Abstract
Background
Dengue and chikungunya are global re-emerging mosquito-borne diseases. In Singapore, sustained vector control coupled with household improvements reduced domestic mosquito populations for the past 45 years, particularly the primary vector Aedes aegypti. However, while disease incidence was low for the first 30 years following vector control implementation, outbreaks have re-emerged in the past 15 years. Epidemiological observations point to the importance of peridomestic infection in areas not targeted by control programs. We investigated the role of vectors in peri-domestic areas.
Methods
We carried out entomological surveys to identify the Aedes species present in vegetated sites in highly populated areas and determine whether mosquitoes were present in open-air areas frequented by people. We compared vector competence of Aedes albopictus and Aedes malayensis with Ae. aegypti after oral infection with sympatric dengue serotype 2 and chikungunya viruses. Mosquito saliva was tested for the presence of infectious virus particles as a surrogate for transmission following oral infection.
Results
We identified Aedes albopictus and Aedes malayensis throughout Singapore and quantified their presence in forested and opened grassy areas. Both Ae. albopictus and Ae. malayensis can occupy sylvatic niches and were highly susceptible to both arboviruses. A majority of saliva of infected Ae. malayensis contained infectious particles for both viruses.
Conclusions
Our study reveals the prevalence of competent vectors in peri-domestic areas, including Ae. malayensis for which we established the vector status. Epidemics can be driven by infection foci, which are epidemiologically enhanced in the context of low herd immunity, selective pressure on arbovirus transmission and the presence of infectious asymptomatic persons, all these conditions being present in Singapore. Learning from Singapore’s vector control success that reduced domestic vector populations, but has not sustainably reduced arboviral incidence, we suggest including peri-domestic vectors in the scope of vector management.
Author summary
Dengue and chikungunya are mosquito-borne diseases and re-emerging as a global burden of the 21st century. Because of the absence of cure and limitations of the current vaccine, vector control remains the sole efficient intervention to mitigate epidemics. The highly-populated city of Singapore represents an example of successful vector control, where the primary vector Aedes aegypti has practically disappeared from households. However, there as well, dengue and chikungunya are re-emerging. In this study, we surveyed peridomestic sites for mosquito vectors and identified Aedes albopictus and Aedes malayensis throughout Singapore and in open-air areas frequented by people. We further showed that both mosquito species are highly susceptible to dengue and chikungunya viruses and detected infectious virus particles in mosquito saliva, indicating their transmission capacity. Our study provides evidence that Ae. albopictus and Ae. malayensis possess all the traits necessary to contribute to virus transmission in cities and suggest that peridomestic areas be included in vector management programme.
Introduction
Globally, dengue virus (DENV) is the most commonly transmitted arbovirus and infects an estimated 390 million people per year with greater than half the world’s population at risk of infection [1]. Chikungunya virus (CHIKV) periodically emerges to cause epidemics in populated areas and is maintained in sylvatic cycles [2, 3]. In domestic settings, both viruses are primarily transmitted by Aedes aegypti [4, 5]. Its prolific adaptation to urban environment, its near-exclusive anthropophilic blood-feeding behaviour, and its proclivity to take multiple blood meals during a single gonotrophic cycle make it the ideal domestic vector [6]. Aedes albopictus belongs to the same subgenus (Stegomyia) and is considered a secondary vector of DENV and CHIKV [2], primarily because of its catholic feeding habits and peridomestic (defined here as city parks and green corridors interspersing housing estates) biology. Aedes albopictus mosquitoes will utilize oviposition sites distant from human habitats [5], but prefer humans as hosts even when other vertebrates are available [7]. This species is a biting nuisance [8, 9] and will enter houses and feed indoors [10, 11]. Both mosquito species are globally distributed and their ranges are expanding [12], facilitating the increasing spread of DENV and CHIKV. With a partially efficacious vaccine against dengue [13, 14] and an absence of curative treatment for both diseases, vector control remains the sole intervention to mitigate these epidemics. However, re-emergence and recent global intensification in the frequency and scale of dengue and chikungunya outbreaks, especially in large cities, [1, 15, 16] have raised concerns about the sustainability of the current approach targeting domestic vectors [1, 16, 17].
In Singapore, dengue outbreaks first appeared in 1960 and rapidly became a major cause of childhood mortality [18]. The subsequent government implementation of a comprehensive and permanent integrated mosquito management program drastically decreased the Aedes house index (the percentage of houses with Aedes mosquitoes) and succeeded in maintaining a low disease incidence until the early 1990s [19]. Today, the vector control programme systematically applies WHO recommendations [5, 20] and includes surveillance, source reduction, reactive adulticiding, insecticide resistance monitoring, public health education, community participation, fines for allowing mosquito breeding, and georeferenced entomologic and clinical surveillance for an annual cost of US$50 million [21].Together with the wide availability of technical amenities like air-conditioning, window screens, better sanitation [22, 23] and piped water supplies [24] that reduce oviposition sites, the extensive vector control program maintains a very low Aedes house index [19]. Yet, dengue epidemics have increased in frequency and intensity for the past 15 years [25, 26], and chikungunya and Zika virus emerged in 2008 and 2016, respectively [27, 28].
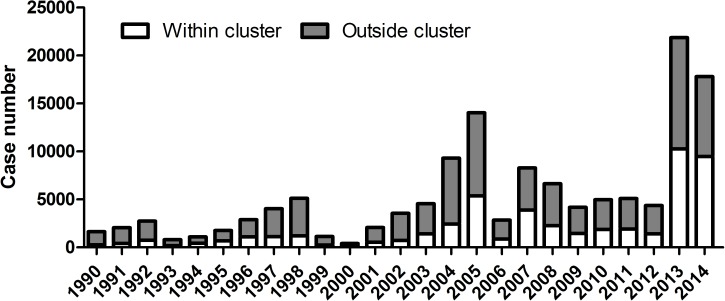
While lowered herd immunity resulting from 30 years of low dengue incidence increased the force of infection [18, 19], there remains an apparent paradox between the very low Aedes house index and the resurgence of dengue and chikungunya in Singapore. To resolve this paradox, we hypothesize that foci of infection exist in peridomestic areas. Several epidemiological observations indicate that non-domestic infections are frequent in Singapore: (i) symptomatic cases are more prevalent in adults than in young children [27, 29], suggesting that the principal site of infection is not in homes where children spend most of their time, (ii) dengue incidence markedly increases for children at the age they start school and thus spend more time outside their home [29], (iii) women, who are more likely to stay home caring for children, have a lower incidence of infection than men [29], and (iv) a majority of infected patients do not live in areas of case-clusters (defined as two or more cases living within 150m from each other and occurring within 14 days), suggesting a similar proportion of infections do not occur in domestic clusters (Fig 1) [30].
Fig 1. Distribution of cases identified within and outside case-clusters from 1990 to 2014.
A case-cluster is defined as two or more infected persons epidemiologically linked by place [within 150m (200m till 2002)] with respect to their home address and time (within 14 days). Numbers above bars represent percentage of cases outside clusters [30].
The structure of Singapore is a matrix of highly populated areas with parks and bosquets, resulting in a vegetation cover of 44% [31]. Forested areas such as parks are frequented weekly by at least 35% of the population [32] and possess all social and environmental characteristics identified in foci of infection [33], i.e. routine attendance, artificial or natural containers, open spaces for daily activities, and the lack of air-conditioning. To determine the potential risk of infection in these sites, we combine country-wide entomological surveys and vector competence studies to determine the distribution and prevalence of competent vectors.
Materials and methods
Sampling surveys
Between 2013 and 2015, oviposition traps filled with distilled water containing a crushed wafer of fish food (TetraMin fish flakes) and a piece of seed germination paper (Anchor Paper) were placed at 12 forested sites throughout Singapore (West Coast Park, Clementi Woods Park, Mount Faber Park, Bukit Batok Town Park, East Coast Park (x 3 sites), Sentosa, Pulau Semkau, Kent Ridge Park, Whampoa along the Kalong River, and Bukit Timah Nature Reserve). Oviposition papers were replaced every 3–4 days. Upon collection, oviposition papers were treated with a 10-fold commercial bleach dilution to surface sterilize them and prevent microbial growth and introduction of field parasites into laboratory colonies. Egg papers were exposed for 10 minutes to this solution before rinsing and drying and kept between 2–4 weeks before hatching. Eggs were hatched in deoxygenated water, larvae were fed a mix of fish food (TetraMin fish flakes) and liver powder (MP Biomedicals), and adults were provided a 10% sucrose solution. The insectary was held at 28°C with 50% humidity on a 12:12h dark:light cycle. Adult mosquitoes were killed by freezing and identified using taxonomic keys to distinguish Ae. albopictus, Ae. aegypti and Ae. malayensis [34] (S1 Fig). All collections were undertaken with permission of the National Parks Board, Singapore (Permit NP/RP11-012-2).
Presence in open-air areas
We conducted a transect study of oviposition preference at two separate sites (transect A and B) in East Coast Park (southern part of Singapore). Both sites were chosen based on the presence of adjacent forested and open(no tree cover)-air patches. In each site, we placed oviposition traps (as above) every 15m along each transect that traversed both forested and open-air patches; three traps in the forested area, and three others in the open area. Oviposition collection was undertaken as described above from 25 July to 23 September 2014 every 3–4 days for a total of 16 and 18 collection dates for transect A and B, respectively. Eggs were counted visually with an Olympus SZ-61 stereoscope and were reared to adults as described above for identification.
Colony establishment and mosquito rearing
The Ae. malayensis colony was established in 2014 from eggs collected using oviposition traps in 2 different forested areas located in the Northern (Sembawang) and the Southern (East Coast Park) regions of Singapore (National Environment Agency Permit NEA/PH/EHD/13-00011). The Ae. aegypti and Ae. albopictus colonies were established in 2010 from eggs collected using oviposition traps from a single neighborhood (Ang Mo Kio-central area) in Singapore. Eggs were reared as described above and 500 morphologically identified adults [34] (S1 Fig) were used to start each colony. Adult mosquitoes were held in rearing cages (Bioquip) supplemented with 10% sucrose and fed pig’s blood (Primary Industries Pte Ltd) twice weekly. To maintain field genetic diversity, the Ae. aegypti and Ae. albopictus colonies were replenished every month from 2010–2014 with 40 to 100 adults obtained from the same site, while all Ae. malayensis used in the infection experiments were F3 and F4 generations.
Virus isolates and propagation
We used the clinical isolates dengue ST (passage 6) [35] and Chikungunya EAS DMERI09/08 (passage 3) viruses, collected from the Singapore General Hospital in 1997 and National University Hospital, Singapore in 2008, respectively (already existing collection). A portion of the E1 gene from CHIKV EAS was amplified and sequenced to validate the absence of the A226V amino acid substitution [9]. All viruses were propagated in Vero cells (ATCC) and titrated by plaque assay in BHK cells (ATCC) as previously described [36].
Oral infection and dissemination study
Three to five day-old Ae. aegypti, Ae. albopictus or Ae. malayensis females were sugar-deprived for 24 h and subsequently offered a blood meal containing a 40% volume of washed erythrocytes from SPF pig’s blood (PWG Genetics), 5% of 100 mM ATP (Thermo Scientific), 5% human serum (Sigma) and 50% volume of a DENV ST or CHIKV EAS virus in RPMI (Gibco). The final concentration of virus in the blood mix was 1x107 pfu/ml and was validated by plaque assay [36]. Mosquitoes were exposed to the artificial blood meal for one hour using a Hemotek membrane feeder system (Discovery Workshops) with a porcine intestine membrane. Fully engorged females were selected and provided access to a 10% sugar solution in an incubation chamber with conditions similar for insect rearing. At fourteen days after the blood meal, 25 mosquitoes were dissected into head/thorax and abdomen halves; this resulted in two halves for each mosquito. Each tissue portion was triturated in 500 μl of maintenance medium as described above and the virus load quantified by RT-qPCR. Three oral infection replicates were performed for each virus-mosquito species combination.
Saliva collection
Five three to five day-old Ae. malayensis females were orally infected with 1x107 pfu/ml of DENV and 1x106 pfu/ml of CHIKV as described above and held for 14 days. The probosces of six infected Ae. malayensis were each inserted into a 10 μl pipette tip containing 6 μl of a 1:1 solution of 15% sucrose and heat-inactivated FCS. The mosquitoes were allowed to expectorate for 30 minutes, after which they were triturated as in the oral infection experiment and quantified for the virus load by RT-qPCR. 0.2 μl of the saliva-containing solution was inoculated intrathoracically into five uninfected Ae. aegypti female mosquitoes aged 3–5 days old using NanoJect II injector (Drummond). Seven days after saliva inoculation, each mosquito was triturated in 500μl of maintenance medium as described above and their virus load was quantified using RT-qPCR.
Quantification of dengue and chikungunya virus load
Triturated mosquitoes or tissues were centrifuged and 400 μl of supernatant was used to extract viral RNA (QIAamp Viral RNA Mini Kit, Qiagen). DENV or CHIKV genome copies were quantified using a one-step RT-qPCR with iTaq Universal probe kit (BioRad) and primers and probes targeting the envelope (DENV) [37] and nsP1 (CHIKV) genes [38]. The 25 μl reaction mix contained 1 μM of forward and reverse primer, 0.125 μM of probe and 4 μl of RNA extract. Thermal profile started at 50°C for 10 min, 95°C for 1 min and 40 cycles of 95°C for 10 sec and 60°C for 15 sec.
An absolute standard curve was generated by amplifying fragments containing the qPCR targets (one fragment for each virus) using forward primers tagged with a T7 promoter; for DENV we used 5'-TAATACGACTCACTATAGGGCAGGATAAGAGGTTCGTCTG-3' and 5'-TTGACTCTTGTTTATCCGCT-3'; for CHIKV we used 5'-TAATACGACTCACTATAGGGTAGAGCGTTGACCCTACTGA-3' and 5'-AAGGATGCCGGTCATTTGAT-3'. The fragments were reverse transcribed using a MegaScript T7 transcription kit (Ambion) and the total amount of RNA was quantified using a Nanodrop (ThermoScientific) to estimate copy number.
Screening of field-collected mosquitoes for viruses
Mosquitoes were collected weekly from June-August, 2013 in Sembawang using CDC traps (Bioquip), BG Sentinel Traps (Biogents), and Mosquito Magnet Mosquito trapper (Mosquito Magnet) that were baited with dry ice. Samples were held at 4°C before being brought to Duke-NUS for identification on a chill table. Mosquitoes were pooled by species and collection week. Aedes albopictus and Ae. malayensis pools were homogenized in 500 μl of maintenance medium as described above. RNA was extracted with a QIAamp Viral RNA Mini Kit (Qiagen), cDNA was generated with Superscript II according to manufacturer’s instructions and screened for flaviviruses with previously described primers (FU1 and cFD3) and protocol [39]. Chikungunya was screened for with a previously described pan-alphavirus RT-PCR [40]. Positive and negative controls were used in each reaction.
Statistical analysis
We conducted three-way mixed-effect ANCOVA to test the impact of transect site, distance along the transect from the forest edge, and collection date (random variable) on the number of Ae. albopictus and Ae. malayensis. Where appropriate, we employed linear regression to study the impact of distance for each individual transect. A one-way ANOVA was used to determine the effect of mosquito species on infection and dissemination rates. We estimated the influence of mosquito species and tissue (abdomen or thorax) on viral genome copy by conducting a two-way ANOVA with tissue nested into species. Tissue was nested into species to estimate variation between tissues within the same species. Viral genome copies were log-transformed to fit a normal distribution. Post-hoc analysis were conducted using Tukey's test. All tests were calculated using Systat 13.0 software (SYSTAT).
Results
Aedes albopictus and Aedes malayensis are present in forested and open areas of city parks
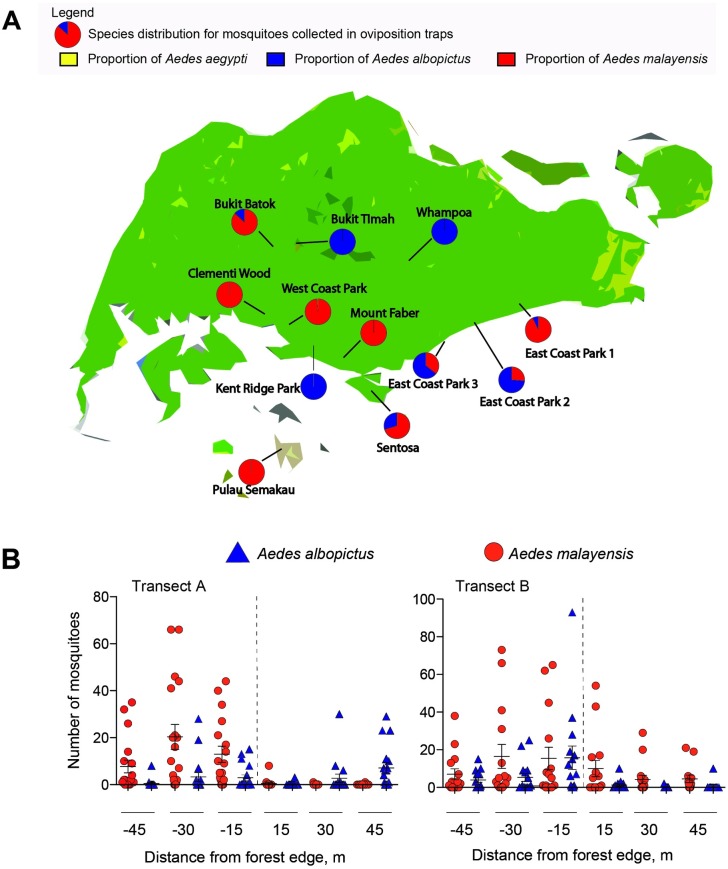
To identify sylvatic vectors, we sampled for container-inhabiting Aedes mosquitoes in the forested urban parks of Singapore, located in population-dense areas, primarily comprised of high-rise apartments. From the oviposition traps set in 12 forested areas and collected from 2013 to 2015, Ae. albopictus and Ae. malayensis comprised almost the entire collection from the oviposition traps set in 12 forested areas with only two Ae. aegypti were identified (S1 Table). Aedes malayensis was the only species detected at three sites, while Ae. albopictus was the only container-inhabiting species detected in three other sites (Fig 2A). Both species were detected in six sites, and more Ae. malayensis eggs were collected in four of these sites (S1 Table).
Fig 2. Distribution of Aedes albopictus and Aedes malayensis in urban parks of Singapore.
(A) Proportion of Ae. malayensis, Ae. albopictus and Ae. aegypti reared from eggs collected in oviposition traps distributed in 12 urban parks. (B) Distribution of Ae. malayensis and Ae. albopictus reared from eggs collected in oviposition traps distributed across transects that spanned forested to open-air habitat at two sites in East Coast Park Singapore.
We then determined whether Ae. malayensis and Ae. albopictus could be detected in open-air grassy sites of city parks. We collected mosquito eggs from oviposition traps set along two transects from within a forest patch to a grassy open-air area in the most visited park in Singapore [32], East Coast Park. Over the two month period, 8,581 eggs were collected, from which 25.84% were reared to adults, resulting in 1,502 Ae. malayensis and 716 Ae. albopictus (S2 Table). Eggs from both species were oviposited in the forested and open areas (Fig 2B), but the effect of distance from the forest edge varied between the two transects for each species (S3 Table). There were more Ae. malayensis in the forested area of transect A, while there was no difference for transect B (linear regression; transect A: df = 1, 86; p = 0.037; transect B: df = 1, 105; p = 0.066). Aedes albopictus distribution was different as mosquitoes were more abundant in the forested area of transect B, but no difference was witnessed between open and forested areas in transect A (transect A: df = 1, 72; p = 0.203; transect B: df = 1, 88; p < 0.001). Together, these results demonstrate that Ae. albopictus and Ae. malayensis are present in areas of city parks frequented by humans.
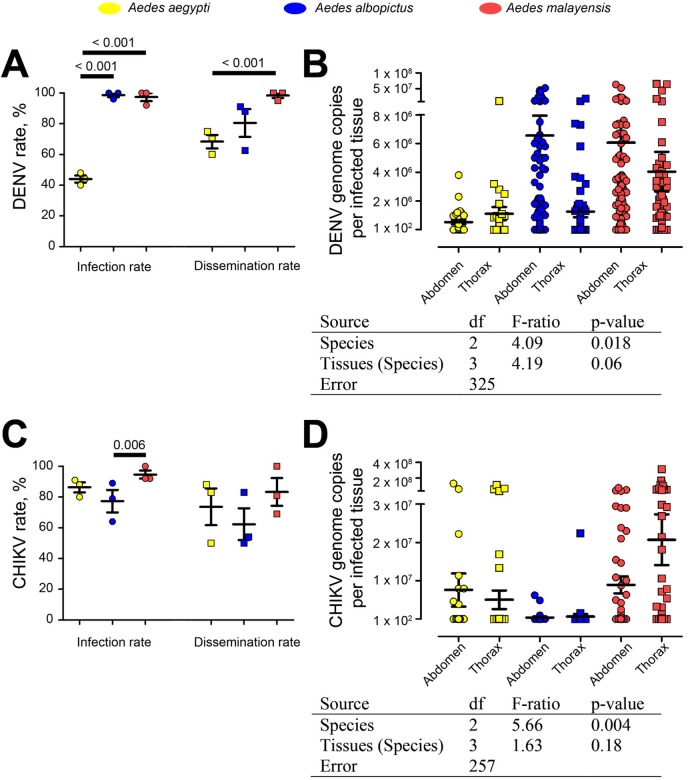
Aedes albopictus and Ae. malayensis from Singapore are highly competent vectors for sympatric DENV-2 and CHIKV
To determine the vector competence of Ae. albopictus and Ae. malayensis, we orally infected the two species with sympatric isolates of DENV serotype 2 and CHIKV. Orally challenged Ae. aegypti were used as controls. At 14 days post-infection, mosquitoes were separated in two halves corresponding to the abdomen and head/thorax, and the virus was quantified in each section. Detection of virus in the thorax was indicative of dissemination from the midgut to the salivary glands, which are present in the thoracic compartment and represent the source organ for transmission via saliva during biting. DENV infection rates were the highest in Ae. albopictus and Ae. malayensis, reaching 100% in two of the three biological repeats, while Ae. aegypti infection rate was significantly lower than both species with an average of 44% (Fig 3A). Total viral genome copies from both body parts was lower in Ae. aegypti than in the two other species (Fig 3B; S4A Table). Dissemination rates in Ae. malayensis reached 100% in two repeats and was significantly higher than in Ae. aegypti and higher than in Ae. albopictus (Fig 3A). Viral genome copies per tissue was significantly higher in thoraxes of Ae. albopictus and Ae. malayensis than for Ae. aegypti (Fig 3B).CHIKV infection rates were significantly higher in Ae. malayensis than in Ae. albopictus and higher than in Ae. aegypti, although average infection was above 75% for all three species (Fig 3C). While not significant, average dissemination rate and total viral genome copies in both abdomen and thorax parts were also higher for Ae. malayensis than for the two other species (Fig 3C and 3D; S4B Table).
Fig 3. Infection and dissemination abilities for DENV and CHIKV in Ae. aegypti, Ae. albopictus and Ae. malayensis.
Mosquitoes were orally infected with the virus and analyzed after 14 days. (A) Infection and dissemination rates for DENV. (B) DENV genome copies per infected tissue in abdomen and thorax. (C) Infection and dissemination rates for CHIKV. (D) CHIKV genome copies per infected tissue in abdomen and thorax. (A and C) Each point represents an independent repeat of 25 mosquitoes. Bars show mean ± s.e.m. T-test significant differences between mosquito species are shown. (B and D). Table below indicates the results from a two-ANOVA testing the impact of species and tissues on viral genome copies per infected tissues.
To detect arboviruses in field-caught Ae. malayensis and Ae. albopictus, we collected a total of 2,432 female Ae. albopictus and 392 female Ae. malayensis from 132 traps nights. Each species was collected in each trap type (S6 Table). There were 15 Ae. malayensis and 54 Ae. albopictus pools tested for flaviviruses and alphaviruses. All pools were negative for both virus families (S7 Table).
To confirm Ae. malayensis transmission capacity, we quantified viral genome copies in Ae. aegypti injected with saliva from orally infected Ae. malayensis. DENV-infected saliva was infectious to a majority of mosquitoes (Table 1; S5A Table). While one saliva extract did not lead to infection, the four other extracts contained enough infectious particles to infect at least 40% of the saliva-inoculated mosquitoes. All CHIKV-infected saliva contained enough virus to infect mosquitoes (Table 1; S5B Table). Two saliva extracts showed high infectivity as they led to CHIKV infection in all the five saliva-inoculated mosquitoes. Inoculation of the other saliva extracts infected between 40 and 80% of the mosquitoes.
Table 1. Infection rate and viral genome copies per infected Ae. malayensis 14 days after injection of saliva collected from DENV- or CHIKV-infected Ae. malayensis.
nd; not detected.
| DENV | CHIKV | |||||
|---|---|---|---|---|---|---|
| Genome copies per mosquito | Infection rate (n / N) |
Genome copies per mosquito | Infection rate (n / N) |
|||
| Repeat | Saliva-collected mosquitoes | Saliva-injected mosquitoes | Saliva-collected mosquitoes | Saliva-injected mosquitoes | ||
| 1 | 4.4 x 106 | 2.4 x 104 | 3 / 5 | 1.3 x 108 | 1.4 x 108 | 5 / 5 |
| 2 | 1.8 x 107 | 1.1 x 103 | 3 / 5 | 1.2 x 108 | 3.1 x 108 | 2 / 5 |
| 3 | 4.5 x 106 | 1.6 x 107 | 5 / 5 | 1.8 x 108 | 8.5 x 102 | 2 / 5 |
| 4 | 9.1 x 106 | 1.0 x 105 | 3 / 5 | 5.2 x 107 | 7.4 x 107 | 4 / 5 |
| 5 | 6.6 x 106 | nd | 0 / 5 | 1.4 x 108 | 1.1 x 108 | 5 / 5 |
| Average | 4.0 x 106 | 14 / 25 | 1.3 x 108 | 18 / 25 | ||
Discussion
Here, we addressed the question of whether outdoor peridomestic mosquito species can participate in the epidemiology of dengue and chikungunya in a highly populated and developed city such as Singapore. Our study revealed the high prevalence of Ae. albopictus and Ae. malayensis in open-air spaces of forested areas, their distribution across Singapore and their high vector competence for DENV and CHIKV.
Confronted with a global rise in the incidence of dengue and chikungunya cases in cities [41], public health authorities need to question the dogma of current vector control approaches that focus on domestic Aedes populations. Changes in world demography and epidemiology has altered the vector control framework [15, 41]. Increase in population density and in global transportation augmented mosquito-human interactions and arbovirus introduction frequency. Interestingly, fine-scale correlation between a reduced Aedes house index and lower dengue burden has seldom been observed [42, 43]. Instead, risk of infection is independent of distance from home and determined by human movement into arboviral foci of infection [44, 45]. High risk transmission areas often have narrow spatial-temporal windows [46, 47], likely because mosquitoes are short-lived (less than 3 weeks) and rarely disperse further than 100m [48, 49]. Identification of sites, for example schools, temples or open-air places [33, 50], and pro-active interventions will enhance the efficacy of vector control. In this transmission context, our findings indicate that peridomestic areas may present a risk for infection.
A combination of biological features determines the vector status of mosquito species, two of which are especially important [51]. The first is their susceptibility to infection, enabling replication of the virus to high titers throughout the mosquito body and particularly in the salivary glands, thus facilitating transmission during subsequent blood feeding [52]. Importantly, vector competence can be affected by intra-species mosquito diversity and virus origin [53, 54]. We therefore conducted a vector competence study with sympatric mosquitoes and viruses. A second important characteristic responsible for the vector status is the proclivity to bite humans, which depends on its anthropophily and presence in human populated areas, such as open-air parks where we identified the two sylvatic species for which we characterized vector competence.
Aedes albopictus is known to be susceptible to DENV and CHIKV infection [51, 55, 56], and in some instances, was found to be more competent than Ae. aegypti [57, 58], as this was the case in our study. Our results demonstrated a higher DENV infection rate for Ae. albopictus than for Ae. aegypti. Of note, the relatively low infection rates for Ae. aegypti were comparable to previous experiments [58]. The global chikungunya outbreak initiated in 2004 was caused by enhanced transmission efficiency by Ae. albopictus following a mutation in the E1 protein of the virus [9, 59], although cross genetic interactions between mosquito and virus strains can affect transmission [60]. Despite the mutation absence from our local isolate, infection and dissemination rates in Ae. albopictus were not significantly different to the ones in Ae. aegypti, indicating Ae. albopictus from Singapore is likely capable of transmitting both CHIKV strains, similarly to Ae. aegypti [61]. Both CHIKV strains are now globally distributed and could be introduced to Singapore [62], thereby increasing the risk of transmission by Ae. albopictus. Moreover, Ae. albopictus has been shown to prefer to bite humans even in the presence of other vertebrates [7]. Aedes albopictus was incriminated as the primary vector in epidemics of dengue and chikungunya in central Africa [63], China [64] and Mediterranean Europe [65, 66]. Interestingly, an epidemiological study in a Japanese city showed that more than 80% of dengue patients during an epidemic visited a city park where Ae. albopictus is present [67].
Aedes malayensis (Colless 1962) is a relatively understudied species with a wide distribution in Southeast Asia [68]. Its presence has been recorded in Taiwan, Vietnam, Cambodia, Peninsular Malaysia, the Andaman and Nicobar Islands of India and across several regions in Thailand [34, 69, 70]. In our study, differences in Ae. malayensis prevalence between sampling sites may reflect variable microhabitat characteristics [71]. Sites with a majority of Ae. malayensis were mainly young secondary forests, whereas sites devoid of Ae. malayensis were a mixture of primary and secondary forests. Aedes malayensis vector competence has not been fully characterized for DENV [58] and is undocumented for CHIKV. A previous study showed the susceptibility of Ae. malayensis to all 4 DENV serotypes after oral infection [58] but did not determine the presence of virus in the saliva. Our data clearly established the high susceptibility of Ae. malayensis and validated its transmission capacity for both DENV-2 and CHIKV. Detection of virus in field-caught vectors is important evidence of potential vector capacity in natural settings. We did not detect DENV or CHIKV in our field-caught Ae. malayensis. However, virus detection in field-caught vectors is challenging. For instance, a previous study failed to detect DENV in Ae. aegypti from the Cape Verde Island where the four DENV serotypes are endemic [72]. Importantly, Ae. malayensis have been shown to bite humans [68, 69] even though they oviposit outside of domiciles [68, 69, 73, 74]. Altogether, these results establish for the first time the vector competence of Ae. malayensis for sympatric DENV-2 and CHIKV and warrants additional study to determine its role as a vector in Southeast Asia. There are a number of other Stegomyia species in Southeast Asia that may be capable of transmitting DENV and CHIKV and should be investigated as well [2, 75–78]. Such peridomestic vectors have been involved in transmitting epidemics of dengue and chikungunya [76, 79].
Our study has some limitations in incriminating Ae. malayensis and Ae. albopictus as important vectors in Singapore. Although vector biting rate can elucidate the involvement of vectors in pathogen transmission, we did not measure this parameter. The absence of prophylaxis or curative agents against these viruses does not warrant ethical clearance for human landing rate studies. Alternatively to our hypothesis that peridomestic Aedes transmission is a cause of recurrent arbovirus outbreaks in Singapore and generally in cities, frequent introductions of viruses from neighboring endemic countries may play a role [41]. Further molecular epidemiology studies are needed to determine the relative importance of virus introduction and peridomestic transmission.
Singapore represents a particular case in Southeast Asia and may illustrate the long-term frailties of the current vector control approach. We should learn from this example to support the continued monitoring of the efficacy of vector management. One of the richest countries (GDP per capita) in the world [80], Singapore is primarily comprised of high-rise buildings [81] equipped with architectural features that reduce potential larval habitats. This city-state can afford a permanent evidence-based integrated vector control programme widely regarded as a worldwide success [42]. The Aedes house index has been maintained at 1–2% for the past 45 years [18], which is well below the 4% threshold defined as an epidemic alert [82]. Yet, the low dengue and chikungunya incidence could not be sustained for more than 30 years [18, 83]. Here, we propose that the presence of highly competent vectors in city parks and forested areas may be contributing to transmission and maintenance of the viruses. Maintenance of low infection rates in few areas is enough to ensure the persistence of arboviruses in large cities and to initiate an outbreak when conditions are favorable [84]. The presence of non-human primates, such as macaques in Singapore, coupled with competent zoonotic vectors may also provide alternative reservoirs as refugia for arboviruses [85, 86]. Risk of infection in parks is increased by the low herd immunity of the Singaporean population [19, 29], the potential presence of asymptomatically infected people or those prior to clinical disease onset who are infectious to mosquitoes [87], and wearing clothes that expose skin to mosquito biting. Furthermore, the high selection pressure [88] on arbovirus transmission due to the overall low domestic vector population may select for more transmissible virus strains. Although further studies, including fine-scale tracking of patients and molecular epidemiology, are required to confirm localization of the foci of infection, our results strongly support the inclusion of peridomestic areas in the scope of vector control and surveillance programmes.
Supporting information
Morphological differences between Ae. malayensis (A) and Ae. albopictus (B). The primary differences are the suprealar scale patch extending to the scutellum in Ae. malayensis (i), the scalloped pattern of abdominal tergites (IV-VI) on Ae. malayensis (ii), and the absence of scales from the subspiracular area in Ae. malayensis (iii). Images credited to Nicky Bay.
(TIF)
(XLSX)
Total numbers of eggs collected and mosquitoes reared from Transect A and B in East Coast Park, Singapore, for the patch fidelity and oviposition experiments.
(XLSX)
(XLSX)
Viral genome copy number in abdomen and thorax of Ae. aegypti, Ae. albopictus and Ae. malayensis at 14 days post oral infection with (A) DENV or (B) CHIKV. nd: not detected.
(XLSX)
Infection rate and viral genome copy number for Ae. malayensis injected with saliva collected from DENV- (A) or CHIKV- (B) infected Ae. malayensis. nd: not detected.
(XLSX)
(XLSX)
(XLSX)
Acknowledgments
We thank HC Tan and APS Rathmore for providing dengue and chikunguna virus isolates. We are grateful to Dr. D. Fonseca at Rutgers University for assistance with sequencing and with the preliminary identifications and to Dr. P. Salgueiro at the Institute of Hygiene and Tropical Medicine in Lisbon for her advice on population genetics. We thank the National Park Board Singapore for their permission to collect in their parks. We thank the many staff that assisted in the collection of these mosquitoes. We thank A. Henry who provided the data to her thesis in Ang Mo Kio on trapping Aedes. We are grateful to Nicky Bay for sharing his time to photograph our specimens.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Support for this research came from a grant from the Singapore Infectious Disease Initiative (SIDI/2013/011) funded by the MOH awarded to IHM, the Naval Medical Research Unit-2 BPA (N40345-11-A-0017-00033) awarded to IHM, from the National Research Foundation Singapore under its NIG scheme (NMRC/BNIG/2032/2015) awarded to JP, and from the Duke-NUS Signature Research Programme funded by the Agency for Science, Technology and Research (A*STAR), Singapore, and the Ministry of Health, Singapore. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Maoyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504–7. doi: 10.1038/nature12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coffey LL, Failloux AB, Weaver SC. Chikungunya virus-vector interactions. Viruses-Basel. 2014;6(11):4628–63. doi: 10.3390/v6114628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powers AM, Logue CH. Changing patterns of chikungunya virus: re-emergence of a zoonotic arbovirus. J Gen Virol. 2007;88(Pt 9):2363–77. doi: 10.1099/vir.0.82858-0 . [DOI] [PubMed] [Google Scholar]
- 4.Gubler DJ. Dengue and Dengue Hemorrhagic Fever. Clin Microbiol Rev. 1998;11(3):480–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Comprehensive guideline for prevention and control of Dengue and Dengue haemorrhagic fever. WHO, editor2011. 196 p. [Google Scholar]
- 6.Ritchie SA. Dengue vector bionomics: Why Aedes aegypti is such a good vector. Dengue and Dengue Hemorrhagic Fever. 2014:455. [Google Scholar]
- 7.Kek R, Hapuarachchi HC, Chung C-Y, Humaidi MB, Razak MABA, Chiang S, et al. Feeding host range of Aedes albopictus (Diptera: Culicidae) demonstrates its opportunistic host-seeking behavior in rural Singapore. J Med Entomol. 2014;51(4):880–4. doi: 10.1603/me13213 [DOI] [PubMed] [Google Scholar]
- 8.Scholte E, Dijkstra E, Ruijs H, Jacobs F, Takken W, Hofhuis A, et al., editors. The Asian tiger mosquito (Aedes albopictus) in the Netherlands: should we worry? Proceedings of the Netherlands Entomological Society Meeting; 2007.
- 9.Vazeille M, Moutailler S, Coudrier D, Rousseaux C, Khun H, Huerre M, et al. Two Chikungunya isolates from the outbreak of La Reunion (Indian Ocean) exhibit different patterns of infection in the mosquito, Aedes albopictus. PLoS ONE. 2007;2(11):e1168 doi: 10.1371/journal.pone.0001168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drago A, editor Education, information and public awareness in vector control. Presentation to the 14th European Conference of the Society of Vector Ecology; 2003.
- 11.Genchi C, Rinaldi L, Mortarino M, Genchi M, Cringoli G. Climate and Dirofilaria infection in Europe. Vet Parasitol. 2009;163(4):286–92. doi: 10.1016/j.vetpar.2009.03.026 [DOI] [PubMed] [Google Scholar]
- 12.Kraemer MU, Sinka ME, Duda KA, Mylne AQ, Shearer FM, Barker CM, et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. eLife. 2015;4 doi: 10.7554/eLife.08347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson NM, Rodríguez-Barraquer I, Dorigatti I, Mier-y-Teran-Romero L, Laydon DJ, Cummings DAT. Benefits and risks of the Sanofi-Pasteur dengue vaccine: Modeling optimal deployment. Science. 2016;353(6303):1033–6. doi: 10.1126/science.aaf9590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilder-Smith A, Gubler DJ. PUBLIC HEALTH. Dengue vaccines at a crossroad. Science. 2015;350(6261):626–7. doi: 10.1126/science.aab4047 [DOI] [PubMed] [Google Scholar]
- 15.Gubler DJ. The changing epidemiology of yellow fever and dengue, 1900 to 2003: full circle? Comp Immunol Microbiol Infect Dis. 2004;27(5):319–30. doi: 10.1016/j.cimid.2004.03.013 [DOI] [PubMed] [Google Scholar]
- 16.Gubler DJ. The global emergence/resurgence of arboviral diseases as public health problems. Archives of Medical Research. 2002;33(4):330–42. doi: 10.1016/s0188-4409(02)00378-8 [DOI] [PubMed] [Google Scholar]
- 17.Guzman MG, Halstead SB, Artsob H, Buchy P, Farrar J, Gubler DJ, et al. Dengue: a continuing global threat. Nat Rev Microbiol. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ooi E-E, Goh K-T, Gubler DJ. Dengue prevention and 35 years of vector control in Singapore. Emerg Infect Dis. 2006;12(6):887–93. PMC3373041. doi: 10.3201/10.3201/eid1206.051210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egger JR, Ooi EE, Kelly DW, Woolhouse ME, Davies CR, Coleman PG. Reconstructing historical changes in the force of infection of dengue fever in Singapore: implications for surveillance and control. Bull WHO. 2008;86(3):187–96. doi: 10.2471/BLT.07.040170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO. Guidelines for dengue surveillance and mosquito control. Geneva, WHO; 2003. [Google Scholar]
- 21.Carrasco LR, Lee LK, Lee VJ, Ooi EE, Shepard DS, Thein TL, et al. Economic impact of Dengue illness and the cost-effectiveness of future vaccination programs in Singapore. PLoS Negl Trop Dis. 2011;5(12):e1426 doi: 10.1371/journal.pntd.0001426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.David MR, Lourenço-de-Oliveira R, Freitas RMd. Container productivity, daily survival rates and dispersal of Aedes aegypti mosquitoes in a high income dengue epidemic neighbourhood of Rio de Janeiro: presumed influence of differential urban structure on mosquito biology. Mem Inst Oswaldo Cruz. 2009;104:927–32. [DOI] [PubMed] [Google Scholar]
- 23.Reiter P, Lathrop S, Bunning ML, Biggerstaff BJ, Singer D, Tiwari T, et al. Texas lifestyle limits transmission of dengue virus. Emerging Infectious Disease journal. 2003;9(1):86 doi: 10.3201/eid0901.020220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmidt WP, Suzuki M, Thiem VD, White RG, Tsuzuki A, Yoshida LM, et al. Population density, water supply, and the risk of dengue fever in Vietnam: Cohort study and spatial analysis. Plos Medicine. 2011;8(8). doi: 10.1371/journal.pmed.1001082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koh BKW, Ng LC, Kita Y, Tang CS, Ang LW, Wong KY, et al. The 2005 dengue epidemic in Singapore: Epidemiology, prevention and control. Ann Acad Med Singap. 2008;37(7):538–45. [PubMed] [Google Scholar]
- 26.Hapuarachchi HC, Koo C, Rajarethinam J, Chong CS, Lin C, Yap G, et al. Epidemic resurgence of dengue fever in Singapore in 2013–2014: A virological and entomological perspective. BMC Infectious Diseases. 2016;16 doi: 10.1186/s12879-016-1606-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leo YS, Chow ALP, Tan LK, Lye DC, Lin L, Ng LC. Chikungunya outbreak, Singapore, 2008. Emerg Infect Dis. 2009;15(5):836–7. doi: 10.3201/eid1505.081390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maurer-Stroh S, Mak TM, Ng YK, Phuah SP, Huber RG, Marzinek JK, et al. South-east Asian Zika virus strain linked to cluster of cases in Singapore, August 2016. Euro Surveill. 2016;21(38):1560–7917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ooi EE, Hart TJ, Tan HC, Chan SH. Dengue seroepidemiology in Singapore. Lancet. 2001;357(9257):685–6. doi: 10.1016/S0140-6736(00)04137-4 [DOI] [PubMed] [Google Scholar]
- 30.Ministry-of-Heath. Vector-borne/Zoonotic diseases. In: Singapore Cdsi, editor.: Ministry of Health, Singapore; 2015. [Google Scholar]
- 31.Abdul Hamid ARB. Ecological Networks: their application for biodiversity conservation in an urbanized environment: National University of Singapore; 2015. [Google Scholar]
- 32.Tan V. Park usage and satisfactory survey. In: Series US, editor. Singapore2013.
- 33.Wen T-H, Lin M-H, Teng H-J, Chang N-T. Incorporating the human-Aedes mosquito interactions into measuring the spatial risk of urban dengue fever. Applied Geography. 2015;62:256–66. [Google Scholar]
- 34.Rattanarithikul R, Harbach RE, Harrison BA, Panthusiri P, Coleman RE, Richardson JH. Illustrated keys to the mosquitoes of Thailand. VI. Tribe Aedini. Southeast Asian J Trop Med Public Health. 2010;41 Suppl 1:1–225. Epub 2010/07/16. . [PubMed] [Google Scholar]
- 35.Schreiber MJ, Holmes EC, Ong SH, Soh HSH, Liu W, Tanner L, et al. Genomic epidemiology of a Dengue virus epidemic in urban Singapore. J Virol. 2009;83(9):4163–73. doi: 10.1128/JVI.02445-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manokaran G, Finol E, Wang C, Gunaratne J, Bahl J, Ong EZ, et al. Dengue subgenomic RNA binds TRIM25 to inhibit interferon expression for epidemiological fitness. Science. 2015;350(6257):217–21. doi: 10.1126/science.aab3369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson BW, Russell BJ, Lanciotti RS. Serotype-specific detection of dengue viruses in a fourplex real-time reverse transcriptase PCR assay. Journal of Clinical Microbiology. 2005;43(10):4977–83. PMC1248506. doi: 10.1128/JCM.43.10.4977-4983.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lanciotti RS, Kosoy OL, Laven JJ, Panella AJ, Velez JO, Lambert AJ, et al. Chikungunya virus in US travelers returning from India, 2006. Emerg Infect Dis. 2007;13(5):764–7. PubMed Central PMCID: PMCPMC2738459. doi: 10.3201/eid1305.070015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuno G, Chang GJ, Tsuchiya KR, Karabatsos N, Cropp CB. Phylogeny of the genus Flavivirus. J Virol. 1998;72(1):73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfeffer M, Proebster B, Kinney RM, Kaaden OR. Genus-specific detection of alphaviruses by a semi-nested reverse transcription-polymerase chain reaction. Am J Trop Med Hyg. 1997;57(6):709–18. [DOI] [PubMed] [Google Scholar]
- 41.Gubler DJ. Cities spawn epidemic dengue viruses. Nat Med. 2004;10(2):129–30. doi: 10.1038/nm0204-129 [DOI] [PubMed] [Google Scholar]
- 42.Morrison AC, Zielinski-Gutierrez E, Scott TW, Rosenberg R. Defining challenges and proposing solutions for control of the virus vector Aedes aegypti. Plos Medicine. 2008;5(3):e68 PMC2267811. doi: 10.1371/journal.pmed.0050068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bowman LR, Runge-Ranzinger S, McCall PJ. Assessing the relationship between vector indices and dengue transmission: A systematic review of the evidence. PLoS Negl Trop Dis. 2014;8(5):e2848 PMC4014441. doi: 10.1371/journal.pntd.0002848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stoddard ST, Forshey BM, Morrison AC, Paz-Soldan VA, Vazquez-Prokopec GM, Astete H, et al. House-to-house human movement drives dengue virus transmission. Proc Natl Acad Sci U S A. 2013;110(3):994–9. doi: 10.1073/pnas.1213349110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vazquez-Prokopec GM, Kitron U, Montgomery B, Horne P, Ritchie SA. Quantifying the spatial dimension of dengue virus epidemic spread within a tropical urban environment. PLoS Negl Trop Dis. 2010;4(12):0000920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salje H, Lessler J, Endy TP, Curriero FC, Gibbons RV, Nisalak A, et al. Revealing the microscale spatial signature of dengue transmission and immunity in an urban population. Proc Natl Acad Sci U S A. 2012;109(24):9535–8. doi: 10.1073/pnas.1120621109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liebman KA, Stoddard ST, Morrison AC, Rocha C, Minnick S, Sihuincha M, et al. Spatial dimensions of dengue virus transmission across interepidemic and epidemic periods in Iquitos, Peru (1999–2003). PLoS Negl Trop Dis. 2012;6(2):e1472 doi: 10.1371/journal.pntd.0001472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maciel-De-Freitas R, Souza-Santos R, Codeço CT, Lourenço-De-Oliveira R. Influence of the spatial distribution of human hosts and large size containers on the dispersal of the mosquito Aedes aegypti within the first gonotrophic cycle. Med Vet Entomol. 2010;24(1):74–82. doi: 10.1111/j.1365-2915.2009.00851.x [DOI] [PubMed] [Google Scholar]
- 49.Harrington LC, Scott TW, Lerdthusnee K, Coleman RC, Costero A, Clark GG, et al. Dispersal of the dengue vector Aedes aegypti within and between rural communities. Amer J Trop Med Hyg. 2005;72(2):209–20. [PubMed] [Google Scholar]
- 50.Méndez F, Barreto M, Arias JF, Rengifo G, Munoz J, Burbano ME, et al. Human and mosquito infections by dengue viruses during and after epidemics in a dengue-endemic region of Colombia. Amer J Trop Med Hyg. 2006;74(4):678–83. [PubMed] [Google Scholar]
- 51.Conway MJ, Colpitts TM, Fikrig E. Role of the vector in arbovirus transmission. Annual Review of Virology. 2014;1(1):71–88. doi: 10.1146/annurev-virology-031413-085513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kramer LD, Ebel GD. Dynamics of flavivirus infection in mosquitoes. Adv Virus Res. Volume 60: Academic Press; 2003. p. 187–232. [DOI] [PubMed] [Google Scholar]
- 53.Fansiri T, Fontaine A, Diancourt L, Caro V, Thaisomboonsuk B, Richardson JH, et al. Genetic mapping of specific interactions between Aedes aegypti mosquitoes and dengue viruses. Plos Genetics. 2013;9(8). doi: 10.1371/journal.pgen.1003621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goncalves CM, Melo FF, Bezerra JM, Chaves BA, Silva BM, Silva LD, et al. Distinct variation in vector competence among nine field populations of Aedes aegypti from a Brazilian dengue-endemic risk city. Parasit Vectors. 2014;7(320):1756–3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gubler DJ, Rosen L. Variation among geographic strains of Aedes albopictus in susceptibility to infection with dengue viruses. Am J Trop Med Hyg. 1976;25(2):318–25. [DOI] [PubMed] [Google Scholar]
- 56.Tesh RB, Gubler DJ, Rosen L. Variation among geographic strains fo Aedes albopictus in susceptibilty to infection with Chikungunya virus. Am J Trop Med Hyg. 1976;25(2):326–35. [DOI] [PubMed] [Google Scholar]
- 57.Vega-Rua A, Zouache K, Caro V, Diancourt L, Delaunay P, Grandadam M, et al. High efficiency of temperate Aedes albopictus to transmit Chikungunya and Dengue viruses in the southeast of France. PLoS ONE. 2013;8(3). doi: 10.1371/journal.pone.0059716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosen L, Roseboom LE, Gubler DJ, Lien JC, Chaniotis BN. Comparative susceptibility of mosquito species and strains to oral and parenteral infection with dengue and Japanese encephalitis viruses. Am J Trop Med Hyg. 1985;34(3):603–15. [DOI] [PubMed] [Google Scholar]
- 59.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in Chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;3(12):e201 doi: 10.1371/journal.ppat.0030201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zouache K, Fontaine A, Vega-Rua A, Mousson L, Thiberge JM, Lourenco-De-Oliveira R, et al. Three-way interactions between mosquito population, viral strain and temperature underlying chikungunya virus transmission potential. Proceedings of the Royal Society B-Biological Sciences. 2014;281(1792). doi: 10.1098/rspb.2014.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weaver SC, Forrester NL. Chikungunya: Evolutionary history and recent epidemic spread. Antiviral Res. 2015;120:32–9. doi: 10.1016/j.antiviral.2015.04.016 [DOI] [PubMed] [Google Scholar]
- 62.Ng LC, Hapuarachchi HC. Tracing the path of Chikungunya virus—Evolution and adaptation. Infection, Genetics and Evolution. 2010;10(7):876–85. doi: 10.1016/j.meegid.2010.07.012 [DOI] [PubMed] [Google Scholar]
- 63.Paupy C, Ollomo B, Kamgang B, Moutailler S, Rousset D, Demanou M, et al. Comparative role of Aedes albopictus and Aedes aegypti in the emergence of Dengue and Chikungunya in central Africa. Vector Borne Zoonotic Dis. 2010;10(3):259–66. doi: 10.1089/vbz.2009.0005 [DOI] [PubMed] [Google Scholar]
- 64.Lai S, Huang Z, Zhou H, Anders KL, Perkins TA, Yin W, et al. The changing epidemiology of dengue in China, 1990–2014: a descriptive analysis of 25 years of nationwide surveillance data. BMC Medicine. 2015;13(1):1–12. doi: 10.1186/s12916-015-0336-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tomasello D, Schlagenhauf P. Chikungunya and dengue autochthonous cases in Europe, 2007–2012. Travel Medicine and Infectious Disease. 2013;11(5):274–84. doi: 10.1016/j.tmaid.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 66.Delisle E, Rousseau C, Broche B, Leparc-Goffart I, L'Ambert G, Cochet A, et al. Chikungunya outbreak in Montpellier, France, September to October 2014. Euro Surveill. 2015;20(17):21108 [DOI] [PubMed] [Google Scholar]
- 67.Tsuda Y, Maekawa Y, Ogawa K, Itokawa K, Komagata O, Sasaki T, et al. Biting density and distribution of Aedes albopictus during the September 2014 outbreak of dengue fever in Yoyogi park and the vicinity of Tokyo metropolis, Japan. Jpn J Infect Dis. 2016;69(1):1–5. doi: 10.7883/yoken.JJID.2014.576 [DOI] [PubMed] [Google Scholar]
- 68.Huang YM. Contributions to the mosquito fauna of Southeast Asia. XIV. The subgenus Stegomyia of Aedes in Southeast Asia. I–The scutellaris group of species. Contrib Am Entomol Inst. 1972;9(1). [Google Scholar]
- 69.Tewari S, Hiriyan J, Reuben R. Epidemiology of subperiodic Wuchereria bancrofti infection in the Nicobar Islands, India. Trans R Soc Trop Med Hyg. 1995;89(2):163–6. [DOI] [PubMed] [Google Scholar]
- 70.Huang Y-M. Medical entomology studies-XI. The subgenus Stegomyia of Aedes in the oriental region with keys to the species (Diptera: Culicidae). DTIC Document, 1979.
- 71.Vezzani D, Rubio A, Velazquez SM, Schweigmann N, Wiegand T. Detailed assessment of microhabitat suitability for Aedes aegypti (Diptera: Culicidae) in Buenos Aires, Argentina. Acta Trop. 2005;95(2):123–31. doi: 10.1016/j.actatropica.2005.03.010 [DOI] [PubMed] [Google Scholar]
- 72.da Moura AJ, de Melo Santos MA, Oliveira CM, Guedes DR, de Carvalho-Leandro D, da Cruz Brito ML, et al. Vector competence of the Aedes aegypti population from Santiago Island, Cape Verde, to different serotypes of dengue virus. Parasit Vectors. 2015;8(114):015–0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rajavel AR, Natarajan R. Mosquitoes of the mangrove forests of India: Part 3—Andaman and Nicobar Islands, including an update on the mosquito fauna of the islands. J Am Mosq Control Assoc. 2006;22(3):366–77. doi: 10.2987/8756-971X(2006)22[366:MOTMFO]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 74.Shriram AN, Ramaiah KD, Krishnamoorthy K, Sehgal SC. Diurnal pattern of human-biting activity and transmission of subperiodic Wuchereria bancrofti (Filariidea: Dipetalonematidae) by Ochlerotatus niveus (Diptera: Culicidae) on the Andaman and Nicobar islands of India. Am J Trop Med Hyg. 2005;72(3):273–7. . [PubMed] [Google Scholar]
- 75.Moore PR, Johnson PH, Smith GA, Ritchie SA, Van den Hurk AF. Infection and dissemination of dengue virus type 2 in Aedes aegypti, Aedes albopictus, and Aedes scutellaris from the Torres Strait, Australia. J Am Mosq Control Assoc. 2007;23(4):383–8. doi: 10.2987/5598.1 [DOI] [PubMed] [Google Scholar]
- 76.Ledermann JP, Guillaumot L, Yug L, Saweyog SC, Tided M, Machieng P, et al. Aedes hensilli as a potential vector of Chikungunya and Zika viruses. PLoS Negl Trop Dis. 2014;8(10):e3188 doi: 10.1371/journal.pntd.0003188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Poole-Smith BK, Hemme RR, Delorey M, Felix G, Gonzalez AL, Amador M, et al. Comparison of vector competence of Aedes mediovittatus and Aedes aegypti for Dengue virus: Implications for dengue control in the Caribbean. PLoS Negl Trop Dis. 2015;9(2). doi: 10.1371/journal.pntd.0003462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Diallo M, Sall AA, Moncayo AC, Ba Y, Fernandez Z, Ortiz D, et al. Potential role of sylvatic and domestic African mosquito species in dengue emergence. Amer J Trop Med Hyg. 2005;73(2):445–9. [PubMed] [Google Scholar]
- 79.Savage HM, Fritz CL, Rutstein D, Yolwa A, Vorndam V, Gubler DJ. Epidemic of dengue-4 virus in Yap State, Federated States of Micronesia, and implication of Aedes hensilli as an epidemic vector. Am J Trop Med Hyg. 1998;58(4):519–24. [DOI] [PubMed] [Google Scholar]
- 80.The-World-Bank. GDP per capita. In: Bank TW, editor. 2016.
- 81.Emporis. Buildings. 2016.
- 82.Sanchez L, Vanlerberghe V, Alfonso L, Marquetti Mdel C, Guzman MG, Bisset J, et al. Aedes aegypti larval indices and risk for dengue epidemics. Emerg Infect Dis. 2006;12(5):800–6. doi: 10.3201/eid1205.050866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Goh KT. Dengue-a re-emerging infectious disease in Singapore. Ann Acad Med Singapore. 1997;26(5):664–70. [PubMed] [Google Scholar]
- 84.de Castro Medeiros LC, Castilho CA, Braga C, de Souza WV, Regis L, Monteiro AM. Modeling the dynamic transmission of dengue fever: investigating disease persistence. PLoS Negl Trop Dis. 2011;5(1):0000942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sam I-C, Chua CL, Rovie-Ryan JJ, Fu J, Tong C, Sitam FT, et al. Chikungunya virus in Macaques, Malaysia. Emerg Infect Dis. 2015;21(9):1683–5. doi: 10.3201/eid2109.150439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vasilakis N, Cardosa J, Hanley KA, Holmes EC, Weaver SC. Fever from the forest: prospects for the continued emergence of sylvatic dengue virus and its impact on public health. Nat Rev Microbiol. 2011;9(7):532–41. doi: 10.1038/nrmicro2595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Duong V, Lambrechts L, Paul RE, Ly S, Lay RS, Long KC, et al. Asymptomatic humans transmit dengue virus to mosquitoes. Proc Natl Acad Sci U S A. 2015;112(47):14688–93. doi: 10.1073/pnas.1508114112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hapuarachchi HC, Koo C, Kek R, Xu H, Lai YL, Liu L, et al. Intra-epidemic evolutionary dynamics of a Dengue virus type 1 population reveal mutant spectra that correlate with disease transmission. Sci Rep. 2016;6(22592). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Morphological differences between Ae. malayensis (A) and Ae. albopictus (B). The primary differences are the suprealar scale patch extending to the scutellum in Ae. malayensis (i), the scalloped pattern of abdominal tergites (IV-VI) on Ae. malayensis (ii), and the absence of scales from the subspiracular area in Ae. malayensis (iii). Images credited to Nicky Bay.
(TIF)
(XLSX)
Total numbers of eggs collected and mosquitoes reared from Transect A and B in East Coast Park, Singapore, for the patch fidelity and oviposition experiments.
(XLSX)
(XLSX)
Viral genome copy number in abdomen and thorax of Ae. aegypti, Ae. albopictus and Ae. malayensis at 14 days post oral infection with (A) DENV or (B) CHIKV. nd: not detected.
(XLSX)
Infection rate and viral genome copy number for Ae. malayensis injected with saliva collected from DENV- (A) or CHIKV- (B) infected Ae. malayensis. nd: not detected.
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.