Abstract
The discovery of leptin has significantly advanced our understanding of the metabolic importance of adipose tissue and has revealed that both leptin deficiency and leptin excess are associated with severe metabolic, endocrine, and immunological consequences. We and others have shown that a prominent role of leptin in humans is to mediate the neuroendocrine adaptation to energy deprivation. Humans with genetic mutations in the leptin and leptin receptor genes have deregulated food intake and energy expenditure leading to a morbidly obese phenotype and a disrupted regulation in neuroendocrine and immune function and in glucose and fat metabolism. Observational and interventional studies in humans with (complete) congenital leptin deficiency caused by mutations in the leptin gene or with relative leptin deficiency as seen in states of negative energy balance such as lipoatrophy, anorexia nervosa, or exercise-induced hypothalamic and neuroendocrine dysfunction have contributed to the elucidation of the pathophysiological role of leptin in these conditions and of the clinical significance of leptin administration in these subjects. More specifically, interventional studies have demonstrated that several neuroendocrine, metabolic, or immune disturbances in these states could be restored by leptin administration. Leptin replacement therapy is currently available through a compassionate use program for congenital complete leptin deficiency and under an expanded access program to subjects with leptin deficiency associated with congenital or acquired lipoatrophy. In addition, leptin remains a potentially forthcoming treatment for several other states of energy deprivation including anorexia nervosa or milder forms of hypothalamic amenorrhea pending appropriate clinical trials.
Keywords: leptin deficiency, lipoatrophy, neuroendocrine and immune function, leptin replacement therapy
The discovery of leptin, the prototype adipocyte–secreted hormone/cytokine (adipokine), in 1994 has revolutionized our understanding of hormonal regulation of body composition and energy homeostasis as well as immune, endocrine, and metabolic physiology and pathophysiology. In addition, our view of adipose tissue has changed substantially within the past decade from that of a depot storage organ to that of an active endocrine organ producing several bioactive peptides (adipokines) and inflammatory and anti-inflammatory molecules.1,2 Although leptin was originally discovered as an antiobesity hormone, it was subsequently found that only a minority of subjects with obesity, that is, those with genetic mutations in the leptin pathway, have morbid obesity due to leptin deficiency. Observational and interventional studies revealed that leptin’s physiological and pathophysiological roles may be more important in the leptin deficiency end of the spectrum. Subsequently, proof-of-concept studies investigated whether leptin treatment either in subjects with congenital leptin deficiency or in those with acquired relative leptin deficiency may restore metabolic, endocrine, and immune functions in those patients.3,4
This review summarizes leptin’s role in the physiology/pathophysiology of several leptin deficiency disease states.
LEPTIN—THE PROTOTYPE ADIPOKINE
Leptin, a 167–amino acid peptide, is the prototypical adipose tissue–derived hormone related to the regulation of energy homeostasis. It exerts pleiotropic effects by binding and activating specific leptin receptors in the hypothalamus and other organs, has direct and indirect effects in metabolically active tissues, and regulates several neuroendocrine axes. Leptin circulates in a biologically active free form and also bound to leptin-binding proteins.3–7 Leptin levels are positively correlated with the amount of body fat, and obese subjects are hyperleptinemic compared with lean individuals.8 However, they appear to be either tolerant or resistant to the central hypothalamic effects of leptin. The reduced sensitivity toward exogenous (administered) and endogenous leptin is commonly referred to as leptin tolerance or leptin resistance.9
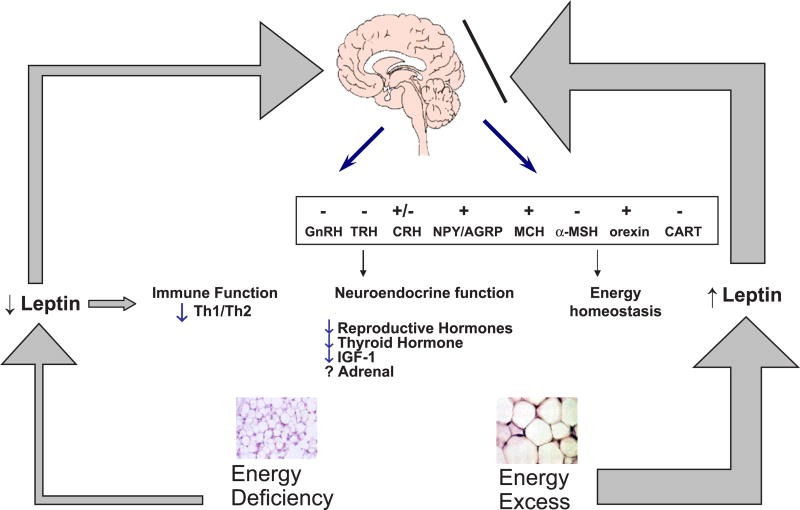
The biological activity of leptin is mediated by activating specific leptin receptors in the brain and peripheral organs (Fig. 1). Deficient leptin signaling due to hyperleptinemia (as described earlier) or hypo/aleptinemia caused by mutations of either leptin or the leptin receptor genes results in hyperphagia and decreased energy expenditure in rodents and humans, which in turn leads to an increasing degree of obesity associated with increased lipid storage in muscle, liver, and other tissues.9 The consequences are a dysfunction of several neuroendocrine axes, including the reproductive, thyroid, and adrenal axes, and an abnormal function of the immune and autonomic systems and bone metabolism.2,4–8 In addition to these well-documented effects of leptin, the hormone has also been proposed to have a cognitive enhancing role in the developing central nervous system as shown by leptin replacement therapy to a boy with a missense mutation of the leptin gene.10 However, the most important function of leptin is the regulation of energy expenditure and food intake, and the major physiological role of leptin is to signal inadequate rather than excess energy stores.2–10
FIGURE 1.
Peripheral and central effects of leptin in regulating neuroendocrine function and energy homeostasis in energy deficiency and energy excess states. In energy deficiency, less leptin is secreted (thin arrow) and results in the physiological changes indicated in the figure. In energy excess states, higher leptin concentrations are circulating (thick arrows), but the brain is largely resistant to the effects of leptin. AGRP indicates agouti-related protein; α-MSH, α-melanocyte–stimulating hormone; CART, cocaine- and amphetamine-regulated transcript; CRH, corticotrophin-releasing hormone; MCH, melanin-concentrating hormone; NPY, neuropeptide Y.
BIOLOGICAL EFFECTS OF LEPTIN
Leptin and the Reproductive Axis
The role of leptin in regulating reproduction and the hypothalamic-pituitary-gonadal (HPG) axis is a crucial, permissive one. Congenital leptin deficiency and/or loss of leptin function due to leptin- or leptin receptor mutations leads to hypogonadotropic hypogonadism with low levels of follicle-stimulating hormone and luteinizing hormone, complete loss of luteinizing hormone pulsatility, lack of pubertal growth spurt, reduced expression of secondary sexual characteristics, and primary/secondary amenorrhea.11,12 The clinical features of hypothalamic hypogonadism and associated disturbances can be restored by leptin administration in replacement doses.13 On the other end of the spectrum, elevated leptin levels due to increased body fat mass associated with (morbid) obesity may also have an inhibitory effect on the HGP axis. Leptin may thus serve as a signal to convey information to the reproductive system that the amount of energy stored in the body as fat is adequate not only for the survival of the individual but also for carrying a pregnancy to term. Because a certain threshold level of energy and body fat mass, which may vary from individual to individual, seems to be necessary for the onset of puberty and normal fertility, leptin has been proposed to be a permissive signal, which can activate the reproductive axis and maintain normal reproductive function by conveying needed information on available energy reserves in the adipose tissue.6,14 Moreover, in states of secondary failure of the HPG axis associated with loss of fat mass, such as in exercise-induced amenorrhea or anorexia nervosa, exogenously administered leptin may fully normalize the function of the HPG axis.7,14
Leptin and the Hypothalamic-Pituitary-Growth Hormone (GH)-Insulinlike Growth Factor 1 (IGF-1) Axis
Congenital leptin deficiency due to a mutation in the leptin gene and/or the leptin receptor gene is associated with a significant delay in growth in early childhood due to abnormal growth hormone secretion and low insulinlike growth factor 1 (IGF-1) and IGF-binding protein 3 (BP3) levels.11,12 Similarly, acute fasting and/or chronic energy deprivation, both of which induce a low leptin state, results in lower IGF levels. Administration of leptin in replacement doses in these conditions prevents the decrease in IGF-1 and IGF-BP3 levels but has no (short-term) effect on circulating levels of growth hormone. Similar results have been observed after long-term leptin administration to healthy lean subjects studied in energy-replete and energy-deficient states such as acute food deprivation or exercise-induced energy deprivation; leptin is capable of upregulating IGFs and altering IGF-PB3.15 However, the exact long-term impact of leptin on the hypothalamic-pituitary-GH-IGF axis and growth is still in the center of intense research efforts.
Leptin and the Hypothalamic-Pituitary-Thyroid (HPT) Axis
A significant and pivotal role of leptin in the regulation of the hypothalamic-pituitary-thyroid axis has been well documented in humans.6–8 Congenital hypoleptinemia due to leptin receptor mutations is associated with hypothalamic hypothyroidism, low circulating thyroxine levels, normal circulating basal thyrotropin (TSH), and a sustained response of TSH to a thyrotropin-releasing hormone challenge.12 Healthy subjects with normal weight exhibit a similar leptin and TSH 24-hour secretion pattern, which is impaired in subjects with congenital leptin deficiency.16 Leptin administration in replacement doses to healthy lean men during a 3-day starvation period significantly blunted the fasting-induced decrease in TSH pulsatility and increased free thyroxine to levels within the reference range.17 The data available to date indicate that leptin may regulate TSH, influencing secondarily circulating thyroxine levels in leptin-replete states. The exact mechanisms underlying these effects require further investigation.
Leptin and the Adrenal Axis
The role of leptin in the regulation of the adrenal axis in humans remains a controversial one. Congenital leptin deficiency in subjects with mutations of the leptin gene or the leptin receptor gene present with normal adrenal function, and interventional studies in healthy subjects with normal weight also failed to demonstrate an effect of leptin on adrenal steroids.12,15–17
Leptin and Immune Function
Leptin exerts direct effects on macrophages by **upregulating phagocytic activity, stimulates secretion of proinflammatory cytokines, and stimulates chemotaxis in polymorphonuclear cells.6 Animal studies and preliminary observational studies in humans with either congenital leptin deficiency or obesity-related hyperleptinemia have revealed that both leptin excess and leptin deficiency may increase an individual’s susceptibility to infection: children with congenital leptin deficiency are prone to early death due to severe infections during childhood because of defects in T-cell number and function.18–20 However, immune function could be markedly improved with leptin administration in replacement doses.19
Our understanding to date strongly supports a role of leptin in immune function, mainly by altering serum levels of inflammatory markers and other cytokines important in the T helper cell response.21 In addition, leptin regulates the T helper 1/T helper 2 immune balance in states of (congenital) leptin deficiency and immune dysfunction.18–21
Considering all these findings from observational and interventional studies together, congenital leptin deficiency and negative energy balance associated with acquired leptin deficiency may alter the nature and vigor of the immune response via leptin-dependent mechanisms. The role of leptin in regulating immune function appears to be a permissive one22; there might exist a critical leptin threshold above which leptin has no major additional physiological effect on neuroendocrine and/or immune function.7
Leptin and Cognitive Development
In addition to the effects of leptin described above, which are all well documented, leptin has also been recently proposed to have a cognitive enhancing role in the developing central nervous system. Treatment of a leptin-deficient boy with recombinant methionyl human leptin (r-metHuLeptin) in replacement doses had significant beneficial effects on cognitive function, leading to improvements in neurocognition.10 Further studies are needed to confirm these beneficial neurocognitive effects in leptin-deficient patients across the life span. In addition, further investigations are necessary to elucidate the hypothesis that leptin replacement may improve cognition in leptin-sufficient patients with delay or decline in cognitive function.
STATES OF LEPTIN DEFICIENCY: PATHOPHYSIOLOGY AND TREATMENT
Congenital Leptin Deficiency
Very rare genetic forms of obesity result from congenital leptin deficiency due to (missense) mutations in the leptin gene or the leptin receptor gene, frequently associated with consanguineous marriage.12,18,19 Congenital leptin deficiency is associated with a morbidly obese phenotype and significant disturbances in metabolic and immune functions (see succeeding paragraphs).
Congenital and Acquired Lipoatrophy
Another diverse group of congenital or acquired states of leptin deficiency represents a group of clinical disorders characterized by complete or partial lack of (subcutaneous) adipose tissue (lipoatrophy), and/or a combination of lack of adipose tissue in certain areas of the body with excess adipose tissue (lipohypertrophy) elsewhere.23 The human immunodeficiency virus (HIV)-associated lipodystrophy syndrome (HALS) represents the most common form of partial acquired lipodystrophy. It is estimated to occur in up to 40% to 84% of patients on highly active antiretroviral treatment for more than 1 year.23
Leptin Deficiency in Anorexia Nervosa and Hypothalamic Amenorrhea
Exercise-induced energy deficiency and eating disorders such as anorexia nervosa are associated with low leptin levels and associated metabolic sequelae. These subjects impress not only with low body fat mass but also with delayed puberty and impaired development of the reproductive system including hypothalamic amenorrhea along with other neuroendocrine dysfunctions.7,14
Metabolic Impact of Leptin Deficiency
Congenital or acquired states of hypoleptinemia are associated with significant metabolic, endocrine, and immunological disturbances. Those include neuroendocrine dysfunction, glucose intolerance and insulin resistance, dyslipidemia, disturbed immune function, and others. Similar to states of low leptin levels due to genetic mutations, nearly all forms of lipodystrophy are associated with insulin resistance, abnormal glucose tolerance, hepatic steatosis, and associated metabolic disorders, including dyslipidemia, mostly hypertriglyceridemia. In addition, HALS has also been linked to endothelial dysfunction and accelerated atherosclerosis.23 In lipoatrophic subjects, adipose tissue accumulates intrahepatically and intramyocellularly, and this is probably the main mechanism by which these subjects become insulin resistant. Both leptin and adiponectin levels are decreased in patients with severe congenital and milder HIV-associated lipoatrophy. Long-term effects of leptin administration in such conditions were originally studied using lipoatrophic mouse models and have subsequently been studied in the context of controlled clinical trials in patients with both severe and partial congenital lipoatrophy induced by administration of highly active antiretrovirals in HIV-positive patients. These patients have milder insulin resistance and milder metabolic syndrome. These trials demonstrated that leptin administration in replacement doses significantly improves glycemia, dyslipidemia, and hepatic steatosis in lipoatrophic, hypoleptinemic patients with severe insulin resistance and also improves dyslipidemia and insulin resistance in HIV-positive patients with partial lipoatrophy.23–28 The resolution of insulin resistance in states of congenital leptin deficiency and lipoatrophy is due to either a direct effect of leptin or a secondary effect due to loss (or redistribution) of ectopic body fat.23 Moreover, adiponectin also improves insulin resistance and metabolic syndrome in hypoadiponectinemic subjects with HALS.29 Because coadministration of both leptin and adiponectin fully normalized insulin sensitivity in animal models of lipoatrophic insulin resistance and metabolic syndrome,30 we are currently performing clinical trials testing whether coadministration of leptin and adiponectin could have additive or synergistic effects in improving insulin resistance and metabolic syndrome.
Clinical Applications of Leptin in Leptin Deficiency
Subjects with congenital absolute leptin deficiency respond in a dramatic fashion to leptin administered in replacement doses, which induce markedly decreased appetite and food intake and which in turn result in a significant reduction in body weight.18,19 In addition, leptin treatment in children with congenital leptin deficiency results in normalization of several neuroendocrine axes, including the reproductive and thyroid axes, and of immune function and cognitive development.10,18,19
Relative leptin deficiency is seen in states of partial lipodystrophy, eating disorders such as anorexia nervosa, and/or exercise-induced energy deficiency, as previously discussed. Interventional studies in women with hypothalamic amenorrhea and low circulating leptin levels have proven the concept that r-metHuLeptin in replacement doses may restore reproductive function, induce ovulation, and increase circulating levels of thyroxine, IGF-1, IGF-BP3, bone alkaline phosphatase, and other bone markers. In addition, r-metHuLeptin replacement restored gonadotropin-releasing hormone pulsatility,13 thus raising the intriguing possibility that leptin administration in replacement physiological doses could also be a potential treatment for some patients suffering from infertility. This hypothesis has been strengthened by the observation that leptin and the soluble leptin receptor are highly interrelated not only with each other but also with other intrafollicular hormones that regulate fertility.31
Preliminary interventional studies in patients with lipoatrophy and metabolic syndrome induced by highly active antiretroviral therapy have shown that r-metHuLeptin therapy in replacement doses in 6 months was associated with approximately 32% significant decrease in visceral fat mass and in improvements in insulin sensitivity, endogenous glucose production, and fasting insulin and glucose levels. In addition, a significant decrease in triglyceride levels, whole body lipolysis, and free fatty acids could also be seen.23,24 Whether r-metHuLeptin alone or in combination with other treatments will find a place in our therapeutic armamentarium for this condition remains to be elucidated in additional long-term studies. Summarizing these initial results, leptin replacement therapy might prove to be an option for patients with disorders that are associated with a new hormone deficiency state, that is, the leptin deficiency. Further studies in this area are ongoing.
THE ROLE OF LEPTIN IN METABOLISM IN STATES OF LEPTIN EXCESS
It is well established that obesity is associated with hyperleptinemia, which may reflect either leptin tolerance or leptin resistance. Despite initial hopes, placebo-controlled trials in obese subjects over periods ranging up to 24 weeks have clinically shown no impressive weight loss in leptin-treated subjects compared with placebo-treated controls.32 Given the initial high expectations for r-metHuLeptin as a potential treatment for obesity and the impressive results seen in leptin-deficient patients,6 results in subjects with garden variety obesity have thus been considered to be disappointing. More recent evidence indicates, however, that coadministration of leptin with medications that could sensitize the body to leptin’s actions could possibly provide better weight loss outcomes.33 Potential future applications of leptin in states of energy excess, that is, obesity, will be presented in detail in a paper by Wyer et al.
DISCUSSION AND FURTHER DIRECTIONS
Leptin, the prototype adipocyte–secreted hormone, the circulating levels of which communicate information regarding the amount of body’s energy reserves, is involved in the regulation of several neuroendocrine axes, immune function, and the regulation of glucose and lipid metabolism. Observational and interventional studies have revealed that leptin’s physiological and pathophysiological roles may be more important in the leptin deficiency end of the spectrum rather than in states of leptin excess. Similar to other hormone deficiency syndromes, leptin deficiency syndromes call for leptin replacement treatment in humans. Thus, r-metHuLeptin replacement could prove to be a new potentially useful medication to be added to our therapeutic armamentarium for disease states of absolute or relative leptin deficiency to restore neuroendocrine, metabolic, and immune functions. Leptin replacement in patients with anorexia nervosa, exercise-induced hypothalamic dysfunction in strenuously exercising women athletes, and/or infertility are currently under intense investigation and is a potentially forthcoming treatment in these conditions pending appropriate clinical trials. Leptin replacement therapy is currently being used for congenital leptin–deficient patients through both a mechanism involving participation in investigator-initiated clinical trials and a named patient/compassionate use mechanism. In addition, leptin replacement therapy is under an expanded access program for subjects with leptin deficiency associated with congenital or acquired lipoatrophy, such as seen in patients with HALS and associated metabolic complications. Because coadministration of both leptin and adiponectin has fully normalized insulin sensitivity in animal studies, we are currently performing clinical trails testing whether coadministration of leptin and adiponectin could have additive or synergistic effects in improving insulin resistance and metabolic syndrome. Finally, the development of leptin sensitizers and/or the results of trials evaluating the coadministration of leptin with other medications, which could act as leptin sensitizers, are anticipated with great expectations.
Acknowledgments
The authors did not receive funding for this work from any of the following organizations: National Institutes of Health, Wellcome Trust, Howard Hughes Medical Institute, and others.
This symposium was supported in part by a grant from the National Center for Research Resources (R13 RR023236).
References
- 1.Zhang Y, Proenca M, Maffei M, et al. Positional cloning of the obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 2.Laclaustra M, Corella D, Ordovas JM. Metabolic syndrome pathophysiology: the role of adipose tissue. Nutr Metab Cardiovasc Dis. 2007;17:125–139. doi: 10.1016/j.numecd.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Licinio J, Caglayan S, Ozata M, et al. Phenotypic effects of leptin replacement on morbid obesity, diabetes mellitus, hypogonadism, and behavior in leptin-deficient adults. Proc Natl Acad Sci. 2004;101:4531–4536. doi: 10.1073/pnas.0308767101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blüher S, Mantzoros CS. Leptin in humans: lessons from translational research. Am J Clin Nutr. 2009;89:991S–997S. doi: 10.3945/ajcn.2008.26788E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flier JS, Maratos-Flier E. What fuels fat. Sci Am. 2007;297:72–81. doi: 10.1038/scientificamerican0907-72. [DOI] [PubMed] [Google Scholar]
- 6.Brennan AM, Mantzoros CS. Drug insight: the role of leptin in human physiology and pathophysiology—emerging clinical applications in leptin deficient states. Nat Clin Pract Endocrinol Metab. 2006;2:1–5. doi: 10.1038/ncpendmet0196. [DOI] [PubMed] [Google Scholar]
- 7.Chan JL, Matarese G, Shetty GK, et al. Differential regulation of metabolic, neuroendocrine, and immune function by leptin in humans. Proc Natl Acad Sci USA. 2006;103:8481–8486. doi: 10.1073/pnas.0505429103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelesidis T, Mantzoros CS. The emerging role of leptin in humans. Pediatr Endocrinol Rev. 2006;3:239–348. Review. [PubMed] [Google Scholar]
- 9.Myers MG, Cowley MA, Münzberg H. Mechanisms of leptin action and leptin resistance. Annu Rev Physiol. 2008;70:537–556. doi: 10.1146/annurev.physiol.70.113006.100707. Review. [DOI] [PubMed] [Google Scholar]
- 10.Paz-Filho GJ, Babikian T, Asarnow R, et al. Leptin replacement improves cognitive development. PLoS ONE. 2008;3(8):1–7. doi: 10.1371/journal.pone.0003098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clement K, Vaisse C, Lahlou N, et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature. 1998;392:398–401. doi: 10.1038/32911. [DOI] [PubMed] [Google Scholar]
- 12.Farooqi S, Wangensteen T, Collins S, et al. Clinical and molecular genetic spectrum of congenital deficiency of the leptin receptor. N Engl J Med. 2007;356:237–247. doi: 10.1056/NEJMoa063988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Welt CK, Chan JL, Bullen J, et al. Recombinant human leptin in women with hypothalamic amenorrhea. N Engl J Med. 2004;351:987–997. doi: 10.1056/NEJMoa040388. [DOI] [PubMed] [Google Scholar]
- 14.Chan JL, Mantzoros CS. Role of leptin in energy-deprivation states: normal human physiology and clinical implications for hypothalamic amenorrhoea and anorexia nervosa. Lancet. 2005;366:74–85. doi: 10.1016/S0140-6736(05)66830-4. [DOI] [PubMed] [Google Scholar]
- 15.Chan JL, Williams CJ, Raciti P, et al. Leptin does not mediate short-term fasting-induced changes in GH pulsatility, but increases IGF-I in leptin deficiency states. J Clin Endocrinol Metab. 2008;93:2819–2827. doi: 10.1210/jc.2008-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mantzoros CM, Ozata M, Negrao AB, et al. Synchronicity of frequently sampled thyrotropin (TSH) and leptin concentrations in healthy adults and leptin-deficient subjects: evidence for possible partial TSH regulation by leptin in humans. J Clin Endocrinol Metab. 2001;86:3284–3291. doi: 10.1210/jcem.86.7.7644. [DOI] [PubMed] [Google Scholar]
- 17.Chan JL, Heist K, DePaoli AM, et al. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest. 2003;111:1409–1421. doi: 10.1172/JCI17490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozata M, Ozdemir IC, Licinio J, et al. Human leptin deficiency caused by a missense mutation: multiple endocrine defects, decreased sympathetic tone, and immune system dysfunction indicate new targets for leptin action, greater central than peripheral resistance to the effects of leptin, and spontaneous correction of leptin-mediated defects. J Clin Endocrinol Metab. 1999;84:3686–3695. doi: 10.1210/jcem.84.10.5999. [DOI] [PubMed] [Google Scholar]
- 19.Farooqi IS, Matarese G, Lord GM, et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest. 2002;110:1093–1103. doi: 10.1172/JCI15693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farooqi IS. Monogenic human obesity. Front Horm Res. 2008;36:1–11. doi: 10.1159/000115333. Review. [DOI] [PubMed] [Google Scholar]
- 21.Chan JL, Moschos SJ, Bullen J, et al. Recombinant methionyl human leptin administration activates signal transducer and activator of transcription 3 signaling in peripheral blood mononuclear cells in vivo and regulates soluble tumor necrosis factor-alpha receptor levels in humans with relative leptin deficiency. J Clin Endocrinol Metab. 2005;90:1625–1631. doi: 10.1210/jc.2004-1823. [DOI] [PubMed] [Google Scholar]
- 22.Papathanassoglou E, El-Haschimi K, Li XC, et al. Leptin receptor expression and signaling in lymphocytes: kinetics during lymphocyte activation, role in lymphocyte survival, and response to high fat diet in mice. J Immunol. 2006;176:7745–7752. doi: 10.4049/jimmunol.176.12.7745. [DOI] [PubMed] [Google Scholar]
- 23.Mantzoros CS. Whither recombinant human leptin treatment for HIV-associated lipoatrophy and the metabolic syndrome? J Clin Endocrinol Metab. 2009;94:1089–1091. doi: 10.1210/jc.2009-0340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee JH, Chan JL, Sourlas E, et al. Recombinant methionyl human leptin therapy in replacement doses improves insulin resistance and metabolic profile in patients with lipoatrophy and metabolic syndrome induced by the highly active antiretroviral therapy. J Clin Endocrinol Metab. 2006;91:2605–2611. doi: 10.1210/jc.2005-1545. [DOI] [PubMed] [Google Scholar]
- 25.Oral EA, Simha V, Ruiz E, et al. Leptin replacement therapy for lipodystrophy. N Engl J Med. 2002;346:57–78. doi: 10.1056/NEJMoa012437. [DOI] [PubMed] [Google Scholar]
- 26.Javor ED, Cochran EK, Musso C, et al. Long-term efficacy of leptin replacement in patients with generalized lipodystrophy. Diabetes. 2005;54:1994–2002. doi: 10.2337/diabetes.54.7.1994. [DOI] [PubMed] [Google Scholar]
- 27.Tsiodras S, Mantzoros C. The role of leptin and adiponectin in the HAART induced metabolic syndrome. Am J Infect Dis. 2006;2:141–152. doi: 10.3844/ajidsp.2006.141.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paz-Filho G, Esposito K, Hurwitz B, et al. Changes in insulin sensitivity during leptin replacement therapy in leptin-deficient patients. Am J Physiol Endocrinol Metab. 2008;295:E1401–E1408. doi: 10.1152/ajpendo.90450.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gavrila A, Hsu W, Tsiodras S, et al. Improvement in highly active antiretroviral therapy-induced metabolic syndrome by treatment with pioglitazone but not with fenofibrate: a 2 × 2 factorial, randomized, double-blinded, placebo-controlled trial. Clin Infect Dis. 2005;40(5):745–749. doi: 10.1086/427697. [DOI] [PubMed] [Google Scholar]
- 30.Yamauchi T, Kamon J, Waki H, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001;7:941–946. doi: 10.1038/90984. [DOI] [PubMed] [Google Scholar]
- 31.Welt CK, Schneyer AL, Heist K, et al. Leptin and soluble leptin receptor in follicular fluid. J Assist Reprod Genet. 2003;20:495–501. doi: 10.1023/B:JARG.0000013649.38415.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badman MK, Flier JS. The adipocyte as an active participant in energy balance and metabolism. Gastroenterology. 2007;132(6):2103–2115. doi: 10.1053/j.gastro.2007.03.058. Review. [DOI] [PubMed] [Google Scholar]
- 33.Roth JD, Roland BL, Cole RL, et al. Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proc Natl Acad Sci USA. 2008;105:7257–7262. doi: 10.1073/pnas.0706473105. [DOI] [PMC free article] [PubMed] [Google Scholar]