Abstract
Every year, almost 62,000 are diagnosed with a head and neck cancer (HNC) and 13,000 will succumb to their disease. In the primary setting, intraoperative radiation therapy (IORT) can be used as a boost in select patients in order to optimize local control. Addition of external beam radiation to limited volumes results in improved disease control over surgery and IORT alone. In the recurrent setting, IORT can improve outcomes from salvage surgery especially in patients previously treated with external beam radiation. The use of IORT remains limited to select institutions with various modalities being currently employed including orthovoltage, electrons, and high-dose rate brachytherapy. Practically, execution of IORT requires a coordinated effort and careful planning by a multidisciplinary team involving the head and neck surgeon, radiation oncologist, and physicist. The current review summarizes common uses, outcomes, toxicities, and technical aspects of IORT in HNC patients.
Keywords: recurrent cancer, locally advanced, head and neck tumors, salivary gland tumors, intraoperative radiation therapy
Introduction
Head and neck cancers (HNCs) continue to take a high toll with an estimated incidence of around 62,000 new cases in the United States in 2016 (1). Radiation therapy (RT) is commonly used as adjuvant treatment or, as definitive modality when surgical resection is not possible. Delivering radiation at the time of resection of HNCs is particularly helpful in cases at high risk for recurrence, particularly where there is gross or microscopic residual disease or for recurrent disease (2). The safety and effectiveness of intraoperative radiation therapy (IORT) for HNCs have been established in studies from several institutions (3–5). Although IORT is mainly used in recurrent patients, few studies reported on its use in the primary setting. Two forms of IORT have been studied for HNCs: high-dose rate (HDR) brachytherapy (6) and external beam that includes electrons and orthovoltage photons IORT (3, 4). The purpose of this manuscript is to review experience over the past four decades with the use of IORT in patients with primary or recurrent cancer of head and neck.
Role of IORT in Head and Neck Tumors
Recurrent HNC
The treatment of recurrent HNC is challenging, especially in the setting of previous irradiation. As per the NCCN 2017 guidelines, surgery is the mainstay of treatment for resectable locoregional recurrences with or without the addition of postoperative reirradiation (7). However, the NCCN adds a word of caution that reirradiation should be limited to a highly selected group of patients (8). The main challenge in reirradiation is the dose limiting tolerance of surrounding normal tissue. Hence, many studies have reported on the use of IORT since it provides the advantage of decreasing the treatment volume to the site that is directly observed in the operating room (OR), in addition to the possibility of operative mobilization of organs at risk, and normal tissue shielding. Encouraging results have been observed with the use of IORT for recurrent head and neck tumors at the primary site, neck, or salivary glands (Table 1).
Table 1.
Summary of retrospective studies on IORT use in recurrent head and neck cancer.
| Reference | Na | Primary location (most common) | Median tumor sizee | IORT location | IORT modality | Dose range | Median dose | Adjuvant therapy at rec. | Hx of RT | Duration to reirradiation | Median F/U | LC | Survival | Toxicity |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scala et al. (9) | n = 76 (87 sites) | Oral cavity (29%), SGT (18%), OP (16%) | Median field size: 5 = 6 cm | Neck (46%); face (13%) | HDR IORT | 12–17.5 Gyb | 12 Gy | 24% EBRT (45 Gy) 41% (chemo) | EBRT: (59.8–63.9 Gy) | 2 years | 11 months | 2 year IFLC: 62% | MS: 33 months (in field control) and 17 months (no control) | Flap revision: 4%, carotid hemorrhage: 1%, vagal neuropathy: 1% |
| Teckie et al. (10) | n = 57 (59 sites) | OP, hypopharynx, SGT | ≤2 cm: 42% 2.1–4 cm: 32% >4 cm: 25% |
Neck (71%); parotid (12%) | HDR IORT | 12–20 Gy | 15 Gy | 21% EBRT: (50 Gy) 27% (chemo) 11% (both) | EBRT: median dose: 66 Gy | Median: 15 months | 16 months | 3-year IFPFS: 57% | 3 year OS: 50% (in field control) vs. 32% (no control) | Fibrosis: 29%, trismus: 24%, cellulitis: 10%, CN injury: 26%, dysphagia: 39%, fistula: 15% |
| Zeidan et al. (11) | n = 46 (out of 96 total) | Parotid gland | ≤2 cm: 47% 2.1–4 cm: 39% >4 cm: 14% |
Parotid (100%) | IOERT (Mobetron) | 15 Gy or 20 Gy | 15–20 Gy | 57% EBRT (45 Gy), 19% chemo | EBRT: median dose: 60 Gy | 8.7 months | 5.6 years | 5 year RFS: 48.1% (recurrent) | 3 year OS: 59%, 5 year OS: 48% (recurrent)c | Comp.: 27% vascular: 7%, trismus: 6%, ORN: 4%, fistulas: 4%, flap necrosis: 2%, wound dehiscence: 2%, neuropathy 1% |
| Zeidan et al. (12) | n = 198 (out of 231 total) | UAD tract | 4.3 cm | Neck (100%) | IOERT | 10–25 Gy | 15–20 Gy | 22% EBRT (45 Gy), 43% chemo | EBRT: dose not reported | NR | 1.03 years | 3 year RFS: 55%, 5 year RFS: 49% (for all) | 3 year OS: 34%, 5 year OS: 26% (for all) | Vascular: 11.3%, fistula: 9.8%, wound dehiscence: 9.8%, neuropathy: 3%ORN: 4% |
| Perry et al. (6) | n = 34 | Salivary gland (21%) and OP (21%) | ≤2 cm: 53% 2.1–4 cm: 26% >4 cm: 21% |
Salivary gland (21%) and OP (21%) | HDR-IORT | 10–20 Gy | 15 Gy | 15% EBRT: (50 Gy) 21% chemo | EBRT: median dose: 63 Gy | median: 16 months | 23 months | 2 year LC = 56% | 2 year OS = 55%, MS = 24 months | Fibrosis: 38, trismus: 23%, cellulitis: 14%, fistula or wound: 9%, ORN 3%, trigeminal neuralgia: 3%, 2nd tumor: 3% |
| Chen et al. (2) | n = 37 (out of 99) | SGT (100%) | ≤2 cm: 28% 2.1–4 cm: 41% >4 cm: 30% |
SGT (100%) parotid most common (34%) | IOERT | 12–18 Gy | 15 Gy | 15% EBRT (54 Gy) 9% chemo | EBRT: median dose 60 Gy | 3.1 years | 3.7 years | 5 year LC: 82% (with IORT) and 60% (without IORT) | 3 year OS: 54%, 5 year OS: 34% (all). MS: 12 mo. (neck rec) vs. 20 months (primary site rec) | Superficial wound infection: 5%, trismus: 3%, Facial neuropathy: 3% |
| Chen et al. (4) | n = 137 d | OP, oral cavity, paranasal sinus, parotid. | ≤2 cm: 45% 2.1–4 cm: 33% >4 cm: 22% |
Local (64%); neck (28%); both (8%) | IOERT | NR | 15 Gy | 26% EBRT (54 Gy) 72% chemo | EBRT median dose: 64 Gy | 13 months | 18 months | 3 year in field control: 62% 3 year LRC 51% |
3 year OS: 36% (3-year OS: 44% primary rec compared with 19% neck rec) | Superficial wound infection: 3%, fistula: 1.5%, wound dehiscence: 0.7%, trismus: 0.7%, neuropathy: 0.7% |
| Pinheiro et al. (13) | n = 44 (34 SCC and 10 non-SCCd) | OP, oral cavity | NR | Skull base (56%) and neck (44%) | IOERT | 12.5–22.5 Gy | NR | NR | NR | NR | 6.3 years | 2 year LF: 54% (SCC) and 48% (non-SCC) | 2 year OS: 50% (non-SCC) and 32% (SCC) | Soft tissue: 11.3%, fistula: 6.8%, neuropathy: 11.3%, fatal hemorrhage: 2.2%, wound: 4.5% |
| Schleicher et al. (14) | n = 84 (113 sites) | Hypopharynx, larynx and OP | Median field size: 34 cm2 | Jugular chain (80%) | IOERT | 10–20 Gy | 20 Gy | 9.5%: chemo | EBRT: median dose: 56 Gy | median: 38.3 weeks | NR | LC: 24% R2, 41.7% R1, 50% R0 | MS = 6.8 months | Wound healing: 9%, 4%, salivary fistula: 3.5%, necrosis: 2% |
| Nag et al. (15) | n = 38 | Larynx and oral cavity | NR | Primary H&N site (29%), neck only (37%) | IOERT | 15 Gy: close or microscopically + margins, 20 for gross | 15 or 20 Gy | 0% EBRT | EBRT: median dose 65.1 Gy | NR | 30 months | 2 year LC = 13%, 2 year LRC: 4% | 2 year OS: 21%, 3 year OS: 8% | Comp.: 16%, orocutaneous fistula: 5%, fatal fistula, wound or tracheal dehiscence and carotid occlusion: 2.6% each |
| Martinez-Monge et al. (16) | n = 23 (31 total) | NR | NR | NR | IOERT | 10–15 Gy | NR | NR | EBRT: median dose 50 Gy | NR | NR | 2 year LRC: 26%: recurrent | 2 year OS: 31% (recurrent) | Comp.: 10% |
| Ling et al. (17) | n = 25 (out of 30 total) | NR | NR | NR | IOERT | 15 Gy | 15 Gy | NR | NR | NR | 30 months | 3 year LRC: 60% (for all) | 3 year OS: 70% (for all) | Comp.: 16% |
| Freeman et al. (18) | n = 52 (out of 75 total) | NR | >3 cm | Neck (100%) | IOERT | 10–25 Gy | 20 Gy | 33% EBRT (Dose NR) | EBRT: dose NR | NR | 2 years | 2 year LC: 68%: all patients | 2 year OS: 45% (all patients) | Comp.: 25% including carotid blowout, sepsis, ORN, PE, flap necrosis, MI and hypocalcemia |
| Toita et al. (19) | n = 17 (22 sites out of 24 total) | Oral cavity (46%) | NR | Neck (86%); primary (14%) | IOERT | 10–30 Gy | 20 Gy | 67% EBRT (41.2 Gy) | EBRT: 26–70 Gy range | NR | 19 months | 2 year LC: 54% allf GR: 0% MR: 55%, CM: 82% | 2 year OS: 45%; 0% GR, 33% MR, 70% CM (all) | Comp: 22%, carotid blowout: 3 patients, osteoradionecrosis (all more than or = 20 Gy): 4 sites |
| Freeman et al. (3) | n = 64 (out of 104 total) | Mucosa of UAD tract (71%), SGT (23%) | NR | Neck (35%), skull base (19%), parotid (17%) | IOERT | 15–20 Gy | 20 Gy: neck, 15 Gy: skull base, oral cavity and SG | NR | NR | NR | 2 years | 2 year LC: 40% (all) | NR | ORN: 6%, fistulas: 6%, carotid blowout: 3%, MI and PE: 3% |
IORT, intraoperative radiation therapy; IOERT, intraoperative electron radiation therapy; HDR IORT, high-dose brachytherapy; F/U, follow-up; LC, local control; IFLC, in-field local control; IFPFS, in-field progression-free survival; RFS, recurrence-free survival; OS, overall survival; SGT, salivary gland tumor; OP, oropharynx; SCC, squamous cell carcinoma; Comp., complications; ORN, osteoradionecrosis; EBRT, external beam radiation therapy; RT, radiation therapy; LRC, locoregional control.
aN: patients with recurrent tumors who received IORT.
b12 Gy: negative margins, 15–17.5 Gy for microscopically positive margins.
c1% LR in the IORT field, 20% regional, 13% distant in all.
dIt included primary and recurrent tumors.
eMedian field size, when available, is given when median tumor size is not reported.
fLC: 78% primary and 43% for neck.
Neck Recurrences
Intraoperative radiation therapy for neck recurrences is one of the most common IORT uses in head and neck tumors probably due to the difficulty of completely resecting recurrent tumors close to critical structures such as the carotid artery or due to fixation to deep tissues especially after fibrosis induced by previous irradiation. We previously reported one of the largest retrospective series on neck IORT (12); it included 231 patients with advanced cervical metastasis, 88% (198 patients) had recurrent tumors. All included patients had either microscopic or gross residual disease. Intraoperative electron radiation therapy (IOERT) with a median dose of 15–20 Gy was used. Postoperative EBRT was offered to 50 patients (21.6%). With a median follow-up of around a year, 5-year recurrence-free survival (RFS) and overall survival (OS) were 49 and 26%, respectively, for all included patients (12). Another study on neck IORT included 52 patients with recurrent tumors who received a median dose of 20 Gy of IOERT. With a median follow up of 2 years, 2-year local control (LC) and OS were 68 and 45%, respectively, for all 75 patients (18). Most of the other series on IORT for neck recurrences, listed in Table 1, included between 17 and 84 patients (10, 14, 15, 19). The majority used IOERT while two of the studies used high dose radiation brachytherapy known as HDR IORT. The median dose ranged from 12 to 20 Gy. Most used adjuvant EBRT in addition to IORT with a median dose range of 41–50 Gy. The 2-year in-field LC reached up to 62%. LC was higher in patients with gross total resection (GTR), where 2-year LC was 50–100% after GTR vs. 0–24% with gross residual disease. It was also higher for primary recurrences as compared to neck recurrences (LC: 100 vs. 75%, respectively). As for survival outcomes, in a study, by Teckie et al, on 57 patients who received 15 Gy of HDR IORT, 3-year OS reached 50% in patients who had in-field control vs. 32% in those not achieving in-field control (10). Survival was also superior for patients with clear margins; where 2-year OS reached 70% in patients with clear margins in a study by Toita et al. which included 17 patients with 22 treated sites (19). In summary, IORT, with a median dose of 15–20 Gy, results in very good LC in patients with neck recurrences and can improve survival outcomes, especially in those who attain negative surgical margins.
Primary Site Recurrences
Good outcomes have been also reported for recurrences at the primary site treated with IORT. Perry et al. presented a study on 34 patients that included salivary gland tumor (SGT) recurrences (21%) in addition to tumor recurrence at other head and neck the primary sites. Most of the patients had a history of irradiation with EBRT to a median dose of 63 Gy. Adjuvant EBRT at recurrence was given to 15% of the patients with a median dose of 50 Gy. With 10–20 Gy of HDR IORT, 2-year LC and 2-year OS were 56 and 55%, respectively (6). An earlier series by Nag et al. reported less favorable outcomes as compared to other listed studies. It included 38 patients, 29% of which were treated with IOERT for primary site recurrence. The dose was 15 Gy for close or microscopically positive margins and 20 Gy for gross disease. It is worth noting however that patients did not receive adjuvant EBRT in addition to IORT resulting in a 2-year LC and OS of 13 and 21%, respectively (15).
SGT Recurrences
Recurrent SGTs were addressed in two main studies, which included patients, treated with IOERT, with the parotid gland being the most common site. Patients in both studies had a history of irradiation (EBRT) with a median dose of 60 Gy. We reported on 46 patients with recurrent parotid tumors treated by 15–20 Gy IOERT in addition to EBRT in 54% (dose of 45 Gy) and chemotherapy in 19%. Favorable outcomes were observed with a relatively long follow-up of 5.6 years. For those with recurrent tumors, 5-year RFS and 5-year OS were both 48% (11). The second study included 37 patients with recurrent SGT who received a median dose of 15 Gy IOERT in addition to EBRT (54 Gy) in 15%. LC at 5 years was better with IORT compared to no IORT (82 vs. 60%) and 5-year OS was 34% for the entire sample (2).
Prognostic Factors
Most of the studies on IORT in the recurrent setting showed a significant correlation between in field control and margin status. Scala et al. reported that 1-year in-field control for patients with negative margins was 82% compared to 56% in those with a positive margin (9). At least five other studies also showed that positive margins (more so for gross residual than microscopic residual) at the time of IORT significantly predicted for in-field failure when compared to close or clear margins (2, 11, 13, 18, 19). In addition, doses of IORT of more than 15 Gy were shown to be associated with better LC (10, 12). Other prognostic factors for LC and RFS include pre-reirradiation recurrence-free interval of more than 12 months (10), use of adjuvant EBRT (9), absence of nodal extra-capsular extension (10), and tumor size (11). Furthermore, patients with neck metastasis who had no PNI, no LVSI, and no involvement of the carotid artery were reported to have better OS after IORT (12). Taken together, these results underscore the prognostic importance of surgical pathology details in addition to treatment dose in this patient cohort.
Locally Advanced (LA) Primary HNC
One of the potential benefits of intraoperative RT in LA HNC is minimization of the time interval between surgery and RT as studies have shown that delayed radiotherapy compromises LC outcomes (20, 21). The importance of IORT in LA HNC is in boosting microscopic or gross residual disease in close proximity to or extending to critical structures, in a setting where negative surgical margins cannot be achieved without significant morbidity. A larger volume is usually irradiated postoperatively using external beam radiation therapy (EBRT). IORT has the advantage of reducing the volume of the radiation boost field, allowing dose escalation to target tissue with selective shielding of sensitive structures.
IORT As a Boost to Primary HNC
The Methodist Hospital of Indiana introduced IORT for HNC in 1982 to improve on LC rates and select patients’ survival outcomes (3, 22). Few studies have examined the role of IORT in the primary HN setting exclusively. Most studies included patients with recurrent HNC, and most included a heterogeneous patient population with a wide variety of HNC disease sites. One of the first published studies by Garrett et al. reported on 28 patients with LA or recurrent HNC treated with surgery followed by IORT with 1-year OS rates of 67%. Indications for IORT in this study were as follows: (1) gross residual disease, (2) microscopic residual disease, or (3) close margins. In this series, all patients with residual gross disease recurred locally, whereas LC rates were 87 and 75% for close surgical margins and microscopic residual disease, respectively. The 43% of the patients received EBRT, in addition to IORT, with a median dose of 50 Gy. Carotid blowout was found to be a major treatment complication (in two patients). Results were not stratified by primary versus recurrent treatment (22). The same group at the Methodist Hospital of Indiana also reported on their experience with IORT in 104 patients with LA and recurrent HNCs (40 patients previously untreated, and the rest with recurrent disease). Patients were treated with surgery followed by IORT at a dose of 15–20 Gy. Some of the indications for IORT use were close surgical margins, fixation to the carotid sheath, deep muscles of the tongue, pre-vertebral fascia, extension to skull base or dura, or preservation of critical structures function, such as facial nerve. The percentage of patients who also received EBRT in addition to IORT was not reported. Results were promising, with 2-year LC rates of 54%, with better LC rates for parotid cancers (n = 19, 2-year LC = 69%) and tongue cancers (n = 16, 2-year LC = 57%) (3). Another small study by Freeman et al. included 25 patients with primary (n = 11) or recurrent (n = 14) tumors close to the skull base, who were treated with IORT for close surgical margins, or residual gross or microscopic disease, with LC rates of 64% at 1 year. The 36% of those patients also received postoperative EBRT (23). A third paper by Freeman et al., mentioned in the above section on neck recurrences, that studied 75 patients with advanced cervical lymph node metastases with 2-year LC and OS of 68 and 45%, respectively, included 22 patients with primary advanced untreated disease. This study did not report on the percent of patients also receiving adjuvant EBRT (18). These three studies with promising results paved the way for more single-institution studies.
In a study by Pinheiro et al., 44 patients with recurrent (n = 31) and LA (n = 13) HNCs (56% with skull base cancers) were treated with IORT at doses between 12.5 and 22.5 Gy, with around 50% tumor control rates overall. All patients with primary LA tumors received adjuvant EBRT (dose not reported) after IORT (13). Similar control rates were also documented in another study including 25 patients with mainly primary (n = 17) LA HNC treated with surgery and 12 Gy of IORT, with 2-year locoregional recurrence-free survival and disease-free survival rates of 58.5 and 50.6%, respectively (21). Nag et al. also studied 53 patients with primary HNC (out of 65 included patients) who were treated with 7.5–20 Gy intraoperative HDR brachytherapy to sites inaccessible to intraoperative electron beam radiotherapy, with 5-year LC rates of 59% and 5-year OS rates of 42%, and no major intraoperative or postoperative complications (24). Although the abovementioned studies have limitations inherent to their retrospective design, they all report LC rates of 50–68% at 2–5 years. It is worth noting that the majority of those studies do not report on adjuvant EBRT use.
Primary SGTs
Locally advanced SGT may involve or be in close contact with vital nerves or blood vessels within the head and neck. Adequate surgical margins might be difficult to attain in such a context. IORT might therefore be a good option in patients with salivary gland cancers at high risk of recurrence. The largest report of IORT in the multimodal management of patients with parotid cancers is a single-practice experience, which included 96 patients with primary (50 patients) or recurrent (46 patients) parotid cancers treated between 1982 and 2007 (11). In this study, 5-year recurrence-free survival (RFS) rates were 77.8% and OS rates were 65.7% for patients treated in the primary setting with IORT boost dose of 15–20 Gy using 4–6 MeV electrons. Larger tumor size was predictive of recurrence after IORT, and patient age was predictive of survival on multivariate analysis. These results have to be put into perspective, as other RT modalities were tried in the management of LA parotid cancers with promising results. The use of fast neutron RT yielded 5-year locoregional control (LRC) rates of 92 and 63% in patients treated with RT alone (without surgery), and with postoperative RT for gross residual disease, respectively (25). Garden et al. also reported LRC of 85% with the use of postoperative EBRT in patients with malignant tumors of the parotid gland (26). Taken together, these studies demonstrate that IORT could be considered as an option in multimodal management of patients with primary HNC, to address gross or microscopic residual disease in a setting where complete resection would be too morbid due to proximity to a major vessel or critical nerve, or as a boost for traditionally radioresistant tumors, such as SGT.
Toxicity of IORT
Intraoperative radiation therapy-related complications rate reported in the literature (Table 1) ranges between 22 and 52% in both the primary and recurrent setting (11–13, 18, 19, 27). Early studies by Toita et al. reported a significant increase in the rate of toxicities with doses exceeding 20 Gy (19), whereas other studies failed to show significant changes in toxicity rates with different doses (10, 12). Of the several reported complications, carotid artery rupture incidence ranged between 2 and 5% (3, 13, 18) and up to 10% in older series (19). Carotid blow out is a treatment complication associated with the highest mortality rates. Fistula/abscess rate ranged between 4 and 15% (3, 4, 10–12, 14, 18, 27). Wound related toxicity from cellulitis to flap necrosis ranged from 0 to 12% (2–4, 6, 10–12, 14, 27). Osteoradionecrosis rates are reported to range from 0 to 13% (3, 4, 6, 11, 12, 14, 19). Furthermore, some studies report on treatment related neuropathy ranging from 1 to 3% and mostly treated by symptomatic pain management (2, 4, 6, 11–13). Of note, higher neuropathy rates were noted in a study from MSKCC reporting the outcomes of 57 patients with recurrent tumors, where neuropathy rates reached 26%, trismus rate of 24%, and fibrosis rate of 29% (10). Similar rates of trismus and fibrosis, 28 and 23% respectively, were reported from MSKCC in another retrospective study of 34 patients with recurrent disease (6). It is worth mentioning, however, that the above studies used different toxicity scales and had variable median follow up. Taken together, IORT in experienced centers has reasonable toxicity profile, and does not increase perioperative mortality (2, 4, 5, 11, 12) or hospital length-of-stay (5).
Radiobiology of IORT
Using IORT in different clinical settings, including HNCs, is well grounded in several well-known radio-biologic principles. IORT provides a significant dose–response relationship advantage with the high dose given in a single IORT fraction having 1.5–2.5 times the biological effectiveness of the same dose given at standard fractionation (28). While it is debatable to rely solely on the linear quadratic model at very high doses, there is little doubt that tumor cell survival is significantly reduced when using a higher dose per fraction as compared to conventional fractionation. Moreover, there remains a need to better evaluate the effects radio-sensitizing compounds may have on normal tissue tolerances as well as tumor cell survival in the IORT setting (29).
Despite the efforts made intraoperatively to decrease the treatment volume, provide adequate retraction, and adequate shielding, the high fraction dose that is used during IORT does not give ample time for normal tissue repair. This may contribute to vessel injury, neuropathies, fibrosis, and other late effects in surrounding healthy tissues (30, 31). However, the quick drop off in dose with IORT HDR may help prevent treating critical structures surrounding the post-op bed to high dose. Regardless of treatment modality (photons/electrons or brachytherapy), treating residual tumor cells with radiation during surgery as opposed to days or weeks postoperatively reduces the disadvantageous role of tumor cell re-population. Also, it is well established that ischemic tumor areas may be more resistant to radiation treatment due to the paucity of oxygen fixing DNA damage caused by free radicals, and thus, a single high IORT dose does not provide ample time for tumor re-oxygenation. However, it is quite likely that the effect of this unfavorable ischemic milieu is counterbalanced by the single high IORT dose, when compared to standard external beam fractionation (12, 31). Moreover, there is evidence to suggest that high dosage of radiation in a single fraction can eradicate cancer stem cells that would have been radioresistant at standard fractionation and has even been theorized to have implications in unleashing favorable immune responses such as the abscopal effect (32, 33). Therefore, IORT has a promising role from a radiobiology perspective, in improving LC after resection of primary or recurrent HNCs.
Modalities for IORT
Intraoperative radiation therapy can be delivered using several techniques and modalities that optimize target dose while minimizing it to the surrounding tissues. HDR brachytherapy, and electron and photon IORT are methods for this localized delivery of dosage. While harboring several similarities, the physics and radiobiology involved generally display a broad variance among the modalities and allow for suitable selections tailored for different HNC patients. Employing these tools correctly plays a particularly critical role in HNCs where surgical management of certain territories may be constrained by essential tissues or adjacent vascular components.
High-dose rate IORT allows the administration of focused radiation in regions where an EBRT cone is not appropriate (34). Application consists of placing a high activity source in close physical proximity to the post-surgical tumor bed while retracting or shielding adjacent structures. Treatment times typically elapse 15–60 min, allowing for treatment during a surgical procedure in a shielded room (35). HDR IORT offers strict spatial restriction of the administered dose, owing to the sharp fall in the inverse square function at short distances from the HDR source, resulting in relatively very little dose delivered beyond the prescribed 100% isodose line (36).
Although HDR IORT offers several advantages in tumor bed management, electron (IOERT) or photon IORT on the other hand provide optimal flexibility for a wide range of treatment sites. These forms of IORT may be delivered using radiation at different energies (37). At the present time, external beam IORT is administered by a dedicated linear accelerator with parallel electron beams of 3–12 MeV kinetic energy or isotropic photon fields with energies between contact and superficial therapy of 50 kV X-rays (38). Such low photon energy beams (e.g., Intrabeam® by Carl Zeiss AG, Germany) have demonstrated favorable outcomes in some sites but with many questions remaining unanswered (39, 40).
Challenges and Future Directions in IORT for HNC
Although IORT has emerged as a feasible modality in management of HNC, several challenges warrant further investigation. First, the efficacy of IORT needs to be further evaluated in randomized phase III trials. Due to paucity of radiotherapy centers with IORT equipment, this is best conducted via multicenter cooperative groups such as International Society of Intraoperative Radiation Therapy. Second, there needs to be professional guidelines describing IORT workflow and coordination between surgical and radiation specialties. Third, the therapeutic window for IORT in HNC patients needs to be further improved by using small molecule adjuncts that radiosensitize tumor cells and/or further protect normal tissues. Recent research efforts cast a promising future for HNC IORT (Figure 1) (28). For instance, the introduction of IOERT treatment planning system (41) affords accurate documentation of target and normal tissues dose distribution. This is anticipated to yield improved target coverage and better documentation of normal tissue doses.
Figure 1.
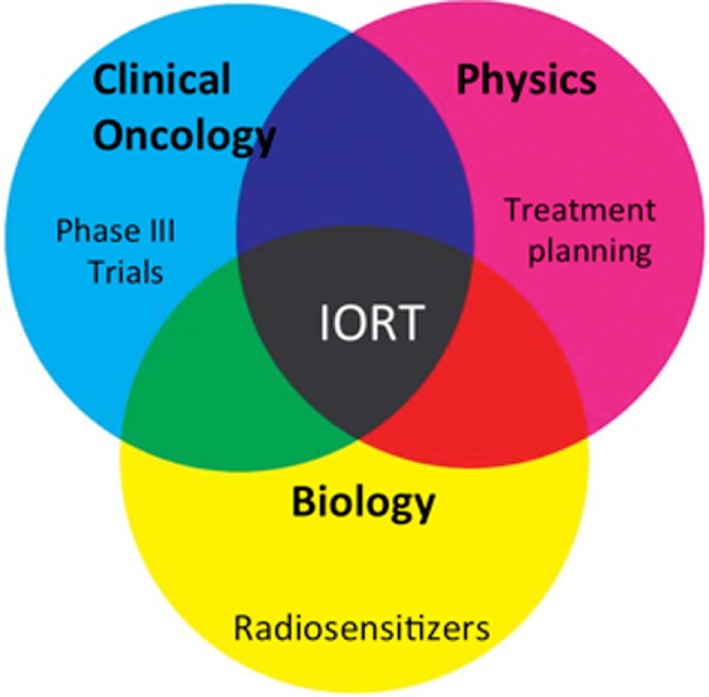
Summary of future directions. Phase III trials (clinical), treatment planning (physics), and radiosensitizers (biology) are at the forefront of current intraoperative radiation therapy research efforts.
Finally, assuring radiation safety when using IORT in the OR is a major concern. Typical stray doses from IORT at a 1 m distance from the patient are around 6 µSv per Gy of patient dose (42). Radiation safety regulations usually require shielding which reduces dose below the permitted constraints at any position around the OR under the assumption that the highest dose of stray radiation occurs in the direction of the beam during the complete workload. This need for structural shielding could be reduced by the possible use of mobile shielding walls (43). For example, in a study from Poland by Rabin et al., they calculated that it is sufficient to have mobile lead shield parameters of 1 cm × 140 cm × 150 cm between the accelerator in the OR and the control room to have the dose distribution in the patient plane meet radiation protection requirements (44). However, some authorities might object to mobile shielding due to the lack of control of correct placement by the personnel. A possible future solution might be the development of interlocked systems, which permit irradiation only if the crucial directions around the accelerator are adequately protected by correctly positioning the mobile shields (43).
Conclusion
Intraoperative radiation therapy has emerged as an effective modality for HNC patients at high risk for local failure. To date, most of the scientific literature on head and neck IORT remains by and large limited to single institutional experiences. Recent technological advances and the advent of new IORT platforms predict an expansion of radiotherapy centers offering IORT. This is anticipated to accelerate opening of multi-institutional clinical trials in order to refine indications for IORT in HNC patients.
Author Contributions
LH and YZ outlined the manuscript. LH added Table 1. LH, KF, IG, PR, J-PO, and YZ wrote the sections of the manuscript. FG, BY, and WJ reviewed and edited the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.American Cancer Society. Cancer Facts & Figures 2016. Atlanta, GA: American Cancer Society; (2016). [Google Scholar]
- 2.Chen AM, Garcia J, Bucci MK, Chan AS, Kaplan MJ, Singer MI, et al. Recurrent salivary gland carcinomas treated by surgery with or without intraoperative radiation therapy. Head Neck (2008) 30(1):2–9. 10.1002/hed.20651 [DOI] [PubMed] [Google Scholar]
- 3.Freeman SB, Hamaker RC, Singer MI, Pugh N, Garrett P, Ross D. Intraoperative radiotherapy of head and neck cancer. Arch Otolaryngol Head Neck Surg (1990) 116:165–8. 10.1001/archotol.1990.01870020041011 [DOI] [PubMed] [Google Scholar]
- 4.Chen AM, Bucci MK, Singer MI, Garcia J, Kaplan MJ, Chan AS, et al. Intraoperative radiation therapy for recurrent head-and-neck cancer: the UCSF experience. Int J Radiat Oncol Biol Phys (2007) 67:122–9. 10.1016/j.ijrobp.2006.08.038 [DOI] [PubMed] [Google Scholar]
- 5.Haller JR, Mountain RE, Schuller DE, Nag S. Mortality and morbidity with intraoperative radiotherapy for head and neck cancer. Am J Otolaryngol (1996) 17:308–10. 10.1016/S0196-0709(96)90016-2 [DOI] [PubMed] [Google Scholar]
- 6.Perry DJ, Chan K, Wolden S, Zelefsky MJ, Chiu J, Cohen G, et al. High-dose-rate intraoperative radiation therapy for recurrent head-and-neck cancer. Int J Radiat Oncol Biol Phys (2010) 76(4):1140–6. 10.1016/j.ijrobp.2009.03.025 [DOI] [PubMed] [Google Scholar]
- 7.NCCN. Head and Neck Cancer. (2017). Available at: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf
- 8.Janot F, de Raucourt D, Benhamou E, Ferron C, Dolivet G, Bensadoun R-J, et al. Randomized trial of postoperative reirradiation combined with chemotherapy after salvage surgery compared with salvage surgery alone in head and neck carcinoma. J Clin Oncol (2008) 26:5518–23. 10.1200/JCO.2007.15.0102 [DOI] [PubMed] [Google Scholar]
- 9.Scala LM, Hu K, Urken ML, Jacobson AS, Persky MS, Tran TN, et al. Intraoperative high-dose-rate radiotherapy in the management of locoregionally recurrent head and neck cancer. Head Neck (2013) 35:485–92. 10.1002/hed.23007 [DOI] [PubMed] [Google Scholar]
- 10.Teckie S, Scala LM, Ho F, Wolden S, Chiu J, Cohen GN, et al. High-dose-rate intraoperative brachytherapy and radical surgical resection in the management of recurrent head-and-neck cancer. Brachytherapy (2013) 12:228–34. 10.1016/j.brachy.2013.01.165 [DOI] [PubMed] [Google Scholar]
- 11.Zeidan YH, Shiue K, Weed D, Johnstone PA, Terry C, Freeman S, et al. Intraoperative radiotherapy for parotid cancer: a single-institution experience. Int J Radiat Oncol Biol Phys (2012) 82:1831–6. 10.1016/j.ijrobp.2011.02.033 [DOI] [PubMed] [Google Scholar]
- 12.Zeidan YH, Yeh A, Weed D, Terry C, Freeman S, Krowiak E, et al. Intraoperative radiation therapy for advanced cervical metastasis: a single institution experience. Radiat Oncol (2011) 6:72. 10.1186/1748-717X-6-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinheiro AD, Foote RL, McCaffrey TV, Kasperbauer JL, Bonner JA, Olsen KD, et al. Intraoperative radiotherapy for head and neck and skull base cancer. Head Neck (2003) 25:217–25; discussion 225–6. 10.1002/hed.10203 [DOI] [PubMed] [Google Scholar]
- 14.Schleicher UM, Phonias C, Spaeth J, Schlöndorff G, Ammon J, Andreopoulos D. Intraoperative radiotherapy for pre-irradiated head and neck cancer. Radiother Oncol (2001) 58(1):77–81. 10.1016/S0167-8140(00)00297-8 [DOI] [PubMed] [Google Scholar]
- 15.Nag S, Schuller DE, Martinez-Monge R, Rodriguez-Villalba S, Grecula J, Bauer C. Intraoperative electron beam radiotherapy for previously irradiated advanced head and neck malignancies. Int J Radiat Oncol Biol Phys (1998) 42:1085–9. 10.1016/S0360-3016(98)00289-2 [DOI] [PubMed] [Google Scholar]
- 16.Martinez-Monge R, Azinovic I, Alcalde J, Aristu J, Paloma V, Garcia-Tapia R, et al. IORT in the management of locally advanced or recurrent head and neck cancer. Front Radiat Ther Oncol (1997) 31:122–5. 10.1159/000061179 [DOI] [PubMed] [Google Scholar]
- 17.Ling SM, Roach M, III, Fu KK, Coleman C, Chan A, Singer M. Local control after the use of adjuvant electron beam intraoperative radiotherapy in patients with high-risk head and neck cancer: the UCSF experience. Cancer J Sci Am (1996) 2:321–9. [PubMed] [Google Scholar]
- 18.Freeman SB, Hamaker RC, Rate WR, Garrett PG, Pugh N, Huntley TC, et al. Management of advanced cervical metastasis using intraoperative radiotherapy. Laryngoscope (1995) 105:575–8. 10.1288/00005537-199506000-00003 [DOI] [PubMed] [Google Scholar]
- 19.Toita T, Nakano M, Takizawa Y, Sueyama H, Kakihana Y, Kushi A, et al. Intraoperative radiation therapy (IORT) for head and neck cancer. Int J Radiat Oncol Biol Phys (1994) 30:1219–24. 10.1016/0360-3016(94)90332-8 [DOI] [PubMed] [Google Scholar]
- 20.Ang KK, Trotti A, Brown BW, Garden AS, Foote RL, Morrison WH, et al. Randomized trial addressing risk features and time factors of surgery plus radiotherapy in advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys (2001) 51:571–8. 10.1016/S0360-3016(01)01690-X [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal DI, Liu L, Lee JH, Vapiwala N, Chalian AA, Weinstein GS, et al. Importance of the treatment package time in surgery and postoperative radiation therapy for squamous carcinoma of the head and neck. Head Neck (2002) 24:115–26. 10.1002/hed.10038 [DOI] [PubMed] [Google Scholar]
- 22.Garrett P, Pugh N, Ross D, Hamaker R, Singer M. Intraoperative radiation therapy for advanced or recurrent head and neck cancer. Int J Radiat Oncol Biol Phys (1987) 13:785–8. 10.1016/0360-3016(87)90300-2 [DOI] [PubMed] [Google Scholar]
- 23.Freeman SB, Hamaker RC, Singer MI, Pugh N, Garrett P, Ross D. Intraoperative radiotherapy of skull base cancer. Laryngoscope (1991) 101:507–9. 10.1288/00005537-199105000-00011 [DOI] [PubMed] [Google Scholar]
- 24.Nag S, Koc M, Schuller DE, Tippin D, Grecula JC. Intraoperative single fraction high-dose-rate brachytherapy for head and neck cancers. Brachytherapy (2005) 4:217–23. 10.1016/j.brachy.2005.06.002 [DOI] [PubMed] [Google Scholar]
- 25.Buchholz TA, Laramore GE, Griffin TW. Fast neutron radiation for recurrent pleomorphic adenomas of the parotid gland. Am J Clin Oncol (1992) 15:441–5. 10.1097/00000421-199210000-00009 [DOI] [PubMed] [Google Scholar]
- 26.Garden AS, el-Naggar AK, Morrison WH, Callender DL, Ang KK, Peters LJ. Postoperative radiotherapy for malignant tumors of the parotid gland. Int J Radiat Oncol Biol Phys (1997) 37:79–85. 10.1016/S0360-3016(96)00464-6 [DOI] [PubMed] [Google Scholar]
- 27.Marucci L, Pichi B, Iaccarino G, Ruscito P, Spriano G, Arcangeli G. Intraoperative radiation therapy as an “early boost” in locally advanced head and neck cancer: preliminary results of a feasibility study. Head Neck (2008) 30:701–8. 10.1002/hed.20777 [DOI] [PubMed] [Google Scholar]
- 28.Calvo FA, Meirino RM, Gunderson LL, Willet CG. Intraoperative radiation therapy. In: Perez CA, Brady LW, Halperin EC, Schmidt-Ullrich RK. editors. Principles and Practice of Radiation Oncology. Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokio: Lippincott Williams & Wilkins; (2003). [Google Scholar]
- 29.Calvo FA, Sole CV, Gonzalez ME, Tangco ED, Lopez-Tarjuelo J, Koubychine I, et al. Research opportunities in intraoperative radiation therapy: the next decade 2013–2023. Clin Transl Oncol (2013) 15:683–90. 10.1007/s12094-013-1019-z [DOI] [PubMed] [Google Scholar]
- 30.Calvo FA, Meirino RM, Orecchia R. Intraoperative radiation therapy first part: rationale and techniques. Crit Rev Oncol Hematol (2006) 59:106–15. 10.1016/j.critrevonc.2005.11.004 [DOI] [PubMed] [Google Scholar]
- 31.Czito BG, Calvo FA, Haddock MG, Palta M, Willett CG. Intraoperative irradiation. In: Gunderson L, Tepper J, editors. Clinical Radiation Oncology. 4th ed. Philadelphia, PA: Elseiver; (2016). p. 325–40.e3. [Google Scholar]
- 32.Kirkpatrick JP, Meyer JJ, Marks LB. The linear-quadratic model is inappropriate to model high dose per fraction effects in radiosurgery. Semin Radiat Oncol (2008) 18:240–3. 10.1016/j.semradonc.2008.04.005 [DOI] [PubMed] [Google Scholar]
- 33.Sologuren I, Rodríguez-gallego C, Lara PC. Immune effects of high dose radiation treatment: implications of ionizing radiation on the development of bystander and abscopal effects. Transl Cancer Res (2014) 3:18–31. 10.3978/j.issn.2218-676X.2014.02.05 [DOI] [Google Scholar]
- 34.Moningi S, Armour EP, Terezakis SA, Efron JE, Gearhart SL, Bivalacqua TJ, et al. High-dose-rate intraoperative radiation therapy: the nuts and bolts of starting a program. J Contemp Brachytherapy (2014) 6:99–105. 10.5114/jcb.2014.42027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Furhang EE, Sillanpaa JK, Hu KS, Harrison LB. HDR-IORT: physics and techniques. In: Gunderson LL, Willett CG, Calvo FA, Harrison LB, editors. Intraoperative Irradiation: Techniques and Results. Totowa, NJ: Humana Press; (2011). p. 73–84. [Google Scholar]
- 36.Crownover RL, Wilkinson DA, Weinhous MS. The radiobiology and physics of brachytherapy. Hematol Oncol Clin North Am (1999) 13:477–87. 10.1016/S0889-8588(05)70069-1 [DOI] [PubMed] [Google Scholar]
- 37.Herskind C, Ma L, Liu Q, Zhang B, Schneider F, Veldwijk MR, et al. Biology of high single doses of IORT: RBE, 5 R’s, and other biological aspects. Radiat Oncol (2017) 12:24. 10.1186/s13014-016-0750-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kalakota K, Small WJ. Intraoperative radiation therapy techniques and options for breast cancer. Expert Rev Med Devices (2014) 11:265–73. 10.1586/17434440.2014.882653 [DOI] [PubMed] [Google Scholar]
- 39.Deneve JL, Hoefer RAJ, Harris EER, Laronga C. Accelerated partial breast irradiation: a review and description of an early North American surgical experience with the intrabeam delivery system. Cancer Control (2012) 19:295–308. [DOI] [PubMed] [Google Scholar]
- 40.Strnad V. Intraoperative radiotherapy (IORT) with 50-kV X-ray machines as boost in breast cancer – more questions than answers. Onkologie (2006) 29:73–5. 10.1159/000091475 [DOI] [PubMed] [Google Scholar]
- 41.Pascau J, Santos Miranda JA, Calvo FA, Bouche A, Morillo V, Gonzalez-San Segundo C, et al. An innovative tool for intraoperative electron beam radiotherapy simulation and planning: description and initial evaluation by radiation oncologists. Int J Radiat Oncol Biol Phys (2012) 83:e287–95. 10.1016/j.ijrobp.2011.12.063 [DOI] [PubMed] [Google Scholar]
- 42.Soriani A, Felici G, Fantini M, Paolucci M, Borla O, Evangelisti G, et al. Radiation protection measurements around a 12 MeV mobile dedicated IORT accelerator. Med Phys (2010) 37:995–1003. 10.1118/1.3298012 [DOI] [PubMed] [Google Scholar]
- 43.Hensley FW. Present state and issues in IORT physics. Radiat Oncol (2017) 12:37. 10.1186/s13014-016-0754-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wysocka-Rabin A, Adrich P, Wasilewski A. Radiation protection studies for a new mobile electron accelerator for intraoperative radiation therapy (IORT). Prog Nucl Sci Technol (2014) 4:298–302. 10.15669/pnst.4.298 [DOI] [Google Scholar]


