Abstract
U.S. young adults coming of age in the early 21st Century are the first cohort to grow up during the obesity epidemic; justifiably, there is much concern about their cardiovascular health. To date, however, no research has examined the extent to which there are disparities in young adult cardiovascular health across the urban-rural continuum. We examine this topic using data from the National Longitudinal Study of Adolescent to Adult Health. We find that young adults who live in metropolitan core areas exhibit more favorable cardiovascular health than individuals who live in smaller types of communities, and that population density largely accounts for this association. Further, individuals living in more densely populated areas in young adulthood relative to adolescence have better cardiovascular health than those who live in areas similar or less dense than their adolescent residence. Our results strongly suggest that the physical and social features of communities represent important contexts for young adult cardiovascular health.
Keywords: rural, urban, population density, cardiovascular health, young adulthood, Add Health
Introduction
The U.S. obesity epidemic began among adolescents in the mid- to late-1990s (Lee et al. 2011). By the late 2000s, 37% of young adults were obese and another 33% were overweight (Hussey et al. 2015; Harris 2010). The early onset and rapid rise in obesity among young adults will threaten their cardiovascular health and future work lives for decades to come. Rising inequality and the slow pace of economic recovery after the Great Recession has furthermore forced many young adults to return home to live with their parents while they finish advanced educational degrees or find employment (Fry 2013), redistributing many of these young adults to rural areas or in the micropolitan and commuting areas of cities. In our highly stratified society, however, educational and work opportunities remain increasingly concentrated in large cities (Burton et al. 2013). Given these dramatic shifts in the health, social and economic contexts in which young people live, it is critically important to understand young adult cardiovascular health in the United States and, in particular, how young adult cardiovascular health differs across residential contexts.
We use data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) to take important steps toward better understanding disparities in young adult cardiovascular health in the United States across the urban-rural continuum. We use a measure of “ideal cardiovascular health” developed by the American Heart Association (Lloyd-Jones et al. 2010) that considers body weight, blood pressure, and other indicators of cardiac and vascular health. First, we document patterns of ideal cardiovascular health among young adults across the urban-rural continuum, as well as according to patterns of residential change from adolescence to young adulthood. Second, we specify multivariate models of ideal cardiovascular health to better understand why there are differences in young adult cardiovascular health across the urban-rural continuum. We focus on the population density of the census tract within which individuals live as one potentially important explanation for differences in young adult cardiovascular health across the urban-rural continuum. We also focus on early life and adolescent factors that are predictors of both young adult geography of residence and cardiovascular health, as well as on young adult socioeconomic, social, and family structure factors that may account for cardiovascular health differences across the urban-rural continuum.
We contribute to the understanding of cardiovascular health disparities in several ways. First, research on geographic based health disparities has tended to focus on morbidity, disability, and mortality patterns among the middle-aged and elderly populations (Glasgow et al. 2004), with relatively little attention given to young adults. This is an important oversight because today’s young adults face a far different social, economic, and epidemiologic context than young adults in the past. Second, we provide greater detail on the geographic context of young adults’ residence through the use of both rural-urban commuting area codes (RUCA) and a measure of neighborhood population density based on census tracts. The RUCA codes and population density are correlated but distinct measures, and population density may be an important explanatory factor for health disparities across the rural-urban continuum. Third, we use high quality, longitudinal, individual-level data to consider geographic context of young adult residence, changes in residential context between adolescence and young adulthood, and cardiovascular health. A longitudinal analysis is particularly important because of the permeability of rural-urban boundaries and selection processes that shape individuals’ decisions to move to or stay in different locations as they make the transition to adulthood. Fourth, we identify and assess the extent to which several different sets of explanatory variables account for differences in young adult cardiovascular health across the urban-rural continuum in the United States.
Geography and Adult Health in the United States
Generally, adults who live in rural communities have poorer health than those living in more urban areas (Anderson et al. 2015; Monnat and Pickett 2011). Whereas mortality rates in the mid-20th century were higher in cities than rural areas, this pattern has since reversed (Cossman et al. 2010). Mortality is now higher in rural areas, in large part due to higher rates of heart disease (Cossman et al. 2010; Eberhardt and Pamuk 2004; Fontanella et al. 2015; Morton 2004; Singh and Siahpush 2013). Health behaviors are also generally worse in rural areas; importantly, obesity and tobacco use are more common in these areas compared to cities (Agunwamba et al. 2016; Befort et al 2012; Rhew et al. 2011; Roberts et al. 2016).
Much of the research focusing on rural health emphasizes less access to health care among adults living in rural areas. Perhaps the most well documented disparity is that health care providers are fewer and farther away in rural areas, compared with urban areas, and rural residents tend to use fewer health care services compared with their urban counterparts (Agency for Healthcare Research and Quality 2014; Caldwell et al. 2016; Hummer et al. 2004; Purnell et al. 2016). Yet health care access is at best only a partial explanation of geographic health disparities (Hartley 2004). Indeed, the economic circumstances of rural residents appears to be an important source of their worse health relative to people living in urban areas (Probst et al. 2011). Shifts in the U.S. economy have moved jobs out of production facilities in rural areas, with cities now offering more and more service, financial, and technology-based employment opportunities. These changes have resulted in fewer employment opportunities for those in rural areas (Burton et al. 2013). The lower economic well-being of people in rural areas may lead to unhealthy stress-related behaviors, such as smoking, illegal drug use (e.g., opiates), alcohol abuse, unhealthy diet, and inactivity, all of which have detrimental consequences for cardiovascular health, even in early adulthood (Pampel et al. 2010; Thoits 2010).
While the documentation of urban-rural health disparities is a fundamental first step, it is important that researchers move beyond an urban-rural dichotomy to better understand more detailed and nuanced measures of geography of residence. Most research examining geographic differences in health uses a simplified operationalization of rural versus urban residential context, which does not acknowledge the connections and blurring between rural and urban spaces (Lichter and Brown 2011). Research taking a more nuanced approach generally demonstrates that health disparities are not based on a simple urban-rural dichotomy. James (2014), for example, reports heterogeneity in mortality rates across non-urban areas of the United States; he finds that areas adjacent to small towns with populations ranging from 2,500 to 19,999 have the highest mortality rates in the United States. Cossman and colleagues (2010) also show that classifying areas as simply urban or rural obscures important heterogeneity in health patterns across U.S. geographic areas. Thus, our analysis incorporates a rural-urban continuum of residence (i.e. RUCA codes) to more comprehensively operationalize the geography of young adult residence.
Differences in cardiovascular health across the urban-rural continuum may in part be explained by the environmental features of communities. In particular, the population density of the local area in which individuals live differs across the urban-rural continuum and may help shape cardiovascular health. More densely populated areas may have greater street connectivity and walkability, and may offer more or better options for increasing physical activity and improving nutrition; access to retail outlets, health care sites, and social services may also be enhanced in densely populated areas (Galea and Vlahov 2005; Saelens et al. 2003). Higher population density may also help facilitate social connections between individuals, which has been shown to exhibit a strong association with cardiovascular health in the United States (Yang et al. 2016). Densely populated areas may also attract young adults who are highly educated and affluent because educational and high-paid employment opportunities are more plentiful in comparison with less densely populated areas (Burton et al. 2013).
Another potential explanation for differences in young adult cardiovascular health across the urban-rural continuum highlights differences among individuals that may lead them to both live outside of metropolitan cores and/or less densely populated areas and have worse cardiovascular health. Rather than the rural or small city contexts reflecting fewer economic opportunities, the low socioeconomic status of rural and small city residents may be the result of more educated individuals (or those seeking more education) leaving such areas, also known as the “brain drain” (Burton et al. 2013). Similarly, the unhealthy behaviors observed in rural and smaller urban areas may result from individuals who engage in these behaviors also preferring to live in smaller and/or less dense areas. However, little research explores the extent to which geographic health differences may be due to the composition of people living in different communities in the United States, and to our knowledge, no research examines cardiovascular health disparities across the urban-rural continuum among young adults.
To summarize, our research questions are as follows:
First, does the cardiovascular health of U.S. young adults differ according to the type of urban or rural area within which they live?
Second, to what extent does the population density of the area within which individuals live explain young adult differences in cardiovascular health across the urban-rural continuum?
Third, to what extent do demographic, socioeconomic, and behavioral compositional factors – measured both during adolescence and young adulthood – explain differences in young adult cardiovascular health across the urban-rural continuum?
Finally, do young adults who live in different geographic contexts compared to adolescence (either in terms of the urban-rural continuum or in terms of population density) exhibit better or worse cardiovascular health in young adulthood relative to those who live in similar contexts across the transition to adulthood?
Methods
Data
We use data from the National Longitudinal Study of Adolescent to Adult Health (Add Health). These data are nationally representative, following a cohort of adolescents into young adulthood. The first wave of data (Wave 1) surveyed adolescents ages 12–19 in 1994–1995, with follow-ups one year later (Wave II; 1995–1996), seven years later (Wave III; 2001–2002), and 14 years later (Wave IV; 2008–2009). Each wave of data provides a wealth of information on health, socioeconomic status, and other social circumstances. We focus on cardiovascular health and residential location in Wave IV, when respondents are aged 24–34, but also consider a number of variables from Wave I to identify factors that are associated with both residential location and young adult cardiovascular health. Our sample includes the 12,252 respondents who participated in Wave IV, have a valid sampling weight, are not pregnant or probably pregnant at the time of the survey, and are not missing on the outcome variable.
Measures
Our outcome measure is a binary indicator of ideal (versus not ideal) cardiovascular health, a concept defined by the American Heart Association (AHA). The AHA introduced ideal cardiovascular health as a tool to monitor and spur efforts to improve cardiovascular health and reduce deaths from cardiovascular diseases and stroke (Lloyd-Jones et al. 2010). It is based on seven indicators that tap into key dimensions of health behavior and health, including body weight, physical activity, smoking, diet, cholesterol, blood pressure, and blood glucose. Subsequent to the initial report identifying the concept of ideal cardiovascular health, a number of studies have demonstrated its strong association with mortality and morbidity (e.g. Dong et al. 2012; Ford et al. 2012; Yang et al. 2012). We operationalize ideal cardiovascular health using AHA guidelines defining ideal health behaviors and health factors (Lloyd-Jones et al. 2010). Based on available data in Add Health, we measure ideal cardiovascular health based on individuals exhibiting six or more of the following: (1) did not smoke in the last 30 days, (2) have a BMI less than 25, (3) had five or more physical activity sessions per week, (4) consume less than four sugar-sweetened beverages per week,1 (5) have a total cholesterol in the bottom seven deciles and no reports of lifetime hyperlipidemia diagnosis or recent use of an antihyperlipidemic medication in the previous four weeks, (6) have systolic blood pressure less than 120, diastolic blood pressure less than 80, and no reports of lifetime hypertension diagnosis or recent use of antihypertensive medications, and (7) have no report of lifetime diabetic diagnosis or recent use of anti-diabetic medication, and no indication of diabetic or pre-diabetic levels of glucose (fasting glucose less than 100 mg/dl, non-fasting glucose levels less than 200 mg/dl, and HbA1c less than 5.7).2 Smoking, physical activity, sugar sweetened beverage consumption, and diagnoses were self-reported by respondents. Interviewers measured height and weight used to calculate BMI and blood pressure. Dried blood spots were assayed to determine cholesterol and glucose levels (for details on these protocols and measures see Entzel et al. 2009; Whitsel et al. 2012; Whitsel et al. 2013).
Our main independent variable is the rural-urban commuting area codes (RUCAs) (United States Department of Agriculture 2016), which are linked to the individual records of Add Health. For both Waves I and IV, the Census tract in which the respondent resides is linked to the RUCA code. Wave IV tracts are identified using Census boundaries in the year 2000 and Wave I tracts are based on 1990 Census boundaries. RUCA codes are taken from these same Census files. RUCA categories include: metropolitan area core, metropolitan area high commuting, metropolitan area low commuting, micropolitan area core, micropolitan area high commuting, micropolitan low commuting, small town core, small town high commuting, small town low commuting, and rural areas (Morrill et al. 1999). Appendix Table 1 displays the characteristics of the 10 categories. Because some of the categories have small numbers of respondents, we combine high and low commuting zones for metropolitan, micropolitan, and small town areas. Thus, we end up with seven different RUCA categories. Further information on RUCA codes can be obtained from the USDA (2016). We measure residential change through comparing movement in or out of metropolitan core areas from adolescence (Wave I) to young adulthood (Wave IV), categorizing individuals as having lived in metropolitan core areas at both time points, at neither time point, in adolescence but not young adulthood, and in young adulthood but not adolescence. Because small percentages of individuals live in other types of locations at either Wave I or Wave IV of Add Health, we are unable to examine patterns other than metropolitan core location (versus non-metropolitan core location).
Appendix Table 1.
RUCA codes with descriptors
| Classification | Description |
|---|---|
| Metropolitan area core | 30% of the population is in an urbanized area (urbanized area has population of 50,000 or more) |
| Metropolitan area high commuting | Primary flow 30% to urbanized area |
| Metropolitan area low commuting | Primary flow 10–30% to urbanized area |
| Micropolitan area core | 30% of the population is in a large urban cluster (large urban cluster has population of 10,000 to 49,999) |
| Micropolitan area high commuting | Primary flow 30% or more to a large urban cluster |
| Micropolitan area low commuting | Primary flow 10–30% to a large urban cluster |
| Small town core | 30% of the population is in a small urban cluster (small urban cluster has population of 2500 to 9,999) |
| Small town high commuting | Primary flow 30% or more to a small urban cluster |
| Small town low commuting | Primary flow 10–30% to a small urban cluster |
| Rural areas | Primary flow is to a tract that is not an urbanized area or an urban cluster |
Source: USDA 2014
We also consider population density at the neighborhood or Census Tract level, measured as the number of people per square kilometer living in each respondent’s residential tract. For Wave IV, population density is identified with American Community Survey five-year estimates (2005–2009) and for Wave I, 1990 Census data provides values for population density. Because the distribution of this variable is skewed, we take the natural log of the value at each wave.3 We show quartiles of the original population density measure in the descriptive statistics. We also create a measure of change in population density from adolescence to young adulthood. We compare Census tract population density in Waves I and IV, and identify those people who lived in a less dense context over time, those who lived in a more densely populated area over time, and those who remained in a similarly dense area over time. Similarity in density (or stability) is defined as living in an area that was within 223 people/km2 of the individual’s adolescent population density, as this value represents the mean population density increase among those who were at the same location at Waves I and IV. We do not distinguish whether the change in population density is due to residential mobility or changes in the environment. Population density is associated with RUCA; those living in core areas have higher average density than those in commuting or rural areas, but the range of population density for each of the RUCA codes is large. Importantly, the variation in population density is sufficient to allow for simultaneous analysis of both RUCA codes and population density.
We also examine a number of factors that may be associated with both residential location and cardiovascular health in young adulthood. Sociodemographic background factors include interview age, gender, race/ethnicity, and nativity status. Interview age is years of age at time of interview, and gender is a dichotomous variable indicating if the respondent is female.4 Race/ethnicity is a mutually exclusive categorical variable that identifies individuals as non-Hispanic White, non-Hispanic Black, Hispanic, and other. Other race/ethnicity includes Asian/Pacific Islander, American Indian/Alaska Native, and those selecting “other” for race. Nativity status is a variable that includes three categories: respondents and their parents were born in the United States, respondents were born in the United States and their parents were foreign-born, and respondents were foreign born.
Other compositional factors that may explain young adult differences in cardiovascular health along the urban-rural continuum include adolescent socioeconomic status, health and health behaviors, and residential location. Socioeconomic background is operationalized through parent educational attainment and household income-to-needs collected in Wave I. Parent educational attainment is a continuous measure of years of education representing the average years for the mother and father, or the single measure for those with information only for the mother or father. Income-to-needs is the ratio of the reported household income to the U.S. census-defined poverty threshold for that year and household size.
Adolescent health includes BMI, depressive symptoms, smoking status, self-rated health, number of physical activity sessions, and alcohol consumption, all measured in Wave I. BMI is measured the same as young adult BMI, but height and weight are self-reported in adolescence.5 Depressive symptoms is a continuous, standardized measure combining responses to 19 questions from the Center for Epidemiological Studies – Depression (CES-D) battery. Smoking status is a dichotomous indicator representing whether the respondent reported any smoking in the last 30 days. Self-rated health in adolescence is a five point scale ranging from poor to excellent. Number of physical activity sessions combines together how often the respondent reports participating in activities in the last seven days. Three questions capture a range of activities, such as participation in sports and working out at the gym. Alcohol consumption is a categorical indicator representing alcohol consumption in the previous 12 months. Those reporting no alcohol consumption are compared to those who report usually consuming one drink, two drinks, or more than two drinks during the times they had an alcoholic drink.
A number of indicators measure achieved SES and the social environment in young adulthood, which also represent potential explanations for cardiovascular health differences across the urban-rural continuum. Educational attainment, household income-to-needs, and employment status represent young adult SES. Educational attainment includes categories for less than high school, high school diploma, some college, and college degree or more (referent). Income-to-needs is a continuous measure that is the ratio of the household’s total income to the poverty threshold defined by the U.S. Census for each year and household size. Employment status is represented with three categories: full-time employment (30+ hours per week), part-time employment (10–29 hours per week), and unemployed (less than 10 hours per week). We define individuals as having high social integration if they report two or more of the following: being married, having six or more close friends, attending church 12 or more times in the past year, and volunteering in the past year. Those meeting this criterion are coded with a “1” for high social integration, and all others are coded “0”. We create a dichotomous measure for young adults who live with children using the Wave IV household roster.
Analytic Approach
We first examine descriptive statistics of ideal cardiovascular health across young adult RUCA codes, young adult population density, movement into or out of metropolitan core areas from adolescence into young adulthood, and changes in population density. Because there are no studies examining the health correlates of a nationally-representative sample of U.S. young adults by residential location, we devote considerable space to describing these patterns. Our logistic regression analysis begins by baseline differences in young adult cardiovascular health across the urban-rural continuum. Subsequently, we add in substantive groups of characteristics (population density, sociodemographic factors, adolescent characteristics, and young adult characteristics) to the models to assess the extent to which they help explain associations between the RUCA measures and ideal cardiovascular health. We do not directly compare results from different logistic regression models, but base our conclusions on general patterns. Variance inflation factor tests produced no evidence of multicollinearity.
All analyses adjust for the complex sampling design to ensure representativeness. We use multiple imputation for those who are missing values on some independent variables to retain the full sample. All independent and dependent variables are used to inform the imputation model. We do not impute values for our outcome variable, ideal CVH, and we have complete information for young adult RUCA codes, young adult population density, adolescent RUCA codes, age, gender, and young adult educational attainment. We impute less than 1% of values for: race/ethnicity, nativity status, adolescent depressive symptoms, adolescent self-rated health, adolescent physical activity, young adult marital status, living with children, young adult employment, and adolescent population density. We impute 2.2% of values for parent education, 23.5% for adolescent income-to-needs, 2.5% for adolescent BMI, 17.9% for adolescent smoking, 1.7% for adolescent alcohol consumption, and 6.6% for young adult income-to-needs.
Results
Descriptive Results
Table 1 displays descriptive statistics. Just 7% of young adults aged 24–32 has ideal cardiovascular health. The average number of ideal indicators for individuals is 3.32, or just under one-half of the maximum of 7. These figures clearly indicate that this young adult cohort has far from ideal cardiovascular health. The percentages of young adults with healthy physical activity (54%), who are nonsmokers (60%), who have ideal blood sugar (62%), and who have ideal cholesterol (65%), while far from 100%, are much higher than the percentages with healthy BMI (33%), who consume few or no sugar-sweetened beverages (29%), and who have ideal blood pressure (29%), for which only one-third or fewer exhibit healthy levels.6
Table 1.
Weighted means of young adult ideal cardiovascular health (CVH) across residential location measures
| Population | Ideal CVH (6–7 indicators) | # ideal CVH indicators | Ideal CVH indicators
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI<25 | 5+ physical activity sessions | ≤3 SSB in last week | Not current smoker | Ideal blood sugar | Ideal blood pressure | Ideal cholesterol | ||||
|
|
|
|
||||||||
| Population | 0.07 | 3.32 | 0.33 | 0.54 | 0.29 | 0.60 | 0.62 | 0.29 | 0.65 | |
| Young adult RUCA | ||||||||||
| Metropolitan core | 0.71 | 0.07 | 3.39 | 0.34 | 0.55 | 0.31 | 0.62 | 0.63 | 0.30 | 0.64 |
| Metropolitan high/low commuting | 0.10 | 0.06 | 3.25 | 0.30 | 0.52 | 0.27 | 0.56 | 0.64 | 0.30 | 0.65 |
| Micropolitan core | 0.07 | 0.06 | 3.17 | 0.28 | 0.50 | 0.26 | 0.61 | 0.59 | 0.25 | 0.69 |
| Micropolitan high/low commuting | 0.03 | 0.04 | 2.99 | 0.30 | 0.50 | 0.16 | 0.55 | 0.57 | 0.28 | 0.63 |
| Small town core | 0.03 | 0.03 | 3.15 | 0.28 | 0.49 | 0.25 | 0.53 | 0.60 | 0.32 | 0.68 |
| Small town high/low commuting | 0.02 | 0.06 | 3.01 | 0.31 | 0.51 | 0.20 | 0.52 | 0.61 | 0.23 | 0.64 |
| Rural | 0.04 | 0.04 | 3.18 | 0.31 | 0.54 | 0.25 | 0.54 | 0.62 | 0.26 | 0.67 |
| Young adult population density | ||||||||||
| <186.06 people/km2 | 0.28 | 0.05 | 3.16 | 0.29 | 0.52 | 0.25 | 0.56 | 0.61 | 0.28 | 0.66 |
| 186.08 – 955.90 people/km2 | 0.26 | 0.07 | 3.36 | 0.33 | 0.52 | 0.31 | 0.62 | 0.64 | 0.30 | 0.63 |
| 956.00– 2352.27 people/km2 | 0.27 | 0.07 | 3.34 | 0.35 | 0.54 | 0.30 | 0.59 | 0.63 | 0.29 | 0.64 |
| 2353+ people/km2 | 0.19 | 0.08 | 3.49 | 0.35 | 0.58 | 0.31 | 0.66 | 0.61 | 0.32 | 0.66 |
| Adolescent to young adult RUCA | ||||||||||
| Metro core to metro core | 0.63 | 0.07 | 3.37 | 0.34 | 0.55 | 0.30 | 0.61 | 0.63 | 0.30 | 0.64 |
| Metro core to other | 0.12 | 0.06 | 3.26 | 0.30 | 0.53 | 0.28 | 0.56 | 0.65 | 0.28 | 0.65 |
| Other to metro core | 0.08 | 0.09 | 3.50 | 0.36 | 0.55 | 0.32 | 0.66 | 0.64 | 0.32 | 0.65 |
| Other to other | 0.17 | 0.05 | 3.10 | 0.29 | 0.50 | 0.22 | 0.57 | 0.58 | 0.27 | 0.67 |
| Adolescent to young adult change in density | ||||||||||
| Decreasing | 0.25 | 0.06 | 3.27 | 0.30 | 0.54 | 0.28 | 0.61 | 0.60 | 0.29 | 0.65 |
| Stable | 0.36 | 0.05 | 3.19 | 0.31 | 0.52 | 0.26 | 0.57 | 0.62 | 0.28 | 0.64 |
| Increasing | 0.38 | 0.09 | 3.48 | 0.37 | 0.56 | 0.32 | 0.63 | 0.64 | 0.31 | 0.65 |
Source: Add Health
Notes: Analysis adjust for complex sampling design. N=12,252
Nearly three-quarters (71%) of young adults live in a metropolitan core, with an additional 10% in high or low commuting areas around these cities. Smaller numbers of individuals live in tracts described as micropolitan, small town, or rural. We divide young adult population density into quartiles in Table 1, so each represents roughly one-quarter of young adults. Table 1 also shows changes in residential context from adolescence to young adulthood. The majority of young adults (63%) lived in a metropolitan core in both adolescence and young adulthood. Smaller proportions lived in a metropolitan core in adolescence and a smaller community in adulthood (12%), lived in a smaller community in adolescence and in a metropolitan core during young adulthood (8%), or did not live in a metropolitan core in either adolescence or young adulthood (17%). The largest proportion of individuals (38%) experienced an increase in population density from adolescence to adulthood, though nearly the same amount lived in a place with similar density (36%).
Although levels of ideal cardiovascular health are very low among young adults living in all types of places, there are clear differences across geographic locations. Individuals living in metropolitan cores and denser areas demonstrate the highest proportion with ideal cardiovascular health, as well as the highest average number of ideal cardiovascular health indicators. Rural areas lag well behind, though small town core areas have the lowest percentage of individuals with ideal CVH. The results demonstrate that RUCA codes do not demonstrate a linear relationship with ideal CVH, in line with previous research showing that mortality rates are not graded across rural-urban continuum codes (James et al. 2014). People living in higher density areas in young adulthood also exhibit higher proportions of ideal cardiovascular health. Focusing on changes in the geography of residence across the transition to adulthood, those living in a metropolitan core in young adulthood who lived in a smaller community in adolescence have the highest proportion of individuals with ideal cardiovascular health, followed by those living in metropolitan core areas in both adolescence and young adulthood. The longitudinal approach to population density indicates that ideal cardiovascular health is most common among those who experience increases in density during the transition to adulthood. Young adults in rural and less densely-settled areas in young adulthood suffer a significant cardiovascular health disparity that will likely be revealed in higher rates of mortality in older age and in lower overall life expectancy.
Additional descriptive statistics (Appendix Tables 2 and 3) demonstrate that there are systematic individual differences in many social, economic, behavioral, and health characteristics by both RUCA code of residence and population density. Notably, those living in more dense areas have higher adolescent and young adult SES, and generally better adolescent health and health behaviors.
Appendix Table 2.
Weighted means of covariates, across residential location categories in young adulthood (Wave IV)
| Population | Young adult RUCA
|
Young adult population density in people/km2
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Metropolitan | Micropolitan | Small town | Rural | <186.06 | 186.08 – 955.90 | 956.00– 2352.27 | 2353+ | |||||
| core | high/low commuting | core | high/low commuting | core | high/low commuting | |||||||
|
|
|
|||||||||||
| Population | 0.71 | 0.10 | 0.07 | 0.03 | 0.03 | 0.02 | 0.04 | 0.28 | 0.26 | 0.27 | 0.19 | |
| Sociodemographics | ||||||||||||
| Age at Wave IV | 28.38 | 28.38 | 28.48 | 28.33 | 28.25 | 28.35 | 28.37 | 28.43 | 28.41 | 28.34 | 28.34 | 28.46 |
| Female | 0.49 | 0.49 | 0.47 | 0.47 | 0.52 | 0.48 | 0.43 | 0.49 | 0.49 | 0.49 | 0.49 | 0.47 |
| Race/ethnicity | ||||||||||||
| White | 0.69 | 0.64 | 0.85 | 0.67 | 0.81 | 0.73 | 0.79 | 0.85 | 0.80 | 0.74 | 0.65 | 0.48 |
| Black | 0.15 | 0.15 | 0.09 | 0.25 | 0.13 | 0.24 | 0.19 | 0.12 | 0.13 | 0.15 | 0.16 | 0.18 |
| Hispanic | 0.12 | 0.16 | 0.05 | 0.04 | 0.04 | 0.01 | 0.01 | 0.01 | 0.04 | 0.09 | 0.15 | 0.25 |
| Other | 0.04 | 0.05 | 0.01 | 0.04 | 0.03 | 0.02 | 0.01 | 0.01 | 0.03 | 0.03 | 0.04 | 0.09 |
| Nativity status | ||||||||||||
| U.S. born and parents U.S. born | 0.87 | 0.84 | 0.94 | 0.95 | 0.95 | 0.97 | 0.99 | 0.98 | 0.95 | 0.90 | 0.87 | 0.72 |
| Parents foreign-born | 0.07 | 0.09 | 0.03 | 0.03 | 0.05 | 0.02 | 0.00 | 0.01 | 0.03 | 0.06 | 0.08 | 0.16 |
| Foreign-born | 0.05 | 0.07 | 0.03 | 0.02 | 0.01 | 0.01 | 0.00 | 0.01 | 0.02 | 0.04 | 0.05 | 0.12 |
| Background SES (Wave I) | ||||||||||||
| Parent education | 13.06 | 13.18 | 12.86 | 13.18 | 12.74 | 12.38 | 12.40 | 12.19 | 12.76 | 13.24 | 13.16 | 13.07 |
| Income-to-needs | 2.90 | 3.04 | 2.77 | 2.52 | 2.59 | 2.90 | 3.00 | 2.35 | 2.64 | 2.93 | 2.99 | 3.13 |
| Adolescent health (Wave I) | ||||||||||||
| BMI | 22.56 | 22.41 | 22.83 | 22.67 | 22.53 | 23.05 | 23.69 | 23.34 | 22.88 | 22.34 | 22.45 | 22.55 |
| Depressive symptoms | −0.05 | −0.05 | −0.08 | −0.08 | 0.00 | −0.02 | −0.15 | −0.06 | −0.04 | −0.08 | −0.05 | −0.03 |
| Smoker | 0.34 | 0.32 | 0.39 | 0.31 | 0.44 | 0.38 | 0.40 | 0.43 | 0.40 | 0.34 | 0.34 | 0.26 |
| Self-rated health | 3.86 | 3.88 | 3.83 | 3.84 | 3.87 | 3.71 | 3.83 | 3.77 | 3.83 | 3.89 | 3.86 | 3.89 |
| Physical activity sessions | 5.46 | 5.53 | 5.31 | 5.49 | 5.14 | 5.45 | 5.52 | 4.83 | 5.25 | 5.49 | 5.44 | 5.76 |
| Alcohol consumption | ||||||||||||
| None | 0.52 | 0.52 | 0.49 | 0.57 | 0.50 | 0.55 | 0.49 | 0.50 | 0.50 | 0.53 | 0.52 | 0.54 |
| usually 1 drink | 0.10 | 0.10 | 0.09 | 0.10 | 0.11 | 0.08 | 0.09 | 0.10 | 0.09 | 0.10 | 0.10 | 0.11 |
| usually 2 drinks | 0.08 | 0.08 | 0.07 | 0.10 | 0.09 | 0.09 | 0.06 | 0.07 | 0.08 | 0.08 | 0.08 | 0.07 |
| usually >2 drinks | 0.30 | 0.30 | 0.35 | 0.23 | 0.30 | 0.28 | 0.36 | 0.33 | 0.32 | 0.30 | 0.30 | 0.27 |
| Young adult factors | ||||||||||||
| Educational attainment | ||||||||||||
| Less than high school | 0.09 | 0.08 | 0.10 | 0.08 | 0.10 | 0.12 | 0.09 | 0.15 | 0.10 | 0.09 | 0.09 | 0.07 |
| High school diploma | 0.27 | 0.25 | 0.32 | 0.30 | 0.35 | 0.39 | 0.45 | 0.38 | 0.35 | 0.25 | 0.25 | 0.24 |
| Some college | 0.34 | 0.34 | 0.36 | 0.38 | 0.37 | 0.32 | 0.31 | 0.28 | 0.35 | 0.35 | 0.35 | 0.30 |
| College degree or more | 0.30 | 0.33 | 0.22 | 0.24 | 0.17 | 0.17 | 0.15 | 0.20 | 0.20 | 0.31 | 0.31 | 0.38 |
| Household income-to-needs | 3.74 | 3.97 | 3.73 | 3.12 | 3.03 | 2.41 | 2.77 | 2.73 | 3.23 | 3.89 | 3.78 | 4.20 |
| Employment | ||||||||||||
| Unemployed | 0.71 | 0.72 | 0.73 | 0.69 | 0.70 | 0.61 | 0.72 | 0.63 | 0.68 | 0.72 | 0.71 | 0.72 |
| Part-time | 0.09 | 0.09 | 0.08 | 0.08 | 0.11 | 0.07 | 0.09 | 0.07 | 0.08 | 0.09 | 0.10 | 0.08 |
| Full-time | 0.20 | 0.19 | 0.19 | 0.23 | 0.19 | 0.32 | 0.19 | 0.31 | 0.23 | 0.19 | 0.19 | 0.20 |
| High social integration | 0.52 | 0.50 | 0.54 | 0.57 | 0.65 | 0.57 | 0.54 | 0.59 | 0.56 | 0.54 | 0.51 | 0.45 |
| Living with children | 0.46 | 0.42 | 0.56 | 0.54 | 0.62 | 0.64 | 0.56 | 0.57 | 0.58 | 0.47 | 0.43 | 0.32 |
Source: Add Health.
Notes: Analysis adjust for complex sampling design. N=12,252
Appendix Table 3.
Weighted means of covariates, across transition to adulthood residential location categories
| Population | Adolescent to young adult
|
Adolescent to young adult change in population density
|
||||||
|---|---|---|---|---|---|---|---|---|
| Metro core to metro core | Metro core to other | Other to metro core | Other to other | Decreasing | Stable | Increasing | ||
|
|
|
|
||||||
| Population | 0.63 | 0.12 | 0.08 | 0.16 | 0.25 | 0.36 | 0.38 | |
| Sociodemographics | ||||||||
| Age at Wave IV | 28.38 | 28.40 | 28.42 | 28.19 | 28.37 | 28.51 | 28.38 | 28.30 |
| Female | 0.49 | 0.49 | 0.46 | 0.52 | 0.49 | 0.48 | 0.50 | 0.48 |
| Race/ethnicity | ||||||||
| White | 0.69 | 0.64 | 0.87 | 0.69 | 0.73 | 0.57 | 0.77 | 0.68 |
| Black | 0.15 | 0.14 | 0.05 | 0.24 | 0.24 | 0.19 | 0.13 | 0.14 |
| Hispanic | 0.12 | 0.17 | 0.06 | 0.03 | 0.01 | 0.18 | 0.07 | 0.13 |
| Other | 0.04 | 0.05 | 0.02 | 0.05 | 0.02 | 0.06 | 0.03 | 0.05 |
| Nativity status | ||||||||
| U.S. born and parents U.S. born | 0.87 | 0.83 | 0.93 | 0.93 | 0.97 | 0.81 | 0.92 | 0.86 |
| Parents foreign-born | 0.07 | 0.10 | 0.03 | 0.03 | 0.02 | 0.10 | 0.05 | 0.08 |
| Foreign-born | 0.05 | 0.07 | 0.03 | 0.03 | 0.01 | 0.08 | 0.03 | 0.06 |
| Background SES (Wave I) | ||||||||
| Parent education | 13.06 | 13.10 | 12.96 | 13.82 | 12.59 | 12.71 | 12.86 | 13.47 |
| Income-to-needs | 2.90 | 3.04 | 3.01 | 3.00 | 2.27 | 2.62 | 2.73 | 3.26 |
| Adolescent health (Wave I) | ||||||||
| BMI | 22.55 | 22.47 | 22.62 | 21.95 | 23.12 | 22.72 | 22.73 | 22.29 |
| Depressive symptoms | −0.05 | −0.04 | −0.11 | −0.10 | −0.04 | −0.03 | −0.03 | −0.09 |
| Smoker | 0.34 | 0.33 | 0.40 | 0.28 | 0.37 | 0.33 | 0.39 | 0.30 |
| Self-rated health | 3.86 | 3.87 | 3.87 | 3.94 | 3.78 | 3.83 | 3.82 | 3.93 |
| Physical activity sessions | 5.46 | 5.53 | 5.50 | 5.53 | 5.13 | 5.27 | 5.40 | 5.65 |
| Alcohol consumption | ||||||||
| None | 0.52 | 0.52 | 0.48 | 0.56 | 0.55 | 0.51 | 0.51 | 0.54 |
| usually 1 drink | 0.10 | 0.10 | 0.10 | 0.10 | 0.09 | 0.10 | 0.09 | 0.11 |
| usually 2 drinks | 0.08 | 0.08 | 0.08 | 0.07 | 0.09 | 0.08 | 0.08 | 0.07 |
| usually >2 drinks | 0.30 | 0.30 | 0.35 | 0.28 | 0.27 | 0.31 | 0.31 | 0.28 |
| Young adult factors (Wave IV) | ||||||||
| Educational attainment | ||||||||
| Less than high school | 0.09 | 0.09 | 0.10 | 0.04 | 0.11 | 0.11 | 0.11 | 0.06 |
| High school diploma | 0.27 | 0.26 | 0.31 | 0.17 | 0.37 | 0.28 | 0.33 | 0.22 |
| Some college | 0.34 | 0.34 | 0.37 | 0.34 | 0.33 | 0.35 | 0.33 | 0.34 |
| College degree or more | 0.30 | 0.32 | 0.22 | 0.45 | 0.20 | 0.26 | 0.23 | 0.38 |
| Household income-to-needs | 3.74 | 3.94 | 3.61 | 4.22 | 2.85 | 3.68 | 3.38 | 4.11 |
| Employment | ||||||||
| Unemployed | 0.71 | 0.71 | 0.71 | 0.77 | 0.67 | 0.70 | 0.69 | 0.73 |
| Part-time | 0.09 | 0.09 | 0.08 | 0.07 | 0.08 | 0.10 | 0.09 | 0.08 |
| Full-time | 0.20 | 0.20 | 0.20 | 0.16 | 0.25 | 0.20 | 0.23 | 0.18 |
| High social integration | 0.52 | 0.49 | 0.54 | 0.57 | 0.59 | 0.50 | 0.53 | 0.52 |
| Living with children | 0.46 | 0.42 | 0.55 | 0.40 | 0.58 | 0.50 | 0.53 | 0.38 |
Source: Add Health.
Notes: Analysis adjust for complex sampling design. N=12,252
Multivariate Models of Young Adult Cardiovascular Health by Geography of Residence
Table 2 presents odds ratios and significance levels from logistic regression models predicting ideal cardiovascular health. Model 1 shows that, compared with those residing in metropolitan core areas, young adults living in metropolitan commuting, micropolitan commuting, small town core, and rural areas are significantly less likely to have ideal cardiovascular health. Those living in micropolitan core and small town commuting areas exhibit no difference in ideal cardiovascular health relative to individuals in metropolitan core areas.
Table 2.
Odds ratios for logistic regression models predicting young adult ideal cardiovascular health
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Young adult RUCA (metro core) | |||||
| Metropolitan high/low commuting | 0.73* | 0.99 | 1.12 | 1.12 | 1.11 |
| Micropolitan core | 0.80 | 0.94 | 1.15 | 1.14 | 1.28 |
| Micropolitan high/low commuting | 0.52+ | 0.76 | 0.88 | 0.90 | 0.95 |
| Small town core | 0.35** | 0.46* | 0.55 | 0.60 | 0.69 |
| Small town high/low commuting | 0.75 | 1.14 | 1.62 | 1.95 | 2.13+ |
| Rural | 0.50* | 0.77 | 0.95 | 0.90 | 0.87 |
| Young adult logged population density | 1.10* | 1.17*** | 1.12** | 1.08* | |
| Age at Wave IV | 0.95 | 1.06+ | 1.05 | ||
| Female | 4.22*** | 4.34*** | 3.92*** | ||
| Race/ethnicity (White) | |||||
| Black | 0.25*** | 0.32*** | *** | ||
| Hispanic | 0.51*** | 0.86 | 0.97 | ||
| Other | 0.93 | 0.88 | 0.87 | ||
| Nativity (US born) | |||||
| Parents foreign born | 0.86 | 0.88 | 0.80 | ||
| Foreign born | 1.84** | 1.81* | 1.67* | ||
| Background SES | |||||
| Income-needs at Wave I | 1.02 | 1.01 | |||
| Parent education at Wave I | 1.16*** | 1.08** | |||
| Adolescent health (Wave I) | |||||
| BMI | 0.84*** | 0.84*** | |||
| Depressive symptoms | 0.94 | 1.00 | |||
| Smoker | 0.68* | 0.81 | |||
| Self-rated health | 1.14* | 1.08 | |||
| Physical activity sessions | 1.01 | 1.00 | |||
| Alcohol consumption (none) | |||||
| usually 1 drink | 1.03 | 0.96 | |||
| usually 2 drinks | 0.95 | 0.85 | |||
| usually >2 drinks | 1.09 | 1.01 | |||
| Adolescent residence (Wave I) | |||||
| Logged population density | 1.00 | 1.01 | |||
| RUCA code (metro core) | |||||
| Metro/micro high/low commuting | 1.20 | 1.11 | |||
| Micro core | 1.22 | 1.13 | |||
| Small town core | 0.78 | 0.67 | |||
| Small town high commuting | 0.91 | 0.86 | |||
| Rural area | 1.60* | 1.50* | |||
| Young adult factors (Wave IV) | |||||
| Educational attainment (BA+) | |||||
| <HS | 0.37** | ||||
| HS | *** | ||||
| Some college | 0.53*** | ||||
| Income-to-needs | 1.04** | ||||
| Employed (full-time) | |||||
| Not employed | 1.14 | ||||
| Part-time | 1.12 | ||||
| High social integration | 1.28* | ||||
| Living with kids | 0.91 | ||||
| Constant | 0.08*** | 0.04*** | 0.05** | 0.01*** | 0.07** |
Source: Add Health
Notes: Analysis adjust for complex sampling design. Referent is in parentheses. N=12,252
p<.10
p<.05
p<.01
p<.001
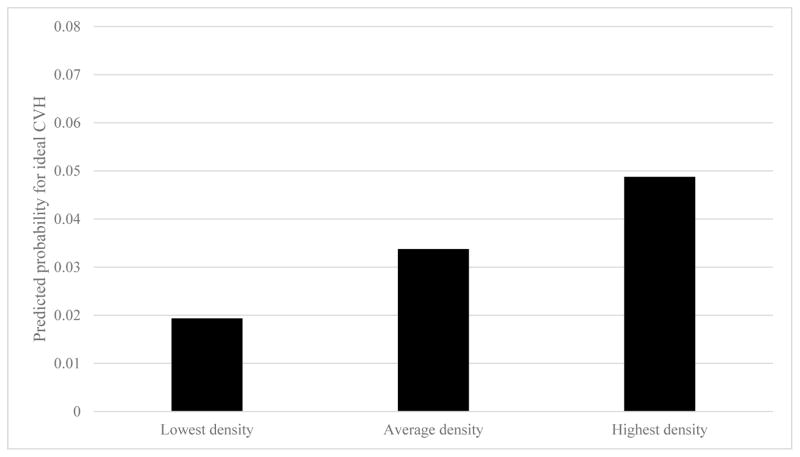
When population density is added in Model 2, only small town core residents have significantly decreased odds of ideal cardiovascular health. With the addition of demographic controls in Model 3, there are no differences in ideal cardiovascular health across the RUCA codes. Population density is a particularly important explanation for young adult differences in cardiovascular health across the urban-rural continuum. Moreover, individuals who live in more densely populated areas are more likely to have ideal cardiovascular health compared to people who live in less densely populated areas. These results remain in subsequent models, with population density attenuating somewhat with the inclusion of additional covariates. For example, the inclusion of young adult educational attainment, income-to-needs, employment status, social integration, and living with children in Model 5 results in a 33 percent reduction in the association between population density and ideal cardiovascular health (compared to Model 4); the associations between education, income, and ideal cardiovascular health are particularly strong. This suggests that the higher socioeconomic status of individuals who live in more densely populated areas is in part responsible for their more favorable young adult cardiovascular health. Nonetheless, young adults who live in higher density areas continue to exhibit significantly higher odds of ideal cardiovascular health, net of background and young adult factors. Figure 1, Panel A displays the predicted probabilities of ideal cardiovascular health for individuals living in the densest, least dense, and average density areas (and otherwise have characteristics equivalent to the referent group or population mean). Although the overall levels of ideal cardiovascular health are low, the relative differences in predicted probabilities are large, with individuals living in the highest density areas in young adulthood exhibiting more than twice the probability of being in ideal cardiovascular health compared with those who living in low density areas.7
Figure 1. Predicted probabilities of ideal cardiovascular health across young adult population density.
Source: Add Health.
N=12, 252.
Notes: Predicted probabilies computed from Table 2, Model 5. Other than population density measures, calculations assume characteristics equivalent to the referent group (for categorical variables) or sample mean (for continuous variables). Analysis adjusts for complex sampling design.
Table 3 presents models examining the same outcome, ideal cardiovascular health, but now considers residential location patterns of stability and change from adolescence to young adulthood. Compared to individuals who lived in metropolitan core areas in both adolescence and young adulthood, those who did not live in metropolitan core areas in either life stage have 38% reduced odds of ideal cardiovascular health in young adulthood. Further, those who lived in metropolitan core areas as adolescents but who live in smaller communities in young adulthood have 25 percent lower odds of ideal cardiovascular health in young adulthood compared with those who consistently lived in a metropolitan core. These differences do not persist once other variables are considered, and like the previous set of results, population density and demographic characteristics account for the observed differences across the rural-urban continuum categories. Model 2 demonstrates that individuals who live in a more densely populated area in young adulthood compared with their residential context in adolescence have higher odds of ideal cardiovascular health relative to those who remained in a similarly dense area during the transition to adulthood. Adolescent and young adult factors appear to attenuate the association, but those who live in increasingly dense residential areas are 32% more likely to have ideal cardiovascular health, net of all covariates (Model 5).8
Table 3.
Odds ratios from logistic regression models predicting young adult ideal cardiovascular health
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Adolescent to young adult RUCA (metro core to metro core) | |||||
| Metro core to other | 0.75+ | 0.89 | 0.84 | 0.90 | 0.98 |
| Other to metro core | 1.27 | 1.16 | 1.16 | 1.06 | 0.96 |
| Other to Other | 0.62** | 0.71* | 0.81 | 1.00 | 1.06 |
| Change in population density (stable) | |||||
| Decreasing | 0.96 | 1.14 | 1.13 | 1.06 | |
| Increasing | 1.48** | 1.65*** | 1.43** | 1.32* | |
| Age at Wave IV | 0.96 | 1.06+ | 1.05 | ||
| Female | 4.18*** | 4.33** | 3.93*** | ||
| Race/ethnicity (White) | |||||
| Black | 0.27*** | 0.34** | 0.41*** | ||
| Hispanic | 0.56** | 0.91 | 1.02 | ||
| Other | 0.96 | 0.92 | 0.91 | ||
| Nativity (US born) | |||||
| Parents foreign born | 0.92 | 0.90 | 0.81 | ||
| Foreign born | 1.99** | 1.85** | 1.71* | ||
| Background SES (Wave I) | |||||
| Income-needs | 1.02+ | 1.01 | |||
| Parent education | 1.16*** | 1.08** | |||
| Adolescent health (Wave I) | |||||
| BMI | 0.84*** | 0.84** | |||
| Depressive symptoms | 0.94 | 1.00 | |||
| Smoker | 0.67** | 0.81 | |||
| Self-rated health | 1.13+ | 1.08 | |||
| Physical activity sessions | 1.01 | 1.00 | |||
| Alcohol consumption (none) | |||||
| usually 1 drink | 1.04 | 0.97 | |||
| usually 2 drinks | 0.95 | 0.85 | |||
| usually >2 drinks | 1.09 | 1.01 | |||
| Young adult factors (Wave IV) | |||||
| Educational attainment (BA+) | |||||
| <HS | 0.38** | ||||
| HS | 0.35*** | ||||
| Some college | 0.53*** | ||||
| Income-to-needs | 1.05** | ||||
| Employed (full-time) | |||||
| Not employed | 1.14 | ||||
| Part-time | 1.13 | ||||
| High social integration | 1.27* | ||||
| Living with kids | 0.89 | ||||
| Constant | 0.08*** | 0.06*** | 0.09** | 0.01*** | 0.10* |
Source: Add Health
Notes: Analysis adjust for complex sampling design. Referent is in parentheses. N=12,252
p<.10
p<.05
p<.01
p<.001
Discussion
This study seeks to identify the extent to which US young adult cardiovascular health differs across the rural-urban continuum and, if so, what explanations may account for this difference. Our results show that young adults who live in metropolitan core areas (which encompasses 71% of young adults) exhibit better cardiovascular health than young adults who live outside of these core areas. Even more striking, young adults who live in low density areas have worse cardiovascular health than young adults who live in more dense areas. Further, the strong association between the population density of individuals’ Census tract and their odds of ideal cardiovascular health explains the association between rural-urban residence and cardiovascular health in our statistical models. The strength of the association between density and cardiovascular health is further bolstered by our examination of residential changes across the transition to adulthood, which shows that individuals who lived in more densely populated areas as they transitioned to adulthood have higher odds of ideal cardiovascular health compared with individuals who lived in similarly dense or less dense areas over time. This finding supports results from other studies demonstrating greater physical activity and reduced BMI among residents of dense or compact areas (e.g. Ewing et al. 2014; Frank et al. 2005; James et al. 2013)
The mechanisms behind the strong association between young adult residence in a densely populated context and cardiovascular health could be compositional in that there are other unobserved factors we have not accounted for that may explain the association. We have controlled for adolescent health behaviors and health factors to help mitigate selection effects, but it could be that there are other factors shaping the migration of healthy young adults to denser areas. This intra-national process could be similar to that in the international migration and health literature, which has shown that immigrants have better health than their US-born counterparts (Hummer et al. 2015). Alternatively, mechanisms underlying the association may be contextual in that it is the physical and social environment in dense areas that promotes health (Sparks 2012), and cardiovascular health in particular. Perhaps most likely, the environments and people within dense areas co-exist in a reciprocal relationship that reinforce certain patterns and behaviors (Cummins et al. 2007). Individuals have preferences and constraints for where they live, including opinions on walkability and proximity to recreation (Berry et al. 2010). Built and social environments may sort these preferences into different lifestyles. Families seek large homes, nice cars, and attractive lawns as a sign of financial well-being and comfort, and as a source of differentiation from those of lower status, such as families living in inner city public housing. Low density neighborhoods make large homes and cars affordable and convenient. These relatively large homes and cars make it easy to obtain, transport, and store large amounts of non-perishable foods, and in turn, are more comfortable for bigger bodies. Government institutions also support low density neighborhoods with large homes and cars, providing wide roads and free parking, among other comforts (Jackson 2009). In contrast, other individuals may seek out dense areas for their activity, diversity, and vibrancy. These dense areas are marked by public spaces that can be difficult for bigger bodies to navigate (Brewis et al. 2016). Expenses associated with owning a car, driving, and parking in dense areas may incentivize walking, cycling, and use of public transportation, and smaller residences may prevent the acquisition of large amounts of food. Across these different communities, the environments and social and cultural norms can propagate a way of life, with important health consequences.
Prior research has often used a rural-urban distinction to measure lifestyle and health differences across residential areas, but this simple dichotomy obscures the complexity of location in today’s increasingly blurred society (Lichter and Brown 2011). The enhanced rural-urban RUCA continuum is a much more refined categorization of residential space, but these rigid categorizations cannot accommodate the blurring, crossing, and shifting of boundaries. Yet, environmental features still distinguish communities and the residents that reside in them from one another. And based on our findings, the population density within which individuals live appears to be a dimension of residential life that is especially important for a set of important health outcomes in early adulthood and, thus, a dimension that cannot be ignored in future work on the topic. Moreover, density is not only a feature of large metropolitan cities but also of smaller cities, small towns, and rural areas, which may make it an important consideration for population health in all types of residential spaces.
As individuals select into different communities and these environments accommodate and encourage different lifestyles, health disparities across contexts may grow. We focus on ideal cardiovascular health here to foreshadow future cardiovascular conditions that today’s young adults have yet to experience. For today’s young adults whose future health and longevity are threatened by the obesity epidemic, these spatial differences may only become more important in the future. Fairly strong differences across population density may widen as young adults settle into their current locations, raise families, and perpetuate their lifestyles. At the same time, rural-urban interdependence may obscure spatial disparities. Research on health and place will need to consider how boundaries are blurred and traversed to identify salient features of social and physical environments.
Acknowledgments
This research was supported by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award (F32 HD 085599) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. We are grateful to the Carolina Population Center and its NIH Center grant (P2C HD050924) for general support. We thank conference attendees, two anonymous reviewers, and the editors Dan Lichter and Jim Ziliak for their helpful comments. A prior version of this paper was presented at The New Rural-Urban Interface Conference in September 2016.
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Footnotes
The AHA healthy diet components include levels of fruit and vegetable, fish, whole grain, sodium, and sugar-sweetened beverage consumption (Lloyd-Jones et al. 2010). We set the sugar-sweetened beverage threshold based on their definition of no more than 36 ounces per week, assuming that one serving is 12 ounces.
Measures for total cholesterol, blood pressure, and glucose are designed to be as close to AHA guidelines as possible given our available information. For example, Add Health does not provide absolute concentrations for cholesterol given the assay method (Whitsel et al. 2013).
We tested for threshold values and squared terms to determine non-linear relationships between population density and ideal cardiovascular health, but the logged term produced the best fitting models.
We tested for interactions between residential location and gender, but none were significant.
BMI based on self-reported height and weight is correlated with measured BMI (in adolescence at Wave II) at over .99.
Our rates for BMI and blood sugar are similar to overall percentages of U.S. adults reported by Lloyd-Jones and colleagues (2010). Our measures of physical activity and total cholesterol reflect greater (or healthier) percentages, likely due to variable construction. The percentage of individuals consuming a healthy amount of sugar-sweetened beverages is much higher than the 0.5% of U.S. adults who meet the AHA healthy diet criterion. Rates of nonsmoking and healthy blood pressure are lower for our sample compared to U.S. adults, which may reflect the unique environment and behaviors of the young adult cohort.
The association between the population density of the tract within which individuals live and cardiovascular health appears to be largely driven by those within metropolitan core areas. The association between population density and cardiovascular health is nearly identical in a full model that includes all covariates but constrains the sample to those in metropolitan core areas, but the effect of population density is smaller and nonsignificant for the same model among those not living in metropolitan core areas.
Using number of ideal cardiovascular health indicators instead of a yes/no distinction produced no substantive differences in the results.
References
- Agency for Healthcare Research and Quality, US Department of Health and Human Services. [accessed 8 September 2016];National healthcare disparities report. 2014 Available from http://www.ahrq.gov/research/findings.
- Agunwamba Amenah A, Kawachi Ichiro, Williams David R, Finney Rutten Lila J, Wilson Patrick M, Viswanath Kasisomayajula. Mental health, racial discrimination, and tobacco use differences across rural-urban California. The Journal of Rural Health. 2016 doi: 10.1111/jrh.12182. Online first. [DOI] [PubMed] [Google Scholar]
- Anderson Timothy J, Saman Daniel M, Lipsky Martin S, Nawal Lutfiyya M. A cross-sectional study on health differences between rural and non-rural US counties using the County Health Rankings. BMC Health Services Research. 2015;15:441–449. doi: 10.1186/s12913-015-1053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Befort Christie A, Nazir Niaman, Perri Michael G. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008) The Journal of Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry Tanya R, Spence John C, Blanchard Chris M, Cutumisu Nicoleta, Edwards Joy, Selfridge Genevieve. A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. International Journal of Behavioral Nutrition and Physical Activity. 2010;7(1):57–68. doi: 10.1186/1479-5868-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewis Alexandra, Trainer Sarah, Han SeungYong, Wutich Amber. Publically misfitting: Extreme weight and the everyday production and reinforcement of felt stigma. Medical Anthropology Quarterly. 2016 doi: 10.1111/maq.12309. Online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton Linda M, Lichter Daniel T, Baker Regina S, Eason John M. Inequality, family processes, and health in the “new” rural America. American Behavioral Scientist. 2013;57(8):1128–1151. [Google Scholar]
- Caldwell Julia T, Ford Chandra L, Wallace Steven P, Wang May C, Takahashi Lois M. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. American Journal of Public Health. 2016;106(8):1463–1469. doi: 10.2105/AJPH.2016.303212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossman Jeralynn S, James Wesley L, Cosby Arthur G, Cossman Ronald E. Underlying causes of the emerging nonmetropolitan mortality penalty. American Journal of Public Health. 2010;100(8):1417–1419. doi: 10.2105/AJPH.2009.174185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins Steven, Curtis Sarah, Diez-Roux Ana V, Macintyre Sally. Understanding and representing ‘place’ in health research: a relational approach. Social Science & Medicine. 2007;65(9):1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- Dong Chuanhui, Rundek Tatjana, Wright Clinton B, Anwar Zane, Elkind Mitchell SV, Sacco Ralph L. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks and hispanics: the northern Manhattan Study. Circulation. 2012;125(24):2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhardt Mark S, Pamuk Elsie R. The importance of place of residence: examining health in rural and nonrural areas. American Journal of Public Health. 2004;94(10):1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entzel Pamela, Whitsel Eric A, Richardson Andrea, Tabor Joyce, Hallquist Suzanne, Husey Jon, Halpern Carolyn T, Harris Kathleen Mullan. [accessed 21 November 2016];Add Health Wave IV documentation: Cardiovascular and anthropometric measures. 2009 Available from http://www.cpc.unc.edu/projects/addhealth/documentation.
- Ewing Reid, Meakins Gail, Hamidi Shima, Nelson Arthur C. Relationship between urban sprawl and physical activity, obesity, and morbidity–Update and refinement. Health & Place. 2014;26:118–126. doi: 10.1016/j.healthplace.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Fontanella Cynthia A, Hiance-Steelesmith Danielle L, Phillips Gary S, Bridge Jeffrey A, Lester Natalie, Sweeney Helen Anne, Campo John V. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatrics. 2015;169(5):466–473. doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford Earl S, Greenlund Kurt J, Hong Yuling. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125(8):987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank Lawrence D, Schmid Thomas L, Sallis James F, Chapman James, Saelens Brian E. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. American Journal of Preventive Medicine. 2005;28(2):117–125. doi: 10.1016/j.amepre.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Fry Richard. A rising share of young adults live in their parents’ home. Washington, D.C: Pew Research Centers Social and Demographic Trends; 2013. [accessed 21 November 2016]. Available from www.pewsocialtrends.org. [Google Scholar]
- Galea Sandro, Vlahov David. Urban health: evidence, challenges, and directions. Annual Review of Public Health. 2005;26:341–365. doi: 10.1146/annurev.publhealth.26.021304.144708. [DOI] [PubMed] [Google Scholar]
- Glasgow Nina, Morton Lois Wright, Johnson Nan E., editors. Critical issues in rural health. Ames, Iowa: Blackwell Publishing; 2004. [Google Scholar]
- Harris Kathleen Mullan. An integrative approach to health. Demography. 2010;47(1):1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley David. Rural health disparities, population health, and rural culture. American Journal of Public Health. 2004;94(10):1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer Robert A, Melvin Jennifer E, He Monica. Immigration, health, and mortality. In: Wright James D., editor. International encyclopedia of social and behavioral sciences. 2. Vol. 11. Oxford: Elsevier Press; 2015. pp. 654–661. [Google Scholar]
- Hummer Robert A, Pacewicz Jan, Wang Shu-Chuan, Collins Chiquita. Health insurance coverage in nonmetropolitan America. In: Glasgow Nina, Morton Lois Wright, Johnson Nan E., editors. Critical issues in rural health. Ames, Iowa: Blackwell Publishing; 2004. pp. 197–210. [Google Scholar]
- Hussey Jon M, Nguyen Quynh C, Whitsel Eric A, Richardson Liana J, Halpern Carolyn Tucker, Gordon-Larsen Penny, Tabor Joyce W, Entzel Pamela P, Harris Kathleen Mullan. Characteristics and reliability of in-home anthropometry: The National Longitudinal Study of Adolescent to Adult Health, Wave IV. Demographic Research. 2015;32(39):1081–1098. doi: 10.4054/DemRes.2015.32.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson Kenneth T. A nation of cities: The federal government and the shape of the American metropolis. The ANNALS of the American Academy of Political and Social Science. 2009;626(1):11–20. [Google Scholar]
- James Peter, Troped Philip J, Hart Jaime E, Joshu Corinne E, Colditz Graham A, Brownson Ross C, Ewing Reid, Laden Francine. Urban sprawl, physical activity, and body mass index: nurses’ health study and nurses’ health study II. American Journal of Public Health. 2013;103(2):369–375. doi: 10.2105/AJPH.2011.300449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James Wesley L. All rural places are not created equal: revisiting the rural mortality penalty in the United States. American Journal of Public Health. 2014;104(11):2122–2129. doi: 10.2105/AJPH.2014.301989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Hedwig, Lee Dohoon, Guo Guang, Harris Kathleen Mullan. Trends in body mass index in adolescence and young adulthood in the United States: 1959–2002. Journal of Adolescent Health. 2011;49(6):601–608. doi: 10.1016/j.jadohealth.2011.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichter Daniel T, Brown David L. Rural America in an urban society: Changing spatial and social boundaries. Annual Review of Sociology. 2011;37:565–592. [Google Scholar]
- Lloyd-Jones Donald M, Hong Yuling, Labarthe Darwin, Mozaffarian Dariush, Appel Lawrence J, Van Horn Linda, Greenlund Kurt, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Monnat Shannon M, Pickett Camille Beeler. Rural/urban differences in self-rated health: Examining the roles of county size and metropolitan adjacency. Health & Place. 2011;17(1):311–319. doi: 10.1016/j.healthplace.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Morrill Richard, Cromartie John, Hart Gary. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geography. 1999;20(8):727–748. [Google Scholar]
- Morton Lois Wright. Spatial patterns of rural mortality. In: Glasgow Nina, Morton Lois Wright, Johnson Nan E., editors. Critical issues in rural health. Ames, Iowa: Blackwell Publishing; 2004. pp. 37–45. [Google Scholar]
- Pampel Fred C, Krueger Patrick M, Denney Justin T. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst Janice C, Bellinger Jessica D, Walsemann Katrina M, Hardin James, Glover Saundra H. Higher risk of death in rural blacks and whites than urbanites is related to lower incomes, education, and health coverage. Health Affairs. 2011;30(10):1872–1879. doi: 10.1377/hlthaff.2011.0668. [DOI] [PubMed] [Google Scholar]
- Purnell Tanjala S, Calhoun Elizabeth A, Golden Sherita H, Halladay Jacqueline R, Krok-Schoen Jessica L, Appelhans Bradley M, Cooper Lisa A. Achieving health equity: Closing the gaps in health care disparities, interventions, and research. Health Affairs. 2016;35(8):1410–1415. doi: 10.1377/hlthaff.2016.0158. [DOI] [PubMed] [Google Scholar]
- Rhew Isaac C, David Hawkins J, Oesterle Sabrina. Drug use and risk among youth in different rural contexts. Health & Place. 2011;17(3):775–783. doi: 10.1016/j.healthplace.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts Megan E, Doogan Nathan J, Kurti Allison N, Redner Ryan, Gaalema Diann E, Stanton Cassandra A, White Thomas J, Higgins Stephen T. Rural tobacco use across the United States: How rural and urban areas differ, broken down by census regions and divisions. Health & Place. 2016;39:153–159. doi: 10.1016/j.healthplace.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens Brian E, Sallis James F, Frank Lawrence D. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. Annals of Behavioral Medicine. 2003;25(2):80–91. doi: 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- Singh Gopal K, Siahpush Mohammad. Widening rural–urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health. 2014;91(2):272–292. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparks P Johnelle. Rural health disparities. In: Kulcsár László J, Curtis Katherine J., editors. International handbook of rural demography. Springer; Netherlands: 2012. pp. 255–271. [Google Scholar]
- Thoits Peggy A. Stress and health major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 Supplement):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture (USDA) Economic Research service. [accessed 7 September 2016];Rural-urban commuting area codes. 2016 Available from http://www.ers.usda.gov/data-products.
- Whitsel Eric, Tabor Joyce W, Nguyen Quynh C, Cuthbertson Carmen C, Wener Mark H, Potter Alan J, Killeya-Jones Ley A, Harris Kathleen Mullan. [accessed 21 November 2016];Add Health Wave IV documentation: Measures of glucose homeostasis. 2012 Available from http://www.cpc.unc.edu/projects/addhealth/documentation.
- Whitsel Eric A, Cuthbertson Carmen C, Tabor Joyce W, Potter Alan J, Wener Mark H, Clapshaw Patric A, Killeya-Jones Ley A, Halpern Carolyn T, Harris Kathleen Mullan. [accessed 21 November 2016];Add Health Wave IV documentation: Lipids. 2013 Available from http://www.cpc.unc.edu/projects/addhealth/documentation.
- Yang Quanhe, Cogswell Mary E, Dana Flanders W, Hong Yuling, Zhang Zefeng, Loustalot Fleetwood, Gillespie Cathleen, Merritt Robert, Hu Frank B. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. Journal of the American Medical Association. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Yang Claire, Boen Courtney, Gerken Karen, Li Ting, Schorpp Kristen, Harris Kathleen Mullan. Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences. 2016;113(3):578–583. doi: 10.1073/pnas.1511085112. [DOI] [PMC free article] [PubMed] [Google Scholar]