Abstract
Secular trends in blood pressure (BP) and body mass index (BMI) during childhood and adolescence are sentinels for the future population cardiovascular disease burden. We examined trends in BP z-score (ages 9–18 years from 1999 to 2014) and BMI z-score (ages 6–18 years from 1996 to 2014) in Hong Kong, China. Overall, BP z-score fell, systolic BP from 0.08 to −0.01 in girls and from 0.31 to 0.25 in boys. However, the trends were not consistent, for both sexes, systolic BP z-score was stable from 1999, decreased slightly from 2002 to 2005 and increased slightly to 2014, diastolic BP z-score decreased slightly from 1999 to 2004 and then remained stable to 2014. In contrast, BMI z-score rose from −0.15 to −0.01 in girls and from 0.14 to 0.34 in boys, mainly during 1997 to 2010. The upper tail of the systolic (except boys) and diastolic BP distribution shifted downwards, whereas the entire BMI distribution shifted upward. BP declined slightly whereas BMI rose in Hong Kong children and adolescents during the last 20 years, with systolic BP and BMI in boys above the reference. This warrants dual action in tackling rising BMI and identifying favorable determinants of BP, particularly targeting boys.
Introduction
Secular trends in blood pressure (BP) and body mass index (BMI) during childhood and adolescence are key global cardiovascular health surveillance indicators. In many long-term developed Western countries, adult systolic BP has decreased since the 1980s1, whereas adult BMI has monotonically increased2. These trends are congruent with declining haemorrhagic stroke but increasing ischemic stroke3 given lower BP particularly reduces haemorrhagic stroke1 while higher BMI promotes the atherosclerosis implicated in ischemic stroke4. In children and adolescents in long-term developed Western populations, declining BP has been documented since the mid-20th century5, followed by a rise from the mid-1980s in the United Kingdom6 and from the early 1990s in the United States7. A monotonic rise in BMI has occurred since the 1960s8, suggesting trends in BP and BMI during childhood and adolescence foreshadow changes in patterns of adult cardiovascular diseases5.
Secular trends in cardiovascular disease, and its drivers, in non-Western settings are more varied. For example, over the last 20 years, BP has increased since the mid-1990s in China9, 10, but recently declined in the Seychelles11 and systolic, but not diastolic, BP has clearly declined in South Korea12. BMI has increased in China13, the Seychelles11, and also in South Korea12. In short, BMI has been generally increasing in children and adolescents in most non-Western populations. Conversely, with longer experience of economic transition, BP tends to decline, as in developed Western settings, but systolic and diastolic BP trends may differ14.
The observed contrasting trends in BMI and BP in early life with economic development could underlie and inform the observed contrasting trends in cardiovascular disease mortality, which are poorly understood15, however these contrasting trends could also be artifacts of sampling at different ages and developmental stages16, secular increases in height14, small samples and few time points17. Hong Kong is an ethnically homogeneous Chinese population with a different social and economic history from the rest of China18. Children and adolescents today in Hong Kong represent the first generation of Chinese to grow up in a post-industrial Chinese setting with living standards and social infrastructure similar to Western Europe, but a much more rapid trajectory of economic development19, which might also have consequences for current patterns of disease20. This raises the question as to whether trends in BP and BMI in Hong Kong would be similar to currently rapidly developing China, or other recently developed non-Western countries, or to Western countries with a longer history of economic development. To address this question, we examined trends in BP at ages 9–18 years from 1999 to 2014 and BMI at 6–18 years from 1996 to 2014 in Hong Kong, where population-representative information on BMI and BP for school age children and adolescents is available.
Results
A total of 402,040 children and adolescents aged 9–18 years contributed to BP measurements from 1999 to 2014 and 1,898,816 aged 6–18 years contributed BMI measurements from 1996 to 2014. Table 1 shows mean age- and height-standardized systolic BP z-score decreased from 0.08 in 1999 to −0.01 in 2014 for girls and from 0.31 to 0.25 for boys. Diastolic BP decreased from −0.12 to −0.22 for girls and from −0.03 to −0.13 for boys. Concomitantly, the proportion with pre-hypertensive BP or hypertensive BP decreased from 18.3% to 9.9% in girls and from 30.6% to 26.4% in boys. In contrast, Table 2 shows mean age-standardized BMI z-score increased from −0.15 in 1996 to −0.01 in 2014 for girls and from 0.14 to 0.34 for boys. Correspondingly, the proportion of overweight or obesity also increased from 13.2% to 14.0% for girls and from 19.0% to 22.4% for boys. Table 3 shows the mean difference in age- and height-standardized systolic BP z-score was −0.006 per year in girls and −0.004 in boys and for diastolic BP was −0.002 in both sexes (model 1). The age-standardized BMI z-score was higher by 0.016 per year in girls and 0.022 in boys. Comparing the changes in BP z-score with BMI z-score over time (from an interaction term between BMI z-score and calendar year) in a regression of BP z-score on BM z-score, the positive coefficient for interaction suggests the association of BP z-score with BMI z-score was stronger over time (model 2).
Table 1.
Age- and Height-Adjusted Systolic and Diastolic Blood Pressure (BP), Age-Standardized Systolic and Diastolic BP,a Age- and Height-Standardized Systolic and Diastolic BP Z-scoresb and Proportion of Prehypertensive BP and Hypertensive BPc Among 196,299 Boys and 205,741 Girls Aged 9 to 18 From 1999 to 2014 in Hong Kong.
| Year | n | % | Age- and height-adjusted | Age- standardized | Age- and height-standardized | Prehypertensive BP | Hypertensive BP | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Systolic BP (mmHg) | Diastolic BP (mmHg) | Systolic BP (mmHg) | Diastolic BP (mmHg) | Systolic BP z-score | Diastolic BP z-score | |||||||||||
| Mean | SD | Mean | SD | Mean | SE | Mean | SE | Mean | SD | Mean | SD | % | % | |||
| Boys | ||||||||||||||||
| 1999 | 9,001 | 4.59 | 110.5 | 8.2 | 61.0 | 2.6 | 110.1 | 0.4 | 61.9 | 0.2 | 0.31 | 1.04 | −0.03 | 0.65 | 21.9 | 8.7 |
| 2000 | 12,073 | 6.15 | 109.6 | 8.1 | 60.7 | 2.5 | 110.2 | 0.3 | 61.3 | 0.2 | 0.37 | 1.05 | −0.10 | 0.58 | 17.7 | 12.1 |
| 2001 | 11,778 | 6.00 | 109.5 | 7.9 | 60.7 | 2.4 | 110.6 | 0.3 | 60.9 | 0.2 | 0.35 | 1.08 | −0.15 | 0.58 | 16.6 | 12.9 |
| 2002 | 12,471 | 6.35 | 109.3 | 7.8 | 60.6 | 2.4 | 110.6 | 0.3 | 61.1 | 0.2 | 0.35 | 1.06 | −0.13 | 0.56 | 16.2 | 12.8 |
| 2003 | 11,070 | 5.64 | 109.5 | 7.9 | 60.6 | 2.4 | 109.6 | 0.4 | 60.4 | 0.2 | 0.24 | 1.09 | −0.18 | 0.58 | 15.3 | 11.0 |
| 2004 | 12,357 | 6.29 | 109.6 | 7.8 | 60.7 | 2.4 | 108.7 | 0.3 | 60.0 | 0.2 | 0.16 | 1.04 | −0.21 | 0.57 | 15.9 | 8.0 |
| 2005 | 12,406 | 6.32 | 109.5 | 7.7 | 60.6 | 2.4 | 108.0 | 0.4 | 59.7 | 0.2 | 0.12 | 1.01 | −0.24 | 0.54 | 16.4 | 6.4 |
| 2006 | 13,224 | 6.74 | 110.0 | 7.7 | 60.8 | 2.4 | 109.1 | 0.3 | 60.7 | 0.2 | 0.17 | 0.99 | −0.19 | 0.52 | 17.5 | 6.4 |
| 2007 | 13,408 | 6.83 | 110.1 | 7.7 | 60.8 | 2.4 | 108.9 | 0.4 | 60.5 | 0.2 | 0.20 | 1.01 | −0.18 | 0.52 | 18.2 | 7.5 |
| 2008 | 13,309 | 6.78 | 110.5 | 7.6 | 60.9 | 2.3 | 109.1 | 0.3 | 60.6 | 0.2 | 0.18 | 1.03 | −0.18 | 0.53 | 18.0 | 7.7 |
| 2009 | 12,896 | 6.57 | 110.1 | 7.5 | 60.8 | 2.3 | 109.8 | 0.3 | 60.9 | 0.2 | 0.22 | 1.04 | −0.17 | 0.53 | 17.1 | 8.4 |
| 2010 | 10,248 | 5.22 | 109.6 | 7.2 | 60.7 | 2.2 | 109.6 | 0.4 | 61.0 | 0.2 | 0.22 | 1.03 | −0.14 | 0.52 | 16.7 | 7.9 |
| 2011 | 13,418 | 6.84 | 111.1 | 7.7 | 61.1 | 2.4 | 109.8 | 0.3 | 60.9 | 0.2 | 0.26 | 1.05 | −0.16 | 0.53 | 20.5 | 9.1 |
| 2012 | 13,221 | 6.74 | 111.3 | 7.8 | 61.2 | 2.4 | 110.4 | 0.3 | 60.9 | 0.2 | 0.29 | 1.04 | −0.15 | 0.53 | 21.5 | 9.2 |
| 2013 | 14,291 | 7.28 | 110.9 | 7.7 | 61.1 | 2.4 | 110.3 | 0.3 | 61.4 | 0.2 | 0.28 | 1.05 | −0.14 | 0.53 | 21.1 | 8.8 |
| 2014 | 11,128 | 5.67 | 110.7 | 7.5 | 61.0 | 2.3 | 108.8 | 0.4 | 61.0 | 0.2 | 0.25 | 1.03 | −0.13 | 0.53 | 18.2 | 8.2 |
| Girls | ||||||||||||||||
| 1999 | 10,072 | 4.90 | 109.2 | 5.5 | 60.7 | 1.8 | 105.3 | 0.4 | 61.3 | 0.3 | 0.08 | 1.05 | −0.12 | 0.69 | 12.4 | 5.9 |
| 2000 | 13,337 | 6.48 | 108.7 | 5.6 | 60.5 | 1.8 | 105.4 | 0.4 | 60.3 | 0.2 | 0.09 | 1.01 | −0.19 | 0.62 | 10.4 | 5.5 |
| 2001 | 13,448 | 6.54 | 108.7 | 5.5 | 60.5 | 1.8 | 105.2 | 0.3 | 59.8 | 0.2 | 0.07 | 0.99 | −0.23 | 0.58 | 9.3 | 5.2 |
| 2002 | 13,464 | 6.54 | 108.5 | 5.5 | 60.4 | 1.8 | 105.0 | 0.3 | 60.0 | 0.2 | 0.05 | 0.99 | −0.23 | 0.58 | 9.7 | 4.5 |
| 2003 | 12,189 | 5.92 | 108.6 | 5.5 | 60.4 | 1.8 | 104.3 | 0.3 | 59.7 | 0.2 | −0.02 | 0.97 | −0.27 | 0.57 | 8.5 | 3.7 |
| 2004 | 13,552 | 6.59 | 108.6 | 5.5 | 60.5 | 1.8 | 103.2 | 0.3 | 59.2 | 0.2 | −0.10 | 0.97 | −0.30 | 0.59 | 7.0 | 2.9 |
| 2005 | 13,363 | 6.50 | 108.5 | 5.4 | 60.4 | 1.7 | 103.7 | 0.3 | 58.9 | 0.2 | −0.11 | 0.93 | −0.32 | 0.55 | 6.7 | 1.7 |
| 2006 | 13,788 | 6.70 | 108.7 | 5.4 | 60.4 | 1.7 | 103.9 | 0.3 | 59.5 | 0.2 | −0.08 | 0.90 | −0.27 | 0.53 | 7.0 | 1.3 |
| 2007 | 13,793 | 6.70 | 108.8 | 5.4 | 60.5 | 1.7 | 104.7 | 0.3 | 59.9 | 0.2 | −0.03 | 0.92 | −0.24 | 0.53 | 7.8 | 1.9 |
| 2008 | 13,717 | 6.67 | 109.0 | 5.3 | 60.6 | 1.7 | 103.7 | 0.3 | 59.5 | 0.2 | −0.08 | 0.95 | −0.27 | 0.54 | 7.4 | 1.8 |
| 2009 | 13,016 | 6.33 | 108.8 | 5.2 | 60.5 | 1.6 | 104.2 | 0.3 | 59.7 | 0.2 | −0.02 | 0.96 | −0.24 | 0.55 | 8.1 | 2.1 |
| 2010 | 9,817 | 4.77 | 108.3 | 5.1 | 60.3 | 1.6 | 103.9 | 0.4 | 59.7 | 0.2 | −0.01 | 0.96 | −0.22 | 0.55 | 8.2 | 2.5 |
| 2011 | 13,454 | 6.54 | 109.2 | 5.4 | 60.6 | 1.7 | 104.2 | 0.3 | 59.8 | 0.2 | −0.04 | 0.96 | −0.26 | 0.55 | 8.1 | 2.4 |
| 2012 | 13,350 | 6.49 | 109.4 | 5.3 | 60.7 | 1.7 | 104.2 | 0.3 | 59.8 | 0.2 | −0.03 | 0.94 | −0.25 | 0.53 | 8.1 | 2.1 |
| 2013 | 14,127 | 6.87 | 109.1 | 5.3 | 60.6 | 1.7 | 105.1 | 0.3 | 60.2 | 0.2 | 0.00 | 0.94 | −0.23 | 0.53 | 7.8 | 2.3 |
| 2014 | 11,254 | 5.47 | 109.1 | 5.3 | 60.6 | 1.7 | 103.6 | 0.4 | 59.8 | 0.2 | −0.01 | 0.95 | −0.22 | 0.52 | 7.7 | 2.2 |
Abbreviations: BP: blood pressure, SD: standard deviation; SE: standard error; z-score: standard deviation score. aAge-standardized systolic or diastolic BP relative to the 2000 World Health Organization World Population Standard. bMean systolic or diastolic BP in z-score relative to age-, sex- and height-standardized blood pressure standards from the United States National High Blood Pressure Education Group in 2004: 1 unit change in systolic BP z-score is approximated to 10.6 mmHg and 1 unit change in diastolic BP z-score is approximated to 11.3 mmHg. cPrehypertensive BP was defined as systolic or diastolic blood pressure > = 90th percentile but <95th percentile or > = 120/80 mmHg; Hypertensive BP was defined as systolic or diastolic blood pressure > = 95th percentile.
Table 2.
Age-Adjusted Body Mass Index (BMI), Age-Standardized BMI,a Age-Standardized BMI Z-scoresb and Proportion of Overweight and Obesityc Among 957,577 Boys and 941,239 Girls Aged 6 to 18 From 1996 to 2014 in Hong Kong.
| Year | n | % | Age-adjusted | Age-standardized | Age-standardized | Overweight | Obesity | |||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | BMI (kg/m2) | BMI z-score | ||||||||
| Mean | SD | Mean | SE | Mean | SD | % | % | |||
| Boys | ||||||||||
| 1996 | 77,869 | 8.13 | 17.9 | 1.0 | 18.3 | 0.02 | 0.14 | 1.38 | 14.4 | 4.6 |
| 1997 | 86,890 | 9.07 | 18.9 | 1.6 | 18.4 | 0.01 | −0.10 | 1.32 | 11.6 | 3.3 |
| 1998 | 57,492 | 6.00 | 18.4 | 1.5 | 18.5 | 0.01 | 0.06 | 1.36 | 13.5 | 4.3 |
| 1999 | 48,965 | 5.11 | 18.2 | 1.4 | 18.6 | 0.02 | 0.14 | 1.37 | 14.5 | 4.8 |
| 2000 | 47,379 | 4.95 | 18.2 | 1.3 | 18.6 | 0.02 | 0.18 | 1.37 | 15.0 | 4.9 |
| 2001 | 47,139 | 4.92 | 18.1 | 1.3 | 18.7 | 0.02 | 0.20 | 1.37 | 15.6 | 4.9 |
| 2002 | 49,116 | 5.13 | 18.1 | 1.3 | 18.6 | 0.02 | 0.19 | 1.38 | 15.2 | 5.1 |
| 2003 | 42,569 | 4.45 | 18.2 | 1.3 | 18.8 | 0.02 | 0.26 | 1.37 | 15.9 | 5.5 |
| 2004 | 45,208 | 4.72 | 18.2 | 1.3 | 18.8 | 0.02 | 0.27 | 1.37 | 16.4 | 5.5 |
| 2005 | 41,653 | 4.35 | 18.3 | 1.3 | 18.9 | 0.02 | 0.30 | 1.37 | 16.9 | 5.6 |
| 2006 | 42,709 | 4.46 | 18.3 | 1.3 | 18.9 | 0.02 | 0.28 | 1.39 | 17.0 | 5.8 |
| 2007 | 41,986 | 4.38 | 18.4 | 1.3 | 19.0 | 0.02 | 0.32 | 1.38 | 17.3 | 6.1 |
| 2008 | 42,254 | 4.41 | 18.4 | 1.3 | 19.1 | 0.02 | 0.37 | 1.39 | 17.8 | 6.8 |
| 2009 | 40,279 | 4.21 | 18.2 | 1.3 | 19.2 | 0.02 | 0.44 | 1.39 | 18.7 | 7.2 |
| 2010 | 34,047 | 3.56 | 18.1 | 1.3 | 19.2 | 0.03 | 0.43 | 1.40 | 18.4 | 7.5 |
| 2011 | 43,531 | 4.55 | 18.3 | 1.4 | 19.2 | 0.02 | 0.40 | 1.38 | 18.2 | 7.0 |
| 2012 | 48,459 | 5.06 | 18.1 | 1.5 | 19.1 | 0.02 | 0.35 | 1.37 | 17.3 | 6.6 |
| 2013 | 58,389 | 6.10 | 17.9 | 1.4 | 19.2 | 0.02 | 0.39 | 1.37 | 17.5 | 6.8 |
| 2014 | 61,643 | 6.44 | 17.6 | 1.3 | 19.0 | 0.02 | 0.34 | 1.37 | 15.9 | 6.5 |
| Girls | ||||||||||
| 1996 | 70,970 | 7.54 | 17.9 | 1.1 | 17.9 | 0.02 | −0.15 | 1.19 | 10.7 | 2.5 |
| 1997 | 94,507 | 10.04 | 19.2 | 1.6 | 18.1 | 0.01 | −0.29 | 1.10 | 8.3 | 1.8 |
| 1998 | 59,055 | 6.27 | 18.7 | 1.6 | 18.1 | 0.01 | −0.22 | 1.13 | 9.3 | 2.1 |
| 1999 | 47,903 | 5.09 | 18.5 | 1.5 | 18.1 | 0.01 | −0.18 | 1.15 | 10.0 | 2.3 |
| 2000 | 46,968 | 4.99 | 18.4 | 1.5 | 18.1 | 0.01 | −0.15 | 1.14 | 10.2 | 2.2 |
| 2001 | 46,558 | 4.95 | 18.3 | 1.4 | 18.1 | 0.01 | −0.13 | 1.14 | 10.5 | 2.3 |
| 2002 | 47,929 | 5.09 | 18.3 | 1.4 | 18.1 | 0.01 | −0.13 | 1.14 | 10.3 | 2.3 |
| 2003 | 42,440 | 4.51 | 18.4 | 1.4 | 18.2 | 0.02 | −0.08 | 1.14 | 11.1 | 2.5 |
| 2004 | 44,391 | 4.72 | 18.4 | 1.4 | 18.3 | 0.02 | −0.08 | 1.13 | 11.0 | 2.4 |
| 2005 | 42,043 | 4.47 | 18.4 | 1.4 | 18.3 | 0.02 | −0.07 | 1.14 | 11.4 | 2.4 |
| 2006 | 41,915 | 4.45 | 18.5 | 1.4 | 18.3 | 0.02 | −0.08 | 1.14 | 11.1 | 2.4 |
| 2007 | 41,219 | 4.38 | 18.5 | 1.4 | 18.4 | 0.02 | −0.04 | 1.13 | 11.8 | 2.5 |
| 2008 | 41,226 | 4.38 | 18.5 | 1.4 | 18.5 | 0.02 | 0.01 | 1.13 | 11.9 | 2.8 |
| 2009 | 38,416 | 4.08 | 18.4 | 1.4 | 18.5 | 0.02 | 0.05 | 1.13 | 12.8 | 3.1 |
| 2010 | 32,410 | 3.44 | 18.2 | 1.3 | 18.5 | 0.02 | 0.06 | 1.16 | 13.4 | 3.3 |
| 2011 | 41,613 | 4.42 | 18.4 | 1.5 | 18.5 | 0.02 | 0.03 | 1.13 | 12.4 | 3.0 |
| 2012 | 46,945 | 4.99 | 18.2 | 1.5 | 18.5 | 0.02 | −0.01 | 1.13 | 11.9 | 2.9 |
| 2013 | 56,496 | 6.00 | 18.0 | 1.5 | 18.5 | 0.02 | 0.02 | 1.12 | 12.0 | 2.9 |
| 2014 | 58,235 | 6.19 | 17.7 | 1.4 | 18.4 | 0.02 | −0.01 | 1.11 | 11.1 | 2.9 |
Abbreviations: BMI: body mass index, SD: standard deviation; SE: standard error; z-score: standard deviation score. aAge-standardized BMI relative to the 2000 World Health Organization World Population Standard. bMean BMI in z-score relative to the 2007 World Health Organization growth references for 5–19 years: 1 unit change in BMI z-score is approximated to 2.67 kg/m2. cOverweight was defined using the International Obesity Task Force cut-offs as equivalent to an adult BMI of 25 or more; Obesity was defined as equivalent to an adult BMI of 30 or more.
Table 3.
Mean Differencea in Age- and Height-Standardized Systolic and Diastolic Blood Pressure (BP) Z-scoresb per Year Among Boys and Girls Aged 9 to 18 From 1999 to 2014 and Age-Standardized Body Mass Index (BMI) Z-scoresc per Year Among Boys and Girls Aged 6 to 18 From 1996 to 2014 in Hong Kong.
| No. | Model 1 | No. | Model 2 | ||||
|---|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | ||||
| Boys | Systolic BP z-score | ||||||
| Year | 195649 | −0.004 | (−0.005, −0.003) | 195633 | −0.012 | (−0.013, −0.011) | |
| BMI z-score *Year | 0.004 | (0.003, 0.004) | |||||
| Diastolic BP z-score | |||||||
| Year | 205608 | −0.002 | (−0.002, −0.001) | 205598 | −0.003 | (−0.004, −0.003) | |
| BMI z-score *Year | 0.0004 | (0.00002, 0.0008) | |||||
| BMI z-score | |||||||
| Year | 957577 | 0.022 | (0.021, 0.022) | ||||
| Girls | Systolic BP z-score | ||||||
| Year | 205608 | −0.006 | (−0.006, −0.005) | 205598 | −0.013 | (−0.013, −0.012) | |
| BMI z-score *Year | 0.004 | (0.003, 0.004) | |||||
| Diastolic BP z-score | |||||||
| Year | 205608 | −0.002 | (−0.002, −0.001) | 205598 | −0.004 | (−0.004, −0.003) | |
| BMI z-score *Year | 0.001 | (0.0006, 0.002) | |||||
| BMI z-score | |||||||
| Year | 941239 | 0.016 | (0.015, 0.016) | ||||
Abbreviations: BP: blood pressure, BMI: body mass index, z-score: standard deviation score; β: beta coefficient. aModel 1 was crude association. Model 2 additionally included BMI z-score time trend (i.e., interaction term between BMI z-score and Year). bMean systolic or diastolic BP in z-score relative to age-, sex- and height-standardized blood pressure standards from the United States National High Blood Pressure Education Group in 2004: 1 unit change in systolic BP z-score is approximated to 10.6 mmHg and 1 unit change in diastolic BP z-score is approximated to 11.3 mmHg. cMean BMI in z-score relative to the 2007 World Health Organization growth references for 5–19 years: 1 unit change in BMI z-score is approximated to 2.67 kg/m2.
Figure 1 shows mean systolic BP z-score was relatively stable from 1999 and then decreased slightly from 2002 to 2005 followed by a slight increase afterwards to 2014 in both sexes. Mean diastolic BP had a slightly decreasing tendency from 1999 to 2004 and then remained stable to 2014. Conversely, mean BMI decreased from 1996 to 1997 and then increased until 2009/2010 followed by stagnation or a very slight decreasing tendency to 2014 in both sexes. Overall, boys had higher systolic BP and BMI than girls, but similar diastolic BP to girls. Somewhat similar changes were identified by sex-specific jointpoint analyses (Appendix Table 1), although no clear changes were identified for BMI in girls.
Figure 1.
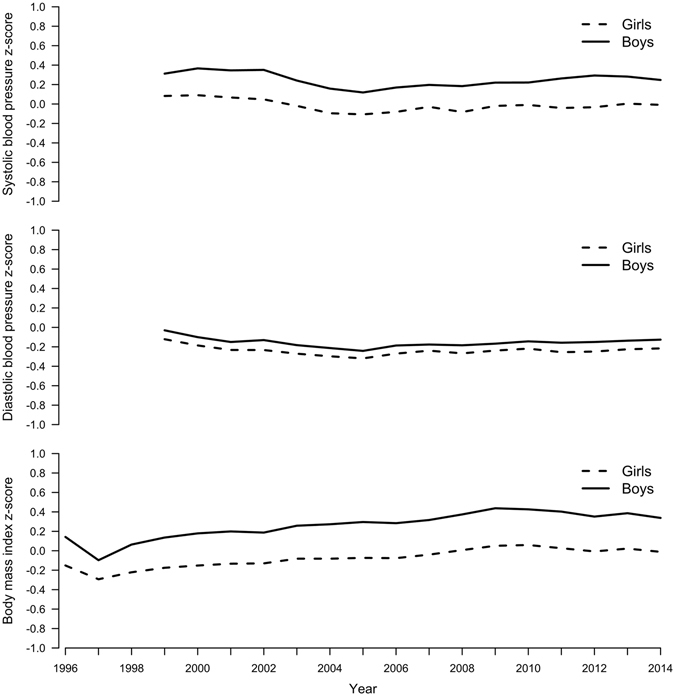
Mean Age- and Height-Standardized Systolic and Diastolic Blood Pressure (BP) Z-scores Among Boys and Girls Aged 9 to 18 From 1999 to 2014 and Mean Age-Standardized BMI Z-scores Among Boys and Girls Aged 6 to 18 From 1996 to 2014 in Hong Kong.
Figure 2 shows the distribution of systolic BP z-score had a marked downward shift in the upper tail for girls as did diastolic BP z-score in both sexes from 1999 to 2014, with overall a narrower distribution. The entire BMI z-score distribution shifted upward in both sexes from 1996 (or 1999) to 2014, but retained a right skewed distribution. The downward shift in the upper tail of the BP distribution and the upward shift of the entire BMI distribution was observed across all ages; except that the distribution of systolic BP in boys at age 12 years or above remained high from 1999 to 2014 (Appendix Fig. 1).
Figure 2.
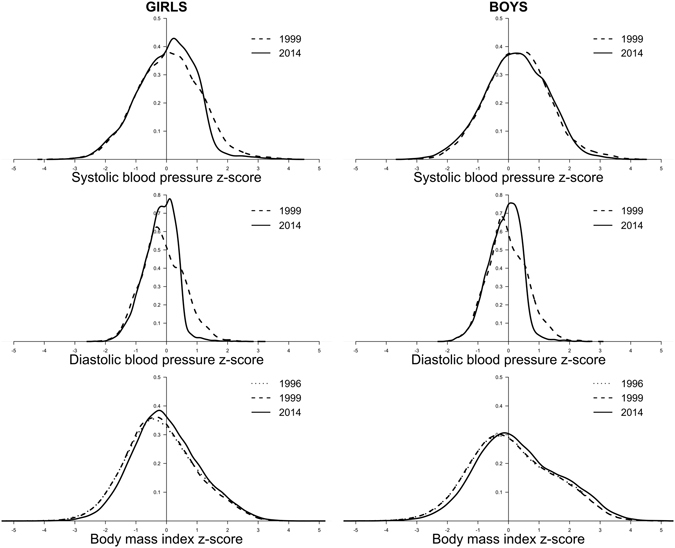
Distribution of Age- and Height-Standardized Systolic and Diastolic Blood Pressure (BP) Z-scores Among Boys and Girls Aged 9 to 18 in 1999 and 2014 and Distribution of Age-Standardized BMI z-scores Among Boys and Girls aged 6 to 18 in 1996 and 2014 in Hong Kong.
Discussion
In a recently developed Chinese setting, overall systolic and diastolic BP declined modestly whereas BMI rose generally among children and adolescents over the last two decades. As a result by 2014, girls on average had BP and BMI below or close to the reference, whilst boys had systolic BP and BMI further above the reference. In addition, the upper end of the systolic and diastolic BP distributions shifted downward (except systolic BP in boys), whereas the entire BMI distribution shifted upward from 1996 to 2014.
This is the first large study with novel use of big data based on bi-annual BP and annual BMI measurements comprehensively covering childhood and adolescence, and so adds evidence concerning BP and BMI trends over nearly 20 years. To our knowledge, five previous studies examining both BP and BMI trends in children and adolescents over a similar period based on a population-representative sample from the same study have been published. The divergent patterns of BP and BMI in Hong Kong are inconsistent with patterns in rapidly developing China9, 10, 13, but are more similar to current trends in some other recently developed settings, such as the Seychelles11 and South Korea12, and are also similar to previous trends in long-term developed settings, such as the United Kingdom6 and the United States7. For instance, in recently developed South Korea, systolic BP z-score also declined but more strongly, by 0.08 per year in boys and 0.093 in girls from 1998 to 2008, with no clear changes in diastolic BP z-score. However, BMI increased from 1998 to 2005 before declining in 2007/08 (overall 0.033 per year) in boys with no changes in girls12, unlike our study showing similar BMI z-score trends in both sexes. Similarly, in earlier decades in the United States, where systolic BP slightly increased in 1979–1982 and then by 1993 gradually returned to same value as 1974, whereas diastolic BP z-score decreased by 0.009 per year in boys and 0.006 in girls from 1974 to 199321. During the same period, BMI z-score monotonically increased by 0.028 per year in boys and 0.024 in girls21.
The BP and BMI profile appears to be more adverse in boys than girls, whether this is a reflection of cultural practises and pressures which emphasize different physical attributes in boys than girls is unknown22. Nevertheless, it does suggest that any future trends in cardiovascular disease presaged by these trends are going to be more adverse in men than women, and perhaps growing boys should particularly be targets of intervention. Notably, these sex differences are congruent with the sex differences in cardiovascular disease that widen with economic development15, suggesting that early life factors contribute to this sexual disparity.
Our findings are consistent with a narrower diastolic BP distribution and an upward shift in BMI distribution in South Korea12 and the Seychelles11, but are inconsistent with their downward shift in systolic BP in both sexes11, 12, given the downward shift in the upper tail of systolic BP was only observed in girls but not boys in our study. It is possible that factors which cause high BP in children and adolescents, such as renal parenchymal disease23, or risk factors for high BP such as sleep disordered breathing24 or early infections25, reduced over the period. The introduction of universal neonatal immunization for hepatitis B in Hong Kong in 198826, or better access to care with the introduction of the Hospital Authority in Hong Kong in 199027 could perhaps play a role, but leaves the lack of fall in the upper tail of the systolic BP distribution in boys aged 12 years or older unexplained. Systolic blood pressure rises more at puberty in boys than girls, and some coincidental factor may be offsetting the downward shift in pubertal boys, such as sleep disorders due to playing computer games28, or environmental factors that promote specifically testosterone29.
Overall, our study adds evidence of some downward secular trend in BP despite rising BMI. Higher BMI is a major risk factor for BP30, which has been confirmed in Mendelian randomization studies of adults31. We also found slightly stronger associations of BP with BMI over time, suggesting the trend of slightly increasing BP after the mid-2000s could be partly related to the increasing BMI trend which could have partly counteracted a potentially more pronounced downward BP trend. Nonetheless, differing trends for BP and BMI here and elsewhere6, 7, 11, 12 also suggest that other environmental factors affect BP. One possibility is sodium intake, because sodium restriction in infancy might affect blood pressure in adolescence32. In Hong Kong, the proportion of young children with sodium intake higher than the recommended intake is less than 10% at <18 months but 31% at 48 months33, most (60%) young children also have vegetable intake and fruit intake lower than the recommendations33. However, whether these intakes have changed over the relevant time period is not known. Moreover, the role of vegetables and fruit in BP has not been clearly established in trials34. Breastfeeding rates have increased since the 1990s in Hong Kong35, although whether breastfeeding affects BP has not been unequivocally established36. Smoking during pregnancy is very low (<5%) in Hong Kong37. Alternatively, physical inactivity is associated with lower lean mass and higher fat mass38. Both lean mass and fat mass are similarly positively associated with BP39. Also, an increasing trend in BMI may be mainly due to gain in body fatness given fat mass may have increased more than lean mass in Chinese children in recent decades40. As such, more gain in fat mass but less lean mass might be possible, but whether this could result in slightly decreasing BP while BMI is increasing remains elusive. Physical inactivity is prevalent in children and adolesents in Hong Kong and is not known to have changed in a similar way as BP in recent decades41, 42. A meta-analysis of short-term trials of physical activity did not reduce BP in children and adolescents43. Two small trials in obese children found physical activity modestly lowered BP, but one showed an increase in lean mass and no change in fat mass and weight44, while the other showed less abdominal fat and an increase in weight45. Future studies are needed to establish the causal role of physical activity and body composition (muscle mass and body fatness) in BP.
Several limitations are noted. First, attending the health assessment is voluntary. Differential selection by child health status or parental attributes or family socioeconomic position could bias the results, which is unlikely given health assessment at the Student Health Service is free and accessible to all public or private school students. However, it would only bias trends if the selection of children attending varied over time. Second, using a single BP measurement at a single visit may slightly overestimate average BP and pre-/hypertensive BP prevalence46, but would not affect comparisons over time. Third, random measurement error is possible, for which the large sample size compensates. Fourth, changes in devices over time could cause an artifactual change. Devices used to measure height and weight are reliable with little difference between devices. BP was measured by an automated oscillometric device, and re-checked with a sphygomanometer manually, which did not change during the period. Fifth, mid-arm circumference in children and adolescents may have increased in recent decades, implying an adult cuff size may be required for BP measurement47. However, BP was measured by nurses following a standard protocol with a cuff size appropriate to the age and size of the child. Sixth, we calculated BMI z-score using the 2007 WHO growth reference which used the same data as the 2000 United States Centers for Disease Control and Prevention reference but a different smoothing technique, and defined overweight and obesity using the International Obesity Task Force (IOTF) cut-offs which are based on nationally representative samples from six regions including Hong Kong48. As such, the absolute magnitude may not be directly comparable, but we focused on change for comparison across populations. Seventh, the study is descriptive and we can only speculate about the aetiologies of the observed divergent trends in BP and BMI. Finally, observed trends in BP might be driven by changes in potential risk factors for BP such as diet, physical activity and smoking, although most of these would also be expected to affect BP through BMI. The trends of these factors over the same period could not be analyzed due to lack of information.
In summary, as in some recently developed or long-term developed settings in earlier decades, divergent overall secular trends in BP and BMI were evident, resulting in systolic BP and BMI in boys further above the reference. Concerted efforts to tackle global increasing BMI trend is imperative; identifying the potential underlying factors that may alleviate the impact of rising BMI on BP or may lower BP independent of BMI are also important to improving future population cardiovascular health with a particular focus on boys.
Methods
Data Source
This study used routinely collected BP and BMI from the Student Health Service of the Department of Health, which provides free annual health assessments for all primary and secondary school students in Hong Kong49, for whom 9 years free universal public education (primary and 3-year junior secondary) has been provided since 1978 and 12 years (plus 3-year senior secondary) since 2008/0950. The Student Health Service was introduced in 1995/96 for primary school students, and was extended to secondary school students in 1996/97, but was suspended for secondary school students in year 2 and above in 2009/10 because of the Human Swine Influenza Vaccination Programme. The participation rate from 1995/96 to 2013/14 was 83.4%51. The health assessments include bi-annual assessments of BP (Primary 5 (age 10–11 years) onwards) and annual measurements of weight and height (Primary 1 (age 6–7 years) onwards). BP was measured by nurses on the right arm in a seated position after more than 10 minutes of rest with an age and size appropriate cuff size using an automated oscillometric device. Initial systolic or diastolic BP higher than the 90th percentile for sex, age and height based on local references was re-checked by physicians with a sphygmomanometer after 15 minutes of rest and this second measurement was recorded. Height without shoes was measured by stadiometer to the nearest 0.1 centimetre and weight without shoes and outer clothing was measured by digital scales to the nearest 0.1 kilogram. BMI was calculated as weight in kilogram divided by height in meters squared. Coverage was incomplete in the early years, so we considered trends of BP since 1999 and BMI since 1996. We randomly selected one time point per participant so that there is no correlation between multiple measurements for the same participant. Given BMI was measured more often than BP and across a wider age range, more children and adolescents with BMI than BP were included.
Outcomes
Blood pressure
Systolic and diastolic BP were considered as standard deviations (z-scores) relative to age-, sex- and height-standardized blood pressure standards from the 2004 United States National High Blood Pressure Education Group52, to account for compositional differences by age, sex and the secular trend in height. Prehypertensive BP was also considered, defined as systolic or diastolic BP greater than or equal to the 90th percentile but less than the 95th percentile based on age-, sex- and height-specific standards or 120/80 mmHg for both boys and girls. Finally, hypertensive BP was defined as systolic or diastolic BP greater than or equal to 95th percentile52.
Body mass index
BMI was considered as z-scores relative to the 2007 World Health Organization (WHO) growth references for 5–19 years53. Overweight or obesity was also considered, defined as a BMI for age and sex corresponding to an adult BMI of ≥25 kg/m2 or ≥30 kg/m2 using the IOTF cut-offs54.
For completeness, age- and height-adjusted BP and age-adjusted BMI by sex were calculated as the internally weighted average BP and BMI accounting for differences in mean age and/or height across years within the sample. Age-standardized BP and BMI by sex were also calculated using the 2000 WHO World Standard Population for direct standardization55.
Statistical analysis
To examine the secular trends in BP from 1999 to 2014 and BMI from 1996 to 2014, we plotted sex-specific mean BP and BMI z-scores by calendar year, and reported the average difference per year. We used jointpoint regression analysis with modified Bayesian information criterion to identify when the slope of BP and BMI z-scores trends changed significantly56. To identify changes in BP or BMI distribution, we plotted their distributions in 1996, 1999 and 2014 using a kernel density function. To identify at what ages changes in BP or BMI distribution occurred, we further plotted their distributions by each age in 1996, 1999 and 2014. We summarized the overall sex-specific changes in BP and BMI z-scores across years by regressing z-scores on calendar year using linear regression. We also assessed whether the strength (slope) of the association of BP with BMI changed over time by regressing BP z-score on BMI z-score, calendar year and the interaction term between BMI z-scores and calendar year, of which a positive interaction term coefficient indicates a stronger association of BP with BMI in later periods11. Statistical analyses were performed using Stata version 12.1 (Stata Corp, College station, Texas, USA), R version 3.0.1 (R Development Core Team, Vienna, Austria) and the jointpoint trend analysis version 4.2.0.1 (National Cancer Institute, USA)57.
Ethics approval
The methods were carried out in accordance with the approved guidelines. The protocol was approved by the Health and Medical Research Fund, Government of the Hong Kong Special Administrative Region (SAR). The study obtained ethical approval from the University of Hong Kong-Hospital Authority Hong Kong West Cluster Joint Institutional Review Board. This study only used de-identified secondary data routinely collected by the Student Health Service, with informed consent obtained from a parent or guardian of the participants prior to participation to the voluntary health assessments.
Electronic supplementary material
Acknowledgements
The authors are grateful to the Student Health Service of the Department of Health, Government of the Hong Kong SAR for their support and for facilitating data access, and the colleagues and the students involved with the Student Health Service throughout the years. Dr. M.K. Kwok thanks the Takemi Program in International Health at the Harvard T.H. Chan School of Public Health for her fellowship during which this manuscript was prepared. This project was supported by the Health and Medical Research Fund [HMRF Grant # 11121371], Government of the Hong Kong SAR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions
M.K. Kwok conceptualized ideas, designed analytic strategy, performed the literature review, conducted data analysis, interpreted findings and drafted the manuscript. G.M. Leung interpreted findings and critically reviewed the manuscript. T.W.H. Chung and K.K.Y. Lee critically reviewed the manuscript. C.M. Schooling conceptualized ideas, directed analytic strategy, interpreted findings, revised drafts of the manuscript critically and supervised the study from conception to completion.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-05133-2
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Danaei G, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 2.Finucane MM, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 4.Song YM, Sung J, Davey Smith G, Ebrahim S. Body mass index and ischemic and hemorrhagic stroke: a prospective study in Korean men. Stroke. 2004;35:831–836. doi: 10.1161/01.STR.0000119386.22691.1C. [DOI] [PubMed] [Google Scholar]
- 5.McCarron P, Smith GD, Okasha M. Secular changes in blood pressure in childhood, adolescence and young adulthood: systematic review of trends from 1948 to 1998. J Hum Hypertens. 2002;16:677–689. doi: 10.1038/sj.jhh.1001471. [DOI] [PubMed] [Google Scholar]
- 6.Peters H, Whincup PH, Cook DG, Law C, Li L. Trends in blood pressure in 9 to 11-year-old children in the United Kingdom 1980-2008: the impact of obesity. J Hypertens. 2012;30:1708–1717. doi: 10.1097/HJH.0b013e3283562a6b. [DOI] [PubMed] [Google Scholar]
- 7.Zachariah JP, et al. Temporal trends in pulse pressure and mean arterial pressure during the rise of pediatric obesity in US children. J Am Heart Assoc. 2014;3:e000725. doi: 10.1161/JAHA.113.000725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 9.Liang YJ, et al. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991-2004. Blood Press. 2011;20:45–53. doi: 10.3109/08037051.2010.524085. [DOI] [PubMed] [Google Scholar]
- 10.Dong B, Wang HJ, Wang Z, Liu JS, Ma J. Trends in blood pressure and body mass index among Chinese children and adolescents from 2005 to 2010. Am J Hypertens. 2013;26:997–1004. doi: 10.1093/ajh/hpt050. [DOI] [PubMed] [Google Scholar]
- 11.Chiolero A, et al. Discordant secular trends in elevated blood pressure and obesity in children and adolescents in a rapidly developing country. Circulation. 2009;119:558–565. doi: 10.1161/CIRCULATIONAHA.108.796276. [DOI] [PubMed] [Google Scholar]
- 12.Khang YH, Lynch JW. Exploring determinants of secular decreases in childhood blood pressure and hypertension. Circulation. 2011;124:397–405. doi: 10.1161/CIRCULATIONAHA.110.014399. [DOI] [PubMed] [Google Scholar]
- 13.Liang YJ, Xi B, Song AQ, Liu JX, Mi J. Trends in general and abdominal obesity among Chinese children and adolescents 1993-2009. Pediatr Obes. 2012;7:355–364. doi: 10.1111/j.2047-6310.2012.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiolero A, Bovet P, Paradis G, Paccaud F. Has blood pressure increased in children in response to the obesity epidemic? Pediatrics. 2007;119:544–553. doi: 10.1542/peds.2006-2136. [DOI] [PubMed] [Google Scholar]
- 15.Ezzati M, et al. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12:508–530. doi: 10.1038/nrcardio.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lurbe E. Childhood blood pressure: trends and future tracks. Hypertension. 2013;62:242–243. doi: 10.1161/HYPERTENSIONAHA.113.01589. [DOI] [PubMed] [Google Scholar]
- 17.Chiolero A, Bovet P, Paradis G. Assessing secular trends in blood pressure in children and adolescents. J Hum Hypertens. 2009;23:426–427. doi: 10.1038/jhh.2008.165. [DOI] [PubMed] [Google Scholar]
- 18.Tsang, S. A modern history of Hong Kong. (I.B. Tauris, 2003).
- 19.Maddison, A. Development centre studies: the world economy: historical statistics., http://www.ggdc.net/maddison/maddison-project/data.htm (Date of access: March 1, 2014) (2003).
- 20.Schooling CM, Leung GM. A socio-biological explanation for social disparities in non-communicable chronic diseases: the product of history? J Epidemiol Community Health. 2010;64:941–949. doi: 10.1136/jech.2008.086553. [DOI] [PubMed] [Google Scholar]
- 21.Freedman DS, et al. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart Study. Pediatrics. 2012;130:e159–166. doi: 10.1542/peds.2011-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu X, et al. Body dissatisfaction, engagement in body change behaviors and sociocultural influences on body image among Chinese adolescents. Body Image. 2010;7:156–164. doi: 10.1016/j.bodyim.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Riley M, Bluhm B. High blood pressure in children and adolescents. Am Fam Physician. 2012;85:693–700. [PubMed] [Google Scholar]
- 24.Nisbet LC, Yiallourou SR, Walter LM, Horne RS. Blood pressure regulation, autonomic control and sleep disordered breathing in children. Sleep Med Rev. 2014;18:179–189. doi: 10.1016/j.smrv.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 26.Special Preventive Programme of Centre for Health Protection; Department of Health; Goverment of Hong Kong SAR. Surveillance of viral hepatitis in Hong Kong - 2011 update report, http://www.info.gov.hk/hepatitis/doc/hepsurv11.pdf (Date of access: 30 June 2016) (2012).
- 27.Hospital Authority. Hospital Authority Introduction, http://www.ha.org.hk/visitor/ha_visitor_index.asp?Parent_ID=10004&Content_ID=10008&Ver=HTML (Date of access: 30 June 2016) (2015).
- 28.Ho SM, Lee TM. Computer usage and its relationship with adolescent lifestyle in Hong Kong. J Adolesc Health. 2001;29:258–266. doi: 10.1016/S1054-139X(01)00261-0. [DOI] [PubMed] [Google Scholar]
- 29.Diamanti-Kandarakis E, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009;30:293–342. doi: 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Health & Social Care Information Centre. Health Survey for England - 2006, CVD and risk factors for adults, obesity and risk factors for children: Volume 2, Obesity and other risk factors in children (2008).
- 31.Fall T, et al. The role of adiposity in cardiometabolic traits: a Mendelian randomization analysis. PLoS Med. 2013;10:e1001474. doi: 10.1371/journal.pmed.1001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geleijnse JM, et al. Long-term effects of neonatal sodium restriction on blood pressure. Hypertension. 1997;29:913–917. doi: 10.1161/01.HYP.29.4.913. [DOI] [PubMed] [Google Scholar]
- 33.Woo, J., Chan, R., Li, L. & Luk, W. A survey of infant and young child feeding in Hong Kong: diet and nutrient intake. (Department of Medicine and Therapeutics and Centre for Nutritional Studies, The Chinese University of Hong Kong and Family Health Service, Department of Health, Hong Kong SAR Government., Hong Kong, 2012).
- 34.Berry SE, Mulla UZ, Chowienczyk PJ, Sanders TA. Increased potassium intake from fruit and vegetables or supplements does not lower blood pressure or improve vascular function in UK men and women with early hypertension: a randomised controlled trial. Br J Nutr. 2010;104:1839–1847. doi: 10.1017/S0007114510002904. [DOI] [PubMed] [Google Scholar]
- 35.Baby Friendly Hospital Initiative. Breastfeeding Trend, http://www.babyfriendly.org.hk/en/breastfeeding-in-hk/breastfeeding-trend/ (Date of access: 30 June 2016) (2015).
- 36.Chung SH, Kim HR, Choi YS, Bae CW. Trends of breastfeeding rate in Korea (1994-2012): comparison with OECD and other countries. J Korean Med Sci. 2013;28:1573–1580. doi: 10.3346/jkms.2013.28.11.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tobacco Control Office of the Department of Health; Hong Kong SAR. Statistics: pattern of smoking in Hong Kong, http://www.tco.gov.hk/english/infostation/infostation_sta_01.html (Date of access: 30 June 2016) (2013).
- 38.Riso EM, Kull M, Mooses K, Hannus A, Jurimae J. Objectively measured physical activity levels and sedentary time in 7-9-year-old Estonian schoolchildren: independent associations with body composition parameters. BMC Public Health. 2016;16:346. doi: 10.1186/s12889-016-3000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brion MA, Ness AR, Smith GD, Leary SD. Association between body composition and blood pressure in a contemporary cohort of 9-year-old children. Journal of Human Hypertension. 2007;21:283–290. doi: 10.1038/sj.jhh.1002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang YX, Wang SR. Changes in skinfold thickness and body composition among children and adolescents in Shandong, China from 1995 to 2010. Journal of Human Nutrition and Dietetics. 2013;26:252–258. doi: 10.1111/jhn.12006. [DOI] [PubMed] [Google Scholar]
- 41.Lam JW, Sit CH, Cerin E. Physical activity and sedentary behaviours in Hong Kong primary school children: Prevalence and gender differences. Prev Med. 2010;51:96–97. doi: 10.1016/j.ypmed.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 42.Department of Health & Hong Kong SAR. Levels of physical activity among children and adolescents, http://www.change4health.gov.hk/en/physical_activity/figures/children/index.html (Date of access: (2015).
- 43.Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8–16. doi: 10.1111/j.1520-037X.2003.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Naylor LH, et al. Resistance training and diastolic myocardial tissue velocities in obese children. Med Sci Sports Exerc. 2008;40:2027–2032. doi: 10.1249/MSS.0b013e318182a9e0. [DOI] [PubMed] [Google Scholar]
- 45.Farpour-Lambert NJ, et al. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396–2406. doi: 10.1016/j.jacc.2009.08.030. [DOI] [PubMed] [Google Scholar]
- 46.Wong SN, Tz Sung RY, Leung LCK. Validation of three oscillometric blood pressure devices against auscultatory mercury sphygmomanometer in children. Blood Pressure Monitoring. 2006;11:281–291. doi: 10.1097/01.mbp.0000209082.09623.b4. [DOI] [PubMed] [Google Scholar]
- 47.Prineas RJ, Ostchega Y, Carroll M, Dillon C, McDowell M. US demographic trends in mid-arm circumference and recommended blood pressure cuffs for children and adolescents: data from the National Health and Nutrition Examination Survey 1988-2004. Blood Press Monit. 2007;12:75–80. doi: 10.1097/MBP.0b013e3280b08342. [DOI] [PubMed] [Google Scholar]
- 48.Wang, Y. F. & Chen, H. J. In Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease Vol. 4 (ed V. R. Preedy) 29–48 (2012).
- 49.Student Health Service of Department of Health & Hong Kong SAR. Student Health Service, http://www.studenthealth.gov.hk/eindex.html (Date of access: 30 June 2016).
- 50.Organisation for Economic Co-operation and Development (OECD). Shanghai and Hong Kong: two distinct examples of education reform in China. Lessons from PISA for the United States, Strong Performers and Successful Reformers in Education. 83-115 (OECD Publishing, 2011).
- 51.Department of Health; Goverment of Hong Kong SAR. Department of Health Annual Report from 1995/96 to 2013/14. (1996–2015).
- 52.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics114, 555–576 (2004). [PubMed]
- 53.World Health Organization (WHO). WHO growth reference 5–19 years. (WHO, Geneva, 2007).
- 54.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Admad, O. B. et al. Age standardization of rates: a new WHO Standard, http://www.who.int/healthinfo/paper31.pdf (Date of access: 30 June 2016) (2001).
- 56.Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19, 335–351 (correction: 2001;2020–2655) (2000). [DOI] [PubMed]
- 57.Statistical Methodology and Applications Branch, Surveillance Research Program & National Cancer Institute. Joinpoint Regression Program, Version 4.2.0 - April 2015, http://surveillance.cancer.gov/joinpoint/ (Date of access: 30 June 2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


