Abstract
Mycoplasma pneumoniae pneumonia (MPP) is one of the most common forms of community-acquired pneumonia in children and adolescents. Outbreaks of MPP occur in 3- to 7-year cycles worldwide; recent epidemics in Korea occurred in 2006–2007, 2011, and 2015–2016. Although MPP is known to be a mild, self-limiting disease with a good response to macrolides, it can also progress into a severe and fulminant disease. Notably, since 2000, the prevalence of macrolide-resistant MPP has rapidly increased, especially in Asian countries, recently reaching up to 80%–90%. Macrolide-resistant Mycoplasma pneumoniae (MRMP) harbors a point mutation in domain V of 23S rRNA with substitutions mainly detected at positions 2063 and 2064 of the sequence. The excessive use of macrolides may contribute to these mutations. MRMP can lead to clinically refractory pneumonia, showing no clinical or radiological response to macrolides, and can progress to severe and complicated pneumonia. Refractory MPP is characterized by an excessive immune response against the pathogen as well as direct injury caused by an increasing bacterial load. A change of antibiotics is recommended to reduce the bacterial load. Tetracyclines or quinolones can be alternatives for treating MRMP. Otherwise, corticosteroid or intravenous immunoglobulin can be added to the treatment regimen as immunomodulators to down-regulate an excessive host immune reaction and alleviate immune-mediated pulmonary injury. However, the exact starting time point, dose, or duration of immunomodulators has not been established. This review focuses on the mechanism of resistance acquisition and treatment options for MRMP pneumonia.
Keywords: Mycoplasma pneumoniae, Pneumonia, Macrolides, Drug resistance, Child
Introduction
Mycoplasma pneumoniae is one of the most common pathogens causing community-acquired pneumonia (CAP) in children and adolescents, accounting for 10%–40% of all cases of CAP, and is substantially more common in children or adolescents than in adults. The recent epidemics in Korea occurred in 2006–2007, 2011, and 2015–2016, and the rate of macrolide-resistant Mycoplasma pneumoniae (MRMP) has been on the rise, with a rate of 14.7% in 2006, 51.6% in 2011, and reaching up to 84.6% in 20151,2,3,4). The rates of MRMP in Japan and China are similar to those in Korea5,6,7), whereas countries in North America and Europe reported an MRMP rate of only approximately 10%8). The high rates of MRMP may be associated with the excessive use of macrolides in Asian countries. Macrolide resistance is associated with point mutations in domain V of 23S rRNA5). The most common mutation is the A2063G transition, followed by the A2064G transition.
Macrolides have been traditionally used as first-line antibiotics in children with M. pneumoniae pneumonia (MPP) because of their low toxicity, low minimum inhibitory concentration (MIC), and no contraindications in children. The usual duration of treatment is recommended at 7–14 days with clarithromycin and 5 days with azithromycin8). Since MRMP pneumonia has more severe clinical outcomes such as a longer duration of fever, cough, and hospital days in addition to radiologic progression, second-line antibiotics or adjunctive immunomodulators are required. Tetracyclines such as doxycycline and minocycline or fluoroquinolones, primarily levofloxacin, can be used as alternative antibiotics in such cases6). However, tetracyclines and levofloxacin are not approved for use in children under 12 years old and under 18 years old, respectively, in Korea. Acquired resistance to tetracyclines and levofloxacin has not yet been reported1), although levofloxacin-resistant S. pneumoniae was isolated9).
The immunopathogenesis of the lung injury caused by MRMP is assumed to be related to an amplified host immune response such as cytokine overproduction and T-cell activation10). Accordingly, the use of immunomodulators such as corticosteroids or intravenous immunoglobulin (IVIG) can reduce the excessive host immune reaction and improve clinical outcomes11,12,13,14). However, the exact time point for the start, duration, or dose of immunomodulators has not been confirmed. This review focuses on the known mechanisms of resistance acquisition and treatment options of MRMP pneumonia.
Mechanisms of resistance acquisition and detection of macrolide resistance
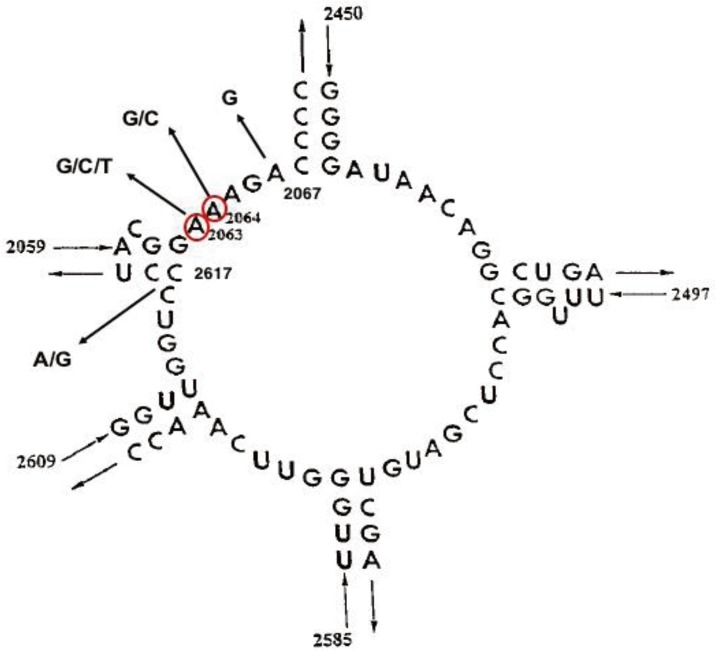
M. pneumoniae is intrinsically resistant to beta-lactams and other antibiotics targeting the bacterial cell wall due to the lack of a cell wall. Therefore, antibiotics that interfere with protein or DNA synthesis, such as macrolides, lincosamides, streptogramin combinations, and ketolides (MLSK), tetracyclines, and quinolones, have been used in clinical practice to treat M. pneumoniae infections. Among these antibiotics, macrolides act on the 50S ribosomal subunit of the bacterial ribosome to inhibit protein synthesis15). The site of peptide bond formation on the large 50S ribosomal subunit forms the central peptidyltransferase loop in domain V of 23S rRNA (Fig. 1)16). Nucleotides on the central loop are necessary for macrolides binding.
Fig. 1. Peptidyltransferase loop of domain V of 23S rRNA of Mycoplasma pneumoniae. Circled nucleotides indicate common mutated positions associated with macrolide resistance in clinical isolates. Adapted from Lucier et al. Antimicrob Agents Chemother 1995;39:2770-3, with permission of American Society for Microbiology16).
The most common mechanisms of macrolide resistance are efflux of the antibiotics (extrusion of the drug from the cell) and target site modification by a post-transcriptional modification of 23S rRNA or mutations in 23S rRNA or ribosomal proteins17). However, only target site modifications through mutations have been associated with macrolide resistance in M. pneumoniae to date18). Although resistance acquired through a target site mutation was detected for all three classes of antibiotics commonly used against M. pneumoniae in mutants selected in vitro, this mechanism of resistance has only been reported in clinical isolates for the MLSK antibiotics8).
Macrolide resistance has been associated with mutations at the sites 2063, 2064, 2067, and 2617 in domain V of the 23S rRNA sequence5,19,20). The A2063G transition is the most common mutation, followed by the A2064G transition5). Although mutations at positions A2067 and C2617 have also been linked to macrolide resistance, they are relatively rare. The resistance level to macrolides varies depending on the position at which the mutation occurs. Comparison of sequencing results with antimicrobial susceptibility testing confirmed that the A2063G and A2064G mutations conferred a high level of resistance to 14- and 15-membered macrolides. Although the A2063G mutation was related to an intermediate level of resistance to 16-membered macrolides, the A2067G transition conferred a high level of resistance to these antibiotics in a mutant selected in vitro (Fig. 1)21,22,23).
Mutations of genes encoding ribosomal proteins L4 and L22 have also been associated with low-level macrolide resistance in a mutant selected in vitro24). However, mutations in ribosomal proteins L4 and L22 have rarely been reported in clinical isolates.
To date, no cross-resistance has been observed between MLSK and other antibiotic classes used to treat M. pneumoniae. In addition, all clinical isolates with macrolide resistance were found to be susceptible to tetracyclines and fluoroquinolones.
To make better clinical decisions in the treatment of MPP, early detection of MRMP is necessary. However, antimicrobial susceptibility testing for M. pneumoniae requires a long period of time because M. pneumoniae is fastidious and slow growing. Therefore, various molecular methods for the rapid detection of MRMP from respiratory samples have been developed. In addition to conventional polymerase chain reaction (PCR) and sequencing of the 23S rRNA gene, PCR-restriction fragment length polymorphism, real-time PCR and high-resolution melt analysis, Cycleave PCR, and a single nucleotide polymorphism-PCR have been introduced to detect macrolide resistance25,26,27,28). Although there are no commercially available sensitive kits to detect MRMP, such kits are expected to become available soon and will be useful for the appropriate management of patients with MPP.
Clinical manifestation and laboratory findings
To date, data collected from patients with MRMP pneumonia suggest that the infection does not increase the severity of disease or the risk of complications in children3,7,29,30). That is, the clinical symptoms, laboratory and radiographic findings, and overall severity of pneumonia are generally similar between MRMP and macrolide-susceptible M. pneumoniae (MSMP) pneumonia.
However, the clinical efficacy of macrolide treatment tends to be lower in patients with MRMP pneumonia than in patients with MSMP pneumonia. Most patients with MRMP pneumonia show persistent signs and symptoms, with a prolonged duration of hospital stay and antibiotic administration compared with patients with MSMP pneumonia. In addition, recent reports demonstrated increased disease progression during therapy and complications in patients with MRMP pneumonia31,32). Surveillance data from Japan also showed that the number of patients requiring hospitalization has gradually increased along with the increase in the prevalence of MRMP pneumonia in children30). Overall, these studies raise the possibility that MRMP infection could increase the severity of pneumonia.
One reason for the inconsistency among previous studies regarding the impact of MRMP on clinical outcomes may be that patients with MRMP pneumonia had more persistent signs and symptoms, which led physicians to add an adjunctive treatment such as corticosteroids or to replace antibiotics to achieve more rapid clinical improvement. Another reason may be related to differences among the populations reported. Most previous studies included patients with moderate to severe disease who required hospitalization, which might lead to an overestimation of the general severity of MSMP pneumonia, assuming that the majority of patients with MSMP pneumonia would have been treated in an outpatient clinic rather than in hospital. Therefore, at this point, the clinical relevance of the increased prevalence of MRMP cannot be definitively established. Continuous surveillance of the influence of MRMP on disease outcome is necessary to better define its clinical relevance and to develop appropriate treatment strategies.
Treatment
1. Antibiotics
Given the rapid spread of macrolide resistance, alternative therapies without cross-resistance are urgently needed, particularly in children for whom macrolide resistance is more common, and tetracyclines and fluoroquinolones cannot be prescribed. Although a recent Cochrane review concluded that there is insufficient evidence on the efficacy of antibiotics for treating MPP in children, and MPP shows a self-limited course even without antibiotics33), macrolides are still recommended as the first-line antibiotics for treating M. pneumoniae infection because of their low toxicity in children. However, the widespread use and misuse of macrolides may cause the rapid emergence of MRMP19). The prevalence of MRMP is highest in Asia, where M. pneumoniae infections are highly prevalent overall, and MRMP may develop during macrolide treatment34). Because there are no appropriate treatment alternatives for children, reducing the indiscriminate abuse of macrolides will be the only key solution to prevent further pandemics of MRMP.
Determination of the MIC is important for establishing the inhibitory activity of an antimicrobial against DNA metabolism and protein synthesis. Macrolides, tetracyclines, and fluoroquinolones have the best MIC values against M. pneumoniae; however, the use of the latter 2 antibiotics is limited owing to concerns of several side effects35). Not all cases of MRMP infection require treatment with a second-line drug such as tetracyclines and fluoroquinolones; some patients could be treated with macrolides even in the presence of macrolide resistance36,37). Fever, which is the clinical decision point to evaluate the suseptibility for the first-line antibiotic, usually subsides within 48–72 hours after treatment in an individual infected with a macrolide-sensitive strain. If the clinical symptoms do not improve within 48–72 hours with the first-line antibiotics, a change to the second-line antibiotics is recommended6). The Pediatric Infectious Diseases Society and the Infectious Diseases Society of America recommend azithromycin as the first-line antibiotic, and clarithromycin, erythromycin (not available in Korea), doxycycline (for children aged ≥8 years), levofloxacin, or moxifloxacin (for adolescents) as the second-line antibiotics38). The Japanese Society of Pediatric Pulmonology, Japanese Society for Pediatric Infectious Disease, Japan Pediatric Society, and Japanese Society of Mycoplasmology recommend macrolides as the first-line drug, and tosufloxacin or tetracyclines as the second-line drugs6).
In Korea, tetracycline is not approved for use in children under 12 years old and can be cautiously used in 8- to 11-year-old children only when there are no alternative antibiotics available.
2. Tetracyclines
Doxycycline, minocycline, oxytetracycline, tetracycline, and tigecycline are the currently available Korean Food and Drug Administration (FDA)-approved tetracyclines. However, none of these drugs has been approved by the Korean FDA for children under 12 years old. The biological action of tetracyclines resides in their inhibitory activity against protein synthesis. Tooth discoloration, gastrointestinal disturbances, photosensitivity, and hepatotoxicity are the most common adverse drug reactions of tetracyclines. The degree of tooth discoloration is known to be dependent on the dose per body weight, duration of use, and stage of tooth development39). Since the calcification of permanent teeth is completed before 7–8 years of age40), this is the main rationale for the prohibition of its use in children under 8 years of age.
Among tetracyclines, minocycline is associated with greater adverse reactions in the bone, central nervous system, and skin than the others41). In particular, the generation of black bones in the oral cavity is one of the most remarkable side effects of minocycline39). Minocycline is not approved in the United States or in the European Union. However, it is the only approved tetracycline in Japan6). To date, only 2 clinical trials have evaluated the efficacy of minocycline in children with MRMP. Although both were non-randomized trials and did not release a safety report, they reported the excellent efficacy of minocycline treatment42,43). A retrospective study on the effectiveness of doxycycline showed that it was more effective than macrolide treatment. The records of a total of 48 children with MPP were reviewed in this study. Among them, 19 children (16 in the MRMP group and 3 in the MSMP group) who were treated with doxycycline showed a faster time to defervescence44). Even though doxycycline is known to cause tooth discoloration due to the low binding affinity to calcium45), one observational study reported an absence of tooth staining with a short course of doxycycline in children under 8 years of age46). Analysis of the pathogens responsible for the MRMP epidemics during 2000–2011 in Korea showed a significantly higher MIC for 50% of the strains and MIC90 for macrolides. However, all of the strains were susceptible to the second-line drugs, including tetracycline, doxycycline, levofloxacin, ciprofloxacin, and moxifloxacin1). In Korea, the needs for second-line antibiotics are increasing. Fortunately, advances in dental care techniques can now allow for the use of tetracyclines in children with severe MRMP with reduced concern about tooth discoloration.
3. Fluoroquinolones
Ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, norfloxacin, ofloxacin, and tosufloxacin are the currently available Korean FDA-approved fluoroquinolones. None of these drugs has been approved by the Korean FDA for children under 18 years old. A recent systematic review on the safety of ciprofloxacin in children reported a frequency of 1.6% musculoskeletal adverse events47). Levofloxacin has been referred to as a respiratory fluoroquinolone owing to its excellent activity against many respiratory bacteria such as Streptococcus pneumoniae and Mycoplasma pneumoniae. However, the results of levofloxacin-related adverse risks are inconsistent48,49), and there is a lack of information on its safety in children. On May 12, 2016, the U.S. FDA advised restricting fluoroquinolone antibiotic use for treating certain uncomplicated infections because of the occurrence of serious adverse reactions such as tendinitis, tendon rupture, worsening of myasthenia gravis, risk of peripheral neuropathy and central nervous system effects, and dermatologic, cardiac, and hypersensitivity reactions50). In addition, the black box warning (FDA's strongest warning) was updated on July 26, 2016 for all oral and injectable fluoroquinolone antibiotics given the disabling and potentially permanent side effects on the tendon, muscle, joints, nerves, and central nervous system51). In particular, they emphasized that “the risk of these serious side effects (of fluoroquinolones) generally outweighs the benefits for patients with acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections, and should be reserved for those who do not have alternative treatment options.” However, they also announced that for some serious bacterial infections, the benefits of fluoroquinolones outweigh the risks and it is appropriate for them to remain available as a therapeutic option. Among the fluoroquinolones, levofloxacin and ofloxacin seem to be associated with a higher risk of causing tendon damage than the other fluoroquinolones, and the tendinitis risk seems to be dependent on the dose and duration of use52). Therefore, prescribing physicians should be aware of balancing the relative risks and benefits associated with fluoroquinolones, and their use in children should be limited to the treatment of life-threatening infections without alternative therapeutic options.
To date, no tetracycline and fluoroquinolone resistance has been reported in cases of MRMP. However, clinicians should be aware of the possibility of second-line drug resistance.
4. Corticosteroid therapy and IVIG
Approximately 0.5%–2% of MPP cases progress to the fulminant type of pneumonia, including fatal respiratory failure, which is most prevalent in adolescents. To date, there is no specific biomarker to predict the progression of fulminant MPP; thus, the treatment strategy largely depends on close observation and the clinician's experience. Although there is no clear guideline yet, systemic corticosteroid or IVIG is considered to be a reasonable treatment option53). Recent evidence shows that the severity of M. pneumoniae infections is largely dependent on the host immune response; thus, use of an immunomodulator such as corticosteroids and IVIG should be considered in the treatment of severe M. pneumoniae infections, regardless of macrolide resistance11,54,55).
Although there are no guidelines put forward for corticosteroid treatment in severe MRMP to date, numerous studies have reported the efficacy of corticosteroids in the treatment of severe MRMP11,12,13,54,56). Unfortunately, the indication, time, dose, and duration of corticosteroids remain unclear. The dose varies from oral prednisolone at 1 mg/kg/day to intravenous methylprednisolone at 30 mg/kg/day for 3 days. Long-lasting fever and a serum lactate dehydrogenase level of ≥480 IU/L are known indications of effective corticosteroid therapy57). A recent randomized controlled study showed that methylprednisolone (2 mg/kg/day for 3 days) and IVIG (400 mg/kg/day for 3 days) therapy in children with refractory MPP who had a fever for at least 7 days or persistent consolidation of more than one lobe despite appropriate macrolides could significantly reduce the fever duration, resorption of atelectasis, and pleural effusion compared to treatment with azithromycin alone12).
IVIG has been used as an immunomodulator in the treatment of immune-mediated diseases. Several studies reported the efficacy of IVIG for severe MPP in children12,58,59). Besides fulminant MPP, there are numerous reports showing that IVIG therapy was effective in treating hemophagocytic syndrome, encephalitis, myocarditis complicated with complete heart block, cold agglutinin-related severe hemolytic anemia, mucositis, Stevens-Johnson syndrome, and acquired hemophilia58,60,61,62).
To date, many studies have reported the efficacy of corticosteroid therapy in refractory MPP. A recent randomized controlled trial showed that early adjunct corticosteroid treatment shortened the time to clinical stability in CAP63). In addition, recent studies reported the efficacy and effectiveness of an early systemic immunomodulator (corticosteroids and/or IVIG) in the treatment of MRMP12,14). The severity and chronicity of infection-associated respiratory disease largely depends on the interaction between the respiratory pathogen and host immune response; thus, early treatment of a systemic immunomodulator to reduce aberrant immune responses in the potential stage of acute respiratory distress syndrome was emphasized64). Nevertheless, there is still controversy related to the optimal timing of immunomodulatory therapy.
Prognosis and complications
Progression and severe complications are hypothesized to result from delayed diagnosis and treatment, macrolide resistance, coinfections with other microorganisms, or host hyper-immune responses53). Initial signs and symptoms cannot generally distinguish MRMP from MSMP. Cases of MRMP tend to show more persistent symptoms, including long-lasting fever, coughing, subsequent longer hospitalization, and the longer use of antibiotics or change to the second-line antibiotics. However, MRMP was not related to more rapid progression or severe complications than MSMP8). By contrast, recent studies reported that MRMP showed more rapid progression31) and a higher incidence of extrapulmonary complications than MSMP32).
MRMP can be associated with serious intra- or extrapulmonary complications, including pleural effusion, bronchiolitis obliterans, atelectasis, or acute respiratory distress syndrome as the intrapulmonary complications53,65). Extrapulmonary complications vary from mild cases such as elevated levels of liver and pancreatic enzymes, rash, proteinuria, arthritis, and vestibular neuritis to more severe complications such as myocarditis, Stevens-Johnson syndrome, erythema multiforme, hemolytic anemia, hemophagocytic syndrome, encephalitis, transverse myelitis, Guillain-Barré syndrome, or cerebellitis55).
There are currently 3 therapeutic options for treating MRMP pneumonia. If patients have only persistent fever and coughing without respiratory difficulties or complications, only maintenance on first-line antibiotics and supportive care are required. If patients have respiratory difficulties, progressive consolidation, or complications, a change to second-line antibiotics and/or the addition of immunomodulators are recommended.
Conclusions
Since 2000, the rates of MRMP pneumonia have rapidly increased, especially in Asian countries where M. pneumoniae infections are highly prevalent. The excessive use of macrolides may contribute to the higher prevalence of MRMP in Asian countries. MRMP can develop during the course of macrolide treatment within an individual patient. Point mutations of 23S rRNA in the region of sites 2063 and 2064 are the most common mechanisms of MRMP. Tetracycline and levofloxacin can be alternative antibiotics for treating MRMP pneumonia, and no resistant strains have been reported to date. However, tetracyclines are not approved for children under 12 years old, and levofloxacin is not approved for children under 18 years of age in Korea. In addition, only a single rRNA of M. pneumonia can increase the possibility of mutation to alternative antibiotics. Excessive host immunity can contribute to refractory MPP; in such cases, immunomodulators such as corticosteroids or IVIG can be added to reduce the immune reaction in refractory MPP. Corticosteroids can attenuate inflammatory reaction associated with MRMP pneumonia. However, determination of the exact timing, duration, and dose of immunomodulators needs further study. Overuse or misuse of antibiotics should be restricted to reduce further acquisition of resistance in MPP.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Hong KB, Choi EH, Lee HJ, Lee SY, Cho EY, Choi JH, et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000-2011. Emerg Infect Dis. 2013;19:1281–1284. doi: 10.3201/eid1908.121455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoo SJ, Kim HB, Choi SH, Lee SO, Kim SH, Hong SB, et al. Differences in the frequency of 23S rRNA gene mutations in Mycoplasma pneumoniae between children and adults with community-acquired pneumonia: clinical impact of mutations conferring macrolide resistance. Antimicrob Agents Chemother. 2012;56:6393–6396. doi: 10.1128/AAC.01421-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seo YH, Kim JS, Seo SC, Seo WH, Yoo Y, Song DJ, et al. Predictive value of C-reactive protein in response to macrolides in children with macrolide-resistant Mycoplasma pneumoniae pneumonia. Korean J Pediatr. 2014;57:186–192. doi: 10.3345/kjp.2014.57.4.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim EK, Youn YS, Rhim JW, Shin MS, Kang JH, Lee KY. Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J Pediatr. 2015;58:172–177. doi: 10.3345/kjp.2015.58.5.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morozumi M, Takahashi T, Ubukata K. Macrolide-resistant Mycoplasma pneumoniae: characteristics of isolates and clinical aspects of community-acquired pneumonia. J Infect Chemother. 2010;16:78–86. doi: 10.1007/s10156-009-0021-4. [DOI] [PubMed] [Google Scholar]
- 6.Yamazaki T, Kenri T. Epidemiology of Mycoplasma pneumoniae infections in Japan and therapeutic strategies for macrolide-resistant M. pneumoniae. Front Microbiol. 2016;7:693. doi: 10.3389/fmicb.2016.00693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu PS, Chang LY, Lin HC, Chi H, Hsieh YC, Huang YC, et al. Epidemiology and clinical manifestations of children with macrolide-resistant Mycoplasma pneumoniae pneumonia in Taiwan. Pediatr Pulmonol. 2013;48:904–911. doi: 10.1002/ppul.22706. [DOI] [PubMed] [Google Scholar]
- 8.Pereyre S, Goret J, Bébéar C. Mycoplasma pneumoniae: current knowledge on macrolide resistance and treatment. Front Microbiol. 2016;7:974. doi: 10.3389/fmicb.2016.00974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmitz J, van der Linden M, Al-Lahham A, Levina N, Pletz MW, Imohl M. Fluoroquinolone resistance in Streptococcus pneumoniae isolates in Germany from 2004-2005 to 2014-2015. Int J Med Microbiol. 2017 Apr 19; doi: 10.1016/j.ijmm.2017.04.003. [Epub] [DOI] [PubMed] [Google Scholar]
- 10.Youn YS, Lee KY. Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2012;55:42–47. doi: 10.3345/kjp.2012.55.2.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luo Z, Luo J, Liu E, Xu X, Liu Y, Zeng F, et al. Effects of prednisolone on refractory mycoplasma pneumoniae pneumonia in children. Pediatr Pulmonol. 2014;49:377–380. doi: 10.1002/ppul.22752. [DOI] [PubMed] [Google Scholar]
- 12.Shan LS, Liu X, Kang XY, Wang F, Han XH, Shang YX. Effects of methylprednisolone or immunoglobulin when added to standard treatment with intravenous azithromycin for refractory Mycoplasma pneumoniae pneumonia in children. World J Pediatr. 2017 Jan; doi: 10.1007/s12519-017-0014-9. Epub. [DOI] [PubMed] [Google Scholar]
- 13.Miyashita N, Kawai Y, Inamura N, Tanaka T, Akaike H, Teranishi H, et al. Setting a standard for the initiation of steroid therapy in refractory or severe Mycoplasma pneumoniae pneumonia in adolescents and adults. J Infect Chemother. 2015;21:153–160. doi: 10.1016/j.jiac.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Youn YS, Lee SC, Rhim JW, Shin MS, Kang JH, Lee KY. Early additional immune-modulators for Mycoplasma pneumoniae pneumonia in children: an observation study. Infect Chemother. 2014;46:239–247. doi: 10.3947/ic.2014.46.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaynor M, Mankin AS. Macrolide antibiotics: binding site, mechanism of action, resistance. Curr Top Med Chem. 2003;3:949–961. doi: 10.2174/1568026033452159. [DOI] [PubMed] [Google Scholar]
- 16.Lucier TS, Heitzman K, Liu SK, Hu PC. Transition mutations in the 23S rRNA of erythromycin-resistant isolates of Mycoplasma pneumoniae. Antimicrob Agents Chemother. 1995;39:2770–2773. doi: 10.1128/aac.39.12.2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leclercq R. Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002;34:482–492. doi: 10.1086/324626. [DOI] [PubMed] [Google Scholar]
- 18.Bébéar CM, Pereyre S. Mechanisms of drug resistance in Mycoplasma pneumoniae. Curr Drug Targets Infect Disord. 2005;5:263–271. doi: 10.2174/1568005054880109. [DOI] [PubMed] [Google Scholar]
- 19.Bébéar C, Pereyre S, Peuchant O. Mycoplasma pneumoniae: susceptibility and resistance to antibiotics. Future Microbiol. 2011;6:423–431. doi: 10.2217/fmb.11.18. [DOI] [PubMed] [Google Scholar]
- 20.Principi N, Esposito S. Macrolide-resistant Mycoplasma pneumoniae: its role in respiratory infection. J Antimicrob Chemother. 2013;68:506–511. doi: 10.1093/jac/dks457. [DOI] [PubMed] [Google Scholar]
- 21.Cardinale F, Chironna M, Dumke R, Binetti A, Daleno C, Sallustio A, et al. Macrolide-resistant Mycoplasma pneumoniae in paediatric pneumonia. Eur Respir J. 2011;37:1522–1524. doi: 10.1183/09031936.00172510. [DOI] [PubMed] [Google Scholar]
- 22.Xin D, Mi Z, Han X, Qin L, Li J, Wei T, et al. Molecular mechanisms of macrolide resistance in clinical isolates of Mycoplasma pneumoniae from China. Antimicrob Agents Chemother. 2009;53:2158–2159. doi: 10.1128/AAC.01563-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akaike H, Miyashita N, Kubo M, Kawai Y, Tanaka T, Ogita S, et al. In vitro activities of 11 antimicrobial agents against macrolide-resistant Mycoplasma pneumoniae isolates from pediatric patients: results from a multicenter surveillance study. Jpn J Infect Dis. 2012;65:535–538. doi: 10.7883/yoken.65.535. [DOI] [PubMed] [Google Scholar]
- 24.Pereyre S, Guyot C, Renaudin H, Charron A, Bébéar C, Bébéar CM. In vitro selection and characterization of resistance to macrolides and related antibiotics in Mycoplasma pneumoniae. Antimicrob Agents Chemother. 2004;48:460–465. doi: 10.1128/AAC.48.2.460-465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsuoka M, Narita M, Okazaki N, Ohya H, Yamazaki T, Ouchi K, et al. Characterization and molecular analysis of macrolide-resistant Mycoplasma pneumoniae clinical isolates obtained in Japan. Antimicrob Agents Chemother. 2004;48:4624–4630. doi: 10.1128/AAC.48.12.4624-4630.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peuchant O, Ménard A, Renaudin H, Morozumi M, Ubukata K, Bébéar CM, et al. Increased macrolide resistance of Mycoplasma pneumoniae in France directly detected in clinical specimens by real-time PCR and melting curve analysis. J Antimicrob Chemother. 2009;64:52–58. doi: 10.1093/jac/dkp160. [DOI] [PubMed] [Google Scholar]
- 27.Liu Y, Ye X, Zhang H, Wu Z, Xu X. Rapid detection of Mycoplasma pneumoniae and its macrolide-resistance mutation by Cycleave PCR. Diagn Microbiol Infect Dis. 2014;78:333–337. doi: 10.1016/j.diagmicrobio.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Ji M, Lee NS, Oh JM, Jo JY, Choi EH, Yoo SJ, et al. Single-nucleotide polymorphism PCR for the detection of Mycoplasma pneumoniae and determination of macrolide resistance in respiratory samples. J Microbiol Methods. 2014;102:32–36. doi: 10.1016/j.mimet.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Matsubara K, Morozumi M, Okada T, Matsushima T, Komiyama O, Shoji M, et al. A comparative clinical study of macrolide-sensitive and macrolide-resistant Mycoplasma pneumoniae infections in pediatric patients. J Infect Chemother. 2009;15:380–383. doi: 10.1007/s10156-009-0715-7. [DOI] [PubMed] [Google Scholar]
- 30.Morozumi M, Iwata S, Hasegawa K, Chiba N, Takayanagi R, Matsubara K, et al. Increased macrolide resistance of Mycoplasma pneumoniae in pediatric patients with community-acquired pneumonia. Antimicrob Agents Chemother. 2008;52:348–350. doi: 10.1128/AAC.00779-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheong KN, Chiu SS, Chan BW, To KK, Chan EL, Ho PL. Severe macrolide-resistant Mycoplasma pneumoniae pneumonia associated with macrolide failure. J Microbiol Immunol Infect. 2016;49:127–130. doi: 10.1016/j.jmii.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Zhou Y, Zhang Y, Sheng Y, Zhang L, Shen Z, Chen Z. More complications occur in macrolide-resistant than in macrolide-sensitive Mycoplasma pneumoniae pneumonia. Antimicrob Agents Chemother. 2014;58:1034–1038. doi: 10.1128/AAC.01806-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gardiner SJ, Gavranich JB, Chang AB. Antibiotics for community-acquired lower respiratory tract infections secondary to Mycoplasma pneumoniae in children. Cochrane Database Syst Rev. 2015;1:CD004875. doi: 10.1002/14651858.CD004875.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hantz S, Garnier F, Peuchant O, Menetrey C, Charron A, Ploy MC, et al. Multilocus variable-number tandem-repeat analysis-confirmed emergence of a macrolide resistance-associated mutation in Mycoplasma pneumoniae during macrolide therapy for interstitial pneumonia in an immunocompromised child. J Clin Microbiol. 2012;50:3402–3405. doi: 10.1128/JCM.01248-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spuesens EB, Meyer Sauteur PM, Vink C, van Rossum AM. Mycoplasma pneumoniae infections--does treatment help? J Infect. 2014;69(Suppl 1):S42–S46. doi: 10.1016/j.jinf.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 36.Li S, Sun H, Liu F, Feng Y, Zhao H, Xue G, et al. Two case reports: whole genome sequencing of two clinical macrolide-resistant Mycoplasma pneumoniae isolates with different responses to azithromycin. Medicine (Baltimore) 2016;95:e4963. doi: 10.1097/MD.0000000000004963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cardinale F, Chironna M, Chinellato I, Principi N, Esposito S. Clinical relevance of Mycoplasma pneumoniae macrolide resistance in children. J Clin Microbiol. 2013;51:723–724. doi: 10.1128/JCM.02840-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25–e76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sánchez AR, Rogers RS, 3rd, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol. 2004;43:709–715. doi: 10.1111/j.1365-4632.2004.02108.x. [DOI] [PubMed] [Google Scholar]
- 40.Jackson R. Tetracycline staining of wisdom teeth. Cutis. 1979;23:613–616. [PubMed] [Google Scholar]
- 41.Carris NW, Pardo J, Montero J, Shaeer KM. Minocycline as A substitute for doxycycline in targeted scenarios: a systematic review. Open Forum Infect Dis. 2015;2:ofv178. doi: 10.1093/ofid/ofv178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Okada T, Morozumi M, Tajima T, Hasegawa M, Sakata H, Ohnari S, et al. Rapid effectiveness of minocycline or doxycycline against macrolide-resistant Mycoplasma pneumoniae infection in a 2011 outbreak among Japanese children. Clin Infect Dis. 2012;55:1642–1649. doi: 10.1093/cid/cis784. [DOI] [PubMed] [Google Scholar]
- 43.Kawai Y, Miyashita N, Kubo M, Akaike H, Kato A, Nishizawa Y, et al. Therapeutic efficacy of macrolides, minocycline, and tosufloxacin against macrolide-resistant Mycoplasma pneumoniae pneumonia in pediatric patients. Antimicrob Agents Chemother. 2013;57:2252–2258. doi: 10.1128/AAC.00048-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lung DC, Yip EK, Lam DS, Que TL. Rapid defervescence after doxycycline treatment of macrolide-resistant Mycoplasma pneumoniae-associated community-acquired pneumonia in children. Pediatr Infect Dis J. 2013;32:1396–1399. doi: 10.1097/INF.0b013e3182a25c71. [DOI] [PubMed] [Google Scholar]
- 45.Forti G, Benincori C. Doxycycline and the teeth. Lancet. 1969;1:782. doi: 10.1016/s0140-6736(69)91787-5. [DOI] [PubMed] [Google Scholar]
- 46.Volovitz B, Shkap R, Amir J, Calderon S, Varsano I, Nussinovitch M. Absence of tooth staining with doxycycline treatment in young children. Clin Pediatr (Phila) 2007;46:121–126. doi: 10.1177/0009922806290026. [DOI] [PubMed] [Google Scholar]
- 47.Adefurin A, Sammons H, Jacqz-Aigrain E, Choonara I. Ciprofloxacin safety in paediatrics: a systematic review. Arch Dis Child. 2011;96:874–880. doi: 10.1136/adc.2010.208843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bradley JS, Kauffman RE, Balis DA, Duffy CM, Gerbino PG, Maldonado SD, et al. Assessment of musculoskeletal toxicity 5 years after therapy with levofloxacin. Pediatrics. 2014;134:e146–e153. doi: 10.1542/peds.2013-3636. [DOI] [PubMed] [Google Scholar]
- 49.Noel GJ, Bradley JS, Kauffman RE, Duffy CM, Gerbino PG, Arguedas A, et al. Comparative safety profile of levofloxacin in 2523 children with a focus on four specific musculoskeletal disorders. Pediatr Infect Dis J. 2007;26:879–891. doi: 10.1097/INF.0b013e3180cbd382. [DOI] [PubMed] [Google Scholar]
- 50.FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together [Internet] Silver Spring (MD): U.S. Food and Drug Administration; 2017. [updated 2017 May 24]. [cited 2017 Feb 20]. Available from: http://www.fda.gov/Drugs/DrugSafety/ucm500143.htm 2016. [Google Scholar]
- 51.Park HY, Lee H, Koh WJ, Kim S, Jeong I, Koo HK, et al. Association of blood eosinophils and plasma periostin with FEV1 response after 3-month inhaled corticosteroid and long-acting beta2-agonist treatment in stable COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;11:23–30. doi: 10.2147/COPD.S94797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bidell MR, Lodise TP. Fluoroquinolone-associated tendinopathy: does levofloxacin pose the greatest risk? Pharmacotherapy. 2016;36:679–693. doi: 10.1002/phar.1761. [DOI] [PubMed] [Google Scholar]
- 53.Izumikawa K. Clinical features of severe or fatal Mycoplasma pneumoniae Pneumonia. Front Microbiol. 2016;7:800. doi: 10.3389/fmicb.2016.00800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.You SY, Jwa HJ, Yang EA, Kil HR, Lee JH. Effects of methylprednisolone pulse therapy on refractory Mycoplasma pneumoniae Pneumonia in Children. Allergy Asthma Immunol Res. 2014;6:22–26. doi: 10.4168/aair.2014.6.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Narita M. Classification of extrapulmonary manifestations due to Mycoplasma pneumoniae infection on the basis of possible pathogenesis. Front Microbiol. 2016;7:23. doi: 10.3389/fmicb.2016.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang L, Gao X, Chen M. Early treatment with corticosteroids in patients with Mycoplasma pneumoniae pneumonia: a randomized clinical trial. J Trop Pediatr. 2014;60:338–342. doi: 10.1093/tropej/fmu022. [DOI] [PubMed] [Google Scholar]
- 57.Oishi T, Narita M, Matsui K, Shirai T, Matsuo M, Negishi J, et al. Clinical implications of interleukin-18 levels in pediatric patients with Mycoplasma pneumoniae pneumonia. J Infect Chemother. 2011;17:803–806. doi: 10.1007/s10156-011-0265-7. [DOI] [PubMed] [Google Scholar]
- 58.Bressan S, Mion T, Andreola B, Bisogno G, Da Dalt L. Severe Mycoplasma pneumoniae-associated mucositis treated with immunoglobulins. Acta Paediatr. 2011;100:e238–e240. doi: 10.1111/j.1651-2227.2011.02342.x. [DOI] [PubMed] [Google Scholar]
- 59.Shen Y, Zhang J, Hu Y, Shen K. Combination therapy with immune -modulators and moxifloxacin on fulminant macrolide-resistant Mycoplasma pneumoniae infection: a case report. Pediatr Pulmonol. 2013;48:519–522. doi: 10.1002/ppul.22650. [DOI] [PubMed] [Google Scholar]
- 60.Chambert-Loir C, Ouachee M, Collins K, Evrard P, Servais L. Immediate relief of Mycoplasma pneumoniae encephalitis symptoms after intravenous immunoglobulin. Pediatr Neurol. 2009;41:375–377. doi: 10.1016/j.pediatrneurol.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 61.Manwani NS, Balasubramanian S, Dhanalakshmi K, Sumanth A. Stevens Johnson syndrome in association with Mycoplasma pneumonia. Indian J Pediatr. 2012;79:1097–1099. doi: 10.1007/s12098-011-0591-x. [DOI] [PubMed] [Google Scholar]
- 62.Ahluwalia J, Wan J, Lee DH, Treat J, Yan AC. Mycoplasma-associated Stevens-Johnson syndrome in children: retrospective review of patients managed with or without intravenous immunoglobulin, systemic corticosteroids, or a combination of therapies. Pediatr Dermatol. 2014;31:664–669. doi: 10.1111/pde.12481. [DOI] [PubMed] [Google Scholar]
- 63.Blum CA, Nigro N, Briel M, Schuetz P, Ullmer E, Suter-Widmer I, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2015;385:1511–1518. doi: 10.1016/S0140-6736(14)62447-8. [DOI] [PubMed] [Google Scholar]
- 64.Lee KY. Pneumonia, acute respiratory distress syndrome, and early immune-modulator therapy. Int J Mol Sci. 2017;18(2):pii: E388. doi: 10.3390/ijms18020388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chaabane N, Coupez E, Buscot M, Souweine B. Acute respiratory distress syndrome related to Mycoplasma pneumoniae infection. Respir Med Case Rep. 2016;20:89–91. doi: 10.1016/j.rmcr.2016.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]