Growing research links posttraumatic stress disorder (PTSD) to a range of cardiometabolic conditions, including metabolic syndrome, heart disease, stroke, and type 2 diabetes (Heppner et al., 2009, Koenen et al., 2017, Roberts et al., 2015, Sumner et al., 2015, Wolf et al., 2016). A number of behavioral (e.g., poor diet, physical inactivity, cigarette smoking, substance use) and physiological (e.g., dysregulation of biological stress response systems, such as the hypothalamic-pituitary-adrenal axis, autonomic nervous system, and immune system) pathways have been proposed to underlie associations between PTSD and cardiometabolic risk (Dedert et al., 2010, Koenen et al., 2017, van Liempt et al., 2013; Wentworth et al., 2013). Additionally, overlapping genetic factors may predispose individuals to both PTSD and cardiometabolic disease. Initial evidence for shared genetic effects across PTSD and cardiometabolic traits comes from studies based on twin designs (Vaccarino et al., 2014, Vaccarino et al., 2013) and candidate gene approaches (Pollard et al., 2016). However, to date, research has not examined the genetic overlap of PTSD and cardiometabolic disease using a genome-wide design.
Recent developments in genetic computational methods now permit the estimation of genetic correlations between complex traits from genome-wide association study (GWAS) summary statistics, referred to as cross-trait LD score regression (LDSR) (Bulik-Sullivan et al., 2015). This cross-trait LDSR approach can be applied flexibly by utilizing summary statistics as input (Bulik-Sullivan et al., 2015). In contrast, other methods designed to identify shared genetic effects (i.e., polygenic scores and restricted maximum likelihood) require individual genotype data, which often cannot be released due to data sharing restrictions. Another advantage of the LDSR method is that it is not biased by sample overlap across studies (Bulik-Sullivan et al., 2015). The LDSR approach also incorporates the effects of all SNPs, including those that do not reach genome-wide significance, thereby improving the accuracy and power of genetic prediction (Dudbridge, 2016). However, one limitation of this method is that it can only be used with samples without recent admixture and for whom suitable large-scale genetic data resources are available. Given these restrictions, it can only be applied to European ancestry (EA) samples, and not African American or Latino populations, at this time.
The Psychiatric Genomics Consortium (PGC)-PTSD working group has been leading efforts to identify genetic risk variants associated with PTSD (Logue et al., 2015), and the first meta-analysis of PTSD GWASs (N=20,070) has been recently completed by this group (Duncan et al., 2017). In the present study, we used summary statistics from the PGC-PTSD meta-analysis of Duncan and colleagues (2017) to conduct the first GWAS-based investigation of potential genetic overlap between PTSD and cardiometabolic traits.
Methods
Cross-trait LDSR (Bulik-Sullivan et al., 2015) was used to estimate genetic correlations between PTSD and coronary artery disease (CAD), anthropometric traits (i.e., body mass index [BMI], waist circumference), glycemic traits (i.e., fasting glucose, fasting insulin, hemoglobin A1C [HbA1C]), type 2 diabetes, and lipids (i.e., low-density lipoprotein [LDL] cholesterol, high-density lipoprotein [HDL] cholesterol, total cholesterol, triglycerides). These traits were selected because of their relevance to cardiometabolic disease, which has been robustly associated with PTSD, as described above (see Koenen et al., 2017, for a review). Analyses were conducted on LD Hub (Zheng et al., 2016), a centralized database of GWAS summary statistics that automates the LDSR pipeline (http://ldsc.broadinstitute.org/). The PGC-PTSD GWAS meta-analysis summary statistics used were based on 9,542 EA participants (25% PTSD cases) that were collected across 9 studies (see Duncan et al., 2017, for study and sample details). These summary statistics were uploaded to LD Hub for genetic correlation with cardiometabolic traits. All cardiometabolic trait GWAS meta-analyses were based on predominantly EA ancestry samples (see Acknowledgements for GWAS study citations). In order to filter out rare or poorly imputed variants, we selected SNPs with a minor allele frequency >0.05 and an imputation information value >0.90. All procedures contributing to this work complied with ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Results
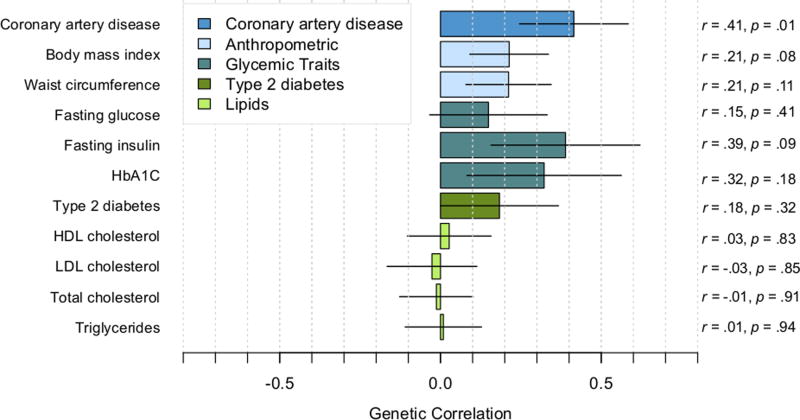
Small to moderate positive correlations were observed between PTSD with CAD, anthropometric traits, and glycemic traits (see Figure 1 for correlations, standard errors, and p-values). The correlation of PTSD with CAD was significant (p=.01), and the correlations of PTSD with BMI and fasting insulin were nominally significant (ps<.10). However, correlations did not survive correction for multiple testing based on either a Bonferroni correction (corrected p-value threshold=.005) or a less stringent correction method (Li and Ji, 2005) for testing multiple correlated traits (corrected p-value threshold=.006). As expected, the cardiometabolic traits had significant genetic correlations with each other. For example, correlations among the top cardiometabolic traits that were associated with PTSD were as follows: CAD-BMI, r=.22; CAD-fasting insulin: r=.27; BMI-fasting insulin: r=.57 (ps<.0001).
Figure 1.
Genetic correlations between posttraumatic stress disorder (PTSD) and cardiometabolic traits. Correlations estimated with cross-trait LD score regression. Lines indicate standard errors.
Discussion
We present the first-ever genetic correlations between PTSD and a range of cardiometabolic outcomes based on GWAS summary statistics. Findings suggested that, in EA individuals, there is potential for shared genetic contributions to PTSD and several cardiometabolic traits, including CAD, BMI, and fasting insulin. These results are indicative of shared genetic risk and consistent with epidemiologic evidence linking PTSD to elevated obesity, cardiovascular, and metabolic risk (Heppner et al., 2009, Kubzansky et al., 2014, Sumner et al., 2015, Wolf et al., 2016). Importantly, the findings from the present research may also help to explain previously observed bidirectional associations between PTSD and cardiometabolic outcomes in the literature (Edmondson et al., 2012, Sumner et al., 2015). Our findings are also consistent with twin and candidate gene research suggesting that there may be genetic linkage between PTSD, cardiovascular disease, and type 2 diabetes (Pollard et al., 2016, Vaccarino et al., 2014, Vaccarino et al., 2013). Although these are promising preliminary results, we note that cross-trait LDSR analyses do not address subgroup-specific effects (e.g., sex-specific effects), and these methods can only be currently applied to EA samples. Furthermore, even though our PTSD GWAS meta-analysis is the largest (and presumably best-powered) to date, it was still underpowered to detect specific risk loci. Better-powered PTSD analyses in the future will also allow for better-powered genetic correlation analyses. Additionally, the current z-score for overall heritability of PTSD was 3 (Duncan et al., 2017), and a heritability z-score greater than 4 has been recommended for testing multiple genetic correlation estimates (Zheng et al., 2016). We will continue to explore these associations as the PGC-PTSD grows and incorporates more samples in future meta-analyses. Nonetheless, we believe that these results provide initial support that the growing number of associations of PTSD and cardiometabolic diseases reported in the literature may be due, in part, to shared genetic contributions.
Acknowledgments
Financial Support: This work was supported by the National Institutes of Health (JAS, K01HL130650), (CN, R01MH106595), (EJW, R03AG051877), (ABA, K02AA023239); and the United States (US) Department of Veterans Affairs Clinical Sciences R&D (CSRD) Service (EJW, Merit Review Award Number I01 CX-001276-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Veterans Affairs, the National Institutes of Health, or the US Government.
We gratefully acknowledge the following GWASs that contributed data to the current study: PTSD (PGC-PTSD; Duncan et al., 2017); CAD (CARDIoGRAM; PMID 26343387); type 2 diabetes (DIAGRAM; PMID 22885922); BMI (GIANT; PMID 20935630); waist circumference (GIANT; PMID 25673412); fasting glucose and insulin (MAGIC; PMID 22581228); HbA1C (MAGIC; PMID 20858683); LDL, HDL, and total cholesterol and triglycerides (GLGC; PMID 20686565). We also acknowledge Jie Zheng for his assistance with LD Hub.
Footnotes
Conflict of Interest
None
References
- Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, ReproGen Consortium, Psychiatric Genomics Consortium, Genetic Consortium for Anorexia Nervosa of the Wellcome Trust Case Control Consortium. Duncan L, Perry JR, Patterson N, Robinson EB, Daly MJ, Price AL, Neale BM. An atlas of genetic correlations across human diseases and traits. Nature Genetics. 2015;47:1236–1241. doi: 10.1038/ng.3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Annals of Behavioral Medicine. 2010;39:61–78. doi: 10.1007/s12160-010-9165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudbridge F. Polygenic epidemiology. Genetic Epidemiology. 2016;40:268–272. doi: 10.1002/gepi.21966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan LE, Ratanatharathorn A, Aiello AE, Almli LM, Amstadter AB, Ashley-Koch AE, Baker DG, Beckham JC, Bierut Lj, Bisson J, Bradley B, Chen CY, Dalvie S, Farrer La, Galea S, Garrett ME, Gelernter JE, Guffanti G, Hauser MA, Johnson EO, Kessler RC, Kimbrel NA, King A, Koen N, Kranzler HR, Logue MW, Maihofer AX, Martin AR, Miller MW, Morey RA, Nugent NR, Rice JP, Ripke S, Roberts AL, Saccone NL, Smoller JW, Stein DJ, Stein MB, Sumner JA, Uddin M, Ursano RJ, Wildman DE, Yehuda R, Zhao H, Daly MJ, Liberzon I, Ressler KJ, Nievergelt CM, Koenen KC. Largest GWAS of PTSD (N=20,070) yields genetic overlap with schizophrenia and sex differences in heritability. Molecular Psychiatry. 2017 doi: 10.1038/mp.2017.77. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS ONE. 2012;7:e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppner PS, Crawford EF, Haji UA, Afari N, Hauger RL, Dashevsky BA, Horn PS, Nunnink SE, Baker DG. The association of posttraumatic stress disorder and metabolic syndrome: a study of increased health risk in veterans. BMC Medicine. 2009;7:1. doi: 10.1186/1741-7015-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Sumner JA, Gilsanz P, Glymour MM, Ratanatharathorn A, Rimm EB, Roberts AL, Winning A, Kubzansky LD. Post-traumatic stress disorder and cardiometabolic disease: improving causal inference to inform practice. Psychological Medicine. 2017;47:209–225. doi: 10.1017/S0033291716002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, Bordelois P, Jun HJ, Roberts AL, Cerda M, Bluestone N, Koenen KC. The weight of traumatic stress: a prospective study of posttraumatic stress disorder symptoms and weight status in women. JAMA Psychiatry. 2014;71:44–51. doi: 10.1001/jamapsychiatry.2013.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Ji L. Adjusting multiple testing in multilocus analyses using the eigenvalues of a correlation matrix. Heredity. 2005;95:221–227. doi: 10.1038/sj.hdy.6800717. [DOI] [PubMed] [Google Scholar]
- Logue MW, Amstadter AB, Baker DG, Duncan L, Koenen KC, Liberzon I, Miller MW, Morey RA, Nievergelt CM, Ressler KJ, Smith AK, Smoller JW, Stein MB, Sumner JA, Uddin M. The Psychiatric Genomics Consortium Posttraumatic Stress Disorder Workgroup: posttraumatic stress disorder enters the age of large-scale genomic collaboration. Neuropsychopharmacology. 2015;40:2287–2297. doi: 10.1038/npp.2015.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard HB, Shivakumar C, Starr J, Eidelman O, Jacobowitz DM, Dalgard CL, Srivastava M, Wilkerson MD, Stein MB, Ursano RJ. “Soldier's heart”: a genetic basis for elevated cardiovascular disease risk associated with post-traumatic stress disorder. Frontiers in Molecular Neuroscience. 2016;9:87. doi: 10.3389/fnmol.2016.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Agnew-Blais JC, Spiegelman D, Kubzansky LD, Mason SM, Galea S, Hu FB, Rich-Edwards JW, Koenen KC. Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: a 22-year longitudinal study. JAMA Psychiatry. 2015;72:203–210. doi: 10.1001/jamapsychiatry.2014.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner JA, Kubzansky LD, Elkind MS, Roberts AL, Agnew-Blais J, Chen Q, Cerdá M, Rexrode KM, Rich-Edwards JW, Spiegelman D, Suglia SF, Rimm EB, Koenen KC. Trauma exposure and posttraumatic stress disorder symptoms predict onset of cardiovascular events in women. Circulation. 2015;132:251–259. doi: 10.1161/CIRCULATIONAHA.114.014492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccarino V, Goldberg J, Magruder KM, Forsberg CW, Friedman MJ, Litz BT, Heagerty PJ, Huang GD, Gleason TC, Smith NL. Posttraumatic stress disorder and incidence of type-2 diabetes: a prospective twin study. Journal of Psychiatric Research. 2014;56:158–164. doi: 10.1016/j.jpsychires.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccarino V, Goldberg J, Rooks C, Shah AJ, Veledar E, Faber TL, Votaw JR, Forsberg CW, Bremner JD. Post-traumatic stress disorder and incidence of coronary heart disease: a twin study. Journal of the American College of Cardiology. 2013;62:970–978. doi: 10.1016/j.jacc.2013.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Liempt S, Arends J, Cluitmans PJ, Westenberg HG, Kahn RS, Vermetten E. Sympathetic activity and hypothalamo-pituitary-adrenal axis activity during sleep in post-traumatic stress disorder: a study assessing polysomnography with simultaneous blood sampling. Psychoneuroendocrinology. 2013;38:155–165. doi: 10.1016/j.psyneuen.2012.05.015. [DOI] [PubMed] [Google Scholar]
- Wentworth BA, Stein MB, Redwine LS, Xue Y, Taub PR, Clopton P, Nayak KR, Maisel AS. Post-traumatic stress disorder: a fast track to premature cardiovascular disease? Cardiology in Review. 2013;21:16–22. doi: 10.1097/CRD.0b013e318265343b. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Bovin MJ, Green JD, Mitchell KS, Stoop TB, Barretto KM, Jackson CE, Lee LO, Fang SC, Trachtenberg F, Rosen RC, Keane TM, Marx BP. Longitudinal associations between post-traumatic stress disorder and metabolic syndrome severity. Psychological Medicine. 2016;46:2215–2226. doi: 10.1017/S0033291716000817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng J, Erzurumluoglu M, Elsworth B, Howe L, Haycock P, Hemani G, Tansey K, Laurin C, Early Genetics and Lifecourse Epidemiology (EAGLE) Eczema Consortium. Pourcain BS, Warrington N, Finucane HK, Price AL, Bulik-Sullivan BK, Anttila V, Paternoster L, Gaunt TR, Evans DM, Neale BM. LD Hub: a centralized database and web interface to perform LD score regression that maximizes the potential of summary level GWAS data for SNP heritability and genetic correlation analysis. Bioinformatics. 2016;33:272–279. doi: 10.1093/bioinformatics/btw613. [DOI] [PMC free article] [PubMed] [Google Scholar]