Abstract
Mindfulness-Based Cognitive Therapy (MBCT) and Mindfulness-Based Stress Reduction (MBSR) emphasize the importance of mindfulness practice at home as an integral part of the program. However, the extent to which participants complete their assigned practice is not yet clear, nor is it clear whether this practice is associated with positive outcomes.
For this systematic review and meta-analysis, searches were performed using Scopus and PubMed for studies published through to the end of 2015, reporting on formal home practice of mindfulness by MBSR or MBCT participants.
Across 43 studies (N = 1427), the pooled estimate for participants' home practice was 64% of the assigned amount, equating to about 30 minutes per day, six days per week [95% CI 60–69%]. There was substantial heterogeneity associated with this estimate. Across 28 studies (N = 898), there was a small but significant association between participants’ self-reported home practice and intervention outcomes (r = 0·26, 95% CI 0·19,–0·34).
MBSR and MBCT participants report completing substantial formal mindfulness practice at home over the eight-week intervention, albeit less than assigned amounts. There is a small but significant association between the extent of formal practice and positive intervention outcomes for a wide range of participants.
Keywords: Mindfulness-based cognitive therapy, Mindfulness-based stress reduction, Treatment engagement, Treatment adherence, Homework, Adherence, Mindfulness practice, Meditation practice
Highlights
-
•
Standard mindfulness interventions assign significant home practice.
-
•
This meta-analysis estimated participants' typical practice completion.
-
•
Average mindfulness home practice time equated to 30 min per day, 6 days per week.
-
•
The extent of practice positively correlated with intervention outcomes.
Contemporary psychological treatments require active engagement by participants, both in sessions with a therapist, and in applying and practicing new skills in their lives. Between-session development of these skills through ‘home practice’ is an integral component of treatment. Such home practice is viewed as necessary for participants to gain the insights and skills for the intended treatment outcomes. For cognitive behavioral therapy (CBT), this takes the form of variable assignments, such as self-monitoring, exposure to feared situations, or scheduling of behavioral experiments that extend the therapeutic sessions. Several meta-analyses have provided evidence for a small to moderate association between home assignment completion and CBT treatment outcomes across different psychological disorders (Kazantzis et al., 2010, Mausbach et al., 2010).
Mindfulness-Based Cognitive Therapy (MBCT) and Mindfulness-Based Stress Reduction (MBSR) are manualized, group-based skills training programs that teach mindfulness both in and between sessions. Between-session practice consists of informal and formal home mindfulness practice that trains attention and develops the ability to respond to difficult mental and physical experiences (Kabat Zinn, 1990, Segal et al., 2012). Informal practices encourage mindfulness in everyday life, for example, by deliberately focusing awareness on everyday activities and savouring pleasant experiences. In a formal practice, participants are given guidance as to the nature and content of the practice (e.g., suggestions as to the posture adopted, attitude and how attention is directed).
Typically, participants’ formal practices are supported by audio recordings. In the early weeks of the intervention, participants are gradually introduced to a range of formal meditation practices, focusing initially on mindfulness of the body and the breath, and later the body in movement and mindfulness of thoughts and other mental events. Early practices are intended to support participants in stabilising attention, beginning to notice patterns of mind wandering and increasing the ability to return the mind to an intended focus of attention when mind wandering occurs. Later practices encourage participants to observe patterns of mind wandering in more detail and approach difficult mental content or unpleasant physical sensations with an attitude of curiosity, acceptance and non-judgement. In the final weeks of these interventions, participants are typically encouraged to develop a pattern of formal meditation practice that fits in with their daily life and which will be sustainable beyond the 8-week intervention. In class, teachers review weekly home practice, inviting participants to share their experiences to aid generalisation of learning. These mindfulness home practices are assumed to be critical to therapeutic change. While a growing number of studies have explored the relationship between practice and change, this research is still at an early stage.
This systematic review and meta-analysis aimed to address two key questions about participants' between-session practice in MBSR and MBCT. First, we examined the extent to which participants report completing the assigned formal mindfulness home practice. This is important because psychological ill-health can compromise an individual's capacity to adhere to treatment guidelines (Prince et al., 2007). Furthermore, where interventions involve extensive behavioral components, adherence is often less than ideal (DiMatteo, 2004). Second, we assessed whether there is evidence that completion of formal practice, which is most frequently recorded in MBSR and MBCT studies (Vettese, Toneatto, Stea, Nguyen, & Wang, 2009), is associated with treatment outcomes. It is widely accepted that the full benefit of many effective treatments can only be achieved if the prescribed regime is followed reasonably closely (Osterberg & Blaschke, 2005), but this has not yet been established for mindfulness practice in MBSR and MBCT.
1. Methods
This review followed procedures outlined in the Cochrane Handbook for Systematic Reviews (Higgins & Green, 2008) and by the Centre for Reviews and Dissemination (CRD, 2014). The review protocol was registered with PROSPERO [CRD42015029959].
2. Search strategy
Searches were performed using Scopus and PubMed for studies published through to the end of 2015, which reported on home practice of mindfulness in MBSR or MBCT. The search terms were: ‘Mindfulness based stress reduction’ or ‘mindfulness based cognitive therapy’, or ‘MBSR’, or ‘MBCT’ and ‘practice’ or ‘homework’ or ‘adherence’ or ‘compliance’ or ‘engagement’ (see Supplementary Materials for search strings). Only primary research presenting novel data on mindfulness practice was included. Two independent reviewers (CP, LP) performed title and abstract screening and full text review using the web-based software platform Covidence, (www.covidence.org; a Cochrane recommended primary screening tool). At full text review, studies were checked to ensure reporting of results from unique, non-overlapping participants. While Covidence does not allow for post hoc calculation of Cohen's Kappa for inter-rater reliability, agreement on screening and data extraction was established between the first two reviewers through discussion for all but 7 issues. These 7 disagreements were resolved with referral to a third reviewer (CC).
We included studies that reported on MBCT or MBSR delivered in line with the format described in the respective manuals, namely an eight-week group program, with class time of 2-2·5 h and one all-day retreat, requiring at-home mindfulness practice for about 45 min, six days per week (Kabat Zinn, 1990, Segal et al., 2013). Studies were excluded if they reported substantial deviations from the standard format such as shortened class times or fewer than eight classes. However, we included studies with reduced home practice requirements (less than the recommended 45 min) as a separate subgroup. Studies were also excluded if they did not report collecting data on participants’ home practice.
We included studies that reported formal home mindfulness practice data (referred to throughout as mindfulness practice) in a format that allowed calculation of average minutes of practice per day, or average number of formal practice sessions per week, for the duration of the course. If studies reported collecting home practice data, but did not report these values, authors were contacted for this information. If authors described the home practice requirements of their intervention, but did not report any actual home practice data, their study was not included in the review. In total, 57 authors were contacted, and 26 responded. Eight authors were able to provide information on formal home practice completion amounts and ten were able to provide information on home practice-outcome associations. Formal practice, defined as the assigned, scheduled home mindfulness sessions (e.g., following a guided meditation, 3-min breathing space), was the focus of our analyses. Formal practice is arguably easier to record in a standard way compared with informal practice, and is more widely reported (Vettese et al., 2009).
In instances of missing or incomplete data, authors were first contacted. Where standard deviations were unavailable after this (12 studies), we compared two methods for SD imputation. The first used an average pooled SD from all other included studies 1 and the second used the largest SD from the available studies. Both yielded similar estimates, so the former method was implemented (Furukawa, Barbui, Cipriani, Brambilla, & Watanabe, 2006). To generate an aggregate estimate of the amount of home practice, a random effects model was implemented with the mean percentage of recommended home practice time (% of 45 min or % of 6 sessions).
3. Data extraction and synthesis
Information was extracted from each study as follows (1) the characteristics of the study, where relevant (design, randomization, blinding, therapist qualifications, number of participants, class attendance recorded, type of outcome measures, overall intervention effects), (2) the characteristics of the intervention, including target population (3) the characteristics of participants, including people who did not complete the MBSR/MBCT program (4) home practice details, including recording method, number of participants providing data, amount of formal practice in minutes (or if practice amount was not reported, the number of formal sessions) (M, SD) (5) data on the association between practice (across the entire course) and intervention outcomes. Table 1 presents study characteristics related to the recording of mindfulness practice, class attendance, teacher training and inclusion of a one-day retreat.
Table 1.
Study characteristics related to recording of practice, class attendance, teacher training and adherence and inclusion of a one-day retreat.
| Study | How was practice recorded? | Frequency of practice form collection | Teacher training reported | Did the authors use a scale/measure to check intervention adherence? | Class attendance reported? | All-day retreat |
|---|---|---|---|---|---|---|
| Studies with standard home practice requirements | ||||||
| Baer, Carmody, and Hunsinger (2012) | Weekly logs | Weekly | N | N | Y | All-day retreat |
| Barnhofer et al. (2009) | Homework records | Not specified | Y | N | Y | Not specified |
| Blom et al. (2014) | Weekly logs | Weekly | N | N | Y | 6 h |
| Bluth, Gaylord, Nguyen, Bunevicius, and Girdler (2015) | Daily logs | Weekly collection | Y | N | Y | 4 h |
| Britton, Haynes, Fridel, and Bootzin (2010) | Weekly logs | Weekly collection | Y | N | Y | All-day retreat |
| Britton, Haynes, Fridel, and Bootzin (2012) | Weekly logs | Weekly | Y | N | Y | All-day retreat |
| Campbell, Labelle, Bacon, Faris, and Carlson (2012) | Daily logs collected at end of course | End of course | Y | N | Y | 6 h retreat |
| Carlson, Speca, Patel, and Goodey (2004) | Daily log | Weekly | N | N | Y | 3 h retreat |
| Carmody and Baer (2008) | Weekly collection | Weekly class | N | N | Y | All-day retreat |
| Carmody et al. (2008) | Course folder with colour tabs | Weekly class | N | N | N | All-day retreat |
| Carmody et al. (2011) | Weekly log collected | Weekly | Y | N | Y | All-day retreat |
| Cole et al. (2015) | Practice logs, frequency not mentioned | Not specified | Y | N | Y | All-day retreat |
| Collard, Avny, and Boniwell (2008) | Questionnaires at start and end | Not specified | N | N | N | Not specified |
| Crane et al. (2014) | Daily log | Weekly | Y | Y | Y | Not specified |
| Day et al. (2014) | Daily online log | Daily | Y | Y | Y | Not specified |
| Del Re, Flückiger, Goldberg, and Hoyt (2013) | Record after each home practice | End of course | Y | N | Y | All-day retreat |
| Eisendrath et al. (2015) | Weekly logs | Weekly | Y | N | Y | Not specified |
| Farb, Segal, and Anderson (2013) | Daily log collected at End of course | End of course | N | N | Y | All-day retreat |
| Foley, Baillie, Huxter, Price, and Sinclair (2010) | Daily log collected at End of course | End of course | Y | N | Y | All-day retreat |
| Geschwind (2012) | Not specified | Not specified | Y | N | Y | All-day retreat |
| Goldsmith et al. (2014) | Weekly logs | Not specified | N | N | N | No retreat |
| Gross et al. (2011) | Electronic loggers | Daily | Y | N | Y | All-day retreat |
| Hawley et al. (2014) | Weekly logs | Weekly | Y | Y | N | Not specified |
| Hoffman et al. (2012) | Weekly sheets | Not specified | Y | N | Y | 6 h |
| Hölzel et al. (2011) | Daily logs | Not specified | N | N | N | 6.5 h |
| Hou et al. (2013) | Weekly collection | Weekly class | Y | N, but sessions videotaped and reviewed | Y | no retreat |
| Jazaieri et al. (2012) | Weekly phone calls to monitor practice | Weekly | Y | N | N | All-day retreat |
| Jensen et al., 2012 | Daily logs | Not specified | Y | N | Y | 7 h retreat |
| Johansson, Bjuhr, Karlsson, Karlsson, and Rönnbäck (2015) | Daily log | End of course | Y | N | Y | 7 h retreat |
| Kluepfel et al. (2013) | Weekly log | Weekly | Y | Y | Y | All-day retreat |
| Labelle, Lawlor-Savage, Campbell, Faris, and Carlson (2015) | Weekly logs | Weekly | Y | N | Y | 6 h retreat |
| MacCoon et al. (2012) | Minutes and sessions recorded; frequency not specified | Not specified | Y | N | Y | 7 h retreat |
| Nyklicek and Kuijpers (2008) | Weekly logs | Weekly | N | N | Y | 6 h retreat |
| Ong et al. (2014) | Daily logs | Not specified | Y | N | Y | 6 h retreat |
| Parkin et al. (2014) | Asked weekly about practice time | Weekly | Y | N | N | No retreat |
| Perich, Manicavasagar, Mitchell, and Ball (2013) | Daily record | Weekly | Y | Y | Y | Not specified |
| Pickut et al. (2015) | Weekly logs | Weekly class | N | N | Y | no retreat |
| Pradhan et al. (2007) | Daily logs | Not specified | Y | N | Y | All-day retreat |
| Ramel, Goldin, Carmona, and McQuaid (2004) | Weekly logs but only half participants filled in; all estimated at follow-up. Data at follow up used | Weekly class | Y | N | N | Not specified |
| Rimes and Wingrove (2011) | Not specified | Not specified | Y | N | Y | Not specified |
| Roland et al. (2015) | Daily log | Weekly class | Y | N | Y | 3 h retreat |
| Shallcross et al. (2015) | Not specified | Not specified | Y | Y | Y | Not specified |
| Shapiro, Brown, and Biegel (2007) | Daily log | Not specified | Y | N | N | Not specified |
| Shapiro, Jazaieri, and Goldin (2012) | Daily log | Weekly class | Y | N | N | half-day retreat |
| Shapiro, Oman, Thoresen, Plante, and Flinders (2008) | Daily logs | Not specified | Y | N | Y | No retreat |
| Vøllestad, Sivertsen, and Nielsen (2011) | Daily log | Not specified | N | N | Y | Half-daYretreat |
| Whitebird et al. (2013) | Daily log | Not specified | Y | N | Y | 5 h retreat |
| Wong et al. (2011) | Weekly log | Weekly class | Y | N | Y | 7 h retreat |
| Zernicke et al. (2013) | Weekly logs | Weekly class | Y | N | Y | 3 h retreat |
| Studies with reduced practice requirements | ||||||
| Astin (1997) | Daily log | Not specified | N | N | N | no retreat |
| Bakker et al. (2014) | Calendar diary | Weekly class | Y | N | Y | Not specified |
| Creswell et al. (2012) | Daily log | Not specified | N | N | Y | 7 h retreat |
| Gross et al. (2011) | Daily log | Regular phone calls | Y | N | Y | Not specified |
| Hölzel et al. (2011) | Not specified a | Not specified | N | N | Y | All-day retreat |
| Kimbrough, Magyari, Langenberg, Chesney and Berman (2010) | Daily log | Weekly class | Y | N | Y | 5 h retreat |
| Rosenzweig et al. (2007) | Not specified | Weekly class | N | N | N | 7 h retreat |
| Walach et al. (2007) | Daily log | Not specified | Y | N | N | 6 h |
| Wells et al. (2013) | Not specified | Not specified | Y | N | Y | one day retreat |
| Wells et al. (2014) | Daily log | Not specified | Y | N | Y | 6 h retreat |
Reduced home practice requirements detailed in Hou et al., 2013.
To analyse the association between practice and outcomes, we used the primary outcome at the end of the intervention (around eight weeks), as reported by the study investigators. If this was not specified, we used the most frequently reported measures across studies (BAI, GAD-7, and BDI, PHQ-9, DASS-21 depression subscale, consistent with (Newby, McKinnon, Kuyken, Gilbody, & Dalgleish, 2015). For the two studies reporting longer-term primary outcomes (e.g., hazard of relapse to depression), we obtained outcome measures recorded at the end of the intervention. This decision was made in order to synthesise as much available comparable data as possible. In some instances, authors reported related measures of one physical outcome (e.g., for sleep, sleep initiation, frequency of awakening) and we computed a composite variable (as outlined by Borenstein, Hedges, Higgins, & Rothstein, 2009).
If authors reported standardized regression coefficients, these were used to estimate correlation coefficients (as described by Peterson & Brown, 2005). For two studies (Carmody et al., 2008, Gross et al., 2011), Spearman's rho values were reported and these were converted to Pearson's r (Gilpin, 1993). Where authors reported only that correlations did not reach significance (n = 6), a correlation coefficient was estimated using the study sample size and a conservative p-value of 0·5. Heterogeneity was investigated using forest plots and the I2 statistic.
4. Subgroup analyses
To assess the differences between a priori identified subgroups of interest (participant group: clinical or nonclinical; intervention primary outcome: physical functioning, psychological functioning or mixed), we conducted subgroup analyses using the mixed effect model approach. We also examined differences across study design (RCTs, non-randomized trials, before and after studies) and differences between MBCT and MBSR.
5. Study quality
We examined the risk of bias of included RCTs using the Cochrane ‘Risk of Bias’ tool (Higgins & Green, 2011) and for other study designs, we recorded applicable information. Assessment of study quality was conducted by two independent reviewers (CP, LP) and disagreements were resolved through discussion. Table 2 presents the characteristics related to these quality indices.
Table 2.
Study characteristics related to quality indices.
| Study | Design | Randomized | Randomization procedure | Treatment allocation concealed | Similar at Baseline | Blinded Outcomes | Dropouts recorded | Dropout Reasons | ITT | Power |
|---|---|---|---|---|---|---|---|---|---|---|
| Studies with standard home practice requirements | ||||||||||
| Baer et al. (2012) | Before and after | N | N/A | N/A | N/A | N | Y | N | N | N |
| Barnhofer et al. (2009) | RCT | Y | Y | N | N | Y | Y | N | Y | Y - but underpowered |
| Blom et al. (2014) | RCT | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Bluth et al. (2015) | Non-randomized controlled trial | N | N/A | N/A | N | N | Y | Y | N | N |
| Britton et al. (2010) | RCT | Y | Y | Y | N | Y | Y | N | N | N |
| Britton et al. (2012) | RCT | Y | Y | N/A | Y | Y | Y | Y | N | N |
| Campbell et al. (2012) | Non-randomized controlled trial | N | N/A | N/A | Y | N | Y | Y | Y | Y |
| Carlson et al. (2004) | Before and after | N | N/A | N/A | N/A | N/A | Y | Y | N | N/A |
| Carmody and Baer (2008) | Before and after | N | N/A | N/A | N/A | N | Y | N | N | N/A |
| Carmody et al. (2008) | Before and after | N | N/A | N/A | N/A | N | Y | N | N/A | N/A |
| Carmody et al. (2011) | RCT | Y | Y | N | N | Y | Y | Y | Y | N |
| Cole et al. (2015) | Before and after | N | N/A | N/A | N/A | N | Y | N/A | N/A | N/A |
| Collard et al. (2008) | Before and after | N | N/A | N/A | N/A | N/A | Y | N | N/A | N/A |
| *Crane et al. (2014) | RCT | Y | Y | N | Y | Y | Y | N | N/A | Y |
| Day et al. (2014) | RCT | Y | N | N/A | Y | N | Y | N | Y | Y |
| Del Re et al. (2013) | Before and after | N | N/A | N/A | N/A | N | Y | N/A | N | N/A |
| Eisendrath et al. (2015) | Non-randomized controlled trial | N | N/A | N/A | Y | N | Y | Y | N | N |
| Farb et al. (2013) | RCT | Y | N | N/A | Y | N | N | N | N | N |
| Foley et al. (2010) | RCT | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Geschwind (2012) | RCT | Y | Y | N | Y | N | Y | Y | Y | Y |
| Goldsmith et al. (2014) | Before and after | N | N/A | N/A | N/A | N/A | Y | N | N/A | N/A |
| Gross et al. (2011) | RCT | Y | Y | N/A | N | N | Y | N | N | Y |
| Hawley et al. (2014) | RCT | Y | NA | N | N/A | Y | N | N | N/A | N/A |
| Hoffman et al. (2012) | RCT | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Hölzel et al. (2011) | Non-randomized controlled trial | N | N/A | N/A | N/A | N | N | N | N/A | N/A |
| Hou et al. (2013) | RCT | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Jazaieri et al. (2012) | RCT | Y | Y | N | Y | N | Y | Y | Y | N |
| Jensen et al. (2012) | RCT | Y | N | Y | N | Y | Y | Y | N | N |
| Johansson et al. (2015) | Non-randomized controlled trial | N | N/A | N/A | Y | N | Y | Y | Y | N |
| Kluepfel et al. (2013) | Before and after | N | N/A | N/A | N/A | N/A | Y | Y | N | N/A |
| Labelle et al. (2015) | Non-randomized controlled trial | N | N/A | N/A | N/A | N | Y | N | Y | Y |
| MacCoon et al. (2012) | RCT | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Nyklicek and Kuijpers (2008) | RCT | Y | Y | N | Y | Y | Y | N | Y | Y |
| Ong et al. (2014) | RCT | Y | Y | Y | Y | N | Y | N | Y | Y |
| Parkin et al. (2014) | Before and after | N | N/A | N/A | N/A | N/A | Y | N | N/A | N/A |
| Perich et al. (2013) | RCT | Y | N | N | Y | Y | Y | N | Y | Y |
| Pickut et al. (2015) | RCT | Y | N | N/A | Y | Y | Y | Y | N | N |
| Pradhan et al. (2007) | RCT | Y | Y | N | N | Y | Y | Y | Y | Y |
| Ramel et al. (2004) | Non-randomized controlled trial | N | N/A | N/A | Y | N | Y | N | N | N |
| Rimes and Wingrove (2011) | Before and after | N | N/A | N/A | N/A | Y | N | N/A | N/A | N/A |
| Roland et al. (2015) | Before and after | N | N/A | N/A | N/A | N | Y | N | N | N/A |
| Shallcross et al. (2015) | RCT | Y | Y | N/A | Y | Y | Y | N | Y | Y |
| Shapiro et al. (2007) | Non-randomized controlled trial | N | N/A | N/A | Y | N | Y | N | N | N |
| Shapiro et al. (2012) | Before and after | N | N/A | N/A | N/A | N/A | Y | N/A | N/A | N |
| Shapiro et al. (2008) | RCT | Y | Y | N/A | Y | N | Y | N | N | N |
| Vøllestad et al. (2011) | RCT | Y | N | N/A | Y | N | Y | Y | Y | N |
| Whitebird et al. (2013) | RCT | Y | Y | N | Y | N | Y | Y | Y | N |
| Wong et al. (2011) | RCT | Y | Y | Y | Y | Y | Y | N | Y | Y |
| Zernicke et al. (2013) | RCT | Y | Y | N | Y | N | Y | Y | Y | Y |
| Studies with reduced practice requirements | ||||||||||
| Astin (1997) | RCT | Y | N | N | Y | N | Y | N | N | N |
| Bakker et al. (2014) | RCT | Y | Y | N | Y | N | Y | N | Y | Y |
| Creswell et al. (2012) | RCT | Y | Y | N | Y | N | Y | N | Y | N |
| Gross et al. (2004) | pre-post | N | N/A | N/A | N/A | N | Y | N | N/A | Y |
| Hölzel et al. (2011) | RCT | Y | Y | ? | Y | Y | Y | Y | N | N |
| Kimbrough et al. (2010) | pre-post | N | N/A | N | N/A | N | Y | Y | N/A | Y |
| Rosenzweig et al. (2007) | pre-post | N | N/A | N/A | N/A | N | Y | Y | N | N/A |
| Walach et al. (2007) | non randomized | N | N/A | N/A | N/A | N | Y | Y | N | N |
| Wells et al. (2013) | RCT | Y | Y | N | N | N | N | N | N/A | N |
| Wells et al. (2014) | RCT | Y | Y | N | N | N | Y | N/A | Y | Y - but underpowered |
Note: Randomized = Was the study randomized? PR = Procedure for randomization described? TA = Treatment allocation concealed? Baseline = Similar at baseline? BO = Blind outcome assessments-if unclear note as N, Dropouts = Number of dropouts mentioned. If no mention, score N, DR = Withdrawal reasons stated for dropouts ITT = Intent to treat analysis, Power = Power calculation described. * RCT details described in Williams et al., 2014.
6. Study characteristics
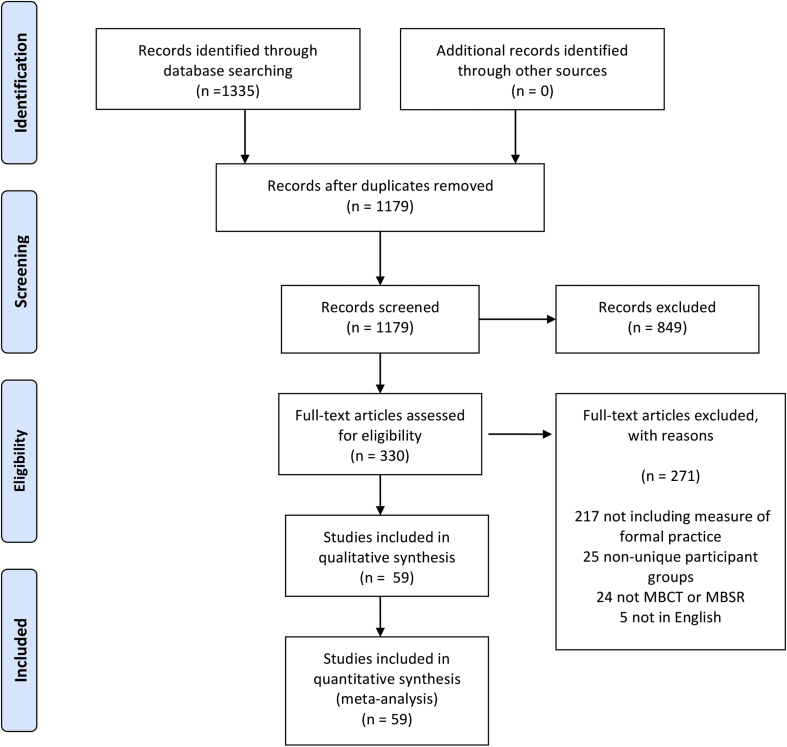
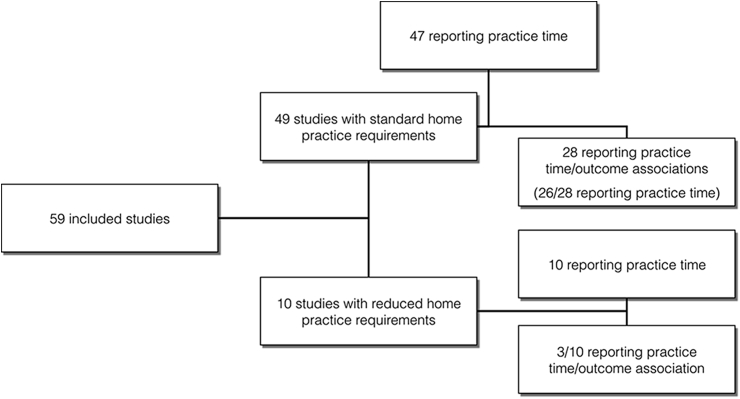
Fig. 1 presents the PRISMA flow chart for the included studies. A total of 49 studies were identified that reported mindfulness practice in MBSR/MBCT with standard home practice requirements (45 min). An additional 10 studies were identified that had reduced home practice requirements (N = 141). Two of the 49 studies reported on associations between mindfulness practice and outcomes (Carmody et al., 2008, Eisendrath et al., 2015) but the mean mindfulness practice data were not available. For the ‘standard’ interventions, 28 studies (N = 898) reported associations between practice and intervention outcomes, or provided this data when contacted. For the ‘reduced practice’ interventions, three studies reported information on the correlation between practice and outcomes, or provided this data when contacted (see Fig. 2).
Fig. 1.
PRISMA diagram of study inclusion.
Fig. 2.
Number of studies reporting on home practice and the association between practice time and outcomes.
Of the 49 studies included with standard home practice requirements, 28 were RCTs, 15 were uncontrolled ‘before and after’ studies and six were non-randomized controlled trials. The majority of studies reported on clinical populations (clinical n = 41; nonclinical = 8). Most reported on MBSR groups (n = 34), while 12 reported on MBCT, and a further two reported on mixed MBCT and MBSR groups. There were a variety of populations treated in these studies, but the most common were depression/anxiety (n = 10), cancer (n = 5) and insomnia (n = 4). The majority examined primary outcomes related to psychological functioning (e.g., depression, anxiety, stress; n = 33), but a substantial proportion examined physical functioning (e.g., blood pressure, sleep, BMI; n = 12), and a smaller number reported ‘mixed’ outcomes (e.g., quality of life; n = 4). Of the 10 studies included with reduced home practice requirements, 6 were RCTs, 3 were uncontrolled ‘before and after’ studies and one was a non-randomized controlled trial. All of these studies examined MBSR participants (see Table 1).
In general, studies reported on the training of the intervention teacher (36/49 of standard format studies, 6/10 reduced practice format) and number of classes attended by participants (37/49 of standard format studies, 7/10 reduced practice format). Only a small number of studies reported using a scale to assess intervention adherence by the teacher (5/49 standard format studies).
7. Risk of bias within randomized controlled trials
The methodological quality of the studies reporting RCTs varied widely (see Table 2). Twenty-six (76%) reported adequate generation of random sequencing, 6 (17%) reported adequately concealing group allocation, and 18 (51%) reported appropriate blinding of outcome assessments. Dropouts were reported for 31 studies (86%), but only a minority reported dropout reasons (46%). Twenty-two studies (63%) reported intent to treat analysis. Seventeen studies reported power calculations, but two of these reported that the sample size was underpowered.
8. How much practice do participants complete in standard format MBSR/MBCT?
Mindfulness practice was typically recorded in paper diaries and collected during the weekly classes (Table 1). Practice records were described as logs, diaries, calendars, or forms (e.g., “Tick boxes were used by participants to record each element of home practice alongside a space to make any free response comments on their home practice for their own benefit and that of the class instructor” from Crane et al., 2014.). One study used an online daily diary recording method (Day et al., 2014), one used electronic loggers (Gross et al., 2011) and one used weekly phone calls to monitor practice (Jazaieri, Goldin, Werner, Ziv, & Gross, 2012). Most studies reported participants’ practice as an average amount (minutes, hours) per week or per day, allowing calculation of an overall percentage of recommended practice completion. Four studies reported only the frequency of practice per week (see Table 1), and this was expressed as a percentage of the recommended 6 times per week.
Four studies were identified as extreme outliers. Three studies reported that participants completed more than 45 min (>100%) of practice and it was not possible to establish if this was combined reports of formal and informal home practice for two cases (Cole et al., 2015, Pradhan et al., 2007). One study was an outlier in the other direction (Del Re et al., 2013), with participants reporting an average of 14% of home practice (SD = 3·14%). These studies were excluded from pooled estimates because of the uncertainty involved in these participant reports, but their exclusion did not impact on the pattern of results.
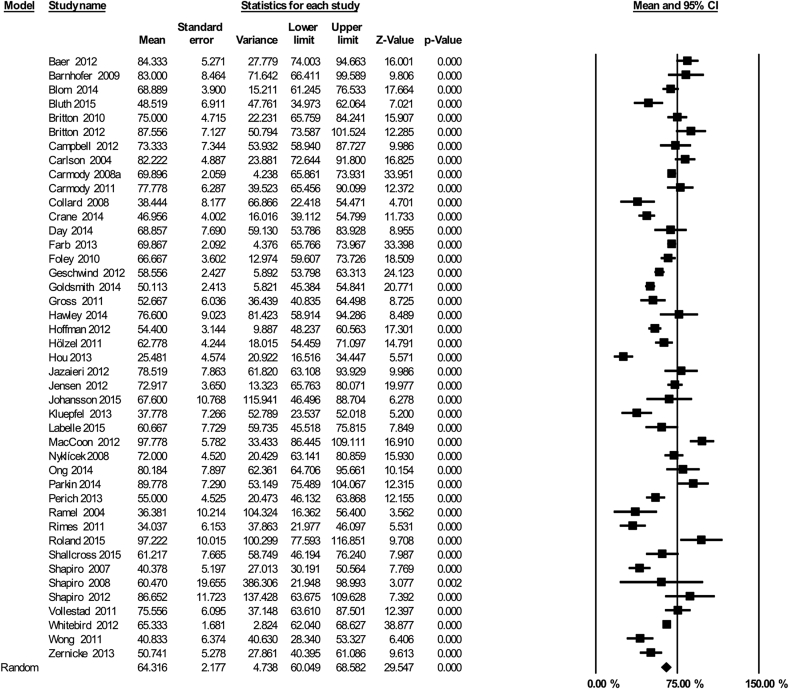
Across the 43 included studies, the pooled estimate for participants’ practice was 64% of the recommended amount (which equates to approximately 29 min per day, Fig. 3, 95% CI 60–69%]. However, there was substantial heterogeneity associated with this estimate, as reflected by I2 = 89%.
Fig. 3.
Mindfulness practice in standard format MBSR/MBCT: Mean percentage of recommended practice (45 min, six days per week) reported across 43 studies.
There were no significant differences in practice for studies examining clinical populations (n = 35, 65·95%, 95% CI 62·06 - 69·83%) and nonclinical populations (n = 8; 56·32%, 95% CI 36·67–76·33; Q = 0·84, df = 1, p = 0·36). We compared studies where primary intervention outcomes related to physical functioning, psychological functioning or a ‘mixed’ outcome (e.g., quality of life). Tau squared values were pooled across subgroups because of the limited number of ‘mixed’ outcome studies as recommended by Borenstein et al., (2009). There were no significant differences in home practice between studies examining primary intervention outcomes related to psychological functioning (n = 29; 67·93%, 95% CI 59·9–75·95%), physical functioning (n = 12, 67·95; 95% CI 59·83–76·07%), and mixed outcomes (n = 3, 66·7%; 95% CI 49·87–83·53%; Q = 1·35, df = 2, p = 0·51).
Comparing MBCT and MBSR, we found no significant differences in home practice reports (MBCT: n = 11, 61.08%, 95% CI 52·7–69·44%; MBSR: n = 21, 64·4%; 95% CI 59.26–69.52%; Q = 0.44, df = 1, p = 0·51).
Finally, three comparisons were performed related to practice recording, study design and study quality. First, studies were compared that asked participants to fill in ‘daily’ logs of practice (n = 18) compared with ‘weekly’ logs (n = 18). While heterogeneity was lower across studies reporting the use of daily logs (I2 = 84%) compared to weekly logs (I2 = 93%), there was no evidence for significant differences in home practice across these two groups (daily: 64·6% 95% CI 59–70·3%; weekly: 65·6%, 95% CI 56·9–74·25%, Q = 0·03, df = 1, p = 0·86). Second, there was also no evidence for significant differences in home practice by study design, comparing RCTs (n = 26; 64·9%, 95% CI 59·4–70·47%), non-randomized trials (n = 7; 61·5%, 95% CI 49·1–73·9%) and before and after studies (n = 10; 64·3%, 95% CI 55·25–73·3%; Q = 0·25, df = 2, p = 0·88). Third, we also restricted analysis to RCTs with a low risk of bias, as indicated by three criteria (see Table 2 reporting of randomization procedure, blinding of outcomes, recording of attrition). Heterogeneity remained high in this subgroup of RCTs (n = 13, 66%, 95% CI 55·76–77·1%, I2 = 93%). Finally, we performed a sensitivity analysis excluding studies with small sample sizes (less than 20, n = 14). The pooled estimate of participants' practice was 62·7% (CI 57·79–67·75%), but again heterogeneity was substantial (I2 = 90%).
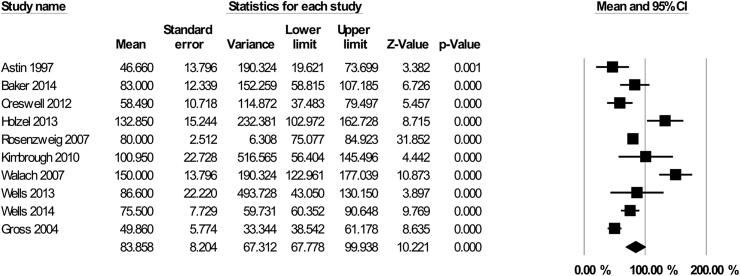
9. Studies with reduced home practice requirements
In 10 studies (N = 141), participants were asked to practice for less than the standard amount (i.e., less than 45 min per day/6 days per week or 270 min). We calculated the amount of practice participants reported completing as a percentage of the amount requested. On average, these studies asked participants to practice for 180 min (SD = 43) across the week (e.g., 30 min per day, 6 days per week, or 45 min per day, 5 days per week). The pooled estimate for participants' practice was 83.86% of the requested amount (which equates to approximately 151 min per week, 95% CI 67.78–99.94%, see Fig. 4). However, there was substantial heterogeneity associated with this estimate, as reflected by I2 = 87.89%. We expressed the practice time of these intervention participants as a percentage of the standard practice time, to compare interventions with different practice requirements. A subgroup comparison showed that participants in the ‘standard practice’ interventions reported completing more practice than those in the ‘reduced practice’ interventions (n = 10, 52.24%, 95% CI 43.18–61.3%, Q = 5.6, df = 1, p = 0·02).
Fig. 4.
Mindfulness practice in MBSR/MBCT with reduced home practice requirements: Mean percentage completed of requested practice reported across 10 studies.
10. Publication bias
We found evidence suggesting a publication bias for the studies reporting on quantity of home practice (see Appendix 2, Fig. 1). Duval and Tweedie's Trim and Fill method, testing for missing studies to the left side of the mean effect based on a random effects model, suggested five missing studies, with an imputed point estimate of 61% (95% CI 56·8 - 65·6%). However, given the substantial heterogeneity associated with the home practice pooled estimate, the Trim and Fill imputed estimate should also be interpreted cautiously (Terrin, Schmid, Lau, & Olkin, 2003).
11. Is there an association between home practice and intervention outcomes?
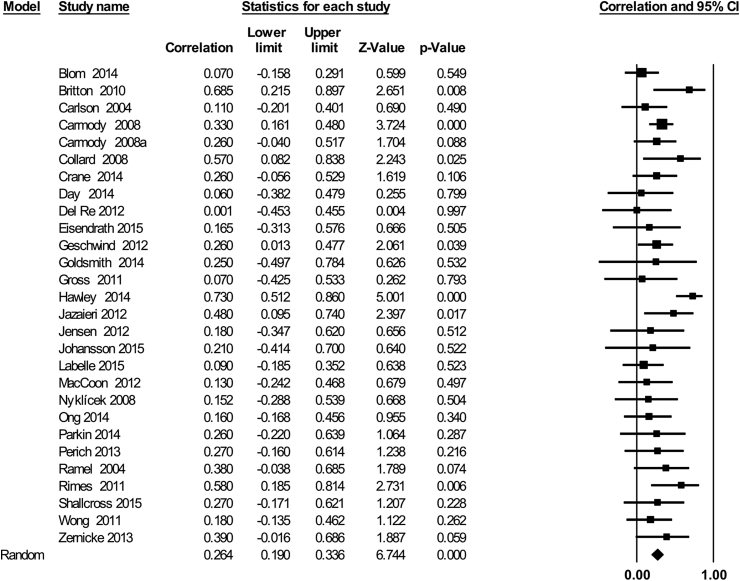
Across the 28 studies, there was a small but significant association between participants’ home practice and intervention outcomes (Fig. 5, r = 0·26, 95% CI 0·19,–0·34, Z = 6·74, p < 0.0001). Heterogeneity of effects between studies did not appear to be substantial (I2 = 17.43%; p = 0·21).
Fig. 5.
The association between home practice and intervention outcomes across 28 studies.
Subgroup analyses showed no evidence of a difference in the relationship between home practice and outcomes across clinical (n = 22, r = 0·25, 95% CI 0·17–0·34) and nonclinical populations (n = 5, r = 0·29, 95% CI 0·07–0·48, Z = 2·5, Q = ·09, df = 1, p = 0·76). There was also no evidence of an overall significant difference in the home practice/outcome association across studies grouped by intervention outcome type (Q = 5·52, df = 2, p = 0·17). However, the majority of available studies reported on primary psychological outcomes (n = 19, r = 0·3, 95% CI 0·21 -·38, Z = 6·37, p < 0·0001), while a smaller number reported on physical outcomes (n = 6, r = 0·, 95% CI -0·001–0·31, Z = 1·95, p = 0·05). Only two studies reported on the association between SHFP and ‘mixed’ (quality of life) intervention outcomes and neither study reported a significant association between practice and outcome (r = 0·13, 95% CI 0·17–0·411, Z = ·85, p = 0·39). There was also no evidence of an effect of study design, comparing RCTs (n = 15, r = ·26, 95% CI 0·143–0·376, Z = 4·21, p < 0·0001), non-randomized trials (n = 4, r = ·19, 95% CI -0·04–0·4, Z = 1·6, p = 0·1), and before and after studies (n = 8, r = ·29, 95% CI 1·48–0·42, Z = 3·9, p < 0·0001; Q = 0·61, df = 2, p = 0·74).
Restricting analysis to RCTs only (n = 15), the association between home practice and outcomes remained small, but significant (r = 0·26, 95% CI 0·143–0·376, Z = 4·21, p < 0·0001). Finally, a meta-regression was performed to examine whether the strength of the association between home practice and outcomes differed dependent on the mean amount of home practice. There was no evidence for a linear impact of mean home practice on the practice-outcome association (Beta = −0·0004, SE = ·003, Z = 0·16, p = 0·86). We found no evidence for a publication bias for studies examining home practice and outcome associations (Supplementary Materials, Fig. 2).
Finally, for the 10 studies with reduced home practice requirements, two reported that there was no significant association between practice and outcomes, but did not report statistical details (Astin, 1997, n = 12; Kimbrough et al., 2010; n = 23). Another study found no significant relationships between home practice completion and post treatment changes in self-reported loneliness (Creswell et al., 2012, r (13) = 0.35, p = 0.22). The remaining 7 studies did not report on the association between home practice and outcomes.
12. Discussion
The available evidence suggests that in standard format MBCT and MBSR, participants complete about 60% of assigned formal home practice, where it is recorded and reported. This equates to around 30 min per day, six days a week and represents a substantial time commitment, albeit less than suggested in standard intervention formats (Kabat Zinn, 1990, Segal et al., 2013). We found no evidence for significant differences in practice completion across clinical and nonclinical participant groups nor between studies targeting psychological and physical health outcomes. We found evidence for a small, significant association between practice and outcomes across the 28 standard format studies. This significant association held across clinical and nonclinical participant groups and across physical and psychological treatment outcomes.
However, there was substantial heterogeneity associated with the pooled estimates of participants' home practice. Even within a priori subgroups, heterogeneity was high and we could not readily identify its source using indices of study quality or study design. Within individual studies, participants’ practice reports were variable, as were reports across studies. This suggests a need for a greater understanding of the individual-level factors affecting reports of mindfulness home practice, as well as study-level factors. We also examined the small body of studies with reduced home practice requirements, which comprised MBSR interventions only. We found that participants in these studies practiced significantly less overall than those asked to practice for the standard amount of time (i.e., 151 min vs. 174 mins per week).
Participants’ perception of treatment plausibility and expectancy of positive outcome have been shown to have a small but significant impact on treatment outcomes for psychological therapies more generally (meta-analysis; Constantino, Arnkoff, Glass, Ametrano, & Smith, 2011). However, such effects have not been clearly established for MBCT or MBSR participants (Crane et al., 2014, but see also; Snippe et al., 2015). Participant personality traits such as compliance or conscientiousness may also be important. Other factors implicated in CBT homework completion, namely motivation to change (Helbig & Fehm, 2004), teacher competence and reviewing of home assignments (Weck, Richtberg, Esch, Höfling, & Stangier, 2013) might be investigated in MBCT/MBSR. Study level factors including therapist adherence to MBSR or MBCT protocols, or indeed an interaction between these factors, might also be relevant. We could not examine these factors because of infrequent investigation.
12.1. The association between home practice and outcomes
We found a small to moderate association between participants' home practice and treatment outcome, where participants are asked to practice for the standard amount of time. There was no evidence of heterogeneity of effects. The strength of the association was similar to that reported in meta-analyses of CBT homework assignments and outcomes (Kazantzis et al., 2010, Mausbach et al., 2010). This finding suggests that there is value in supporting and encouraging participants’ home practice in MBCT and MBSR. Mindfulness practice is often conceptualized as a form of mental training (Tang, Hölzel, & Posner, 2015) and like physical training, greater practice may confer greater benefit. Given the small size of the practice and outcome association, exploration of additional participant engagement variables, such as class attendance, alongside home practice, may be fruitful. Finally, there was insufficient data from studies with reduced home practice requirements to address the practice/outcome question.
These findings should also be considered in relation to the small number of dismantling trials that have tested whether mindfulness is the “active ingredient” in MBSR (MacCoon et al., 2012) and MBCT (Williams et al., 2014). For MBSR, a trial with a nonclinical participant sample suggests that it is no more effective than an active control condition (health enhancement programme) in improving well-being indices. For MBCT, evidence suggests that it is more beneficial for patients with recurrent depression at increased vulnerability (history of childhood trauma) than an active control condition. However, there was no significant advantage for MBCT over the active treatment in the overall patient sample. Overall, these trials raise questions about the active components of treatment, but they do not directly test the importance of home practice itself in MBSR or MBCT.
12.2. Limitations
While our findings suggest that home practice is clinically important, there are a number of caveats. We found some evidence of underreporting of participants' home practice, with lower practice amounts less likely to be reported. However, we did not find any evidence of a publication bias for studies reporting on the association between practice and outcomes. Nonetheless, it should be noted that the majority of studies of MBSR/MBCT do not report on participants' home practice. Furthermore, the home practice reports examined here were from participants' who had completed the 8-week interventions. This review draws attention to the need to record and report where possible, home practice from all participants (completers and non-completers). This would provide a broader understanding of participants’ behavior outside of class time and its impact on outcomes.
The quality of the evidence included here is another limitation. We did not restrict inclusion based on study design because the aim was to examine home practice completion rather than the efficacy of MBSR or MBCT as interventions. Nevertheless, many of the included RCTs were at risk for bias from lack of outcome assessment blinding, allocation concealment, high attrition and lack of intention-to-treat analysis. These sources of bias have been identified in previous systematic reviews of RCTs of meditation interventions generally (e.g., Goyal et al., 2014).
There is much potential for improved methodology in studying home practice and outcomes in MBSR and MBCT. Current estimates of mindfulness practice rely on participants’ retrospective self-reports, but it is unclear how this relates to their actual practice behavior. Related to this, included studies typically reported asking participants to complete daily diaries or weekly forms. We found no differences between mindfulness practice recorded using either form type. However, it is difficult to ascertain the actual frequency with which participants completed these forms.
Furthermore, few studies provided details on the specific forms filled in by participants (e.g., form by Crane et al., 2014). Development and widespread use of standard home practice reporting forms would be helpful in ensuring consistency in participant experience and in reporting across studies. Future use of smartphone apps, text message reminders to fill in practice diaries, or online portals, may support participants in recording home practice. In addition, this would provide researchers with a means to assess the frequency and timing of practice recording. Smartphone apps may be particularly valuable as a method of recording informal practices in real-time (e.g., when participant undertake unscheduled ‘additional breathing spaces’ in response to stressful events, and ‘noticings’ – bringing mindful awareness to moments in daily life). Future studies may also examine whether specific practices (e.g., body scan, yoga) are more robustly correlated with treatment outcomes than others.
Furthermore, participants' practice ‘quality’ may be crucial (Del Re et al., 2013), but again this presents an inherent measurement challenge. We also did not examine informal practice, which has been investigated in two recent studies but was not found to affect intervention outcomes (Crane et al., 2014, Hawley et al., 2014). However, as has been widely discussed, informal practice is more challenging to quantify when compared with formal practice, which has a more standard duration with audio guidance. Teacher competence in reviewing home practice, and providing formative feedback, may be particularly important in obtaining insights into practice behavior, in increasing engagement with practice, and indeed in increasing the beneficial effects of practice on outcome.
A further limitation of the current evidence is that studies investigating the formal home practice and outcome association are correlational. An arguably better strategy to investigate whether home practice is necessary for positive treatment outcomes might involve randomly assigning participants to ‘MBSR/MBCT as usual’ compared with a ‘no formal practice’ format. Finally, we chose to focus our analysis on studies reporting outcomes immediately post intervention and the majority of MBCT/MBSR studies to date have been over a relatively short time frame. This allowed us to synthesize a reasonably large body of studies. However, MBCT has been shown to protect against relapse to depression (Kuyken et al., 2015), an outcome that requires longer assessment periods. An important future avenue therefore will be to examine practice, and its continuation beyond the eight-week intervention, and longer-term effects.
Author contributions
All authors contributed to the study design and writing of the manuscript. CP and LP performed the literature searches and data extraction. CP performed the data analysis and CP and CC performed the data interpretation.
Acknowledgements
CP received funding from TrygFonden Charitable Foundation (ID: 117642). WK's research is funded by the Wellcome Trust (104908/Z/14/Z & WT104908MA) & NIHR, Health Services and Delivery Research Programme, (12/64/0412). CC is affiliated with the University of Oxford Mindfulness Centre and is funded by the Wellcome Trust, 104908/Z/14/Z (PI Professor Mark Williams).
Footnotes
The average SD from the included studies was 31.7%.
Data provided by authors when contacted.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.brat.2017.05.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Astin J.A. Stress reduction through mindfulness meditation. Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychotherapy and Psychosomatics. 1997;66(2):97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- Baer R.A., Carmody J., Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2012;68:755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Bakker J.M., Lieverse R., Menne-Lothmann C., Viechtbauer W., Pishva E., Kenis G.…Wichers M. Therapygenetics in mindfulness-based cognitive therapy: Do genes have an impact on therapy-induced change in real-life positive affective experiences. Transl Psychiatry. 2014:4. doi: 10.1038/tp.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhofer T., Crane C., Hargus E., Amarasinghe M., Winder R., Williams J.M.G. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behaviour Research and Therapy. 2009;47:366–373. doi: 10.1016/j.brat.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blom K., Baker B., How M., Dai M., Irvine J., Abbey S. Hypertension analysis of stress reduction using mindfulness meditation and yoga: Results from the HARMONY randomized controlled trial. American Journal of Hypertension. 2014;27:122–129. doi: 10.1093/ajh/hpt134. [DOI] [PubMed] [Google Scholar]
- Bluth K., Gaylord S., Nguyen K., Bunevicius A., Girdler S. Mindfulness-based stress reduction as a promising intervention for amelioration of premenstrual dysphoric disorder symptoms. Mindfulness. 2015;6:1292–1302. doi: 10.1007/s12671-015-0397-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. 2009. Introduction to meta-analysis. [Google Scholar]
- Britton W.B., Haynes P.L., Fridel K.W., Bootzin R.R. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosomatic Medicine. 2010;72:539–548. doi: 10.1097/PSY.0b013e3181dc1bad. [DOI] [PubMed] [Google Scholar]
- Britton W.B., Haynes P.L., Fridel K.W., Bootzin R.R. Mindfulness-based cognitive therapy improves polysomnographic and subjective sleep profiles in antidepressant users with sleep complaints. Psychother Psychosom. 2012;81:296–304. doi: 10.1159/000332755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell T.S., Labelle L.E., Bacon S.L., Faris P., Carlson L.E. Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: A waitlist-controlled study. Journal of Behavioral Medicine. 2012;35:262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- Carlson L.E., Speca M., Patel K.D., Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- Carmody J., Baer R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Carmody J.F., Crawford S., Salmoirago-Blotcher E., Leung K., Churchill L., Olendzki N. Mindfulness training for coping with hot flashes: Results of a randomized trial. Menopause. 2011;18:611–620. doi: 10.1097/gme.0b013e318204a05c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J., Reed G., Kristeller J., Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of Psychosomatic Research. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Centre for Reviews and Dissemination . 2014. Prospero: International prospective register of systematic reviews. [Google Scholar]
- Cole M.A., Muir J.J., Gans J.J., Shin L.M., D'Esposito M., Harel B.T. Simultaneous treatment of neurocognitive and psychiatric symptoms in veterans with post-traumatic stress disorder and history of mild traumatic brain injury: A pilot study of mindfulness-based stress reduction. Military Medicine. 2015;180:956–963. doi: 10.7205/MILMED-D-14-00581. [DOI] [PubMed] [Google Scholar]
- Collard P., Avny N., Boniwell I. Teaching Mindfulness Based Cognitive Therapy (MBCT) to students: The effects of MBCT on the levels of Mindfulness and Subjective Well-Being. Counselling Psychology Quarterly. 2008;21:323–336. [Google Scholar]
- Constantino M.J., Arnkoff D.B., Glass C.R., Ametrano R.M., Smith J.Z. Expectations. Journal of Clinical Psychology. 2011;67:184–192. doi: 10.1002/jclp.20754. [DOI] [PubMed] [Google Scholar]
- Crane C., Crane R.S., Eames C., Fennell M.J., Silverton S., Williams J.M. The effects of amount of home meditation practice in Mindfulness Based Cognitive Therapy on hazard of relapse to depression in the Staying Well after Depression Trial. Behaviour Research and Therapy. 2014;63:17–24. doi: 10.1016/j.brat.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J.D., Irwin M.R., Burklund L.J., Lieberman M.D., Arevalo J.M.G., Ma J.…Cole S.W. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain, Behavior, and Immunity. 2012;26(7):1095–1101. doi: 10.1016/j.bbi.2012.07.006. http://dx.doi.org/10.1016/j.bbi.2012.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day M.A., Thorn B.E., Ward L.C., Rubin N., Hickman S.D., Scogin F. Mindfulness-based cognitive therapy for the treatment of headache pain: A pilot study. Clinical Journal of Pain. 2014;30:152–161. doi: 10.1097/AJP.0b013e318287a1dc. [DOI] [PubMed] [Google Scholar]
- Del Re A.C., Flückiger C., Goldberg S.B., Hoyt W.T. Monitoring mindfulness practice quality: An important consideration in mindfulness practice. Psychotherapy Research. 2013;23(1):54–66. doi: 10.1080/10503307.2012.729275. [DOI] [PubMed] [Google Scholar]
- DiMatteo M.R. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Eisendrath S.J., Gillung E., Delucchi K., Mathalon D.H., Yang T.T., Satre D.D. A preliminary Study: Efficacy of mindfulness-based cognitive therapy versus sertraline as first-line treatments for major depressive disorder. Mindfulness. 2015;6:475–482. doi: 10.1007/s12671-014-0280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb N.A., Segal Z.V., Anderson A.K. Mindfulness meditation training alters cortical representations of interoceptive attention. Social Cognitive and Affective Neuroscience. 2013;8:15–26. doi: 10.1093/scan/nss066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley E., Baillie A., Huxter M., Price M., Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. Journal of Consulting & Clinical Psychology. 2010;78:72–79. doi: 10.1037/a0017566. [DOI] [PubMed] [Google Scholar]
- Furukawa T.A., Barbui C., Cipriani A., Brambilla P., Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology. 2006;59(1):7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Geschwind N.P.F.H.M.v.O.J.W.M. Efficacy of mindfulness-based cognitive therapy in relation to prior history of depression: Randomised controlled trial. British Journal of Psychiatry. 2012;201:320–325. doi: 10.1192/bjp.bp.111.104851. [DOI] [PubMed] [Google Scholar]
- Gilpin A.R. Table for conversion of Kendall's Tau to Spearman's Rho within the context of measures of magnitude of effect for meta-analysis. Educational and Psychological Assessment. 1993;53:87–92. [Google Scholar]
- Goldsmith R.E., Gerhart J.I., Chesney S.A., Burns J.W., Kleinman B., Hood M.M. Mindfulness-based stress reduction for posttraumatic stress symptoms: Building acceptance and decreasing shame. Journal of Evidence-based Complementary & Alternative Medicine. 2014;19:227–234. doi: 10.1177/2156587214533703. [DOI] [PubMed] [Google Scholar]
- Goyal M., Singh S., Sibinga E.M.S., Gould N.F., Rowland-Seymour A., Sharma R.…Haythornthwaite J.A. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C.R., Kreitzer M.J., Reilly-Spong M., Wall M., Winbush N.Y., Patterson R. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: A randomized controlled clinical trial. Explore (NY) 2011;7:76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley L.L., Schwartz D., Bieling P.J., Irving J., Corcoran K., Farb N.A.S. Mindfulness practice, rumination and clinical outcome in mindfulness-based treatment. Cognitive Therapy and Research. 2014;38:1–9. [Google Scholar]
- Helbig S., Fehm L. Problems with homework in CBT: Rare exception or rather frequent? Behavioural and Cognitive Psychotherapy. 2004;32:291–301. [Google Scholar]
- Higgins J.P., Green S. 2008. Cochrane Handbook for systematic reviews of Interventions: Cochrane book series. [Google Scholar]
- Hoffman C.J., Ersser S.J., Hopkinson J.B., Nicholls P.G., Harrington J.E., Thomas P.W. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology. 2012;30:1335–1342. doi: 10.1200/JCO.2010.34.0331. [DOI] [PubMed] [Google Scholar]
- Hölzel B.K., Carmody J., Vangel M., Congleton C., Yerramsetti S.M., Gard T. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research - Neuroimaging. 2011;191:36–43. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou R.J., Wong S.Y.S., Yip B.H.K., Hung A.T.F., Lo H.H.M., Chan P.H.S. The effects of mindfulness-based stress reduction program on the mental health of family caregivers: A randomized controlled trial. Psychotherapy and Psychosomatics. 2013;83:45–53. doi: 10.1159/000353278. [DOI] [PubMed] [Google Scholar]
- Jazaieri H., Goldin P.R., Werner K., Ziv M., Gross J.J. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. Journal of Clinical Psychology. 2012;68:715–731. doi: 10.1002/jclp.21863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen C.G., Vangkilde S., Frokjaer V., Hasselbalch S.G. Mindfulness training affects attention-Or is it attentional effort? Journal of Experimental Psychology: General. 2012;141:106–123. doi: 10.1037/a0024931. [DOI] [PubMed] [Google Scholar]
- Johansson B., Bjuhr H., Karlsson M., Karlsson J.O., Rönnbäck L. Mindfulness-based stress reduction (MBSR) delivered live on the internet to individuals suffering from mental fatigue after an acquired brain injury. Mindfulness. 2015;6:1356–1365. [Google Scholar]
- Kabat Zinn J. Bantam Books; 1990. Full catastrophe Living: Using the wisdom of your body and mind to face stress, pain and illness. [Google Scholar]
- Kazantzis N., Whittington C., Dattilio F. Meta-analysis of homework effects in cognitive and behavioral therapy: A replication and extension. Clinical Psychology: Science and Practice. 2010;17:144–156. [Google Scholar]
- Kimbrough E., Magyari T., Langenberg P., Chesney M., Berman B. Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology. 2010;66(1):17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- Kluepfel L., Ward T., Yehuda R., Dimoulas E., Smith A., Daly K. The evaluation of mindfulness-based stress reduction for veterans with mental health conditions. Journal of Holistic Nursing. 2013;31:248–255. doi: 10.1177/0898010113495975. [DOI] [PubMed] [Google Scholar]
- Kuyken W., Hayes R., Barrett B., Byng R., Dalgleish T., Kessler D. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): A randomised controlled trial. Lancet (London, England) 2015;386:63–73. doi: 10.1016/S0140-6736(14)62222-4. [DOI] [PubMed] [Google Scholar]
- Labelle L.E., Lawlor-Savage L., Campbell T.S., Faris P., Carlson L.E. Does self-report mindfulness mediate the effect of Mindfulness-Based Stress Reduction (MBSR) on spirituality and posttraumatic growth in cancer patients? Journal of Positive Psychology. 2015;10:153–166. [Google Scholar]
- MacCoon D.G., Imel Z.E., Rosenkranz M.A., Sheftel J.G., Weng H.Y., Sullivan J.C. Vol. 50. 2012. pp. 3–12. (The validation of an active control intervention for mindfulness based stress reduction (MBSR)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach B.T., Moore R., Roesch S., Cardenas V., Patterson T.L. The relationship between homework compliance and therapy outcomes: An updated meta-analysis. Cognitive Therapy and Research. 2010;34:429–438. doi: 10.1007/s10608-010-9297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., McKinnon A., Kuyken W., Gilbody S., Dalgleish T. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review. 2015;40:91–110. doi: 10.1016/j.cpr.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Nyklicek I., Kuijpers K.F. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine. 2008;35:331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.C., Manber R., Segal Z., Xia Y., Shapiro S., Wyatt J.K. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37:1553–1563. doi: 10.5665/sleep.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterberg L., Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Parkin L., Morgan R., Rosselli A., Howard M., Sheppard A., Evans D. Exploring the relationship between mindfulness and cardiac perception. Mindfulness. 2014;5:298–313. [Google Scholar]
- Perich T., Manicavasagar V., Mitchell P.B., Ball J.R. The association between meditation practice and treatment outcome in Mindfulness-based Cognitive Therapy for bipolar disorder. Behaviour Research and Therapy. 2013;51:338–343. doi: 10.1016/j.brat.2013.03.006. [DOI] [PubMed] [Google Scholar]
- Peterson R.A., Brown S.P. On the use of beta coefficients in meta-analysis. Journal of Applied Psychology. 2005;90:175–181. doi: 10.1037/0021-9010.90.1.175. [DOI] [PubMed] [Google Scholar]
- Pickut B., Vanneste S., Hirsch M.A., Van Hecke W., Kerckhofs E., Marien P. Mindfulness training among individuals with Parkinson's Disease: Neurobehavioral effects. Parkinson’s Disease. 2015;2015:816404. doi: 10.1155/2015/816404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan E.K., Baumgarten M., Langenberg P., Handwerger B., Gilpin A.K., Magyari T. Effect of mindfulness-based stress reduction in rheumatoid arthritis patients. Arthritis & Rheumatology. 2007;57:1134–1142. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- Prince M., Patel V., Saxena S., Maj M., Maselko J., Phillips M.R. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Ramel W., Goldin P.R., Carmona P.E., McQuaid J.R. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research. 2004;28:433–455. [Google Scholar]
- Rimes K.A., Wingrove J. Pilot study of mindfulness-based cognitive therapy for trainee clinical psychologists. Behavioural and Cognitive Psychotherapy. 2011;39:235–241. doi: 10.1017/S1352465810000731. [DOI] [PubMed] [Google Scholar]
- Roland L.T., Lenze E.J., Hardin F.M., Kallogjeri D., Nicklaus J., Wineland A.M. Effects of mindfulness based stress reduction therapy on subjective bother and neural connectivity in chronic tinnitus. Otolaryngology–head and Neck Surgery: Official Journal of American Academy of Otolaryngology-head and Neck Surgery. 2015;152:919–926. doi: 10.1177/0194599815571556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig S., Reibel D.K., Greeson J.M., Edman J.S., Jasser S.A., McMearty K.D., Goldstein B.J. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: A pilot study. Alternative Therapies in Health and Medicine. 2007;13:36–38. [PubMed] [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford Press; 2012. Mindfulness-based cognitive therapy for depression. [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford Press; 2013. Mindfulness-based cognitive therapy for depression. [Google Scholar]
- Shallcross A.J., Gross J.J., Visvanathan P.D., Kumar N., Palfrey A., Ford B.Q. Relapse prevention in major depressive disorder: Mindfulness-based cognitive therapy versus an active control condition. Journal of Consulting and Clinical Psychology. 2015;83:964–975. doi: 10.1037/ccp0000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro S.L., Brown K.W., Biegel G.M. Teaching self-care to caregivers: Effects of mindfulness-based stress reduction on the mental health of therapists in training. Training and Education in Professional Psychology. 2007;1:105–115. [Google Scholar]
- Shapiro S.L., Jazaieri H., Goldin P.R. Mindfulness-based stress reduction effects on moral reasoning and decision making. Journal of Positive Psychology. 2012;7:504–515. [Google Scholar]
- Shapiro S.L., Oman D., Thoresen C.E., Plante T.G., Flinders T. Cultivating mindfulness: Effects on well-being. Journal of Clinical Psychology. 2008;64:840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- Snippe E., Schroevers M.J., Annika Tovote K., Sanderman R., Emmelkamp P.M.G., Fleer J. Patients' outcome expectations matter in psychological interventions for patients with diabetes and comorbid depressive symptoms. Cognitive Therapy and Research. 2015;39:307–317. doi: 10.1007/s10608-014-9667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y.Y., Hölzel B.K., Posner M.I. The neuroscience of mindfulness meditation. Nature Reviews Neuroscience. 2015;16:213–225. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- Terrin N., Schmid C.H., Lau J., Olkin I. Adjusting for publication bias in the presence of heterogeneity. Statistics in Medicine. 2003;22:2113–2126. doi: 10.1002/sim.1461. [DOI] [PubMed] [Google Scholar]
- Vettese L.C., Toneatto T., Stea J.N., Nguyen L., Wang J.J. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy. 2009;23:198–225. [Google Scholar]
- Vøllestad J., Sivertsen B., Nielsen G.H. Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behaviour Research and Therapy. 2011;49:281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Walach H., Nord E., Zier C., Dietz-Waschkowski B., Kersig S., Schupbach H. Mindfulness-based stress reduction as a method for personnel development: A pilot evaluation. International Journal of Stress Management. 2007;14(2):188–198. http://dx.doi.org/10.1037/1072-5245.14.2.188 [Google Scholar]
- Weck F., Richtberg S., Esch S., Höfling V., Stangier U. The relationship between therapist competence and homework compliance in maintenance cognitive therapy for recurrent Depression: Secondary analysis of a randomized trial. Behavior Therapy. 2013;44:162–172. doi: 10.1016/j.beth.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Wells R.E., Burch R., Paulsen R.H., Wayne P.M., Houle T.T., Loder E. Meditation for migraines: A pilot randomized controlled trial. Headache. 2014;54(9):1484–1495. doi: 10.1111/head.12420. [DOI] [PubMed] [Google Scholar]
- Wells R.E., Yeh G.Y., Kerr C.E., Wolkin J., Davis R.B., Tan Y.…Kong J. Meditation's impact on default mode network and hippocampus in mild cognitive impairment: Pilot study. Neuroscience Letters. 2013;556:15–19. doi: 10.1016/j.neulet.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitebird R.R., Kreitzer M., Crain A.L., Lewis B.A., Hanson L.R., Enstad C.J. Mindfulness-based stress reduction for family caregivers: A randomized controlled trial. The Gerontologist. 2013;53:676–686. doi: 10.1093/geront/gns126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J.M.G., Crane C., Barnhofer T., Brennan K., Duggan D.S., Fennell M.J.V.…Russell I.T. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82(2):275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.Y., Chan F.W., Wong R.L., Chu M., Lam Y.K., Mercer S.W. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: A randomized comparative trial. The Clinical Journal of Pain. 2011;27:724–734. doi: 10.1097/AJP.0b013e3182183c6e. [DOI] [PubMed] [Google Scholar]
- Zernicke K.A., Campbell T.S., Blustein P.K., Fung T.S., Johnson J.A., Bacon S.L. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: A randomized wait-list controlled trial. International Journal of Behavioral Medicine. 2013;20:385–396. doi: 10.1007/s12529-012-9241-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.