Abstract
Purpose
Shared decision-making, when physicians and patients collaborate and agree on health care decisions, is a key tenant of patient-centered care. Choice of access site for neurovascular procedures is rarely a shared decision point between physicians and patients. We present our initial evaluation of patient preference for radial over femoral access for cerebrovascular procedures.
Materials and Methods
IRB approved single-center, prospective, and consecutive survey of all patients undergoing transradial access for cerebrovascular imaging and intervention. Primary inclusion criteria were patients who had previously undergone a transfemoral access procedure and chose to have their second procedure via a transradial approach. All patients underwent pre-procedural neurologic and extremity exams (including Barbeau tests for radial access suitability prior to radial access), post-procedural neurological evaluation and radial access assessment post-procedure, and complete neurological and radial access-site evaluation in the neurointerventional outpatient clinic 1–2 week post-procedure.
Results
Twenty five consecutive patients who underwent radial access cerebrovascular procedures after previous femoral access cerebrovascular procedures (16 diagnostic angiograms and 9 interventional procedures) were included. No major complications (including hematomas, infection, or delayed radial artery occlusion) were encountered during the immediate post-procedurral period or on outpatient follow-up (average 8 days). On immediate post-procedural examination, 16% had mild bruising and 24% had mild pain at the radial access site. Of the 25 patients included in this study, 24 strongly preferred radial access over femoral access and reported that, if they needed another procedure, they would prefer radial access.
Conclusion
There was nearly unanimous patient preference for radial over femoral access for cerebrovascular procedures in this single-center prospective analysis. There were no major complications and no incidences of delayed radial occlusion. In the current age of value-based and patient-centered medicine, the radial approach should be considered for nearly all neurovascular procedures.
INTRODUCTION
Radial access for interventional procedures dates back to 1948 when Radner et al. [1] first described a transradial catheterization using a radial artery cut-down approach. Thereafter, percutaneous radial access was explored when Mandel and Dauchet [2] as well as Slogoff et al. [3] described the safety and potential complications of radial artery cannulation for the purpose of monitoring in a surgical and critical care setting. Campeau [4] presented the first large transradial case series in 1989 when he described selective coronary angiography in 100 patients [4]. Radial access for percutaneous coronary interventions (PCIs) has been extensively studied, has become the standard of care for PCI in Europe, and has been increasingly utilized in the United States. Compared with conventional transfemoral and transbrachial access, radial access has been associated with lower complication rates at the access site, improved post-procedural comfort, and earlier ambulation/return to daily activities, and has been proven to be more cost effective [5, 6]. Complications rates associated with femoral artery and brachial artery access range from 2% to 8% [7] and from 6.5% to 11% [8–10], respectively, while radial access complication rates are typically <1% in high volume centers with experienced operators. A meta-analysis demonstrated a major reduction in bleeding complications with radial access compared with traditional femoral access [(OR 0.22) 95% CrI 0.16–0.29] as well as a decreased composite outcome of death or MI [(OR 0.69) 95% CrI 0.55–0.84] [11]. Several recent large randomized cardiology trials have shown superiority of the radial approach over the femoral approach for PCI in acute coronary syndrome. Radial access was associated with reduction in mortality, myocardial infarction, and stroke [12–14].
The importance of patient-centered medicine is becoming increasingly recognized in health care. Shared decision-making, when physicians and patients collaborate and agree on health care decisions, is a key tenant of patient-centered care. Choice of access site for neurovascular procedures is rarely discussed between physicians and patients. Kiemeneij et al. [5] and Goldberg et al. [15] demonstrated that, in the coronary setting, 75%–76% of patients preferred the radial approach compared with traditional femoral access [5, 15]. Beyond complications associated with access routes and feasibility, patient access-site preference for cerebrovascular procedures has never been previously studied. In this unique study, we present our initial evaluation of patient preference for radial versus femoral access for cerebrovascular procedures. Only patients who had previously undergone a femoral angiogram and subsequently chose radial access for their second procedure were included. Using this design, we were able to directly compare the experience that each patient had between femoral access and radial access. This study design has not previously been described in the cerebrovascular literature.
MATERIALS AND METHODS
This study was an IRB-approved single-center prospective survey of all patients undergoing transradial access for cerebrovascular imaging and intervention. All procedures were performed by a single operator at our center who had performed more than 50 previous transradial procedures. The two primary inclusion criteria were:
patients having previously undergone a femoral access for cerebrovascular procedure
patients with complete palmar arches confirmed with normal Barbeau testing [15].
The primary exclusion criteria were patients with insufficient palmar collaterals, based on a failed Barbeau test.
Patients who met the criteria were given a detailed explanation of this study. All enrolled patients were consented and underwent a neurovascular procedure via a transradial approach. Data collection was performed by review of electronic medical records (inpatient and outpatient) and patient surveys filled out post-procedure and as outpatients with the assistance of the Neurointerventional Surgery nurse practitioners. Patients who met the criteria underwent focused physical exams that were the basis of the surveys filled out by the medical providers. The surveys were filled out prior to discharge after their radial procedure as well as at the standard 1–2 week initial outpatient follow-up visit.
The questionnaires were unique and carefully created as to assure patient understanding and accurate patient responses. The patients were given ample opportunity to ask questions during the surveys to verify full understanding of the survey content. All patients were able to fill out the questionnaires on their own. The survey questions were assessed on a 1–5 Likert scale and are detailed in Table 1. At the routine initial outpatient follow-up visit, patients were again examined for any neurological or access-site complications, including Doppler evaluation of the ipsilateral radial and ulnar arteries.
Table 1. Patient Survey.
| 1.) Do you prefer radial or femoral access for your neurovascular procedure? | Radial or Femoral |
| 2.) A. Was the radial or femoral procedure less painful overall? B. The radial procedure was less painful overall. |
Radial or Femoral 1–5 |
| 3.) A. Was the radial or femoral procedure less embarrassing? B. The radial procedure was less embarrassing. |
Radial or Femoral 1–5 |
| 4.) A. Was the radial or femoral procedure less stressful? B. The radial procedure was less stressful. |
Radial or Femoral 1–5 |
| 5.) A. Was the radial or femoral procedure less painful during the procedure? B. I felt less pain during the procedure with the radial procedure. |
Radial or Femoral 1–5 |
| 6.) A. Was the radial or femoral procedure less painful after the procedure? B. I felt less post-procedure pain with the radial procedure. |
Radial or Femoral 1–5 |
| 7.) A. Was your recovery time shorter with the radial or femoral procedure? B. I had a shorter recovery time with the radial procedure. |
Radial or Femoral 1–5 |
| 8.) A. Did you have more complications with the radial or femoral procedure? B. I encountered no complications with my radial procedure. |
Radial or Femoral 1–5 |
| 9.) A. Could you start eating sonner with the radial or femoral procedure? B. I could start eating sooner with my radial procedure. |
Radial or Femoral 1–5 |
| 10.) Do you have any other complaints? | Open Answer |
| Medical Provider Survey after radial access | |
| 1.) Is there bruising at the radial access site? | Yes or No |
| 2.) Is there a hematoma at the radial access site? | Yes or No |
| 3.) How much pain is the patient having? | None, Mild, Moderate, or Significant |
KEY: 1–5 Scale
1 – Strongly Disagree
3 – Neutral
5 – Strongly Agree
At an out-patient follow-up visit between 7 and 14 days (average 8 days), all patients were assessed for bruising, hematoma, infection, pain, and patency of the radial and ulnar arteries (by palpation and confirmed with Doppler ultrasound examination). Additional measures were also collected, primarily from the operative reports, including the fluoroscopy times, radiation doses, amount and types of contrast injected, medications administered, types of sheaths and catheters utilized, and specific vessels selected during each case.
RESULTS
A total of 25 patients undergoing radial access procedures were included. Five of these patients had repeated radial access procedures (diagnostic or interventional). There were a total of 5 male and 17 female patients with median age of 59. The procedures included 16 diagnostic angiograms and 9 interventional procedures, including balloon-assisted coiling, Pipeline stent placement, AVM embolizations, stent-assisted coiling, and primary coil embolization.
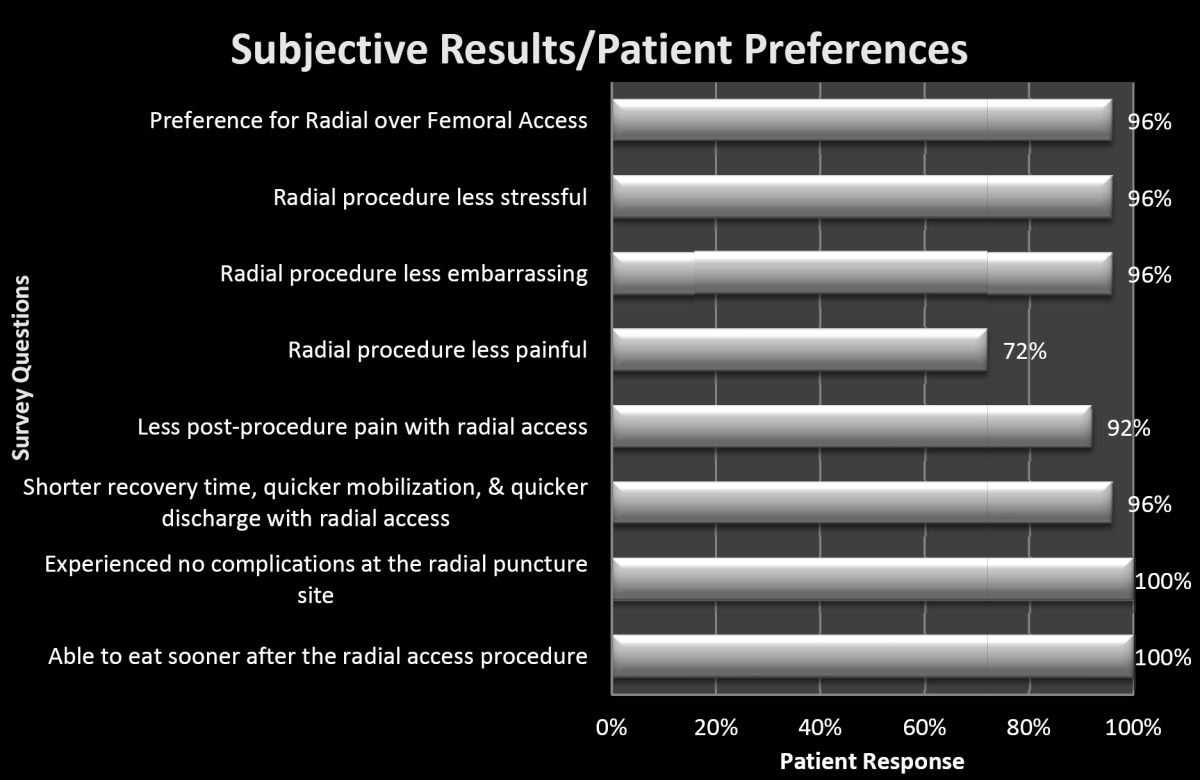
Of the 25 patients included in this study, 24 preferred radial access over their femoral access for their neurovascular procedures. Furthermore, collected data was divided into subjective and objective results. Subjectively, the radial approach was found to be less stressful, less embarrassing, and less painful peri-procedurally and post-procedurally. The vast majority of patients, 88%, reported no pain at the follow-up evaluation. Two patients reported mild pain and one reported severe pain. The patient with severe pain associated with radial access was a female with diminutive stature and of Korean descent. Detailed subjective results are illustrated in Table 2.
Table 2. Subjective Results / Patient Preferences.
|
The immediate post-procedure examination (within six hours of completion) was objective and as follows: no hematomas, 16% (4/25) had mild bruising at the radial access site, and 24% had mild pain at the radial access site. At the first outpatient follow-up (average 8 days), there were no major complications including hematomas or infection, and there was 100% radial and ulnar artery patency based on palpation and confirmed with Doppler ultrasound. Two patients had slight bruising at the radial access site. One patient reported nonspecific ipsilateral forearm erythema (potentially related to tape/prep material). There were no occurrences of delayed radial occlusion.
DISCUSSION
Although the literature and experience is lacking in neurointerventional literature, the near unanimous preference for radial access over traditional femoral access is not surprising given the success and widespread adaptation in the field of cardiology. Radial access has been described for neurovascular procedures in case series with good success rates and low complications [16–22]. Decreased stress and embarrassment as well as decreased pain throughout the course of the patient’s care are only a few of the advantages of the radial approach. Some neurovascular procedures may be simpler with a radial approach such as accessing the vertebrobasilar system. Accessing the vertebral arteries may occasionally be challenging via the transfemoral approach if there is severe tortuosity of the left subclavian artery or more commonly the innominate artery [18]. Radial access is infrequently utilized for cerebrovascular procedures for two main reasons: 1) technical limitations associated with catheter technology and 2) physician preference.
The majority of patients experienced decreased pain, but it was not as unanimous of an opinion as with other questions. This was likely due to less conscious sedation administered earlier in the study. By the end of this study and after this study, we found that pain, spasm, and overall patient experience were significantly improved with generous administration of both conscious IV sedation and local anesthesia around the sheath insertion site. This was particularly true in women of short stature, a population at a particularly high risk of spasm and pain. This change in approach to the level of sedation and anesthesia may have improved the experience in the single patient who did not prefer radial over femoral access.
No significant complications including vascular injury, occlusion, bleeding, or compartment syndrome were encountered in 25 successive radial access procedures. Both diagnostic and interventional neurovascular procedures were successfully performed via the radial approach, with most diagnostic procedures being performed with a 4F sheath and almost all interventional procedures performed with a Terumo 6F slender radial sheath (Terumo Corporation, Tokyo, Japan). The 6F slender sheath is an ultrathin 10-cm sheath that has a smaller outer diameter, closer to a typical 5F sheath, with an inner diameter that accommodates 6F guiding catheters. The most common neurovascular guide was a Cordis Envoy DA 6F 95-cm 071-inch catheter (Cordis, Hialeah, FL, USA). Major complications including stroke, radial artery occlusion, and vascular injury after radial access were not encountered. There was 100% patency of the accessed radial vessels at follow-up.
Technical limitations of catheter flexibility/pushability and catheter/guide lengths are still encountered due to the lack of availability of radial specific devices for cerebrovascular procedures. These technical limitations are becoming more easily surmounted by improved catheter designs which incorporate multiple transitions with flat/round wire reinforcement and longer available lengths (up to 105 cm). Physician preference for femoral access is likely multifactorial. Potential barriers include lack of training, discomfort of lab staff/setup, perceived longer procedure time, and discomfort with radial access. Although not suited for all patients, the authors contend that radial access should be considered in all patients undergoing a cerebrovascular procedure. The cardiology literature includes tens of thousands of patients and demonstrates statistically lower incidence of myocardial infarctions, strokes, and decreased mortality [6, 12, 13].
Considering the patient experience and allowing patients to participate in decision making for access sites during cerebrovascular procedures is consistent with the principle of shared decision making. This partnership between physicians and patients results in increased patient knowledge, more accurate risk perception, a greater number of decisions consistent with patients’ values, reduced level of internal decisional conflict for patients, fewer patients remaining passive or undecided, and improved overall patient satisfaction [23–25].
CONCLUSION
There was nearly unanimous patient preference for radial over femoral access for cerebrovascular procedures in this single-center prospective analysis. There were no major complications and no incidences of delayed radial occlusion. In the current age of value-based and patient-centered medicine, the radial approach should be considered for nearly all neurovascular procedures.
REFERENCES
- Radner S. Thoracal aortography by catheterization from the radial artery; preliminary report of a new technique. Acta radiol. 1948;29:178–180. doi: 10.3109/00016924809132437. [DOI] [PubMed] [Google Scholar]
- Mandel MA, Dauchot PJ. Radial artery cannulation in 1,000 patients: precautions and complications. J Hand Surg Am. 1977;2:482–485. doi: 10.1016/s0363-5023(77)80030-0. [DOI] [PubMed] [Google Scholar]
- Slogoff S, et al. On the safety of radial artery cannulation. Anesthesiology. 1983;59:42–47. doi: 10.1097/00000542-198307000-00008. [DOI] [PubMed] [Google Scholar]
- Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet cardiovasc Diagn. 1989;16:3–7. doi: 10.1002/ccd.1810160103. [DOI] [PubMed] [Google Scholar]
- Kiemeneij F, et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269–1275. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- Hamon M, et al. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care** and Thrombosis of the European Society of Cardiology. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2013;8:1242–1251. doi: 10.4244/EIJV8I11A192. [DOI] [PubMed] [Google Scholar]
- Archbold RA, et al. Radial artery access for coronary angiography and percutaneous coronary intervention. BMJ. 2004;329:443–446. doi: 10.1136/bmj.329.7463.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Tostado, et al. The brachial artery: a critical access for endovascular procedures. J Vasc Surg. 2009;49:378–385. doi: 10.1016/j.jvs.2008.09.017. discussion 85. [DOI] [PubMed] [Google Scholar]
- Heenan SD, et al. Transbrachial arteriography: indications and complications. Clin Radiol. 1996;51:205–209. doi: 10.1016/s0009-9260(96)80324-2. [DOI] [PubMed] [Google Scholar]
- Grollman JH, Jr, Marcus R. Transbrachial arteriography: techniques and complications. Cardiovasc Intervent Radiol. 1988;11:32–35. doi: 10.1007/BF02577022. [DOI] [PubMed] [Google Scholar]
- Bertrand OF, et al. Transradial approach for coronary angiography and interventions: results of the first international transradial practice survey. JACC Cardiovas Interv. 2010;3:1022–1031. doi: 10.1016/j.jcin.2010.07.013. [DOI] [PubMed] [Google Scholar]
- Jolly SS, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- Romagnoli E, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–2489. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Bernat I, et al. ST-segment elevation myocardial infarction treated by radial or femoral approach in a multicenter randomized clinical trial: the STEMI-RADIAL trial. J Am Coll Cardiol. 2014;63:964–972. doi: 10.1016/j.jacc.2013.08.1651. [DOI] [PubMed] [Google Scholar]
- Goldberg SL, et al. Learning curve in the use of the radial artery as vascular access in the performance of percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn. 1998;44:147–152. doi: 10.1002/(sici)1097-0304(199806)44:2<147::aid-ccd5>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Matsumoto Y, et al. Transradial approach for diagnostic selective cerebral angiography: results of a consecutive series of 166 cases. AJNR Am J Neuroradiol. 2001;22:704–708. [PMC free article] [PubMed] [Google Scholar]
- Levy EI, et al. Transradial cerebral angiography: an alternative route. Neurosurgery. 2002;51:335–340. discussion 40–42. [PubMed] [Google Scholar]
- Nohara AM, Kallmes DF. Transradial cerebral angiography: technique and outcomes. AJNR Am J Neuroradiol. 2003;24:1247–1250. [PMC free article] [PubMed] [Google Scholar]
- Bendok BR, et al. Neuroendovascular interventions for intracranial posterior circulation disease via the transradial approach: technical case report. Neurosurgery. 2005;56:E626. doi: 10.1227/01.NEU.0000154820.28342.38. ;discussion E. [DOI] [PubMed] [Google Scholar]
- Lawson MF, et al. Direct radial artery access with the 070 neuron guide catheter for aneurysm coiling: a novel application of the neuron catheter for cerebral interventions. Neurosurgery . 2012;71:onsE329–34. doi: 10.1227/NEU.0b013e318265a454. discussion onsE34. [DOI] [PubMed] [Google Scholar]
- Park JH, et al. Efficacy of transradial cerebral angiography in the elderly. J Korean Neurosurg Soc. 2013;53:213–217. doi: 10.3340/jkns.2013.53.4.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satti SR, et al. Radial access for cerebrovascular procedures: case report and technical note. Interv Neuroradiol. 2016;22:227–235. doi: 10.1177/1591019915617314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry MJ. Shared decision making: informing and involving patients to do the right thing in health care. J Ambul Care Manage. 2012;35:90–98. doi: 10.1097/JAC.0b013e318249482f. [DOI] [PubMed] [Google Scholar]
- Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev . 2011:CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Street RL., Jr The values and value of patient-centered care. Ann Fam Med. 2011;9:100–103. doi: 10.1370/afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]


