Editor’s Note:
Much is yet to be discovered about the precise biological changes that cause Alzheimer’s, disease, why it progresses more quickly in some than in others, and how the disease can be prevented, slowed, or stopped. And while researchers continue to search for the magic pill that can prevent or halt the spread of amyloid in the brain, our authors believe that changing or modifying one’s lifestyle and attitude can make a difference in both prevention and treatment.
Memory problems come in all shapes and sizes. Some people tend to forget where they put their cell phone, or cannot easily recall names. Or they can’t recall taking their medication or remember the birthday or anniversary of a loved one. Whether they admit to themselves that their forgetfulness seems to happen with greater frequency or they worry about losing their memory as they age, they are right to be concerned. Because our aging population is on the rise, Alzheimer’s disease (AD)—an irreversible, progressive form of dementia that slowly destroys memory and thinking skills as people age and is ultimately fatal—has steadily risen from about 4 million in the late 1990s to 5.4 million today.1
The disease is currently ranked as the sixth leading cause of death in the US, but estimates by the National Institute on Aging indicate that it may rank third, just behind heart disease and cancer, as a cause of death for older people.2 But here is some good news: Whether you want to reverse cognitive deficits now or avoid them later, more and more studies are suggesting that there is much you can do to keep your mind sharp.
While a pharmaceutical approach to preventing AD has proved elusive, practical lifestyle choices to reduce AD are based on good science and good sense. The secret may lie in epigenetics, the effect one’s lifestyle has on one’s genes, and thus on the risk for disease. Of course, the wisdom that lifestyle has an impact on health is not new; we have been reciting adages such as “an apple a day keeps the doctor away” for ages. Research in a variety of areas has confirmed that sensible everyday choices can significantly reduce the risk of AD. According to the National Institutes of Health, $991 million was dedicated to AD research in 2016, but how much of that went towards lifestyle-modification and prevention is unclear.3
Funding uncertainty notwithstanding, the positive effects of a healthier lifestyle on cognition were recently documented for the first time in a longitudinal study. The two-year, 1,200 participant Finnish Interventional Geriatric Study for the Prevention of Cognitive Disability (FINGER) showed that a healthy diet, exercise, socialization, and mental stimulation can dramatically reduce the development of AD in people at risk for cognitive decline.4 The French MAPT Study: A Multidomain Approach for Preventing Alzheimer’s Disease also suggested that lifestyle modification has an effect in reducing risk factors.5 This multi-domain approach is consistent with the four-pillar strategy recommended by a number of reputable sources, including the Alzheimer’s Research and Prevention Foundation (ARPF), the Dana Alliance, the American Association of Retired Persons, and the Alzheimer’s Association.
The aforementioned studies add substantially to mounting scientific evidence that suggests lifestyle and psychological well-being play a critically important role in Alzheimer’s prevention. We have taken them into account, along with our own findings, in fine-tuning our longstanding recommendations for staving off and even helping to reverse AD to the following four strategies. The secret to AD prevention is tied to maintaining connections: between your brain cells, other people, and your well-being.
Pillar 1: Diet and Supplements
Diet is one of the most important targets for lifestyle modification to prevent AD. Many people still blindly follow the Standard American Diet, or SAD. According to the US Government, about 75 percent of all Americans do not consume an adequate amount of vegetables and fruits, while most exceed the recommended amount of sugars, saturated fats, sodium, and calories. Studies show that rejecting SAD may be critical in the fight against AD.6
The science reveals that those who eschew processed foods and choose whole, real-food options have the least decline in mental faculty. Research published in the Alzheimer’s Association’s journal Alzheimer’s & Dementia, for example, confirms that making the switch from a fat- and meat-heavy way of eating to a primarily plant-based diet—no matter how old a person is when doing so— can slow and possibly reverse memory loss. The components of a healthy diet may enhance cognitive performance by one or more of several actions: affecting synaptic plasticity, synaptic membrane fluidity, glucose utilization, mitochondrial function, or reducing oxidative stress.7
Many studies highlight the Mediterranean diet that is rich in vegetables, fruit, nuts, olive oil, and fish or seafood. Researchers at UCLA discovered that study participants who followed this eating plan, which is modeled on the traditional diet of certain Mediterranean peoples, had lower levels of AD’s hallmark amyloid-beta plaques in the spaces between their brain nerve cells, along with fewer telltale tangles of tau protein—meaning those important cell connections were firing properly.8 And at the Mayo Clinic, through MRI scans, researchers found that participants who followed the Mediterranean diet for a year had greater thickness in parts of their brain’s cortex that play a role in memory. Those on the SAD diet, on the other hand, lost cortex. These findings have implications for maintaining cognitive function: positive associations of the Mediterranean Diet scores were observed with average cortical thickness in parietal and frontal lobes, and in regions of the brain that mediate or support elements such as memory, executive function, and language.9 Americanized versions of the Mediterranean diet, as well as the MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) and DASH (Dietary Approaches to Stop Hypertension) diets, have also shown promising results. Research from Rush University, where the MIND diet was developed by nutritional epidemiologist Martha Clare Morris, revealed that the MIND diet could turn back your mental aging clock the equivalent of up to 7.5 years. Although this is now widely accepted by researchers, further confirmative studies are ongoing.10
The ARPF nutrition plan has much in common with both the Mediterranean and MIND diets. Some of the organization’s main tenets are:
Vegetarian foods: A vegetarian diet—full of fruits and vegetables, nuts and seeds, legumes and soy—improves focus and begets higher productivity. Wild-caught salmon is the only animal protein the Alzheimer’s Research & Prevention Foundation’s diet recommends for its brain-friendly omega-3 fats, advising eating it only two to three times a week.
Juicing: Fresh juices are alive with the vitamins, minerals, trace elements, and phytonutrients needed to strengthen the brain.
Supplements: Take a high-potency multivitamin and multi-mineral supplement that includes folic acid. Memory specific supplements of omega-3 oils, phosphatidyl-serine, coenzyme Q10, alpha lipoic acid, huperzine-A, and resveratrol are also recommended.
As previously noted, we suspect that certain genes can influence risk of developing AD. But well-chosen foods and their nutrients may move gene expression toward a sharp brain. “Genetics are not our destiny,” says Victor S. Sierpina, M.D., professor of family and integrative medicine at the University of Texas Medical Branch in Galveston. “How we eat can have a major impact in reducing our risk of developing this feared condition.” By moving away from the SAD diet to a more Mediterranean-type diet, it is possible to eat for optimal brain health.
Pillar 2: Physical and Mental Exercise
The evidence is convincing: Both physical and mental exercise are absolutely essential in preventing AD. Exercise increases blood flow to the brain, augments crucial brain compounds such as brain-derived neurotrophic factor (BDNF), and, perhaps most significantly, causes neurogenesis, or the growth of new brain cells. In a study at Columbia University, researchers showed that older men who exercised on a treadmill four times a week for 30 minutes grew new cells in their dentate gyrus, an important area of the brain related to memory and cognition such as executive function.11 And guess what? One can experience these brain-boosting effects of exercise regardless of one’s age or existing level of fitness or cognitive decline.
Current wisdom recommends 150 minutes a week of cardio (aka aerobic) exercise, plus several sessions of strength training. But the benefits of even mild exercise begin to accrue right away. Just getting out and taking a 20 to 30- minute brisk walk three times a week will improve brain and memory function. Like diet, exercise also creates a healthy epigenetic response. Those who are already in good physical condition should add more variety and intensity to their workouts. Get a trainer, join a gym, play tennis, swim, or take a boot camp, Zumba, or cycling class. Find enjoyable activities and make them part of your routine.
Additionally, keeping one’s mind active is an important aspect of AD prevention. There are a variety of ways to do this. One of them, reading, is one of the best ways to stay sharp—not only does learning take place, but the mind is forced to think and engage outside of everyday tasks. Other simple strategies—or what are sometimes called brain-aerobic activities—include playing and listening to music, creating and viewing art, or completing crossword puzzles. All stimulate and challenge the brain, giving it a nice “workout.” Remember, it’s not just about physical fitness, it’s about mental conditioning as well.
Pillar 3: Yoga/Meditation
Chronic stress is a major risk factor for AD.12 It may be useful to experience stress if one is running for his or her life, but not when just trying to live one’s life. Stress has a detrimental effect on genes, causing them to express themselves in unhealthy ways, such as by producing inflammation, a trademark of AD. The frenzied pace of life that people experience in today’s world is only accelerating, so it is helpful to find a regular activity to soothe the harmful force of stress on the brain.
Published research over the past 13 years reveals that a simple, 12-minute yoga/meditation technique called Kirtan Kriya (KK) has significant brain boosting benefits. KK has been examined at leading medical schools, with the impressive, perhaps surprising, results published in more than one medical journal, including the Journal of Alzheimer’s Disease.13
The actual age of KK is unknown. It was passed down from master to student for generations in the East until Yogi Bhajan (1929–2004) brought it to the West in about 1970. Kirtan means “singing” and Kriya means “an action with specific effects.” KK involves singing the sounds Saa Taa Naa Maa (a mantra) while repeating sequential movements (mudras) with the fingertips.
Ancient yogis did not have imaging or blood tests to unravel the biochemical changes created by KK and other yoga exercises, but modern science has shown that practicing KK reduces stress levels and increases blood flow to parts of the brain that are central to memory and brain function.14 For example, KK activates the anterior cingulate gyrus (ACG), an important brain region for stress balance and emotional and cognitive control. A robust ACG is essential to memory: Research in the elderly who’ve maintained sharp minds shows they have preserved their ACGs and other significant brain areas as they have aged.15
The prefrontal cortex (PFC), the chief executive officer of your brain, essential for planning and organization, is also activated by meditation. So is the posterior cingulate gyrus (PC), one of the first areas to decline in function when memory loss strikes. Such findings have led Andrew Newberg, M.D., of Thomas Jefferson Medical School, to say, “There is a true anti-aging effect in long-term practitioners of KK; they have bigger brains.”
A study at the University of Pennsylvania, which followed people with early cognitive decline for eight weeks, demonstrated that practicing the yoga/meditation technique started reversing memory loss and reduced anxiety, two hallmarks of early AD.16 A UCLA study of family dementia caregivers revealed that KK not only lowered their stress and improved their memory, but also reduced inflammatory genes and increased the enzyme telomerase by 43 percent, the largest increase ever recorded. Increasing this enzyme elongates the DNA protective cap, the telomere, which is crucial for a long life and a sharp mind.17
Additionally, at West Virginia University, subjects with the earliest form of memory loss, subjective cognitive decline (SCD), showed an improvement in cognitive function with KK.18 And a landmark study at UCLA found that subjects with an advanced form of early memory loss called mild cognitive impairment (MCI) had better memory outcomes with KK than those who practiced a standard memory-improvement approach.19 KK apparently enhanced brain cell connectivity as well. Importantly, the positive benefits lasted through the six-month follow up period of the study.20
KK has practical advantages. It only takes 12 minutes a day and requires no equipment or lengthy or expensive training sessions. One can practice KK at home with an easy-to-follow CD, for example, and it is completely safe, with no side effects reported. Its lack of time requirements makes the practice perfect for caregivers, and it’s easy for seniors with decreased mobility and activity levels.
Pillar 4: Psychological Well-Being
Meditation also enhances psychological well-being (PWB) by promoting acceptance of self and others, increasing self-confidence, reducing negativity, and providing a foundation for independent living, sustained personal growth, socializing with like-minded people, service to others, and aging with purpose. These PWB factors lower the risk for cognitive decline and help reduce cholesterol and inflammation.21 In fact, Purpose in Life is a new movement in neuroscience that links the belief that one’s life has meaning and purpose to a robust and persistently improved physiological health outcome—not only to treat AD, but also to treat spinal cord injuries, stroke, and immunological and cardiovascular issues that include but extend beyond the brain.22
Positive emotions—love, compassion, and appreciation—counteract the physiology of the stress response and support a healthy brain throughout life. Beyond that, PWB may create an enhanced sense of spirituality, which preliminary studies suggest slows the progression of AD.23 Moreover, per Helen Lavretsky, M.D., a geriatric psychiatrist at UCLA, spirituality is a way to develop personalized, patient-centered healthcare. There is evidence of a close relationship between spirituality, cognitive health, and successful aging.24 Finally, in a very recent, and as of yet, unpublished three-year study, spirituality was associated with lowered atrophy rates in brain regions related to memory, visuospatial attention, and behavioral deficits in subjects at risk for AD.25
As it currently stands, or until the pharmaceutical world can meet the enormous challenge of discovering the magic anecdote that can make amyloid disappear, living a healthy life offers the best chance for aging AD-free and nourishing a sharp mind. Small, easily achieved shifts in one’s daily routine can make all the difference in brain health. If everyone made such shifts, it is likely that the widespread prediction of a continuing Alzheimer’s epidemic would shift, too, with fewer reported cases.
Figure 1.
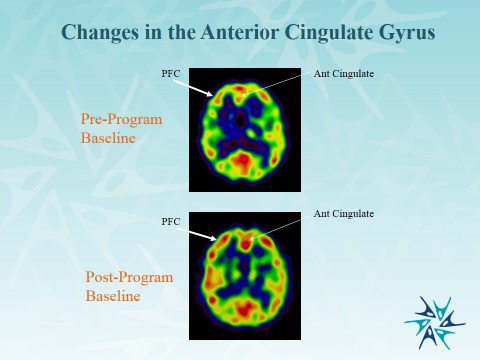
Increased Size of PFC and ACG after Eight Week Program of 12 Minutes a day of KK.13 (Courtesy of the Alzheimer’s Research and Prevention Foundation.)
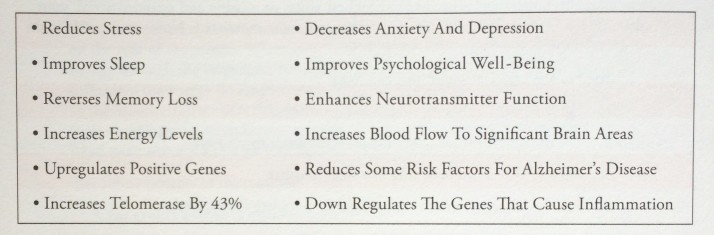
Figure 2.
A summary of the effects of KK. (Courtesy of the Alzheimer’s Research and Prevention Foundation.)
Biographies
Dharma Singh Khalsa, M.D., is the president/medical director of the Alzheimer’s Research and Prevention Foundation (AARPF) and the author of Brain Longevity (Warner Books, 1997). He is also a clinical associate professor, Division of General Internal Medicine, Geriatrics, and Integrative Medicine at the University of New Mexico Health Sciences Center in Albuquerque, and an associate editor of The Journal of Alzheimer’s Disease. Born in Ohio and raised in Florida, Khalsa graduated from Creighton University School of Medicine in 1975 and received his postgraduate training in anesthesiology at the University of California, San Francisco. He is board certified in anesthesiology and pain management and a diplomat of the American Academy of Anti-Aging Medicine.
George Perry, Ph.D., is dean of the College of Sciences and holds the Semmes Foundation Distinguished University Chair in Neurobiology at the University of Texas at San Antonio. He obtained his Ph.D. from Scripps Institution of Oceanography in 1979 and received a postdoctoral fellowship in the Department of Cell Biology at Baylor College of Medicine. Perry is editor-in-chief for the Journal of Alzheimer's Disease and is a foreign correspondent member of the Spanish Royal Academy of Sciences, the Academy of Science Lisbon, and a foreign member of the Mexican National Academy of Sciences. He is a recipient of the National Plaque of Honor from the Republic of Panama Ministry of Science and Technology. Perry’s research is primarily focused on how Alzheimer’s disease develops and the physiological consequences of the disease at a cellular level.
References
- 1.Alzheimer’s Association. 2016 Alzheimer’s Disease Facts and Figures. Alzheimer’s & Dementia. 2016;12(4) doi: 10.1016/j.jalz.2016.03.001. https://www.alz.org/documents_custom/2016-facts-and-figures.pdf. [DOI] [PubMed] [Google Scholar]
- 2.National Institute on Aging. Number of Alzheimer’s Deaths Found to be Underreported. May 22, 2014. https://www.nia.nih.gov/research/announcements/2014/05/number-alzheimers-deaths-found-be-underreported.
- 3.National Institutes on Health. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC) Feb 10, 2016. https://health.gov/dietaryguidelines/2015/guidelines/chapter-2/current-eating-patterns-in-the-united-states/
- 4.Ngandu T, Lehtisalo J, Solomon A, Kivipelto M, et al. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): Study Design and Progress. The Lancet. 2015;385(9984):2255–2263. doi: http://dx.doi.org/10.1016/S0140-6736(15)60461-5. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60461-5/abstract. [Google Scholar]
- 5.Andrieu S, Vellas B. MAPT Study: A Multidomain Approach for Preventing Alzheimer’s Disease. Presentation of soon to be published data at ISTAART, Alzheimer’s Association International Conference; Toronto, Canada. 2016. [Google Scholar]
- 6.US Office of Disease Prevention and Health Promotion. Current Eating Patterns in the United States. 2015. https://health.gov/dietaryguidelines/2015/guidelines/chapter-2/current-eating-patterns-in-the-united-states/
- 7.Shakersain B, Santoni G, Larsson SC, Xu W. Prudent Diet May Attenuate the Adverse Effects of Western Diet on Cognitive Decline. Alzheimer’s & Dementia. 2016. pp. 100–09. https://www.researchgate.net/publication/281588866_Prudent_diet_may_attenuate_the_adverse_effects_of_Western_diet_on_cognitive_decline. [DOI] [PubMed]
- 8.Merrill DA, Siddarth P, Raji CA, Emerson ND, Rueda F, Ercoli LM, Miller KJ, Lavretsky H, Harris LM, Burggren AC, Bookheimer SY, Barrio JR, Small GW. Modifiable Risk Factors and Brain Positron Emission Tomography Measures of Amyloid and Tau in Nondemented Adults with Memory Complaints. The American Journal of Geriatric Psychiatry. 2016. pp. 729–737. https://www.ncbi.nlm.nih.gov/pubmed/27421618/ [DOI] [PMC free article] [PubMed]
- 9.Staubo SC, Aakre JA, Vemuri P, Syrjanen JA, Mielke MM, Geda YE, Kremers WK, Machulda MM, Knopman DS, Petersen RC, Jack CR, Jr, Roberts RO. Mediterranean Diet, Micronutrients and Macronutrients, and MRI Measures of Cortical Thickness. Alzheimer’s & Dementia. 2016. published online. doi: http://dx.doi.org/10.1016/j.jalz.2016.06.2359. http://www.alzheimersanddementia.com/article/S1552-5260(16)32661-9/pdf. [DOI] [PMC free article] [PubMed]
- 10.Morris MC, Tangney CC, Wang Y, Barnes LL, Bennett D, Aggarwal N. MIND Diet Score More Predictive than DASH or Mediterranean Diet Scores. Alzheimer’s & Dementia. 2014. p. 166. doi: http://dx.doi.org/10.1016/j.jalz.2014.04.164. http://www.alzheimersanddementia.com/article/S1552-5260(14)00292-1/fulltext.
- 11.Pereira AC, Huddleston DE, Brickman AM, Sosunov AA, Hen R, McKhann GM, Sloan R, Gage FH, Brown TR, Small SA. An In Vivo Correlate of Exercise-induced Neurogenesis in the Adult Dentate Gyrus. Proceedings of the National Academy of Sciences. 2007;104(13):5638–5643. doi: 10.1073/pnas.0611721104. http://www.pnas.org/content/104/13/5638.short. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lupien SJ, McEwen B, Gunner M, et al. Effects of Stress Throughout the Lifespan on the Brain, Behavior and Cognition. Nature. 2009;10:434–445. doi: 10.1038/nrn2639. http://www.nature.com/nrn/journal/v10/n6/abs/nrn2639.html. [DOI] [PubMed] [Google Scholar]
- 13.Khalsa DS. Stress, Meditation and Alzheimer’s Disease Prevention: Where The Evidence Stands. Journal of Alzheimer’s Disease. 2015;48:1–12. doi: 10.3233/JAD-142766. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4923750/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newberg AB, Wintering N, Khalsa DS, Roggenkamp H, Waldman MR. Meditation Effects on Cognitive Function and Cerebral Blood Flow in Subjects with Memory Loss: A Preliminary Study. Journal of Alzheimer’s Disease. 2010;20(2):517–26. doi: 10.3233/JAD-2010-1391. http://www.ncbi.nlm.nih.gov/pubmed/20164557. [DOI] [PubMed] [Google Scholar]
- 15.Harrison TM, Weintraub S, Mesulam MM, Rogalski E. Superior Memory and Higher Cortical Volumes in Unusually Successful Cognitive Aging. Journal of the International Neuropsychological Society. 2012;18(6):1081–1085. doi: 10.1017/S1355617712000847. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3547607/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moss AS, Wintering N, Roggenkamp H, Khalsa DS, Waldman MR, Monti D, Newberg AB. Effects of An 8-Week Meditation Program on Mood and Anxiety in Patients With Memory Loss. Journal of Alternative and Complementary Medicine. 2012;18(1):48–53. doi: 10.1089/acm.2011.0051. http://www.ncbi.nlm.nih.gov/pubmed/22268968. [DOI] [PubMed] [Google Scholar]
- 17.Lavretsky H, Epel E, Siddarth P, Nazarian N, St Cyr N, Khalsa DS, Lin J, Blackburn E, Irwin MR. A Pilot Study of Yogic Meditation for Family Dementia Caregivers with Depressive Symptoms: Effects on Mental Health, Cognition, and Telomerase Activity. International Journal of Geriatric Psychiatry. 2013;28(1):57–65. doi: 10.1002/gps.3790. http://www.ncbi.nlm.nih.gov/pubmed/22407663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Innes K, Selfe TK, Khalsa DS, Kandati S. Effects of Meditation versus Music Listening on Perceived Stress, Mood, Sleep, and Quality of Life in Adults with Early Memory Loss: A Pilot Randomized Controlled Trial. Journal of Alzheimer’s Disease. 2016;52(4):1277–98. doi: 10.3233/JAD-151106. http://www.ncbi.nlm.nih.gov/pubmed/27079708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eyre HA, Acevedo B, Yang H, Siddarth P, Van Dyk K, Ercoli L, Leaver AM, St Cyr N, Narr K, Baune BT, Khalsa DS, Lavretsky H. Changes in Neural Connectivity and Memory Following a Yoga Intervention for Older Adults: A Pilot Study. Journal of Alzheimer’s Disease. 2016;52(2):673–684. doi: 10.3233/JAD-150653. http://www.ncbi.nlm.nih.gov/pubmed/27060939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang Y, Leaver AM, Pattharee Paholpak PS, Ercoli L, St Cyr NM, Eyre HA, Narr KL, Khalsa DS, Lavretsky H. Neurochemical and Neuroanatomical Plasticity Following Memory Training and Yoga Interventions in Older Adults with Mild Cognitive Impairment. Frontiers in Aging Neuroscience. 2016;8:277. doi: 10.3389/fnagi.2016.00277. http://dx.doi.org/10.3389/fnagi.2016.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryff CD, Singer BH, Dienberg LG. Positive Health: Connecting Well-Being with Biology. Philosophical Transactions of the Royal Society of London, Series B, Biological Sciences. 2004;359:1383–1394. doi: 10.1098/rstb.2004.1521. http://scholar.google.com/citations?view_op=view_citation&hl=en&user=YIlu3jYAAAAJ&citation_for_view=YIlu3jYAAAAJ:WF5omc3nYNoC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of Purpose in Life on Incident Alzheimer’s Disease and Mild Cognitive Impairment in Community-Dwelling Older Persons. Archives of General Psychiatry. 2010;67(3):304–310. doi: 10.1001/archgenpsychiatry.2009.208. http://jamanetwork.com/journals/jamapsychiatry/fullarticle/210648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaufman Y, Anaki D, Binns M, Freedman M. Cognitive decline in Alzheimer Disease: Impact of Spirituality, Religiosity, and QOL. Neurology. 2007;68(18):1509–14. doi: 10.1212/01.wnl.0000260697.66617.59. https://www.ncbi.nlm.nih.gov/pubmed/17470754. [DOI] [PubMed] [Google Scholar]
- 24.Lavretsky H. Resilience and Aging Research and Practice. Johns Hopkins University Press; Baltimore, Maryland: 2014. pp. 94–129. [Google Scholar]
- 25.Sheardova K, Nedleska Z, Sumec R, Marciniak R, Belaskova S, Uller M, Hort J. The Effect of Spirituality/Religiosity on Regional Brain Atrophy in Subjects at Risk of Alzheimer’s Disease, 3-year Follow-up Data from Czech Brain Aging Study. Personal Communication. To be presented at AAIC July 2017.