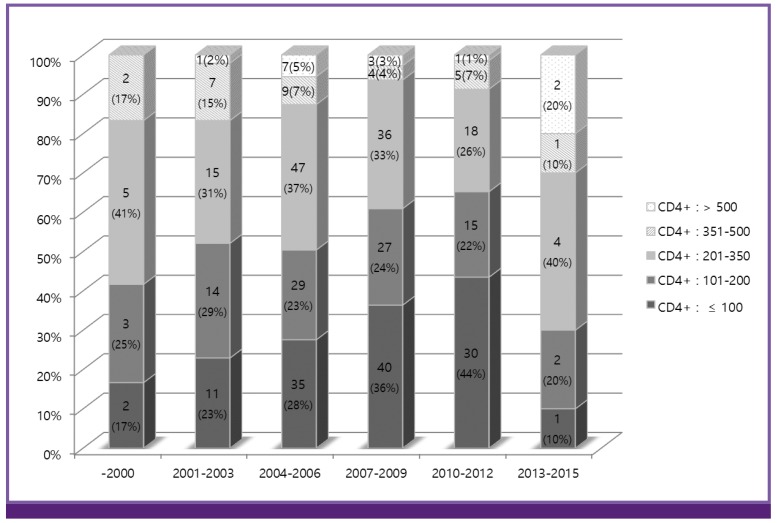
The overall trend found was that the proportion of patients whose CD4+ cell count at initiation of HAART was over 350 cells/mm3 has decreased (Fig. 3), whereas, the proportion of patients with CD4+ cell counts lower than 350 cells/mm3 at initiation of HAART has increased. In addition, the proportion of patients with CD4+ cell counts lower than 100 cells/mm3 at initiation of HAART has increased; in 2010-2012 period, those patients account for 43% (Fig. 3). CD4+ cell counts lower than 200 cells/mm3 at initiation of HAART showed increasing tendency (30-65%, maximum at 2010-2012 period).
Figure 3.
The trend of CD4+ cell count at the time of initiating highly active antiretroviral therapy by 3-year intervals. As of 2015, 376 HIV patients were included. CD4+ cell count, ≤100, 101-200, 201-350, 351-500, and >500 cells/mm3, is stratified for each time interval. Values are presented as number (percentage).
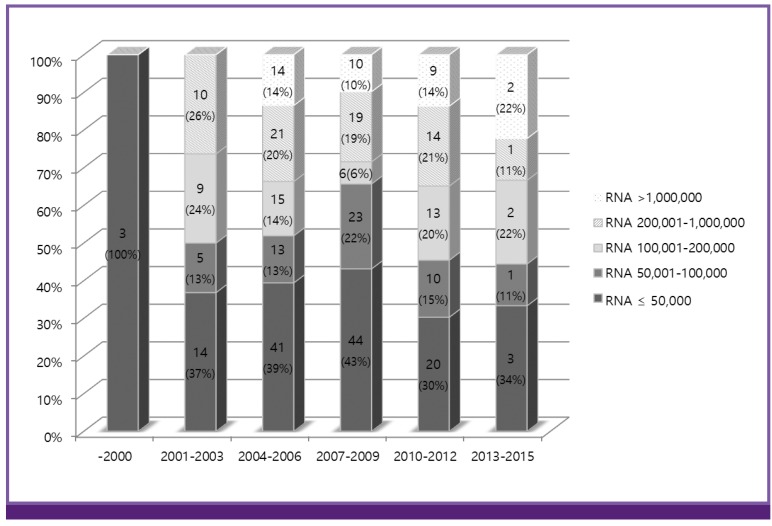
A total of 322 HIV-infected patients met the criteria for analysis of HIV-RNA titers at initiation of HAART. The mean and median values of HIV-RNA titers were 493,116 copies/mL and 83,500 copies/mL (IQR, 15,763-292,500 copies/mL), respectively. The proportion of patients with HIV-RNA <50,000 copies/mL has steadily decreased, and patients with high RNA titer at treatment has increased (Fig. 4).
Figure 4.
The trend of HIV-RNA titer at the time of initiating highly active antiretroviral therapy by three-year intervals. As of 2015, 322 HIV patients were included. Level of HIV-RNA: ≤50,000; 50,001-100,000; 100,001-200,000; 200,001-1,000,000; and >1,000,000 copies/mL is stratified for each time interval. Values are presented as number (percentage).
Discussion
Based on Korea HIV/AIDS Cohort Study data, we found from our analysis that patients whose CD4+ cell count at the time of diagnosis was lower than 350 cells/mm3 accounted for over half of all patients. In particular, the proportion of patients with CD4+ cell count ≤100 cells/mm3 at the time of diagnosis has steadily increased from 2000 to the 2010-2012 time interval. In other Korea HIV data from the Korea National Institute of Health, the proportion of patients with CD4+ T cell count <200 cells/mm3 increased from before 1993 to the period of 2004 to 2006 [15]. Similar to previous reports, our cohort data showed gradual increase of patients with CD4+ cell count <200 cells/mm3. Presentation of CD4+ cell count lower than 350 cells/µL at the time of diagnosis has also been found in other countries. In northwest Spain data from 2004-2013, 53.1% of newly infected HIV patients had low CD4+ cell counts (CD4+ count <350 cells/mm3) [16]. In the United Kingdom, 49% of newly infected HIV patients in 2011 were diagnosed at a low CD4+ cell count, lower than 350 cells/mm3 [17]. Shen et al. reported the CD4+ cell count at the time of diagnosis in China. From 2009-2010, about 72% of patients had a low CD4+ cell count, ≤200 cells/mm3, which was lower than in our report [18].
Our study showed that many patients initiated HAART at a low CD4+ cell count. The proportion of patients with a low CD4+ cell count at time of HAART initiation gradually increased until recently. We think that this result is influenced by an increase in patients with low CD4+ cell count at the time of diagnosis. More patients with CD4+ cell count ≤100 cells/µL at time of diagnosis have been observed, and this tendency has increased over time.
In contrast to our national trends, recent reports from Asia showed a tendency towards increased CD4+ cell count at initiation of treatment. The TAHOD-TASER Cohort Study reported trends of CD4+ cell count at the initiation of HAART over time. Before 2010, median CD4+ cell count at the start of treatment was lower than 200 cells/mm3. Since 2011, median CD4+ cell count has been increasing substantially. The median CD4+ cell count in 2011 and after 2011 was 249 cells/mm3 and 302 cells/mm3, respectively. In addition, the proportion of patients with CD4+ cell count <200 cells/mm3 at initiation of HAART markedly decreased over time, from 82.4% in 2007 to 36.3% after 2011 [2]. This CD4+ cell count trend was similar to the findings from a study performed in Shanghai, China. The median CD4+ cell count had increased from 65 cells/mm3 in 2006 to 203 cells/mm3 in 2011. The proportion of patients with CD4+ cell count <200 cells/mm3 decreased from 88.5% in 2006 to 49.6% in 2011 [19]. In Rwanda, an upswing in the median CD4+ cell count at HAART initiation was observed. While the median CD4+ cell count was 183 cells/mm3 in 2007, the median CD4+ cell count was 293 cells/mm3 in 2011-2012. The proportion of patients with advanced HIV disease (CD4+ cell count <200 cells/mm3 or WHO stage IV) had decreased from 66.2% to 29.4% [20]. In these three studies, the proportion of patients with CD4+ cell count <200 cells/mm3 at HAART initiation, after 2010, was similar to our findings. However, the findings showed improvement in CD4+ cell counts at HAART initiation, which was in contrast to what we observed in our cohort data. Research from industrialized countries show a stable median CD4+ cell count over 300 cells/mm3 at HAART initiation for a period of about twenty years [21,22]. In this study, consistent low median CD4+ cell counts have been observed, which were lower than those observed in other developed countries.
Upon comparing the factors based on the CD4+ cell count at diagnosis (cutoff point: 200 cells/mm3 or 350 cells/mm3), the median age at diagnosis was higher in patients with a low CD4+ cell count than in patients with a high CD4+ cell count. In addition, between 2001 and 2012, the median age at diagnosis for each period was high. Among the associated risk factors, a history of tuberculosis was observed more frequently in patients with a low CD4+ cell count. This finding may be associated with the risk of opportunistic tuberculous infection. Moreover, sexual contact among males and a history of syphilis were more frequently recorded in patients with a high CD4+ cell count. This finding suggests that the opportunity of diagnostic test would have influenced the rate of low CD4+ cell count at diagnosis.
Our study has limitations. The size of the study population, when divided into each three-year interval time period, was small. However, we believe our cohort data provides an understanding of early-stage immune status of Korean HIV patients, as well as CD4+ status at initial treatment.
In summary, the Korea HIV/AIDS Cohort Study population comprised patients who had CD4+ cell count and HIV-RNA titer values at the time of diagnosis and initiation of AHAART. Our findings, based on analysis of cohort study data, suggest that early detection of HIV patients and earlier initiation of HAART, to treat and prevent the spread of HIV infection, is needed.
Acknowledgments
This study was supported by a grant for the Chronic Infectious Disease Cohort Study (Korea HIV/AIDS Cohort Study, 2016-E51003-00) from the Korea Centers for Disease Control and Prevention. We thank the members of the Korea HIV/AIDS Cohort. The Korea HIV/AIDS Cohort study group consists of Min Ja Kim, Jang Wook Sohn, Young Kyung Yoon, Jun Hee Woo, Sang Il Kim, Youn Jeong Kim, Dae Won Park, Won Suk Choi, Seong-Heon Wie, Ji-An Hur, Shin-Woo Kim, Hyun-Ha Chang, Min Jung Kim, Sang Ah Lee, Woo-Joo Kim, Joon-Young Song, Joong Shik Eom, Jin Seo Lee, So Yeon Park, Hye Won Jeong, Jin-Soo Lee, Ji Hyeon Baek, Hee Jung Choi, June Myung Kim, Jun Yong Choi, Nam Su Ku, Hyo-Youl Kim, Young Hwa Choi, Eun Jung Lee, Tae Hyong Kim, Bo Youl Choi, Mee-Kyng Kee, Chun Kang, and Ju-yeon Choi.
Footnotes
Conflict of Interest: No conflicts of interest.
References
- 1.Hermans SM, van Leth F, Manabe YC, Hoepelman AI, Lange JM, Kambugu A. Earlier initiation of antiretroviral therapy, increased tuberculosis case finding and reduced mortality in a setting of improved HIV care: a retrospective cohort study. HIV Med. 2012;13:337–344. doi: 10.1111/j.1468-1293.2011.00980.x. [DOI] [PubMed] [Google Scholar]
- 2.Kiertiburanakul S, Boettiger D, Lee MP, Omar SF, Tanuma J, Ng OT, Durier N, Phanuphak P, Ditangco R, Chaiwarith R, Kantipong P, Lee CK, Mustafa M, Saphonn V, Ratanasuwan W, Merati TP, Kumarasamy N, Wong WW, Zhang F, Pham TT, Pujari S, Choi JY, Yunihastuti E, Sungkanuparph S TREAT Asia HIV Observational Databases (TAHOD); TREAT Asia Studies to Evaluate Resistance (TASER) Trends of CD4 cell count levels at the initiation of antiretroviral therapy over time and factors associated with late initiation of antiretroviral therapy among Asian HIV-positive patients. J Int AIDS Soc. 2014;17:18804. doi: 10.7448/IAS.17.1.18804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Fact sheet: 2014 statistics. [Accessed 24 August 2015]. Available at: http://www.unaids.org/en/resources/documents/2015/20150714_factsheet.
- 4.Asfaw A, Ali D, Eticha T, Alemayehu A, Alemayehu M, Kindeya F. CD4 cell count trends after commencement of antiretroviral therapy among HIV-infected patients in Tigray, Northern Ethiopia: a retrospective cross-sectional study. PLoS One. 2015;10:e0122583. doi: 10.1371/journal.pone.0122583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamashita TE, Phair JP, Muñoz A, Margolick JB, Detels R, O’Brien SJ, Mellors JW, Wolinsky SM, Jacobson LP. Immunologic and virologic response to highly active antiretroviral therapy in the Multicenter AIDS Cohort Study. AIDS. 2001;15:735–746. doi: 10.1097/00002030-200104130-00009. [DOI] [PubMed] [Google Scholar]
- 6.Kelley CF, Kitchen CM, Hunt PW, Rodriguez B, Hecht FM, Kitahata M, Crane HM, Willig J, Mugavero M, Saag M, Martin JN, Deeks SG. Incomplete peripheral CD4+ cell count restoration in HIV-infected patients receiving long-term antiretroviral treatment. Clin Infect Dis. 2009;48:787–794. doi: 10.1086/597093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker JV, Peng G, Rapkin J, Abrams DI, Silverberg MJ, MacArthur RD, Cavert WP, Henry WK, Neaton JD Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA) CD4+ count and risk of non-AIDS diseases following initial treatment for HIV infection. AIDS. 2008;22:841–848. doi: 10.1097/QAD.0b013e3282f7cb76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim JG, Kumwenda J, Grinsztejn B, Pilotto JH, Godbole SV, Mehendale S, Chariyalertsak S, Santos BR, Mayer KH, Hoffman IF, Eshleman SH, Piwowar-Manning E, Wang L, Makhema J, Mills LA, de Bruyn G, Sanne I, Eron J, Gallant J, Havlir D, Swindells S, Ribaudo H, Elharrar V, Burns D, Taha TE, Nielsen-Saines K, Celentano D, Essex M, Fleming TR, HPTN 052 Study Team Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European AIDS Clinical Society (EACS) The European Guidelines for treatment of HIV infected adults in Europe. [Accessed 4 November 2015]. Available at: http://www.eacsociety.org/files/2015_eacsguidelines_8.0-english_revised-20151104.pdf.
- 10.Department of Health and Human Services (HHS) Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. [Accessed 8 April 2015]. Available at: https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf.
- 11.World Health Organization (WHO) Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. [Accessed 30 September 2015]. Available at: http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf. [PubMed]
- 12.The Korean Society for AIDS The 2013 clinical guidelines for the diagnosis and treatment of HIV/AIDS in HIV-infected Koreans. Infect Chemother. 2013;45:455–461. doi: 10.3947/ic.2013.45.4.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kiertiburanakul S, Boonyarattaphun K, Atamasirikul K, Sungkanuparph S. Clinical presentations of newly diagnosed HIV-infected patients at a university hospital in Bangkok, Thailand. J Int Assoc Physicians AIDS Care (Chic) 2008;7:82–87. doi: 10.1177/1545109708315485. [DOI] [PubMed] [Google Scholar]
- 14.Korean Society for AIDS The 2015 clinical guidelines for the treatment and prevention of opportunistic infections in HIV-infected Koreans: guidelines for opportunistic infections. Infect Chemother. 2016;48:54–60. doi: 10.3947/ic.2016.48.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kee MK, Lee JH, Kim GJ, Choi BS, Hong KJ, Lee JS, Kim SS. Decrease of initial CD4+ T-cell counts at the time of diagnosis of HIV infection in Korea; 1988-2006. Int J STD AIDS. 2010;21:120–125. doi: 10.1258/ijsa.2008.008405. [DOI] [PubMed] [Google Scholar]
- 16.Pernas B, Mena A, Cañizares A, Grandal M, Castro-Iglesias A, Pértega S, Pedreira JD, Poveda E. Trends on epidemiological, virological, and clinical features among newly diagnosed HIV-1 persons in Northwest Spain over the last 10 years. J Med Virol. 2015;87:1319–1326. doi: 10.1002/jmv.24185. [DOI] [PubMed] [Google Scholar]
- 17.Delpech V, Brown AE, Croxford S, Chau C, Polavarapu V, Cooper N, Rooney G, Yin Z. Quality of HIV care in the United Kingdom: key indicators for the first 12 months from HIV diagnosis. HIV Med. 2013;14(Suppl 3):19–24. doi: 10.1111/hiv.12070. [DOI] [PubMed] [Google Scholar]
- 18.Shen Y, Lu H, Wang Z, Qi T, Wang J. Analysis of the immunologic status of a newly diagnosed HIV positive population in China. BMC Infect Dis. 2013;13:429. doi: 10.1186/1471-2334-13-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen Y, Wang J, Qi T, Wang Z, Lu H. Trends in clinical characteristics of HIV-infected patients initiating antiretroviral therapy in Shanghai from 2006 to 2011. Int J STD AIDS. 2013;25:504–510. doi: 10.1177/0956462413515198. [DOI] [PubMed] [Google Scholar]
- 20.Mutimura E, Addison D, Anastos K, Hoover D, Dusingize JC, Karenzie B, Izimukwiye I, Mutesa L, Nsanzimana S, Nash D IeDEA Central Africa Collaboration. Trends in and correlates of CD4+ cell count at antiretroviral therapy initiation after changes in national ART guidelines in Rwanda. AIDS. 2015;29:67–76. doi: 10.1097/QAD.0000000000000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miranda AC, Moneti V, Brogueira P, Peres S, Baptista T, Aldir I, Ventura F, Borges F, Mansinho K. Evolution trends over three decades of HIV infection late diagnosis: the experience of a Portuguese cohort of 705 HIV-infected patients. J Int AIDS Soc. 2014;17(Suppl 3):19688. doi: 10.7448/IAS.17.4.19688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lesko CR, Cole SR, Zinski A, Poole C, Mugavero MJ. A systematic review and meta-regression of temporal trends in adult CD4(+) cell count at presentation to HIV care, 1992-2011. Clin Infect Dis. 2013;57:1027–1037. doi: 10.1093/cid/cit421. [DOI] [PubMed] [Google Scholar]