Abstract
Background
Immunization is one of the most effective public health measures to prevent disease, but vaccination rates in adult populations still remain below the targets. Patient and physician attitudes about vaccination are important for adult vaccination. In this study, we aimed to determine patient attitudes and perceptions about vaccination and the vaccination coverage rates of adult patients in a university hospital in Turkey.
Material/Methods
A survey was conducted between October 2014 and May 2015 at the Internal Medicine Outpatient Clinics of a university hospital. Adult patients were asked to fill out a questionnaire on their perceptions and attitudes about vaccination and their vaccination status.
Results
We interviewed 512 patients ages 19–64 years. Eighty percent of the study population thought that adults should be vaccinated, while only 36.1% of the patients stated that vaccination was ever recommended to them in their adult life. Forty-eight percent of the patients stated that they were vaccinated at least once in their adulthood. The most commonly received vaccine was tetanus vaccine in general, while influenza vaccine was the leading vaccine among patients with chronic medical conditions. While 71.4% of the patients to whom vaccination was recommended received the vaccine, 34.9% of the patients received a vaccine without any recommendation.
Conclusions
Although the vaccine coverage rates among adults in this survey were low, the perceptions of patients about adult vaccination were mainly positive and of many of them positively reacted when their physician recommended a vaccine.
MeSH Keywords: Immunization Programs, Patient Acceptance of Health Care, Primary Prevention, Vaccination
Background
The success of childhood immunization programs on the global scale caused a paradigm shift in vaccine-preventable diseases (VPDs). In 2015, 86% of infants worldwide had received the required 3 doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) recommended by the WHO, which is an indicator of immunization program performance [1]. Transmission of poliovirus and measles and rubella viruses has been eliminated in the U.S. and smallpox has been eradicated worldwide. Declines were 80% or greater for cases and deaths of most vaccine-preventable diseases targeted since 1980, including hepatitis A, acute hepatitis B, Hib, and varicella [2]. However, vaccine coverage rates (VCRs) in adult populations still remain below the targets and outbreaks of VPDs continue to occur even in countries with well-established vaccination programs [3]. They are not just “childhood diseases” and many of them have even more impact on adult populations.
Reports in the literature indicate that VPDs lead to approximately 45 000 deaths each year in the U.S., with the majority due to influenza [4]. Estimates show that during the 2015–2016 season, the overall burden of influenza was substantial, with 25 million influenza illnesses and 12 000 pneumonia and influenza (P and I) deaths in the U.S. and people 65 years and older made up 64% of P and I deaths [5]. More than 29 000 cases and more than 3200 deaths from invasive pneumococcal disease are estimated to have occurred in the U.S. in 2014. More than half of these cases occurred in adults who should have received the pneumococcal vaccine [6]. Human papillomavirus (HPV) causes cervical cancer, with an estimated 266 000 deaths globally in 2012 [7]. Tetanus mortality is the highest among elderly people over 80 years of age [8]. In 2012, pertussis re-emerged as a VPD of adolescents and adults, with an incidence rate rising over 4 years to nearly 50% in England and >48 000 cases of pertussis were reported nationally, the largest number in the United States since 1955 [9,10]. Furthermore, in 2009, a measles epidemic started in eastern and southern Europe which caused several thousands of cases with casualties [11].
Despite the documented burden of VPDs, adult vaccination remains an underused public health strategy, and vaccination coverage rates are below the set targets. Furthermore, data for adult VCRs in most European countries are incomplete and there are no targets except for influenza vaccine [3]. In the U.S., the Department of Health has established the ‘Healthy People 2020’ initiative, which specified goals for different vaccines for adults. In the U.S., VCRs in adults aged 65 years and older have improved over time, but VCRs remained quite low for younger adults at risk. For instance, in the 2015–2016 season, influenza vaccination coverage among adults 19–64 years old at high risk was 46%, whereas it was 63% among adults aged 65 years and older [12]. According to the latest data in Europe, the VCR for influenza was 44.7% for adults 65 years of age and older and 45.6% for younger adults with specific risk factors [13]. In 2013, pneumococcal vaccination coverage among adults aged 19–64 years at high risk was 21.2% overall, and it was 60% among adults aged 65 years and older in the U.S. [14]. The latest data from Europe indicates that pneumococcal VCR for adults aged 19–64 years at high risk and adults aged 65 years and older was only 10% [15].
Barriers to life-long vaccination include organizational barriers, healthcare provider-related barriers, patient-related barriers, healthcare system-related barriers, and socioeconomic factors. Patient-related barriers include inadequate patient knowledge and awareness, negative perceptions and attitudes, and low health literacy [3]. Patient and physician attitudes about vaccination may be important determinants of adult VCRs. The most important barriers to adult vaccination are misperceptions and low awareness of patients, and inadequate knowledge and negative attitudes of physicians. Many adults are unaware of which vaccinations they need and when they should receive them. People’s awareness about protecting their own health is also important in achieving the targeted level of adult immunization. The attitude and behavior of individuals are influenced by their health literacy, and limited health literacy may cause misperceptions and noncompliance. Several studies have shown that lack of recommendation by a physician was the main reason for not being vaccinated [16–18]. Furthermore, advice from friends, family, and colleagues is cited more than awareness of illness and vaccination as a reason for support for vaccination in the literature. The other reasons for vaccine hesitancy are safety concerns, lack of awareness, low perceived severity of illness, and a belief in alternative medicine and distrust of government sources [19]. Inadequate knowledge of physicians or even inability to take action in spite of good level knowledge might influence vaccine recommendations. Adult vaccine schedules that conflict with evidence-based recommendations create confusion among patients and healthcare providers [16]. Focussing only on vaccination coverage rates and neglecting underlying attitudes is likely to underestimate the challenge of maintaining target VCRs [19]. In this study, we aimed to determine patients’ attitudes and perceptions about vaccination and to assess the VCRs of adult patients in a university hospital in Turkey.
Material and Methods
Study population and sample selection
A survey was conducted between from October 2014 to May 2015 among general internal medicine outpatient clinics of a university hospital in Turkey. All consecutive patients visiting the outpatient clinics in this time period were invited to participate. Patients who agreed to participate and signed informed consent were interviewed by a physician who administered the survey in a standard fashion to all participants. Patient interviews were conducted immediately after the medical encounter with their doctors and patients with incomplete entries were excluded from the study.
Measures
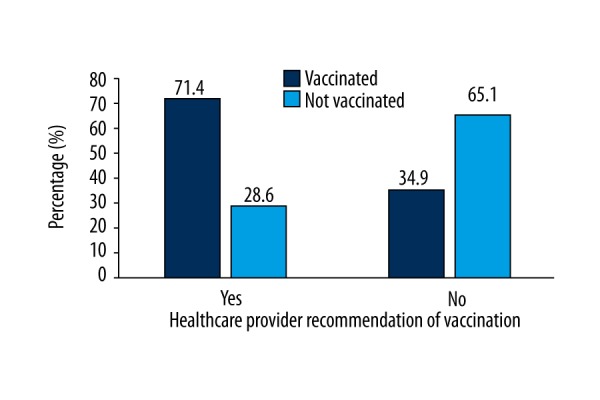
A standardized questionnaire was developed for the survey based on data in the literature. We pilot-tested the questionnaire for clarity, length, and face validity among 10 patients and modified several questions that were found to be unclear. The questionnaire consisted of multiple choice and open-ended questions covering 5 areas: 1) sociodemographic data; 2) risk factors for VPDs; 3) knowledge about adult vaccination; 4) any vaccination recommendation given and vaccination status; and 5) perceptions and attitudes about vaccination. Participant demographic characteristics included age, gender, marital status, education, employment status, medical history, lifestyle with regards to alcohol consumption and tobacco usage, contact with an infant in their household, and other risk factors for VPDs (Appendix 1).
Advisory Committee on Immunization Practices (ACIP) recommendations were used to define indications for vaccination [20]. We used the WHO definition for determining patient risk: those at high risk for developing influenza-related complications were defined as high-risk patients, including pregnant women, children aged 6 months to 5 years, the elderly (aged more than 65 years), those with chronic medical conditions, and healthcare workers [21].
Statistical analysis
Descriptive statistics were used to summarize demographic variables and vaccination behaviors. Chi-square statistics were used to examine the univariate relationship between the dependent variables of vaccination status and the independent variables of demographics, knowledge, attitude, and behaviors regarding vaccination. Statistical significance was determined by a p-value <0.05. Data analysis was performed using SPSS version 18 (SPSS Inc., 2009, PASW Statistics for Windows, Version 18.0, Chicago, SPSS, Inc).
Ethics
All participants provided written informed consent prior to study initiation. Approval was obtained from the Research Ethics Committee of Hacettepe University Faculty of Medicine, and the research was conducted in accordance with Good Clinical Practice guidelines.
Results
A total of 512 patients were recruited to the study, with a median age of 38 years (19–64) and 64.6% were females. Sociodemographic characteristics and comorbidities of the patients are given in Table 1.
Table 1.
Sociodemographic characteristics and comorbidities of the patients.
| Variable | Total* (N=512) |
|---|---|
| Age (years)# | 38 (19–64) |
| Male | 181 (35.4) |
| Married | 319 (62.7) |
| High school or higher grade | 70.5 (361) |
| Living in urban | 491 (96.3) |
| Smoker or ex-smoker | 164 (32.8) |
| Alcoholism | – |
| Cardiovascular disease | 9 (1.8) |
| Chronic pulmonary disease | 35 (6.8) |
| Diabetes | 49 (9.6) |
| Chronic renal failure, nephrotic syndrome | 1 (0.1) |
| Chronic liver disease | 1 (0.1) |
| Immunosupression | 3 (0.6) |
| Malignancy | 5 (0.9) |
| Morbid obesity | – |
| Pregnancy | – |
| Contact with an infant | 115 (22.8) |
| Healthcare worker | 12 (2.4) |
| Functional or anatomical aasplenia | 2 (0.4) |
| Cochlear implant, cerebrospinal fluid leaks | – |
| Residents of nursing homes | – |
Values presented are numbers with column percentages in parentheses;
Age is expressed as median, with minimum-maximum in parentheses.
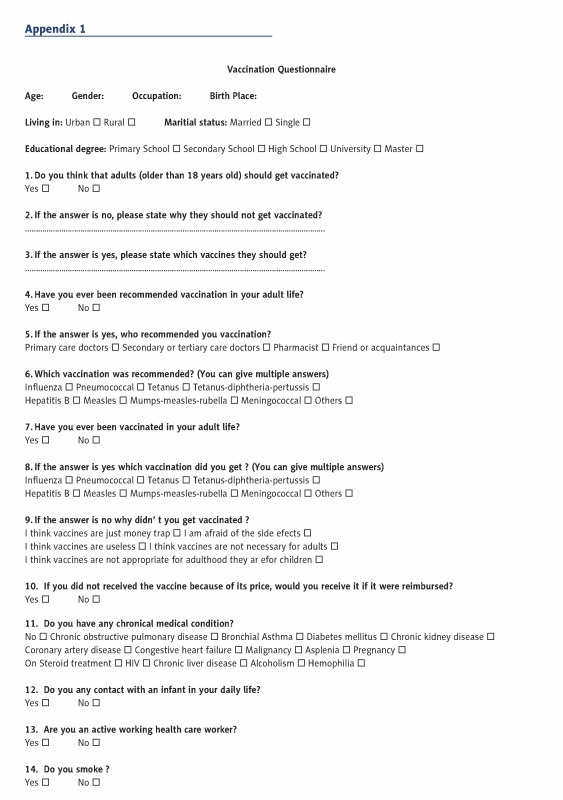
While 80.1% of the patients responded that adults should get vaccines, 15.2% thought that adults do not need to be vaccinated and 4.7% had no idea. There was no relationship between patient attitudes about vaccination and age, gender, marital status, educational level, or place of residence. Among those who thought that adults should not be vaccinated, 45.3% stated that ‘vaccines are not necessary for adults’, 21.9% were afraid of the adverse effects, 14.1% stated that ‘vaccines are useless’, 14.1% thought vaccines are not appropriate for adults, and 4.7% thought that vaccines were just a “money trap” (Figure 1).
Figure 1.
Patients’ assumptions about vaccination.
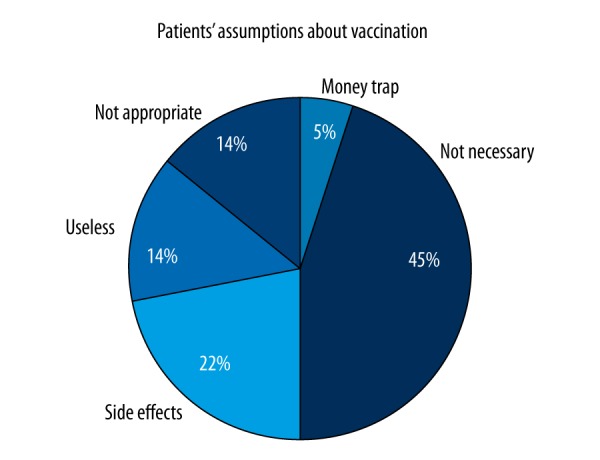
Those who thought that adults should be vaccinated were asked about which vaccination should be given to adult patients. The top-ranking answers were influenza (31.1%), hepatitis B (16.4%), and tetanus (15%) (Figure 2).
Figure 2.
Patients’ knowledge about the vaccines indicated in adult life.
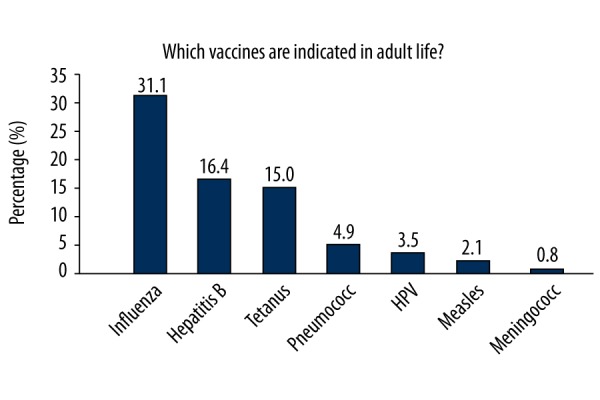
Only 36.1% of the patients stated that vaccination was ever recommended to them in their adult life and 48% stated that they were vaccinated at least once in adulthood. Recommendation was mostly made by the doctors from secondary or tertiary care rather than primary care doctors (14.5% and 10.5%, respectively). The most commonly recommended vaccines were influenza and hepatitis B (18% and 10.5%, respectively). Vaccination occurred in 71.4% of patients whose physician recommended vaccination, whereas 34.9% of the patients received at least 1 vaccine in adult life even though recommendation from a physician was lacking (p<0.001) (Figure 3).
Figure 3.
The effect of healthcare provider recommendations on receiving vaccine.
Overall, the most commonly received vaccine was tetanus (23%), while influenza vaccine was the most common among patients with chronic lung disease, chronic cardiovascular disease, and diabetes, but the coverage rates of influenza vaccination for patients with these medical conditions were still low (34.3% p=0.000, 62.5% p=0.000, and 26.5% p=0.001, respectively). Participants with chronic lung disease and chronic cardiovascular disease were also more likely to receive pneumococcal vaccines than those without these diseases (chronic lung disease 8.6% p=0.007 and chronic cardiovascular disease 12.5%, p=0.042). The influenza VCR was 18.5% in high-risk patients and 11.7% overall. The pneumococcal VCR was only 2.9% in patients aged 19–64 years with risk factors.
Discussion
We found knowledge gaps and misperceptions that might lead to low VCRs among adults attending general internal medicine outpatient clinics. Even in patients defined as high-risk by the WHO [21] the influenza VCR was only 18.5% but the target VCR set by the Centers for Disease Control and Prevention (CDC) is 70% [22] and by the European Commission target is 75% for elderly over 65 and people with specific health conditions/diseases [23], and this VCR is lower than in the U.S. and Europe [12,13]. The Healthy People 2020 target for pneumococcal VCR is 90% for adults 65 years of age and older and 60% for younger adults with specific risk factors [22]. In our study, the pneumococcal VCR was only 2.9% in patients with specific risk factors for pneumococcal infection, which is dramatically lower than many developed countries (21.2% in the U.S. [14] and 10% in Europe [15]).
We found the most commonly received vaccine in general was tetanus (23%) and influenza vaccine was the most common among patients with chronic lung disease, chronic cardiovascular disease, and diabetes. This finding is also consistent with the data from European countries showing that the most commonly recommended vaccine is influenza vaccine followed by tetanus vaccine in European countries [24]. In Turkey, soldiers receive the tetanus vaccine during compulsory military service and women receive the vaccine during pregnancy as a part of the maternal-neonatal tetanus elimination program. Additionally, tetanus vaccine is commonly administered as postexposure prophylaxis, and the lack of standard documentation for adults in Turkey leads to the administration of several tetanus vaccines after each possible exposure related to trauma or accidents.
There are many barriers to effective life-long vaccination, including organizational barriers, healthcare provider-related barriers, patient-related barriers, healthcare system-related barriers, and socioeconomic factors. Healthcare system-related barriers are lack of prioritization of vaccination, lack of recall systems and delivery, lack of monitoring and data, and lack of funding. Socioeconomic factors include inaccurate information in the public media, anti-vaccine movements, denial of disease risk, and the harms and risks of the disease- overconfidence vaccine paradox (forgetting the impact and the burden of VPDs as the disease is no longer seen after successful vaccination programs), and the gap between the science and the public. Patient-related barriers are inadequate knowledge and awareness, negative perceptions and attitudes, and low health literacy. Healthcare provider-related barriers are healthcare provider’s inadequate knowledge and awareness, negative perception and attitudes, and lack of effective communication with patients [3,25,26]. Although the low VCRs are disappointing, the perceptions and the attitudes of the adult patients responding to this survey were basically positive and indeed showed that there is room for improvement. Eighty percent of the patients agreed that adults do receive vaccines, while nearly half of the patients who thought that adults should not be vaccinated simply did not know that adults need vaccines [16]. Moreover, a considerable number of patients admitted that they received at least 1 vaccine in adulthood despite the lack of a recommendation by a doctor. These results show that there are major knowledge gaps about adult vaccination in the community, and the attitudes of the patients seem to be basically positive. It is clear that many of these perceptions can be positively reinforced with counseling and increasing the health literacy level of patients. Moreover, adults need to be informed about the vaccine paradox: with the increasing childhood VCRs, many diseases tend to be forgotten and adults do not perceive themselves as being at risk [11].
A doctor’s recommendation has a strong influence on a patient’s decision to receive a vaccine, even when the patient comes in with a resistant attitude about vaccination [27]. Although 80% of the ambulatory adult patients in this study population thought that adults should get vaccines, only 48% of them were vaccinated in adulthood, and only 36% stated that they have ever been recommended to get a vaccine. Of those who received a healthcare provider recommendation to have vaccination, 71% subsequently received a vaccine. Interestingly, 48% reported that they had received a vaccine, meaning some of them had received vaccines regardless of their physician’s recommendation. Unfortunately, our research has shown that many healthcare providers do not routinely recommend vaccines to their adult patients, despite evidence showing that the vast majority of patients will receive vaccinations if their healthcare provider recommends them [16,28,29]. The reasons for this missed opportunity may include clinicians’ knowledge and attitudes, as well as the systems of their practices. Doctors may also not realize the morbidity and mortality risks of VPDs [18] and perceive diseases as only ‘childhood communicable diseases’. Some of them may have limited knowledge about the availability and efficacy of the vaccines, or are unaware of national guidelines or recommendations. Additionally, the lack of good communication between doctors and the patients due to time constraints and quantitative performance pressures might have negative effects on vaccine recommendations [19,30]. Healthcare providers can play a major role in adult vaccination uptake, and they can be role models as well. In a review by Wheelock et al., the recommendation from a healthcare provider was reported to be the most common motivator for vaccination, whereas not recommending vaccination is reported as a reason for not receiving influenza vaccination [28]. In our research, 71% of the patients who were recommended vaccination by their healthcare provider were vaccinated, showing the key behavior-modifying role of healthcare providers.
The findings of local surveys such as the current one can be used to improve adult vaccination strategies on a national basis. The following actions are suggested to change behavior of patients and improve adult vaccination: education of the public about vaccine benefits and evidence-based guidance on potential vaccine adverse effects; making vaccines free and easily available; sharing real-time, trusted pharmacovigilance data and improving health literacy; changing healthcare provider’s attitudes by education; making doctors believe in vaccines and act as mentors and role models for vaccination; and integrating preventive health measures into every doctor-patient encounter and implementing high-quality health communication in patient visits.
The major limitation of this study was that vaccines were self-reported and therefore might be subject to recall bias. However, in the literature, self-reported influenza, pneumococcal polysaccharide, hepatitis A, hepatitis B, and HPV vaccination status among adults has been shown to be sensitive and specific [31].
Conclusions
This study demonstrated that there are knowledge gaps and misperceptions that might lead to low VCRs in an adult population attending general internal medicine outpatient clinics. Although the low VCRs are disappointing, the perceptions and the attitudes of the adult patients responding to this survey were basically positive and indeed showed that there is room for improvement. The findings of local surveys such as the current one can be used to improve adult vaccination strategies on a national basis.
Appendix 1
Footnotes
The study was presented as a poster presentation at the 14th Congress of the European Federation of Internal Medicine in Russia, 14–16 October, 2015
Source of support: Departmental sources
Statement
There is no support or financial disclosure stated by any of the authors. There is no conflict of interest stated by any of the authors.
References
- 1.World Health Organization. UNICEF: Global immunization vision and strategy 2006–2015. WHO; Geneva, Switzerland: 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roush SW, Murphy TV. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298:2155–63. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 3.Ozisik L, Tanriover MD, Rigby S, Unal S. ADVICE for a healthier life: Adult Vaccination Campaign in Europe. Eur J Intern Med. 2016;33:14–20. doi: 10.1016/j.ejim.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 4.Pham H, Geraci SA, Burton MJ. Adult immunizations: Update on recommendations. Am J Med. 2011;124:698–701. doi: 10.1016/j.amjmed.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 5.Rolfes MA, Foppa IM, Garg S, et al. Estimated influenza illnesses, medical visits, hospitalizations, and deaths averted by vaccination in the United States. 2016. [Date accessed: 19.12.2016]. https://www.cdc.gov/flu/about/disease/2015-16.htm.
- 6.Centers for Disease Control and Prevention. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Streptococcus pneumoniae, 2014. 2014. Available via the internet: http://www.cdc.gov/abcs/reports-findings/survreports/spneu14.pdf.
- 7.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer; 2013. [accessed on 19/12/2016]. [ http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx#] Available from: http://globocan.iarc.fr. [Google Scholar]
- 8.Pascual FB, McGinley EL, Zanardi LR, et al. Tetanus surveillance – United States, 1998–2000. MMWR Surveill Summ. 2003;52:1–8. [PubMed] [Google Scholar]
- 9.Confirmed pertussis in England and Wales continues to increase, in Health Protection Report, 2012, The UK Government Web Archive
- 10.Centers for Disease Control and Prevention. [Summary of Notifiable Diseases, 2012]. MMWR. 2014;61(53):105. [Google Scholar]
- 11.Carrillo-Santisteve P, Lopalco PL. Measles still spreads in Europe: Who is responsible for the failure to vaccinate? Clin Microbiol Infect. 2012;18(Suppl 5):50–56. doi: 10.1111/j.1469-0691.2012.03982.x. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2015–16 Influenza Season. [Access date: 19/12/2016]. https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm.
- 13.European Centre for Disease Prevention and Control. Seasonal influenza vaccination in Europe – Overview of vaccination recommendations and coverage rates in the EU Member States for the 2012–13 influenza season. Stockholm: ECDC; 2015. [Google Scholar]
- 14.Williams WW, Lu PJ, O’Halloran A, et al. Vaccination coverage among adults, excluding influenza vaccination – United States, 2013. Morb Mortal Wkly Rep. 2015;64:95–102. [PMC free article] [PubMed] [Google Scholar]
- 15.European Centre for Disease Prevention and Control. Surveillance of invasive bacterial diseases in Europe, 2012. Stockholm: ECDC; 2015. [Google Scholar]
- 16.Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med. 2008;121:S28–35. doi: 10.1016/j.amjmed.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Nowalk MP, Zimmerman RK, Shen S, et al. Barriers to pneumococcal and influenza vaccination in older community-dwelling adults (2000–2001) J Am Geriatr Soc. 2004;52:25–30. doi: 10.1111/j.1532-5415.2004.52006.x. [DOI] [PubMed] [Google Scholar]
- 18.Lode H, Ludwig E, Kassianos G. Pneumococcal infection – low awareness as a potential barrier to vaccination: results of a European study. Adv Ther. 2013;30:387–405. doi: 10.1007/s12325-013-0025-4. [DOI] [PubMed] [Google Scholar]
- 19.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 20.Kim DK, Bridges CB, Harriman KH. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older – United States, 2015. Morb Mortal Wkly Rep. 2015;64:91–92. [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. Influenza (Seasonal), Fact sheet 211. Apr, 2009. [Google Scholar]
- 22.U.S. Department of Health and Human Services. Healthy People 2020. Washington, DC: [Accessed 25.11.2015]. Office of Disease Prevention and Health Promotion. Available at http://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. [Google Scholar]
- 23.The Council of the European Union. Council recommendation on seasonal influenza vaccination. Available from: http://ec.europa.eu/health/ph_threats/com/Influenza/docs/seasonflu_rec2009_en.pdf. [DOI] [PubMed]
- 24.Kanitz EE, Wu LA, Giambi C, et al. Variation in adult vaccination policies across Europe: an overview from VENICE network on vaccine recommendations, funding and coverage. Vaccine. 2012;30:5222–28. doi: 10.1016/j.vaccine.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Kimmel SR, Burns IT, Wolfe RM, Zimmerman RK. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2007;56:S61–69. [PubMed] [Google Scholar]
- 26.MacDougall DM, Halperin BA, MacKinnon-Cameron D, et al. The challenge of vaccinating adults: Attitudes and beliefs of the Canadian public and healthcare providers. BMJ Open. 2015;5:e009062. doi: 10.1136/bmjopen-2015-009062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eppes C, Wu A, You W, et al. Barriers to influenza vaccination among pregnant women. Vaccine. 2013;31:2874–78. doi: 10.1016/j.vaccine.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 28.Wheelock A, Thomson A, Sevdalis N. Social and psychological factors underlying adult vaccination behavior: Lessons from seasonal influenza vaccination in the US and the UK. Expert Rev Vaccines. 2013;12:893–901. doi: 10.1586/14760584.2013.814841. [DOI] [PubMed] [Google Scholar]
- 29.Influenza vaccination and self-reported reasons for not receiving influenza vaccination among Medicare beneficiaries aged > or =65 years – United States, 1991–2002. Morb Mortal Wkly Rep. 2004;53:1012–15. [PubMed] [Google Scholar]
- 30.Hurley LP, Bridges CB, Harpaz R, et al. U.S. physicians’ perspective of adult vaccine delivery. Ann Intern Med. 2014;160:161. doi: 10.7326/M13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rolnick SJ, Parker ED, Nordin JD, et al. Self-report compared to electronic medical record across eight adult vaccines: do results vary by demographic factors? Vaccine. 2013;31:3928–35. doi: 10.1016/j.vaccine.2013.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]