Abstract
Purpose
HIV-infected pregnant women in sub-Saharan Africa are at risk for depression and alcohol abuse. Young women may be more vulnerable, but little is known about the psychosocial functioning of this population.
Methods
We compared younger (18–24 year-olds) and older (≥25 year-olds) HIV-infected pregnant women initiating antiretroviral therapy (ART) in Cape Town, South Africa. Women were assessed on a range of psychosocial measures, including the Alcohol Use Disorders Identification Test, and the Edinburgh Postnatal Depression Scale (EPDS).
Results
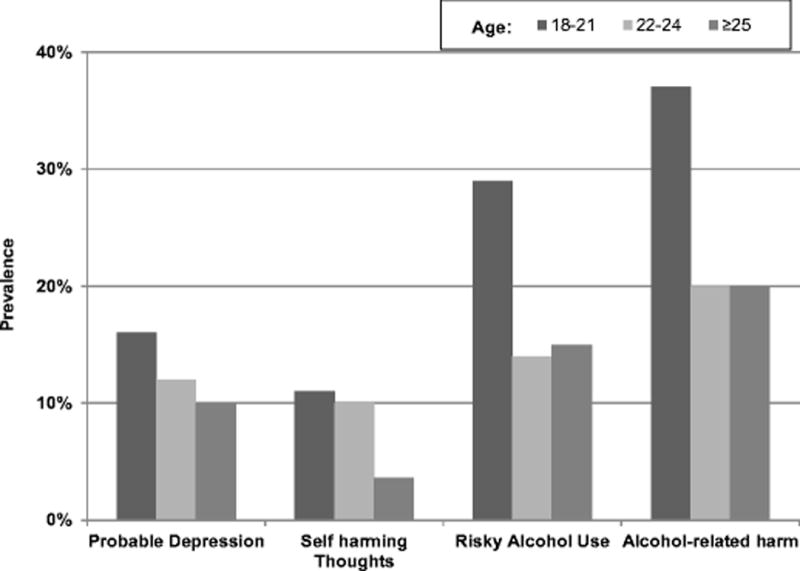
Among 625 women initiating ART, 16% reported risky alcohol use, and 21% alcohol-related harm; these percentages were similar across age groups. When younger women were stratified by age, 37% of 18–21 year-olds vs. 20% of 22–24 year-olds reported alcohol-related harm (p=0.02). Overall, 11% of women had EPDS scores suggesting probable depression, and 6% reported self-harming thoughts. Younger women reported more depressive symptoms. Report of self-harming thoughts was 11% in younger and 4% in older women (p=0.003). In multivariable analysis, age remained significantly associated with depressive symptoms and report of self-harming thoughts. Level of HIV-related stigma and report of intimate partner violence modified the association between age and depressive symptoms.
Conclusions
Young HIV-infected pregnant women in South Africa were more likely to report depressive symptoms and self-harming thoughts compared to older women and the youngest women reported the highest levels of alcohol-related harm. HIV-related stigma may be a moderating factor. These findings have implications for maternal and infant health, underscoring the urgent need for effective targeted interventions in this vulnerable population.
Keywords: HIV, pregnancy, South Africa, depression, alcohol, youth
Background
The transition from adolescence to the independence of young adulthood is a complex process that involves the development of gradually increasing abilities for long-term planning, self-reliance, and emotional stability. Limited capacities in these domains place adolescents and young adults at risk for hazardous substance use, risky sexual behaviors, and poor mental health outcomes. South Africa has high rates of adolescent and youth pregnancy, with 12.4% of young women age 15–19 years old reporting ever having been pregnant (Gray and Vawda 2016). Young women in South Africa are also at high risk of new HIV acquisition, with the highest lifetime risk occurring before the age of 25 (Kharsany et al. 2012; Pettifor et al. 2005). Emerging data from Kenya and South Africa demonstrated that being an HIV-infected adolescent mother was associated with decreased engagement in antenatal care, lower uptake of prevention of mother-to-child transmission (PMTCT) services and antiretroviral therapy (ART), increased dropout at all stages of the PMTCT care and treatment cascade, and 2–3 times the odds of mother-to-child HIV transmission when compared to adult women (Fatti et al. 2014; Horwood et al. 2013; Ramraj 2015; Ronen 2015; Woldesenbet et al. 2015).
There are several psychosocial factors that may be associated with poorer PMTCT outcomes among HIV-infected pregnant women in South Africa, including depression, alcohol use, and intimate partner violence. Among HIV-infected pregnant women in South Africa, prevalence of depression is 30–50%, and is associated with less social support, higher levels of HIV-related stigma, and poverty (Desmond et al. 2012; Napierala Mavedzenge et al. 2011; O’Connor et al. 2011). Among HIV-infected pregnant women in South Africa, 20–30% used alcohol; those using alcohol were more likely to be young, and report depressive symptoms (Desmond et al. 2012; O’Connor et al. 2011; Vythilingum et al. 2012). Women in South Africa also report high rates of intimate partner violence during pregnancy, with prevalence rates ranging from 30–50% (Shamu et al. 2011). Both depression and alcohol abuse are associated with poor adherence to ART, which could lead to poor PMTCT outcomes(Psaros et al. 2014) (Nakimuli-Mpungu et al. 2012; Psaros et al. 2014; Turan et al. 2014). Additional data are needed in South Africa evaluating depression and alcohol use and their effects on uptake and maintence of PMTCT and resulting infant outcomes. In addition, 60% of pregnancies in South Africa are unplanned with even higher rates (85%) among younger women (Woldesenbet et al. 2015). Most HIV-infected women are diagnosed when they are routinely tested when presenting for antenatal care during pregnancy.
Studies among South African adolescents report 20–40% prevalence of depression, and 13% risky alcohol use (Cheng et al. 2014; Kaufman et al. 2014; Nduna et al. 2010). Some studies suggest that younger age may be associated with risky alcohol use and depression during pregnancy (HIV-status not specified) (Hartley et al. 2011; O’Connor et al. 2011). Evaluation of depression, alcohol use and other psychosocial factors in young HIV-infected pregnant women, who may be at highest risk for adverse psychosocial profile, pregnancy and PMTCT outcomes, has not been well described, which may be critical for prevention and treatment efforts. To date, few evidence-based interventions exist for this population.
The World Health Organization has identified young people as a vulnerable population, defined as 15 to 24 years of age (World Health Organization. 2013). Therefore, the goals of this paper are to describe demographic and psychosocial factors in HIV-infected pregnant women, comparing younger women in the cohort, 18–24 years old to those ≥25 years old (World Health Organization. 2013). Elucidating these factors presents an opportunity for potential interventions to improve maternal treatment outcomes in this highly vulnerable and under recognized population that may have far reaching implications for their children and families.
Methods
Study Sample
HIV-infected pregnant women were recruited from the Gugulethu Midwife Obstetric Unit in Cape Town, South Africa, a large public sector clinic providing primary antenatal services to the surrounding district and sees approximately 4800 women annually. This facility serves an estimated population of 350,000, with high levels of poverty; 60% of the community lives in informal housing, and has an unemployment rate of 40% (Myer et al. 2015). More than 95% of women attend at least one antenatal clinic visit before delivery, and PMTCT services are integrated into antenatal care. HIV prevalence was 33% among women attending the clinic, and 23% in the surrounding district. ART has been integrated into antenatal care since January 2012, and Option B+ since July 2013 (Myer et al. 2016). During the study period, 99–100% of women offered HIV testing accepted testing. Depending on the time period based on changing service delivery models at the clinic, approximately 34–46% of HIV-infected women presenting to care were already on ART, and 54–66% were not on ART at time of presentation to care. Prior to July 2013, 83% of those ART eligible were initiated on ART during pregnancy. After the adoption of Option B+, 92% of women initiated ART during pregnancy (Myer et al. 2016).
Data for this study came from an observational cohort of HIV-infected pregnant women enrolled in the Strategies to Optimize Antiretroviral Therapy Services for Maternal and Child Health (MCH-ART) study, a multiphase implementation science study evaluating strategies for HIV care and treatment delivery during the post-partum period to HIV-infected pregnant women initiating ART and their exposed infants (https://clinicaltrials.gov/ct2/show/NCT01933477) (Myer et al. 2016). This is a secondary analysis that focuses on the observational cohort of women who initiated ART during pregnancy, and were followed through delivery. Of 658 ART eligible women, 628 women were enrolled, with 23 women not successfully enrolled due to late gestational age at presentation to care, and seven women refusing participation.
Procedures/Measurements/Variables
Women found to be HIV-infected upon presentation to antenatal care were referred for enrollment into the study. These women completed demographic and pregnancy-related questionnaires at their first antenatal care visit (first study visit). CD4 (Beckman Coulter) and HIV viral load (Abbott RealTime HIV-1) testing was performed as part of routine care and subsequently abstracted from patient charts for study purposes. These laboratory blood tests were processed by the South African National Health Laboratory Services. Questionnaires were selected based on prior use and/or validation in African populations. All questionnaires were translated into isiXhosa, back translated into English, and administered by trained interviewers.
A composite poverty score was developed in order to categorize participants into tertiles based on their relative level of disadvantage. This composite score was calculated based on current employment status and a standardized composite asset index score based on housing type and household access to a flush toilet, piped water inside the home, electricity, and a refrigerator, telephone and television. Participants were categorized from least to most disadvantaged based on this score (Brittain et al. 2016).
The London Measure of Unplanned Pregnancy (LMUP) was administered at the first study visit. Women also were administered a range of psychosocial measures, including the Edinburgh Postnatal Depression Scale (EPDS), the Alcohol Use Disorders Identification Test (AUDIT), self-reported Perceived Availability of Social Support, and HIV Social Impact Scale (a measure of stigma), all administered during the second study visit which corresponded with their second antenatal clinic visit.
The LMUP assesses pregnancy intention of the current pregnancy. It contains six questions each scored from 0–2, and is scored on a scale of 0–12, with lower scores indicating unplanned pregnancy, and higher scores indicating planned pregnancy. It was recently validated in Malawi (Hall et al. 2013).
The EPDS contains ten questions assessing depressive symptoms experienced in the past seven days, with each question scored on a scale of 0–3, and total scores ranging from 0–30. It has been validated for use in pregnant women, and has been validated in multiple African settings (Tsai et al. 2013). In this analysis, the EPDS is used as a continuous variable due to the variability of scores in the South African literature and to be able to evaluate depressive symptoms (Hartley et al. 2011; Turan et al. 2014; Vythilingum et al. 2012). The most widely used cut-off score in the South African literature is ≥13 to suggest probable depression (Manikkam and Burns 2012; Rochat et al. 2013; Turan et al. 2014; Vythilingum et al. 2012). Therefore this cut-off score was also used to be able to compare overall prevalence of probable depression with other cohorts in South Africa. Question 10 of the EPDS, regarding self-harming thoughts in the past seven days, was also examined individually.
The AUDIT, one of the most widely used assessments of alcohol use globally (Babor et al. 2001), contains ten questions assessing patterns of alcohol use in the prior twelve months, with each question scored on a scale of 0–4, and total scores ranging from 0–40. An overall score above six indicates risky alcohol use (Vythilingum et al. 2012). Any score greater than zero in questions 7–10 indicate that alcohol-related harm (e.g. memory loss, injury to self or others, etc.) has already been experienced (Babor et al. 2001).
The Social Impact Scale is a measure of HIV-related stigma and contains seven questions each scored from 1–5 for a total score of 7–35, with higher scores indicating more stigma. This scale also assesses for two dimensions of stigma, social rejection and internalized shame (Fife 2000).
The Perceived Availability of Social Support contains twelve questions each scored from 1–5 for a total score of 12–60, with higher scores indicating greater perceived social support (Cohen 1988).
The World Health Organization Violence Against Women Questionnaire contains thirteen questions, four relating to psychological violence, six relating to physical violence, and three relating to sexual violence (García-Moreno 2005). In this analysis, we included any experience of psychological, physical or sexual intimate partner violence during the past twelve months.
Statistical analysis was conducted using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Categorical comparisons were made using Chi-squared tests, and means were compared by Student’s t-tests. First, the associations between age, defined as younger (18–24 years old) vs. older (≥25 years), and a variety of demographic and psychosocial factors were investigated. A second univariate analysis was then performed in order to identify other demographic and psychosocial variables that could be associated with the outcomes found to be significantly different between the two age groups (depressive symptoms and report of self-harming thoughts). These other demographic and psychosocial variables included: harmful alcohol use, experience of alcohol-related harm, pregnancy intentions, social support, social impact score, and intimate partner violence. A multivariable linear regression model was then built to assess the associations between age and depressive symptoms while adjusting for the significant associations found on the second univariate analysis. Similarly, a multivariable logistic regression model was built in order to assess the associations between age and report of self-harming thoughts. Variables that significantly modified the association between age and depressive symptoms or age and report of self-harming thoughts were analyzed using stratification by categorical variable or tertiles for continuous variables.
The younger age group was further stratified into women 18–21 years and women 22–24 years of age; these sub-groups were compared to further elucidate if the youngest women were at higher risk for an adverse psychosocial profile. There were several missing questionnaires due to accidental skipping of questionnaires in the cohort overall. Nine LMUP were missing, and the Perceived Availability of Social Support, HIV Social Impact Scale, and World Health Organization Violence Against Women Questionnaire each had two questionnaires missing.
All procedures were reviewed and approved by the Human Research Ethics Committee of the University of Cape Town Faculty of Health Sciences and the Institutional Review Board of Columbia University Medical Center. Written informed consent was obtained from all individual participants included in the study. Women found to have symptoms of depression, suicidality or problematic alcohol use were linked to the appropriate clinical and social services both within the clinic and in the community. Any woman found to be experiencing intimate partner violence was referred to the main local non-governmental agency who support victims of domestic violence and the South African Police Service.
Results
Demographic Characteristics
A total of 628 HIV-infected pregnant women who were enrolled in the study were initiated on ART in antenatal services in Cape Town, South Africa between March 2013 and June 2014. Three women did not complete the questionnaires, two missed the visit when the questionnaires were administered, and one was lost to follow up; therefore 625 women were included in this analysis (Table 1). At enrollment, the mean age was 28 years; mean CD4 cell count and HIV-RNA viral load were 383 cells/mm3 and 3.9 log copies/mL respectively (CD4 results were missing for 17 women). Eighteen percent of women were presenting with their first pregnancy, and 55% were diagnosed with HIV during the current pregnancy. During the second study visit when most of the questionnaires were administered, 94% of the women were in their second or third trimester, and 84% had initiated tenofovir and efavirenz with either lamivudine or emtricitabine as a daily single-pill combination regimen for a mean time of 20 days. The remaining 16% had not yet initiated ART by the second antenatal visit (but were still included in the study). Overall, 41% of women were married or cohabitating, 26% had completed secondary or tertiary level of education, 38% were employed, including 11% who reported being in school.
Table 1.
Demographic and psychosocial characteristics in younger versus older HIV-infected pregnant women in Cape Town, South Africa
| Demographic Characteristics | All (n=625) | 18–24 years (n=160) | ≥25 years (n=465) | p-value |
|---|---|---|---|---|
| Age, Mean (SD) | 28 (5.3) | 22 (1.7) | 30 (4.3) | |
| First pregnancy, n(%) | 114 (18) | 78 (49) | 36 (8) | <0.001 |
| Married or cohabitating, n(%) | 258 (41) | 44 (28) | 214 (46) | <0.001 |
| CD4 (cells/mm3), Mean (SD) ‡ | 383 (204) | 412 (193) | 372 (207) | 0.04 |
| Viral load at initiation (log copies/mL), Mean (SD) | 3.9 (1.0) | 4.0 (0.9) | 3.9 (1.0) | 0.6 |
| HIV diagnosis during current pregnancy, n(%) | 343 (55) | 114 (71) | 229 (49) | <0.001 |
| On ART n(%) | 523 (84) | 133 (83) | 390 (84) | 0.8 |
| Time on ART (days) Mean (SD) | 20 (16) | 20 (13) | 20 (17) | 0.7 |
| Gestational Age | 0.36 | |||
| First Trimester, n(%) | 41 (7) | 13 (8) | 28 (6) | |
| Second Trimester, n(%) | 355 (57) | 95 (59) | 260 (56) | |
| Third Trimester, n(%) | 229 (37) | 52 (33) | 177 (38) | |
| Highest Level of Education, n(%) | 0.4 | |||
| Primary/some Secondary | 460 (74) | 114 (71) | 346 (74) | |
| Completed secondary/any tertiary | 165 (26) | 46 (29) | 119 (26) | |
| Employment, n(%) | ||||
| Employed (% yes) | 237 (38) | 54 (34) | 183 (39) | 0.2 |
| Full time | 145 (61) | 17 (31) | 128 (70) | <0.001 |
| Part time/Informal | 65 (27) | 17 (31) | 48 (26) | |
| School | 27 (11) | 20 (37) | 7 (4) | |
| Poverty level | 0.8 | |||
| Most disadvantaged | 226 (37) | 59 (37) | 167 (37) | |
| Moderately disadvantaged | 189 (31) | 46 (29) | 143 (32) | |
| Least disadvantaged | 192 (32) | 53 (34) | 139 (31) | |
| Psychosocial Characteristics | ||||
| Depression symptoms | ||||
| EPDS Score (Mean, SD) | 5.3 (5.3) | 6.1 (6.0) | 5.0 (5.0) | 0.03 |
| Self-harming thoughts | 36 (6) | 17 (11) | 19 (4) | 0.003 |
| Alcohol Use (AUDIT), n(%) | ||||
| Risky alcohol use (>6) | 102 (16) | 32 (20) | 70 (15) | 0.1 |
| Alcohol-related harm | 134 (21) | 42 (26) | 92 (20) | 0.09 |
|
Pregnancy Intentions (LMUP),§ Mean (SD) |
5 (3.6) | 5 (3.5) | 5 (3.6) | 0.4 |
|
Availability of Social Support,* Mean (SD) |
51 (9.9) | 51 (9.7) | 51 (10.0) | 0.6 |
|
Social Impact Scale,* Mean (SD) Total score |
15 (5.8) | 15 (5.8) | 15 (5.9) | 0.4 |
| Social Rejection | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 0.9 |
| Internalized Shame | 12 (4.7) | 11.5 (4.7) | 12 (4.7) | 0.3 |
| Intimate Partner Violence, n(%)* | ||||
| Any abuse % | 132 (21) | 40 (25) | 92 (20) | 0.2 |
| Psychological | 92 (15) | 28 (18) | 64 (14) | 0.2 |
| Physical | 96 (15) | 31 (20) | 65 (14) | 0.1 |
| Sexual | 14 (2.2) | 1 (0.5) | 13 (3) | 0.1 |
Seventeen missing CD4.
Social Impact Scale and Intimate Partner Violence, and social support: 2 questionnaires not completed.
LMUP: 9 questionnaires not completed
The mean age for younger women (ages 18–24 years) was 22 years and 30 years for older women (≥25 years). Younger women were more likely to be experiencing their first pregnancy, to have been diagnosed with HIV during this current pregnancy, and were less likely to be married or cohabitating. Using the poverty composite score, 37% of women were categorized as the most disadvantaged, 31% moderately disadvantaged, and 32% least disadvantaged. Poverty levels were not significantly different between the two groups.
Psychosocial characteristics
Psychosocial characteristics are presented in Table 1. Pregnancy intentions were low with a mean LMUP score of 5. On average, women reported a high level of social support (mean score 51), and experiencing low stigma (mean score 15) on the Social Impact Scale. Overall, 21% of women reported having experienced any kind of intimate partner violence, with 15% reporting psychological abuse, 15% reporting physical abuse, and 2.2% reporting sexual abuse by their partners during the past 12 months. There were no differences in pregnancy intentions, perceived availability of social support, stigma, or intimate partner violence between younger and older women.
Mean score on the EPDS was low at 5.3. Eleven percent of women had depression scores ≥13, suggesting probable depression, and 6% reported self-harming thoughts during the last seven days. On the AUDIT, 16% reported risky alcohol use, and 21% reported alcohol-related harm (e.g. memory loss, injury to self or others related to alcohol use) over the past twelve months. Younger women reported more depressive symptoms with a mean EPDS score of 6.1 vs. 5.0 in older women (p=0.03) and were more likely to report self-harming thoughts in the last seven days (11% vs 4%, p=0.003) compared to older women.
Depressive symptoms and associated factors
Women who reported higher depressive symptoms were younger, single, reported harmful alcohol use, alcohol-related harm, lower pregnancy intentions, less social support, experiencing higher levels of stigma, and intimate partner violence (Table 2). After adjusting for these variables and for poverty, younger age remained significantly associated with more depressive symptoms (β=0.9, 95% CI: 0.1–1.8, p=0.04). Those reporting self-harming thoughts were more likely to be younger, report experience of higher levels of stigma, and intimate partner violence (Table 3). After adjusting for these variables and for poverty, younger age remained significantly associated with report of self-harming thoughts (aOR=3.2, 95% CI: 1.5–6.6, p=0.002). Poverty level was not significantly associated with depressive symptoms or report of self-harming thoughts.
Table 2.
Univariate and multivariable analysis of Depressive symptoms (EPDS)
| Characteristic, n(%) | Mean EPDS score (SD) | Beta (95% CI) | p-value | Adjusted beta (95% CI) | p-value |
|---|---|---|---|---|---|
| Age 18–24 | 6.1 (6.0) | 1.1 (0.2, 2.1) | 0.02 | 0.9 (0.1, 1.8) | 0.04 |
| ≥25 (reference) | 5.0 (5.0) | ||||
| HIV diagnosis during current pregnancy | |||||
| Yes | 5.3 (5.3) | 0.0 (−0.83, 0.83) | 1.0 | — | — |
| No (ref) | 5.3 (5.2) | ||||
| First pregnancy | |||||
| Yes | 5.5 (5.8) | 0.3 (−0.8, 1.3) | 0.6 | — | — |
| No (ref) | 5.2 (5.2) | ||||
| Highest Level of Education, n(%) | |||||
| Primary/some Secondary | 5.3 (5.2) | 0.2 (−0.8, 1.1) | 0.7 | — | — |
| Completed secondary/any tertiary (ref) | 5.2 (5.5) | ||||
| Relationship status | |||||
| Single | 5.7 (5.5) | 0.9 (0.1, 1.8) | 0.03 | 0.8 (−0.1, 1.6) | 0.07 |
| Married or Cohabitating (ref) | 4.7 (4.8) | ||||
| Poverty level | |||||
| Most disadvantaged | 5.7 (5.4) | 0.9 (−0.1, 2.0) | 0.07 | 0.5 (−0.5, 1.4) | 0.3 |
| Moderately disadvantaged | 5.2 (5.4) | 0.5 (−0.6, 1.5) | 0.4 | 0.1 (−0.9, 1.0) | 0.9 |
| Least disadvantaged (ref) | 4.8 (5.0) | ||||
| Alcohol | |||||
| Harmful alcohol use | |||||
| Yes | 6.4 (5.6) | 1.4 (0.3, 2.5) | 0.01 | −0.3 (−1.8, 1.2) | 0.7 |
| No (ref) | 5.0 (5.2) | ||||
| Experienced alcohol-related harm | |||||
| Yes | 6.6 (5.9) | 1.7 (0.7, 2.7) | 0.001 | 0.9 (−0.5, 2.2) | 0.2 |
| No (ref) | 4.9 (5.0) | ||||
| Pregnancy intention | −0.2 (−0.3, −0.04) | 0.01 | −0.1 (−0.2, 0.04) | 0.2 | |
| Social Support | −0.1 (−0.1, −0.06) | <0.001 | −0.01 (−0.05, 0.03) | 0.7 | |
| Social Impact Score | 0.4 (0.3, 0.4) | <0.001 | 0.3 (0.3, 0.4) | <0.001 | |
| Intimate Partner Violence | |||||
| Yes | 7.7 (5.7) | 3.1 (2.1, 4.1) | <0.001 | 2.3 (1.3, 3.3) | <0.001 |
| No (ref) | 4.6 (5.0) |
Table 3.
Univariate and multivariable analysis of Self-harming thoughts
| Characteristic, n(%) | Odds ratio (95% CI) | p-value | Adjusted odds ratio (95% CI) | p-value |
|---|---|---|---|---|
| Age 18–24 | 2.8 (1.4, 5.5) | 0.003 | 3.2 (1.5, 6.6) | 0.002 |
| HIV diagnosis during current pregnancy | 0.9 (0.5, 1.8) | 0.8 | — | |
| First pregnancy | 1.3 (0.6, 2.9) | 0.5 | — | |
| Highest Level of Education, n(%) | — | |||
| Primary/some Secondary | 1.9 (0.8, 4.6) | 0.2 | — | |
| Completed secondary/any tertiary (ref) | — | |||
| Relationship status | 0.7 | — | ||
| Single | 1.3 (0.6, 2.5) | 0.5 | ||
| Married or Cohabitating (ref) | ||||
| Poverty level | ||||
| Most disadvantaged | 1.6 (0.7, 3.9) | 0.3 | 1.2 (0.5, 3.2) | 0.7 |
| Moderately disadvantaged | 1.6 (0.6, 3.9) | 0.3 | 1.6 (0.6, 4.1) | 0.4 |
| Least disadvantaged (ref) | ||||
| Alcohol | — | |||
| Harmful alcohol use | 0.6 (0.2, 1.8) | 0.4 | — | |
| Experienced alcohol-related harm | 1.2 (0.6, 2.7) | 0.6 | — | |
| Pregnancy intention | 1.0 (0.9, 1.1) | 0.7 | — | |
| Social Support | 1.0 (1.0, 1.0) | 0.5 | — | |
| Social Impact Score | 1.2 (1.1, 1.3) | <0.001 | 1.2 (1.1, 1.3) | <0.001 |
| Intimate Partner Violence | 2.5 (1.3, 5.1) | 0.009 | 1.9 (0.8, 3.9) | 0.1 |
Level of stigma and report of intimate partner violence significantly modified the association between age and depressive symptoms. To evaluate this further, stigma was stratified by tertiles into low (<14), medium (14–18) and high (>18) levels of stigma; and intimate partner violence dichotomized to no experience of intimate partner violence and any experience of intimate partner violence. Among women experiencing the highest levels of stigma, the younger women reported significantly more depressive symptoms compared to older women (mean EPDS score 10.4 vs. 6.9, p<0.001, Figure 1). Among women experiencing intimate partner violence, younger women reported more depressive symptoms compared to older women (mean 9.8 vs. 6.8, p=0.01, Figure 2).
Figure 1. Depressive symptoms stratified by stigma and age*.
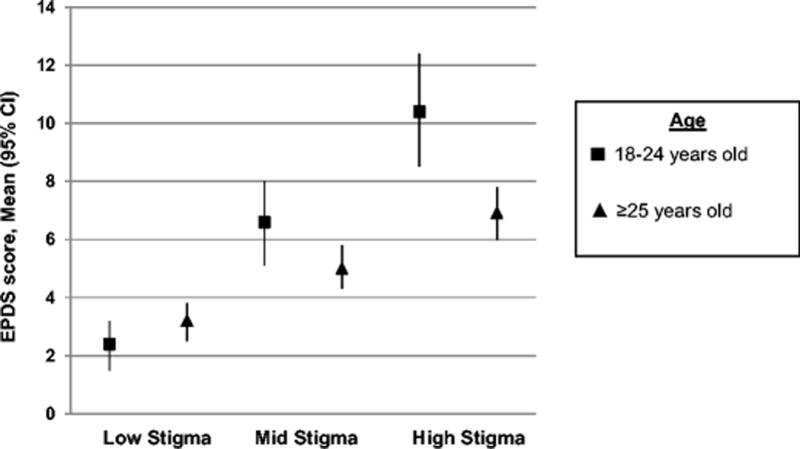
* p=0.13 (comparing 18–24 vs. ≥25 among women reporting low stigma), p=0.06 (comparing 18–24 vs. ≥25 among women reporting mid stigma), p=0.004 (comparing 18–24 vs. ≥25 among women reporting high stigma)
Figure 2. Depressive symptoms stratified by intimate partner violence (IPV) and age*.
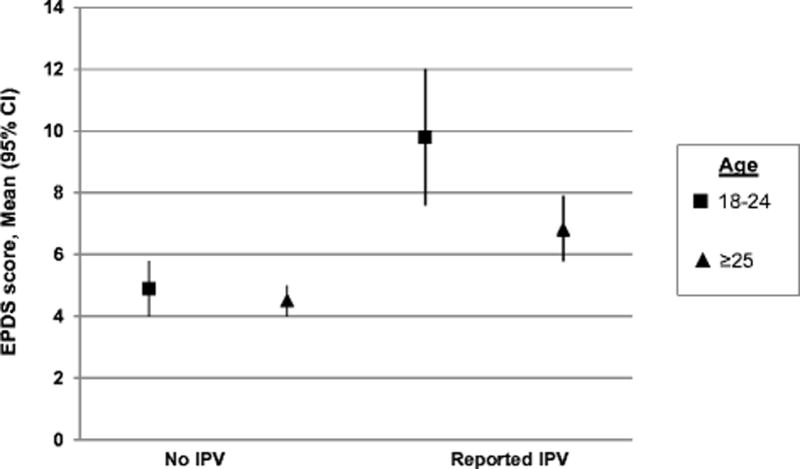
* p=0.5 (comparing 18–24 vs. ≥25 among women not reporting IPV), p=0.02 (comparing 18–24 vs. ≥25 among women reporting IPV).
Sub-group analysis of youngest women 18–21 versus 22–24
Overall, demographic characteristics were similar in women 18–21 compared to women 22–24 years old. There were no differences in mean CD4, HIV-RNA viral load, proportion diagnosed with HIV during the current pregnancy, proportion already initiated on ART, mean time on ART, education, or employment. The youngest women, age 18–21, were much more likely to be experiencing their first pregnancy (73% versus 33% in those 22–24 years old), and less likely to be married or cohabitating (8% versus 40% in those 22–24 years old). Of 18–21 year olds, 63% were still in school, which was significantly higher than those 22–24 years old. Assessing psychosocial factors, women 18–21 years old had similar levels of depressive symptoms, reports of self-harming thoughts, pregnancy intentions, social support, stigma, and intimate partner violence. The youngest women, 18–21 years, reported significantly higher rates of risky alcohol at 29% (compared to 14% in women 22–24 years, p=0.03), and higher rates of alcohol-related harm at 37% (compared to 20% in women 22–24 years, p=0.02, Figure 3).
Figure 3.
Patterns of depression and alcohol use by age
Discussion
Among this cohort of HIV-infected pregnant women initiating ART, there were low rates of scores suggesting probable depression and report of thoughts of self-harm at 11 and 6% respectively, and moderately high rates of reported risky alcohol use and experience of alcohol- related harm at 16 and 21% respectively. Our rates of probable depression were much lower than those reported in the South African literature, which ranges from a depression prevalence of 40–50% among pregnant women, and similar rates among HIV-infected women presenting for antenatal care (Hartley et al. 2011; Manikkam and Burns 2012; Rochat et al. 2013; Vythilingum et al. 2012). To measure significant depression symptoms, much of the reported literature in South Africa uses a cutoff of 12–13 on the EPDS (Hartley et al. 2011; Manikkam and Burns 2012; Rochat et al. 2013; Sawyer et al. 2010; Tsai et al. 2013; Vythilingum et al. 2012). While the EPDS has been validated in South Africa, the cutoff point for possible clinical depression is unclear. Mean EPDS scores among this population have been reported to be 12–13.5, which is higher than our mean of 5.3 (Manikkam and Burns 2012; O’Connor et al. 2011). Our lower scores on the EPDS may also be due to the fact that our sample of women is engaged in antenatal care and have agreed to be part of a larger research study. They may therefore be intrinsically at less risk for depression and alcohol use, although we are limited by the lack of data on women who did not present to antenatal care. Women who are linked to care and initiated on ART have been shown to have lower depression prevalence than those who are not (Turan et al. 2014). Depression during pregnancy has been associated with low birth weight, preterm labor, intrauterine growth retardation, and increased risk of alcohol use (Grote et al. 2010; Vythilingum et al. 2012). Treatment of depression has been shown to improve adherence to ART (Sin and DiMatteo 2014). Therefore, while the rates of depression in our cohort was relatively low, our data is biased towards those engaged in care, and further studies are needed to further elucidate the role of screening and treating depression in order to improve health outcomes for this population. Young HIV-infected pregnant women were more likely to report depressive symptoms and self-harming thoughts. Younger age remained significantly associated with depressive symptoms and self-harming thoughts even after adjusting for other factors. In HIV-infected adolescents and young adults in South Africa, prevalence of depression ranges from 18–41% (Cheng et al. 2014; Kim et al. 2014; Nduna et al. 2010). We also did not detect differences by age or associations with our outcomes despite high levels of poverty. This may be because overall rates of poverty are high in this community with little variance, limiting our study’s ability to evaluate the effects of poverty on depression and other psychosocial factors.
Our overall moderately high rate of risky alcohol use is comparable to that reported in the literature among pregnant and HIV-infected pregnant women in South Africa (Desmond et al. 2012; O’Connor et al. 2011), and is consistent with the high rates of fetal alcohol syndrome reported in the Western Cape, South Africa (May et al. 2007; Olivier et al. 2013). We also found moderately high rates of harmful alcohol use during pregnancy, with the youngest women (18–21) reporting the highest rates of risky alcohol use (29%) and alcohol-related harm (37%). Depressive symptoms and risky alcohol use may be contributing to and be consistent with emerging literature regarding poor PMTCT engagement and outcomes among younger HIV-infected pregnant women (Ramraj 2015; Ronen 2015; Woldesenbet et al. 2015).
Stigma and intimate partner violence were found to have significant associations with depressive symptoms and self-harming thoughts, which is consistent with prior studies (Psaros et al. 2014; Turan et al. 2014). While both groups of women experienced similar amounts of stigma and intimate partner violence, younger women reporting higher levels of stigma and experience of intimate partner violence were more likely to have depressive symptoms and self-harming thoughts when compared to older women reporting similar levels of stigma and intimate partner violence. This may be related to the transition towards adulthood and under-developed coping mechanisms and emotional stability, and these vulnerabilities may therefore be consistent with normative developmental challenges such as the importance of fitting into peer groups, risk-taking behaviors, and struggles with self-esteem and insecurity. However, this is exacerbated by HIV and pregnancy making these young HIV-infected pregnant women highly vulnerable, and may have long-term consequences for their own health outcomes and those of their infants and families.
The study has several strengths. It has an overall large sample size compared to previous studies, and has used a wide breadth of questionnaires to evaluate many psychosocial aspects in this population, allowing us to evaluate their potential associations with one another. It also draws attention to the youngest and most vulnerable women within this population. Our study has several limitations. Our sample consisted of HIV-infected pregnant women presenting to antenatal care who were also willing to participate in a research study, so may not be representative of the general population. Also, while the questionnaires are validated in our population, the cut-off scores still vary in the literature. All questionnaires were completed using face to face interviews, and may therefore have some under-reporting (of symptoms) bias. The cross-sectional nature of the study does not allow us to evaluate causality or evaluate symptom progression or resolution over the course of pregnancy or postpartum. Finally, while we would have liked to capture pregnant women even younger than 18 years of age, the larger overall study design excluded those experiencing pregnancy among this age group.
Conclusion
HIV-infected young pregnant women are at increased risk for depressive symptoms and self-harming thoughts, even after adjusting for other significant demographic and psychosocial factors. The youngest women have high levels of alcohol-related harm. Given the impact of depression and alcohol abuse on HIV treatment and pregnancy outcomes, these data point to the need for interventions targeting this highly vulnerable population.
Acknowledgments
We would like to acknowledge the South African women who agreed to participate in this study, as well as the Gugulethu Maternal Obstetrics Unit staff and interviewers for their logistical support. This study is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development R01-HD074558. Marcia Wong is supported by the National Institute of Allergy and Infectious Disease T32- AI100852.
List of abbreviations
- ART
antiretroviral therapy
- PMTCT
prevention of maternal to child transmission
- MCH-ART
Strategies to Optimize Antiretroviral Therapy Services for Maternal and Child Health
- LMUP
London Measure of Unplanned Pregnancy
- EPDS
Edinburgh Postnatal Depression Scale
- AUDIT
Alcohol Use Disorders Identification Test
- OR
Odds ratio
Footnotes
Conflict of Interests:
All the authors declare that they have no conflict of interests.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Literature Cited
- Babor TF, Higginsbiddle JC, Saunders JB, Monteiro M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care 2001 [Google Scholar]
- Brittain K, Mellins CA, Phillips T, Zerbe A, Abrams EJ, Myer L, Remien RH. Social Support, Stigma and Antenatal Depression Among HIV-Infected Pregnant Women in South Africa. AIDS Behav. 2016 doi: 10.1007/s10461-016-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y, et al. The association between social support and mental health among vulnerable adolescents in five cities: findings from the study of the well-being of adolescents in vulnerable environments. J Adolesc Health. 2014;55:S31–38. doi: 10.1016/j.jadohealth.2014.08.020. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical diseases. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Desmond K, et al. Alcohol consumption among HIV-positive pregnant women in KwaZulu-Natal, South Africa: prevalence and correlates. Drug and alcohol dependence. 2012;120:113–118. doi: 10.1016/j.drugalcdep.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatti G, Shaikh N, Eley B, Jackson D, Grimwood A. Adolescent and young pregnant women at increased risk of mother-to-child transmission of HIV and poorer maternal and infant health outcomes: A cohort study at public facilities in the Nelson Mandela Bay Metropolitan district, Eastern Cape, South Africa. S Afr Med J. 2014;104:874–880. doi: 10.7196/samj.8207. [DOI] [PubMed] [Google Scholar]
- Fife B, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior. 2000;41:50–67. [PubMed] [Google Scholar]
- García-Moreno C. World Health Organization: multi-country study on women’s health and domestic violence against women: initial results on prevalence, health outcomes and women’s responses. World Health Organization; Geneva: 2005. [Google Scholar]
- Gray A, Vawda Y. South African Health Review 2016 2016 [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction Arch Gen Psychiatry. 2010;67:1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall J, Barrett G, Mbwana N, Copas A, Malata A, Stephenson J. Understanding pregnancy planning in a low-income country setting: validation of the London measure of unplanned pregnancy in Malawi. BMC Pregnancy Childbirth. 2013;13:200. doi: 10.1186/1471-2393-13-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley M, et al. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. 2011;8:9. doi: 10.1186/1742-4755-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwood C, Butler LM, Haskins L, Phakathi S, Rollins N. HIV-infected adolescent mothers and their infants: low coverage of HIV services and high risk of HIV transmission in KwaZulu-Natal, South Africa. PLoS One. 2013;8:e74568. doi: 10.1371/journal.pone.0074568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman ZA, Braunschweig EN, Feeney J, Dringus S, Weiss H, Delany-Moretlwe S, Ross DA. Sexual risk behavior, alcohol use, and social media use among secondary school students in informal settlements in Cape Town and Port Elizabeth, South Africa. AIDS Behav. 2014;18:1661–1674. doi: 10.1007/s10461-014-0816-x. [DOI] [PubMed] [Google Scholar]
- Kharsany AB, Mlotshwa M, Frohlich JA, Yende Zuma N, Samsunder N, Abdool Karim SS, Abdool Karim Q. HIV prevalence among high school learners - opportunities for schools-based HIV testing programmes and sexual reproductive health services. BMC Public Health. 2012;12:231. doi: 10.1186/1471-2458-12-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MH, et al. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children’s Depression Inventory-Short amongst HIV-positive adolescents in Malawi. J Int AIDS Soc. 2014;17:18965. doi: 10.7448/IAS.17.1.18965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikkam L, Burns JK. Antenatal depression and its risk factors: an urban prevalence study in KwaZulu-Natal. S Afr Med J. 2012;102:940–944. doi: 10.7196/samj.6009. [DOI] [PubMed] [Google Scholar]
- May PA, et al. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug Alcohol Depend. 2007;88:259–271. doi: 10.1016/j.drugalcdep.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer L, Phillips T, Manuelli V, McIntyre J, Bekker LG, Abrams EJ. Evolution of antiretroviral therapy services for HIV-infected pregnant women in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2015 doi: 10.1097/QAI.0000000000000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer L, et al. Optimizing Antiretroviral Therapy (ART) for Maternal and Child Health (MCH): Rationale and Design of the MCH-ART Study. J Acquir Immune Defic Syndr. 2016;72(Suppl 2):S189–196. doi: 10.1097/QAI.0000000000001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16:2101–2118. doi: 10.1007/s10461-011-0087-8. [DOI] [PubMed] [Google Scholar]
- Napierala Mavedzenge S, Olson R, Doyle AM, Changalucha J, Ross DA. The epidemiology of HIV among young people in sub-Saharan Africa: know your local epidemic and its implications for prevention. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2011;49:559–567. doi: 10.1016/j.jadohealth.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Nduna M, Jewkes RK, Dunkle KL, Shai NP, Colman I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc. 2010;13:44. doi: 10.1186/1758-2652-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor MJ, Tomlinson M, Leroux IM, Stewart J, Greco E, Rotheram-Borus MJ. Predictors of alcohol use prior to pregnancy recognition among township women in Cape Town, South Africa. Social science & medicine. 2011;72:83–90. doi: 10.1016/j.socscimed.2010.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivier L, Urban M, Chersich M, Temmerman M, Viljoen D. Burden of fetal alcohol syndrome in a rural West Coast area of South Africa. S Afr Med J. 2013;103:402–405. doi: 10.7196/samj.6249. [DOI] [PubMed] [Google Scholar]
- Pettifor AE, et al. Young people’s sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS. 2005;19:1525–1534. doi: 10.1097/01.aids.0000183129.16830.06. [DOI] [PubMed] [Google Scholar]
- Psaros C, et al. PMTCT Adherence in Pregnant South African Women: The Role of Depression, Social Support, Stigma and Structural Barriers to Care. AIDS Research and Human Retroviruses. 2014;30:A61. doi: 10.1093/abm/kaaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramraj T, Jackson D, Dinh T, Olorunji S, Lombard C, Sherman G, Puren A, Ramokolo V, Noveve N, Singh Y, Magasana V, Bhardwaj S, Pillay Y, Goga AE. Mother-to-child transmission of HIV amongst adolescents: findings from three national surveys, South Africa, - 2010, 2011, 2012. 8th IAS Conference on HIV Pathogenesis, Treatment & Prevention; Vancouver, Canada. 2015. [Google Scholar]
- Rochat TJ, Tomlinson M, Newell ML, Stein A. Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS) Arch Womens Ment Health. 2013;16:401–410. doi: 10.1007/s00737-013-0353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronen K, Mcgrath C, Langat A, Kinuthia J, Omolo D, Singa B, Katana A, Nganga L, John-Stewart G. Lower ANC attendance and PMTCT uptake in adolescent versus adult pregnant women in Kenya. 8th IAS Conference on HIV Pathogenesis, Treatment & Prevention; Vancouver, Canada. 2015. [Google Scholar]
- Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010;123:17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One. 2011;6:e17591. doi: 10.1371/journal.pone.0017591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: a meta-analysis. Ann Behav Med. 2014;47:259–269. doi: 10.1007/s12160-013-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strategic Development Information City of Cape Town GIS Department. City of Cape Town - Census 2011-Gugulethu. 2011 http://www.capetown.gov.za/en/stats/2011CensusSuburbs/2011_Census_CT_Suburb_Gugulethu_Profile.pdf. Accessed September 17 2016.
- Tsai AC, Scott JA, Hung KJ, Zhu JQ, Matthews LT, Psaros C, Tomlinson M. Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. PLoS One. 2013;8:e82521. doi: 10.1371/journal.pone.0082521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Stringer KL, Onono M, Bukusi EA, Weiser SD, Cohen CR, Turan JM. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth. 2014;14:400. doi: 10.1186/s12884-014-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingum B, Roos A, Faure SC, Geerts L, Stein DJ. Risk factors for substance use in pregnant women in South Africa. S Afr Med J. 2012;102:851–854. doi: 10.7196/samj.5019. [DOI] [PubMed] [Google Scholar]
- Woldesenbet S, et al. Missed Opportunities along the Prevention of Mother-to-Child Transmission Services Cascade in South Africa: Uptake, Determinants, and Attributable Risk (the SAPMTCTE) PLoS One. 2015;10:e0132425. doi: 10.1371/journal.pone.0132425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. HIV and adolescents: guidance for HIV testing and counselling and care for adolescents living with HIV: recommendations for a public health approach and considerations for policy-makers and managers. 2013. [PubMed] [Google Scholar]


