Abstract
Background
The aim of this study was to assess the efficacy of meaning-centered group psychotherapy for cancer survivors (MCGP-CS) to improve personal meaning, compared to supportive group psychotherapy (SGP) and care as usual (CAU).
Methods
A total of 170 cancer survivors were randomly assigned to one of the three study arms: MCGP-CS (n = 57), SGP (n = 56), CAU (n = 57). Primary outcome measure was Personal Meaning Profile (total score PMP). Secondary outcome measures were subscales of the PMP, psychological well-being (SPWB), posttraumatic growth (PTGI), mental adjustment to cancer (MAC), optimism (LOT-R), hopelessness (BHS), psychological distress (anxiety and depression, HADS), and quality of life (EORTC QLQ-C30). Outcome measures were assessed before randomization, post-intervention, after three and six months follow-up (FU).
Results
Linear mixed model analyses (intention-to-treat) showed significant differences between MCGP-CS, SGP and CAU on the total PMP score, and on (sub)scales of the PMP, SPWB, MAC, and HADS. Post-hoc analyses showed significantly stronger treatment effects of MCGP-CS compared to CAU on personal meaning (d=0.81), goal-orientedness (d=1.07), positive relations (d=0.59), purpose in life (d=0.69); fighting spirit (d=0.61) (post-intervention), helpless/hopeless (d=−0.87) (3 months FU); distress (d=−0.6) and depression (d=−0.38) (6 months FU). Significantly stronger effects of MCGP-CS compared to SGP were found on personal growth (d=0.57) (3 months FU), and environmental mastery (d=0.66) (6 months FU).
Conclusions
MCGP-CS is an effective intervention for cancer survivors to improve personal meaning, psychological well-being and mental adjustment to cancer in the short term, and to reduce psychological distress in the long run.
Introduction
Nowadays, more than half of the cancer patients can be treated successfully and become long-term survivors (Miller et al., 2016). Cancer survivors are at increased risk for psychological distress (Hoffman et al., 2009) and of the struggle with unmet psychological needs (Thewes et al., 2004; Santin et al., 2015). There is growing attention on the important role of sense of meaning in improving psychological well-being, and preventing or reducing psychological distress among cancer patients (LeMay and Wilson 2008). Up until now, research on meaning in cancer patients focused mostly on patients with advanced cancer, who might face death and meaning-related existential issues like demoralization and the desire for hastened death (McClain, Rosenfeld, and Breitbart 2003; Lethborg et al. 2007). However, sense of meaning is also an important issue in cancer survivors (Tomich and Helgeson 2002; van der Spek et al. 2013). The cancer diagnosis and the treatment with curative intent often imply fundamental uncertainties that patients have to deal with. These include the possible recurrence of the cancer, or negative (long-term) side-effects of the treatment, and are often accompanied by losses in different domains of life (i.e. physical, social, personal), which can challenge the experience of meaning in life (Lee 2008; van der Spek et al. 2013). According to Frankl (1955, 1959), suffering can trigger a need for meaning, and also an opportunity for growth and meaning. Breitbart (2014) describes that after the diagnosis of a potentially deadly illness like cancer “either one has a loss of sense of meaning and purpose in life, or one has sustained or even heightened sense of meaning, purpose, and peace, which allows one to value more profoundly the time remaining and positively appraise events”. Patients who experience more meaning, have higher psychological well-being, a more successful adjustment, better quality of life, and less psychological distress after the cancer diagnosis, than patients who experience little meaning in life (Jaarsma et al. 2007; Zika and Chamberlain 1992; Park et al. 2008).
Breitbart and colleagues (Breitbart et al. 2015) developed and evaluated meaning-centered group psychotherapy (MCGP), in order to meet the needs of patients with advanced cancer to help with meaning-making, improving spiritual well-being and reducing psychological distress. In a randomized controlled trial among 273 patients with advanced cancer, MCGP was compared to supportive group psychotherapy (SGP) (Breitbart et al. 2015). After controlling for sex, social support, religiosity and cognitive functioning, intention-to-treat analyses showed significant positive effects of MCGP on spiritual well-being, quality of life, hopelessness, depression, and desire for hastened death immediately after the intervention and at two months follow-up, with small to moderate effect sizes (−0.27 to −0.67).
Besides MCGP there are several other interventions that focus, at least partly, on sense of meaning in advanced cancer patients and that show varying degrees of positive effects (LeMay and Wilson 2008; Chochinov et al. 2011; Kissane et al. 2003; Lee et al. 2006; Spiegel and Spira 1991; Yalom and Greaves 1977). To our knowledge there are no evidence based meaning-focused interventions specifically targeting cancer survivors treated with curative intent. We adjusted the MCGP manual for cancer survivors (MCGP-CS) and subsequently conducted a feasibility study, which showed good acceptability, compliance, and satisfaction of MCGP among cancer survivors (van der Spek et al. 2014).
The aim of the present study was to assess the efficacy of MCGP-CS among cancer survivors to improve personal meaning. Based on earlier studies (Jaarsma et al. 2007; Lee et al. 2006; Zika and Chamberlain 1992; Breitbart et al. 2015; LeMay and Wilson 2008) we also expected a positive effect of MCGP-CS on psychological well-being, posttraumatic growth, adjustment to cancer, optimism, and quality of life. Moreover, we expected MCGP-CS to reduce hopelessness and psychological distress. In this randomized controlled trial (RCT), MCGP-CS was compared with SGP and with care as usual (CAU) to investigate the value of group psychotherapy, specifically focusing on personal meaning compared to regular supportive group psychotherapy and to standard care. We specifically expected that MCGP-CS would at least perform better than SGP on personal meaning. Efficacy was evaluated post-intervention and at three and six months follow-up, to obtain insight into a possible decay of the effect.
Methods
Study design and population
This study was a multi-center RCT with three study arms. The methods of this study have been described in a previously published study protocol (van der Spek, Vos, et al. 2014). The study protocol was approved by the Medical Ethics Committee of the Leiden University Medical Center and the trial was registered in the Netherlands Trial Register (NTR3571).
Eligible participants were adult cancer survivors who were diagnosed in the last five years, who were treated with curative intent, and who had completed their main treatment (i.e. surgery, radiotherapy, chemotherapy). Participants had to have an expressed need for psychological care and at least one psychosocial complaint (e.g. depressed mood, anxiety, coping issues, life questions, meaning-making problems, relationship problems).
Participants were excluded if they suffered from severe cognitive impairment, had current psychological treatment, or insufficient mastery of the Dutch language. The criteria were ascertained during a telephonic interview by a trained psychologist (KH).
Cancer survivors were recruited between August 2012 and September 2014 via four hospitals and via public media (i.e. advertisements on websites of patient societies, and in magazines and local newspapers). Cancer survivors were informed about the study, and asked to respond if they were interested in participating. The cancer survivors who signed the informed consent were randomized into one of the three study arms: MCGP-CS, SGP and CAU. All participants provided written informed consent.
Interventions
Meaning-centered group psychotherapy for cancer survivors (MCGP-CS)
The main purpose of MCGP-CS is to sustain or enhance a sense of meaning or purpose in a patient’s life, in order to cope better with the consequences of cancer. Theoretically, enhanced meaning is considered to be the catalyst of positive psychological outcomes. MCGP-CS is an adaptation of meaning-centered group psychotherapy (MCGP) for advanced cancer patients. MCGP was developed based on the work on meaning-making of Viktor Frankl (Frankl, 1986, 1998), and influenced by the existential work of Yalom (1980), Chocinov et al. (2005), and Kissane et al. (2003). Important existential concepts are incorporated in the theoretical framework of MCGP, such as identity, freedom, existential guilt, and existential isolation. A more comprehensive description of MCGP is published elsewhere (Breitbart, 2002, 2014, 2015). The adaptations concerned the use of different terminologies and topics more relevant for survivors. For instance, the topic “a good and meaningful death” was replaced by the topic “carrying on in life despite limitations”. Also, brief mindfulness exercises were added, to help participants with introspection before each group exercise. MCGP-CS is a manualized eight-week intervention that makes use of didactics, group discussions and experiental exercises that focus around themes related to meaning and cancer survivorship. The sessions lasted two hours each and were held weekly. The participants used a workbook (called Life lessons portfolio) and completed homework assignments every week. MCGP-CS was led by a psychotherapist with considerable experience in treating patients with cancer. The psychotherapists partaking in this study were trained in MCGP-CS during a pilot study (van der Spek, van Uden-Kraan, et al. 2014). Each session addressed a theme related to the concepts and sources of meaning (Table 1).
Table 1.
| Session | MCGP-CS | SGP |
|---|---|---|
| 1 | Concept and sources of meaning | Group member introductions |
| 2 | Meaning before and after cancer | The need for support |
| 3 | The story of our life as a source of meaning: what made us who we are today | Coping with the medical test and communicating with providers |
| 4 | The story of our life as a source of meaning: things we have done and want to do in the future | Coping with family and friends |
| 5 | Attitudinal sources of meaning: encountering life’s limitations | Coping with vocational issues |
| 6 | Creative sources of meaning: responsibility, courage and creativity | Coping with body image and physical functioning |
| 7 | Experiental sources of meaning | Coping with the future |
| 8 | Termination: presentations of our life lessons and goodbyes | Termination: goodbyes and how do we go on from here? |
Meaning-Centered Group Psychotherapy for Cancer Survivors
Supportive Group Psychotherapy
Supportive group psychotherapy (SGP)
SGP is an eight-week social supportive group therapy following Payne et al.(Payne, Vroom, and Phil 2009) The sessions lasted two hours and were held weekly. Each group was supervised by a psychotherapist with considerable experience in treating patients with cancer. In SGP no specific attention is paid to meaning. The psychotherapists were trained to avoid group discussions on meaning-related topics. The psychotherapist has an unconditionally positive regard and empathetic understanding, stimulates patients to actively share their experiences, and focuses on positive emotions and expression of feelings. Each of the eight sessions had a different theme (Table 1).
Care as usual (CAU)
Cancer survivors assigned to the CAU study arm did not participate in one of the group interventions. If a patient in the CAU study arm asked the researcher for psychological care, he or she was referred to their general practitioner. Health care uptake was monitored, to enable detailed post-hoc description of what CAU entailed.
There were two psychotherapists involved in this study, who facilitated MCGP-CS as well as SGP. In both treatment arms, the psychotherapist wrote a short summary of each session and noted whether the protocol was followed. All sessions were audiotaped, and randomly selected audio fragments were analyzed by a researcher (NvdS) to establish whether the therapy protocol was followed correctly. During the trial, three evaluation sessions with the therapists were held in which they obtained feedback from each other and from the researchers (NvdS and IV) on conducting the therapies according to the manuals, based on the summaries of the sessions and the analysis of the audio fragments. The therapy protocols of both MCGP-CS and SGP were followed accurately and meaning was barely discussed in SGP. Based on these analyses and evaluation, we concluded that treatment integrity was good.
Outcome measurement
The primary outcome was personal meaning, secondary outcomes were psychological well-being, posttraumatic growth, adjustment to cancer, optimism, hopelessness, psychological distress (anxiety and depression), and global quality of life. Outcome measures were collected at baseline before the intervention was scheduled and before randomization (t0), with follow-up assessments one week post-intervention (t1) and after three (t2) and six (t3) months follow-up (FU).
The primary outcome measure was Personal Meaning Profile-Dutch Version (PMP-DV) (total score) (Jaarsma et al. 2007).
Secondary outcome measures were: subscales of PMP (relation to God/higher order, dedication to life, fairness of life, goal-orientedness, and relations with others), Ryff’s Scales of Psychological Well-being (SPWB) (no total score available; eight subscales positive relations, autonomy, environmental mastery, personal growth, purpose in life, self-acceptance, inner strength, and higher power) (van Dierendonck 2004); Posttraumatic Growth Inventory (PTGI) (total score) (Jaarsma and Pool 2003); Mental Adjustment to Cancer (MAC) (no total score available; five subscales fighting spirit, helpless/hopeless, anxious preoccupation, fatalism, and avoidance) (Watson et al. 1988); Life Orientation Test-Revised (LOT-R) (total score) (ten Klooster et al. 2010); Beck’s Hopelessness Scale (BHS) (total score) (Young et al. 1992), Hospital Anxiety and Depression Scale (HADS) (total score, and subscales anxiety and depression) (Spinhoven 1997); and EORTC QLQ-C30 version 3.0 (global quality of life subscale) (Fayers & Bottomley 2002).
A study specific questionnaire at baseline comprised questions about sociodemographic factors (i.e. age, gender, religious background, marital status, household composition, education level, history of psychological treatment, other important negative life events in the past two years). Clinical characteristics (i.e. type of cancer, cancer treatment, time since diagnosis) of the patients recruited in hospitals were retrieved from the hospital information system, the clinical characteristics of patients recruited via public media were obtained from self-reports.
Sample size
Based on a priori power analyses for hierarchical multiple regression, assuming a power of .80, Cohen’s d of .80 and alpha of .05, each study condition needed at least 43 cancer survivors. We anticipated a 30% loss for the follow-up, and therefore included 56 cancer survivors per condition at baseline.
Randomization and blinding
This was a three-arm RCT study with block randomization. A computer-generated randomization table with random block sizes was prepared by an independent researcher not involved in the study. Participants were allocated to a group. When the group counted between seven and ten survivors, the group was randomly assigned by the independent researcher, using a list of sequentially numbered allocations, to one of the three study arms. Participants and psychotherapists were aware of the allocated arm, whereas data managers were blinded to the allocation.
Statistical analyses
Descriptive statistics, ANOVAs, independent samples t-tests, Kruskal-Wallis tests, and χ2 tests were used to determine whether patient characteristics (sociodemographic and clinical) were similar across experimental conditions. Missing values were excluded analysis by analysis. Results were reported on an intention-to-treat basis. Linear mixed models (LMM), with fixed effects for group, assessment and their two-way interaction, as well as a random intercept for randomization group and subjects (nested within the randomization group), were used to investigate differences in the course of the outcome measures between the three groups. Potential confounders were checked for all outcome measures and were added as fixed effects as well, in case they differed between experimental conditions. Post-hoc analyses were performed to assess which two groups differed significantly (via LMM) and at which points in time (via independent sample t-tests). Post-hoc analyses were corrected for multiple testing by Bonferroni’s correction, and for the potential confounders that differed significantly between conditions. Effect sizes (Cohen’s d) were calculated by dividing the difference in change since the baseline between groups by the pooled standard deviation, at the separate points in time (post-intervention, three months FU and six months FU). Effect sizes of 0.2 were categorized as small, 0.5 as medium, and 0.8 as large (Cohen 1977). For all analyses SPSS 20 was used; a p-value < 0.05 was considered to indicate statistical significance.
Results
Study population
A total of 2192 cancer survivors were approached via their hospital to participate in this study. Of these patients 411 (19%) applied for participation in response to this mailing (Figure 1). Eight participants applied in response to the advertisement in public media. Of the 419 cancer survivors who were screened for eligibility, 148 were ineligible and 87 declined to participate. A total of 184 consented to participate. Of those, 170 participants (40 male, 130 female) completed the baseline questionnaire and were randomly assigned to MCGP-CS (n = 57), SGP (n = 56), or CAU (n = 57). Table 2 displays the sociodemographic and clinical characteristics of the study population. There was a significant difference with respect to gender between the three groups, with more males in the MCGP-CS condition. When comparing the outcome measures at baseline (means and SD in Table 3), there was a significant difference between the study arms on positive relations (MCGP-CS = 4.1, SGP = 4.5, CAU = 4.5, χ2 = 6.685, df = 2, p = .035).
Figure 1.
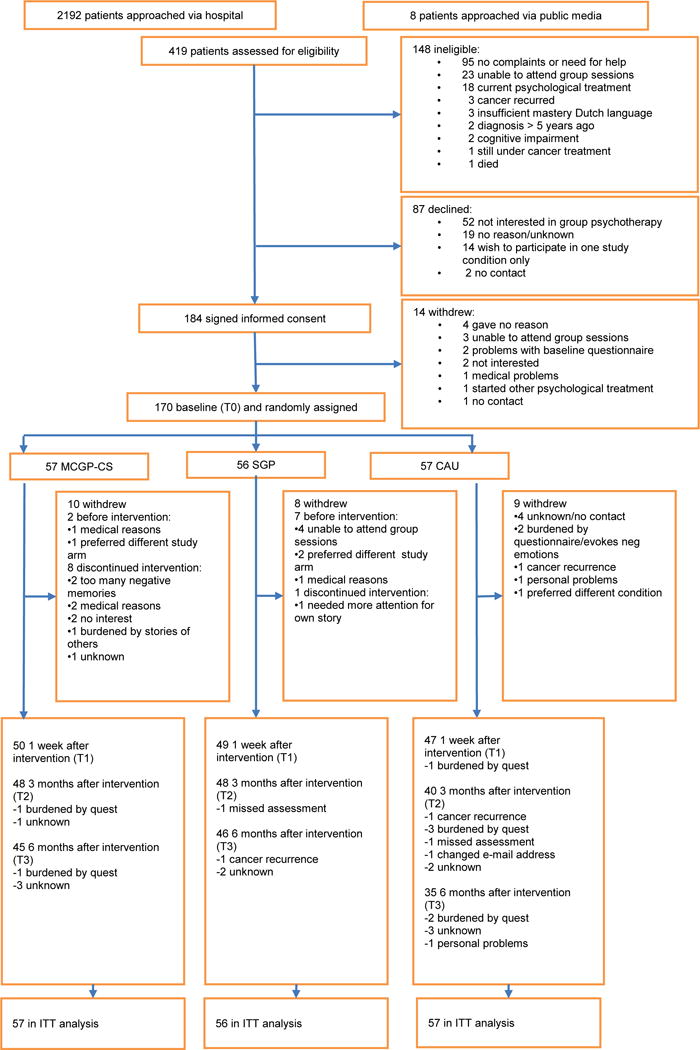
CONSORT diagram. Meaning-centered group psychotherapy for cancer survivors (MCGP-CS), supportive group psychotherapy (SGP), and care as usual (CAU)
Table 2.
Participant characteristics
|
MCGP-CS (n = 57) |
SGP (n = 56) |
CAU (n = 57) |
P | χ2 | |
|---|---|---|---|---|---|
| Age Mean (SD) | 58.6 (10.7) | 55.5 (9.6) | 57.3(10.4) | .340 | 2.58 |
| Sex Female N (%) | 40 (70%)* | 49 (88%) | 51 (90%) | .012 | 8.83 |
| Level of education | .156 | 6.65 | |||
| Low | 18 (32%) | 9 (16%) | 17 (30%) | ||
| Medium | 20 (35%) | 25 (45%) | 14 (26%) | ||
| High | 19 (33%) | 22 (39%) | 25 (44%) | ||
| Religion | .181 | 3.42 | |||
| Christian | 23 (40%) | 32 (57%) | 30 (53%) | ||
| No religion | 34 (60%) | 24 (43%) | 27 (47%) | ||
| Marital status Single N (%) | 12 (21%) | 9 (16%) | 13 (23%) | .650 | 0.86 |
| Household composition | |||||
| Lives alone | 10 (18%) | 11 (20%) | 11 (19%) | ||
| Lives with partner | 28 (49%) | 27 (48%) | 21 (37%) | ||
| Lives with children | 2 (4%) | 1 (2%) | 3 (5%) | ||
| Lives with partner and children | 17 (30%) | 17 (30%) | 22 (39%) | ||
| Type of cancer | .071 | 8.63 | |||
| Breast | 30 (53%) | 40 (71%) | 42 (74%) | ||
| Colon | 15 (26%) | 12 (21%) | 10 (18%) | ||
| Other | 12 (21%) | 4 (7%) | 5 (9%) | ||
| Months since last cancer treatment | 19 (6–58) | 16 (5–52) | 18 (3–55) | .888 | 0.241 |
| Median (range) | |||||
| Type of treatment | |||||
| Chemotherapy N (%) | 26 (53%) | 34 (61%) | 36 (67%) | .124 | 4.18 |
| Surgery N (%) | 57 (100%) | 56 (100%) | 56 (98%) | .369 | 1.99 |
| Radiation N (%) | 31 (54%) | 32 (57%) | 33 (58%) | .924 | 0.16 |
| Hormonal therapy N (%) | 22 (30%) | 28 (47%) | 30 (47%) | .280 | 2.54 |
| History psychological treatment N (%) | .724 | 3.65 | |||
| Received psychological treatment in the last year | 12 (21%) | 11 (20%) | 7 (13%) | ||
| Received psychological treatment > 1 year ago | 21 (37%) | 21 (37%) | 17 (31%) | ||
| Never received psychological treatment before | 24 (42%) | 24 (43%) | 31 (56%) | ||
| Significant negative event in past 2 years other than cancer N (%) | 27 (47%) | 31 (54%) | 33 (55%) |
Kruskall Wallis
significant difference between MCGP-CS and CAU
Table 3.
Linear Mixed Models analyzing treatment outcome
| Baseline, T0 | Post-intervention, T1 | 3-month follow-up, T2 | 6-month follow-up, T3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
|
MCGP-CS (n=57) |
SGP (n=56) |
CAU (n=57) |
MCGP-CS (n=50) |
SGP (n=50) |
CAU (n=47) |
MCGP-CS (n=48) |
SGP (n=48) |
CAU (n=40) |
MCGP-CS (n=45) |
SGP (n=46) |
CAU (n=35) |
||
|
| |||||||||||||
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | P | |
| PMP | |||||||||||||
| Total Score* | 58.0(15.9) | 60.2(13.3) | 58.8(11.7) | 61.0(16.2) | 62.3(13.1) | 56.3(13.1) | 60.9(17.2) | 61.5(14.8) | 58.2(14.9) | 60.4(16.6) | 61.1(14.3) | 58.7(13.2) | .019 |
|
| |||||||||||||
| Rel. God/higher order | 31.9(25.0) | 39.3(23.5) | 29.8(20.0) | 35.6(26.4) | 40.4(25.7) | 28.7(22.6) | 36.0(27.2) | 41.0(24.4) | 30.6(21.7) | 34.8(24.6) | 39.3(22.6) | 32.5(23.1) | .198 |
| Dedication to life | 67.1(18.8) | 66.0(11.2) | 67.7(10.5) | 69.2(17.8) | 67.4(10.4) | 64.6(11.6) | 69.7(18.6) | 65.5(12.0) | 66.9(11.8) | 69.7(19.3) | 67.0(11.6) | 67.2(10.4) | .141 |
| Fairness of life | 55.7(15.9) | 54.8(14.8) | 54.7(15.3) | 60.3(15.9) | 59.4(16.7) | 54.3(17.2) | 59.8(18.4) | 59.1(17.2) | 55.6(17.3) | 60.8(18.4) | 58.7(17.7) | 56.7(16.9) | .339 |
| Goal-orientedness* | 68.7(0.20) | 71.0(16.9) | 71.5(17.5) | 73.6(19.7) | 72.5(16.1) | 63.0(23.3) | 69.6(21.5) | 71.1(18.4) | 66.1(20.9) | 67.2(21.7) | 69.7(18.1) | 67.2(20.1) | <.001 |
| Relations with others | 70.6(26.2) | 73.9(25.3) | 74.8(21.3) | 70.4(25.3) | 77.8(22.2) | 73.7(21.6) | 71.9(25.2) | 76.3(22.1) | 74.5(21.7) | 70.1(27.5) | 75.0(23.7) | 71.1(23.2) | .344 |
| SPWB | |||||||||||||
| Psych. well-being | |||||||||||||
| Positive relations* | 4.1(1.0) | 4.5(1.0) | 4.5(0.83) | 4.4(1.1) | 4.7(0.95) | 4.4(0.93) | 4.3(1.0) | 4.6(0.95) | 4.5(0.86) | 4.3(1.1) | 4.6(1) | 4.4(0.87) | .036 |
| Autonomy1 | 4.2(0.85) | 4.3(0.83) | 4.3(0.72) | 4.4(0.80) | 4.5(0.76) | 4.4(0.76) | 4.4(0.76) | 4.4(0.87) | 4.4(0.62) | 4.4(0.78) | 4.4(0.93) | 4.4(0.55) | .384 |
| Environm. Mastery* | 4.2(0.74) | 4.3(0.71) | 4.4(0.72) | 4.5(0.75) | 4.3(0.79) | 4.4(0.67) | 4.5(0.70) | 4.3(0.67) | 4.5(0.69) | 4.5(0.80) | 4.3(0.71) | 4.5(0.69) | .012 |
| Personal Growth* | 4.2(0.75) | 4.4(0.59) | 4.3(0.60) | 4.4(0.68) | 4.4(0.56) | 4.3(0.62) | 4.4(0.63) | 4.3(0.60) | 4.3(0.66) | 4.3(0.72) | 4.4(0.60) | 4.3(0.67) | .032 |
| Purpose in life* | 4.1(0.89) | 4.3(0.77) | 4.4(0.62) | 4.4(0.89) | 4.3(0.80) | 4.3(0.65) | 4.3(0.78) | 4.3(0.84) | 4.3(0.58) | 4.3(0.85) | 4.2(0.87) | 4.4(0.61) | .007 |
| Self-acceptance | 4.0(0.87) | 4.2(0.80) | 4.3(0.64) | 4.2(0.82) | 4.3(0.83) | 4.3(0.63) | 4.3(0.77) | 4.2(0.81) | 4.4(0.57) | 4.3(0.78) | 4.2(0.88) | 4.3(0.72) | .262 |
| Spiritual well-being | |||||||||||||
| Inner strength | 4.0(0.69) | 4.1(0.80) | 4.1(0.66) | 4.2(0.80) | 4.2(0.74) | 4.1(0.78) | 4.3(0.82) | 4.2(0.83) | 4.1(0.86) | 4.2(0.91) | 4.2(0.84) | 4.2(0.60) | .245 |
| Higher Power | 2.8(1.4) | 3.1(1.3) | 2.8(1.3) | 3.0(1.3) | 3.2(1.3) | 2.7(1.2) | 3.0(1.4) | 3.1(1.2) | 2.7(1.2) | 3.0(1.3) | 3.2(1.2) | 2.9(1.2) | .452 |
| PTGI | |||||||||||||
| Total score | 41.8(20.5) | 48.2(17.4) | 46.4(18.4) | 48.1(20.5) | 52.6(17.1) | 49.1(19.5) | 46.3(21.2) | 52.1(17.1) | 49.5(21.3) | 45.8(23.3) | 49.3(19.6) | 51.4(19.3) | .453 |
| MAC | |||||||||||||
| Fighting spirit* | 46.0(5.4) | 45.9(5.6) | 47.3(4.3) | 47.7(6) | 45.5(5.1) | 46.8(5.2) | 47.0(4.9) | 47.0(4.5) | 46.5(5.8) | 47.3(6) | 46.9(46.5) | 45.8(5.7) | .001 |
| Helpless/Hopeless* | 10.7(2.9) | 10.7(2.9) | 10.3(2.5) | 9.6(3) | 10.6(2.9) | 10.2(2.7) | 9.6 (2.9) | 10.2(2.9) | 11.0(2.7) | 10.0(3.4) | 10.4(2.9) | 10.9(3.4) | .005 |
| Anxious preoccupation | 22.4(3.3) | 23.1(3.3) | 22.8(3.6) | 21.7(3.2) | 22.3(3.3) | 22(3.2) | 20.9(3.4) | 22.4(3.9) | 22.3(3.4) | 21.1(3.9) | 21.7(3.6) | 22.4(3.8) | .231 |
| Fatalism1 | 19.1(2.5) | 18.6(3.1) | 18.5(2.8) | 19(3.1) | 18.5(2.6) | 18.2(3.0) | 18.3(2.7) | 18.8(2.5) | 18.7(2.7) | 18.6(2.8) | 18.4(2.3) | 18.7(2.7) | .113 |
| Avoidance | 1.7(0.70) | 1.8(0.90) | 1.6(0.78) | 1.8(0.83) | 1.7(0.65) | 1.5(0.76) | 1.7(0.71) | 1.6(0.70) | 1.7(0.85) | 1.7(0.68) | 1.7(0.80) | 1.8(0.79) | .734 |
| LOT-R | |||||||||||||
| Optimism1 | 12.2(3) | 12.1(2.4) | 12.1(3.5) | 13.2(3.2) | 11.8(2.5) | 12.4(2.7) | 12.8(3.2) | 12.4(2.7) | 12.4(3) | 13(3.9) | 12.2(2.9) | 12.2(3.2) | .442 |
| BHS | |||||||||||||
| Total score | 6.6(4.9) | 6.0(4.8) | 5.8(3.8) | 5.3(5) | 5.6(4.7) | 6.1(4.2) | 5.0(4.7) | 6.0(4.6) | 5.9(5.2) | 4.9(4.9) | 5.7(5.0) | 5.6(4.9) | .109 |
| HADS | |||||||||||||
| Total score* | 12.3(6.5) | 12.4(6.5) | 11.8(5.2) | 9.8(6.2) | 10.6(6.6) | 11.1(6.8) | 9.5(7.6) | 10.9(7) | 10.9(6.5) | 8.8(7.0) | 10.4(6.9) | 12.3(8.1) | .025 |
| Anxiety | 7.2(3.9) | 7.9(3.8) | 7.4(2.8) | 6.1(3.8) | 6.8(3.7) | 6.8(3.6) | 5.6(4.0) | 7.1(3.9) | 6.5(3.6) | 5.5(3.8) | 6.8(3.7) | 7.4(4.1) | .133 |
| Depression* | 5.1(3.5) | 4.5(3.3) | 4.4(3.3) | 3.7(3.3) | 3.8(3.4) | 4.3(4.1) | 3.9(3.8) | 3.8(3.5) | 4.3(3.8) | 3.3(3.8) | 3.6(3.7) | 5.0(4.8) | .025 |
| EORTC QLQ-C30 | |||||||||||||
| Global quality of life | 71.6(17.0) | 70.2(17.3) | 72.7(13.3) | 72.6(18.1) | 76.4(17.4) | 74(17.1) | 73.5(19.5) | 76.6(17.5) | 73.5(18.3) | 73(22.1) | 74.6(15.6) | 68.5(22.4) | .263 |
Corrected for gender
= p<.05
Abbreviations: PMP, Personal Meaning Profile; SPWB, Ryff’s Scale of Psychological Well-being; PTGI, Post Traumatic Growth Inventory; MAC, Mental Adjustment to Cancer Scale; LOT-R, Life Orientation Test-Revised; BHS, Beck’s Hopelessness Scale; HADS, Hospital Anxiety and Depression Scale; EORTC QLQ-C30 quality of life questionnaire; MCGP-CS, Meaning-Centered Group Psychotherapy for Cancer Survivors; SGP, Supportive Group Psychotherapy; CAU, Care As Usual
In MCGP-CS, two participants (4%) never attended any group sessions, and in SGP seven participants (13%) never attended. In MCGP-CS, eight participants (14%) did not complete the intervention, mostly because the intervention differed from their expectations or because of medical reasons. In SGP, one participant discontinued (2%) due to lack of interest in the intervention. A total of 147 participants (86%) completed the assessment post-intervention, 136 (80%) the three-month follow-up, and 126 (74%) the six-month follow-up. In CAU, most participants received no additional psychosocial care during the study (93%), 7% received additional care (i.e. psychotherapy, self-help group, social work, or spiritual counseling).
Efficacy of MCGP-CS
Table 3 shows the results of the LMM analyzing outcome measures per time assessment. In these models, the random slope for randomization group was removed as the estimated variance of randomization group was zero. Significant differences (corrected for sex) between MCGP-CS, SGP, and CAU were found on the course of personal meaning (total score PMP), and on secondary outcomes: subscale PMP (i.e. goal-orientedness), psychological well-being (SPWB) (i.e. positive relations, purpose in life, environmental mastery, personal growth), adjustment to cancer (MAC) (i.e. fighting spirit, helpless/hopeless), and psychological distress (HADS) (i.e. total score and depression). There were no significant differences between the three groups on the course of posttraumatic growth (PTGI), optimism (LOT-R), hopelessness (Beck’s Hopelessness Scale) or global quality of life (EORTC QLQ-C30) (Table 3).
Post-hoc analyses showed significantly stronger treatment effects of MCGP-CS compared to CAU with respect to the course of personal meaning, goal-orientedness, positive relations, purpose in life, fighting spirit, helpless/hopeless, distress, depression, and significantly stronger effects of MCGP-CS compared to SGP for personal growth and environmental mastery (Table 4). Significantly stronger treatment effects of SGP compared to CAU were observed for goal-orientedness and fighting spirit.
Table 4.
Linear Mixed Model analyses: differences between two study arms
| MCGP-CS-CAU | MCGP-CS-SGP | SGP-CAU | |
|---|---|---|---|
|
| |||
| p-value | p-value | p-value | |
| PMP | |||
| Total Score | .027* | .73 | .084 |
|
| |||
| Goal-orientedness | <.001* | 1.00 | .009* |
| SPWB | |||
| Positive relations | .033* | 1.00 | .56 |
| Environmental mastery | .19 | .006* | 1.00 |
| Personal Growth | .26 | .021* | .24 |
| Purpose in life | .021* | .057 | .73 |
| MAC | |||
| Fighting spirit * | .021* | .072 | .024* |
| Helpless/Hopeless* | .012* | .38 | .084 |
| HADS | |||
| Total score* | .018* | 1.00 | .31 |
| Depression * | .012* | 1.00 | .40 |
p<.05
Abbreviations: PMP, Personal Meaning Profile; SPWB, Ryff’s Scale of Psychological Well-being; PTGI, Post Traumatic Growth Inventory; HADS, Hospital Anxiety and Depression Scale; MAC, Mental Adjustment to Cancer Scale; MCGP-CS, Meaning-Centered Group Psychotherapy for Cancer Survivors; SGP, Supportive Group Psychotherapy; CAU, Care As Usual
Table 5 shows treatment effects post-intervention, and at the follow-up after three and six months. When comparing MGCP-CS with CAU post-intervention, large effect sizes were found on the primary outcome measure personal meaning and secondary outcome goal-orientedness, and medium effect sizes on positive relations, purpose in life, and fighting spirit. At the follow-up after three months, a large effect size was found on helpless/hopeless. At the follow-up after six months, a medium effect size was found on distress, and a small effect on depression (six months FU). When comparing MCGP-CS with SGP, a medium effect size was found for personal growth (three months FU), and environmental mastery (six months FU). When comparing SGP to CAU, a large effect was observed for goal-orientedness (post-intervention).
Table 5.
Treatment effects post-intervention (T1), at 3-month (T2) and 6-month (T3) follow-up compared to baseline (T0)
| T1 vs T0 | T2 vs T0 | T3 vs T0 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| MCGP-CS-CAU | MCGP-CS-SGP | SGP-CAU | MCGP-CS-CAU | MCGP-CS-SGP | SGP-CAU | MCGP-CS-CAU | MCGP-CS-SGP | SGP-CAU | |
|
| |||||||||
| d, p | 1d, p | d, p | d, p | d, p | d, p | d, p | d, p | d, p | |
| PMP | |||||||||
| Total Score | 0.81, <.001 | 0.17, ns | 0.66, ns | 0.32, ns | 0.17, ns | 0.18, ns | 0.19, ns | 0.16, ns | 0.03, ns |
|
| |||||||||
| Goal-orientedness | 1.07, <.001 | 0.23, ns | 0.86, <.001 | 0.37, ns | 0.02, ns | 0.38, ns | 0.08, ns | −0.03, ns | 0.12, ns |
| SPWB | |||||||||
| Positive relations | 0.59, .008 | 0.23, ns | 0.41, ns | 0.38, ns | 0.21, ns | 0.18, ns | 0.51, ns | 0.29, ns | 0.27, ns |
| Environmental mastery | 0.47, ns | 0.65, .003 | −0.22, ns | 0.33, ns | 0.57, .021 | −0.24, ns | 0.31, ns | 0.66, 0.01 | −0.34, ns |
| Personal growth | 0.56, ns | 0.58, .022 | 0.02, ns | 0.31, ns | 0.57, .031 | −0.24, ns | 0.16, ns | 0.31, ns | −0.14, ns |
| Purpose in life | 0.69, <.001 | 0.62, ns | 0.09, ns | 0.48, ns | 0.34, ns | 0.13, ns | 0.12, ns | 0.39, ns | −0.26, ns |
| MAC | |||||||||
| Fighting spirit | 0.61, .012 | 0.54, ns | 0.06, ns | 0.51, ns | 0.04, ns | 0.47, ns | 0.56, ns | 0.04, ns | 0.54, ns |
| Helpless/Hopeless | 0.49, ns | 0.43, ns | 0.04, ns | −0.87, .001 | −0.28, ns | −0.58, ns | −0.41, ns | −0.16, ns | −0.32, ns |
| HADS | |||||||||
| Total score | 0.39, ns | 0.1, ns | 0.32, ns | −0.31, ns | −0.22, ns | −0.05, ns | −0.6, .014 | −0.26, ns | −0.45, ns |
| Depression | −0.51, ns | −0.21, ns | −0.29, ns | −0.32, ns | −0.14, ns | −0.17, ns | −0.38, .017 | −0.25, ns | −0.20, ns |
Only those scales are shown with significant differences after LMM analysis
d corresponds to between group difference score of Cohen’s d
Abbreviations: PMP, Personal Meaning Profile; SPWB, Ryff’s Scale of Psychological Well-being; PTGI, Post Traumatic Growth Inventory; HADS, Hospital Anxiety and Depression Scale; MAC, Mental Adjustment to Cancer Scale; MCGP-CS, Meaning-Centered Group Psychotherapy for Cancer Survivors; SGP, Supportive Group Psychotherapy; CAU, Care As Usual
Discussion
This randomized controlled trial provides evidence for the efficacy of MCGP-CS to improve personal meaning among cancer survivors. With respect to the secondary outcomes, support was found that MCGP-CS also improves goal-orientedness, psychological well-being and adjustment to cancer. Furthermore, that it reduces psychological distress and depressive symptoms in cancer survivors in the long run, at six months after intervention.
The results of this study are in line with the results of a previous study on MCGP for cancer patients in the palliative phase (Breitbart et al. 2015), showing that MCGP is not only beneficial for patients with advanced cancer, but also for survivors. Another new finding of the present study is that positive effects of MCGP-CS occurred not only shortly after the intervention but also in the longer term. Although the effect with respect to personal meaning, psychological well-being, and adjustment to cancer decayed, longer-term effects were found on environmental mastery, distress and depressive symptoms. Interestingly, the effect of MCGP-CS on distress and depressive symptoms did only occur at the long-term follow-up. An explanation may be that experiencing personal meaning or purpose after a search for meaning precedes a decrease in psychological distress, in accordance with Park’s Meaning Making Model (Crystal L Park 2010). However, further research is needed to explore this finding.
MCGP-CS had no significant effect on posttraumatic growth (PTG). Growth is considered a part of psychological well-being (Wong 2010), therefore it was hypothesized that MCGP-CS could improve PTG as well. However, recent empirical findings suggest that PTG is not related to psychological well-being (Zoellner et al. 2011). This might explain why we did not find any effect on PTG. Interestingly, MCGP-CS did have an effect on personal growth. Whereas PTG entails growth that is specifically attributed to cancer as a traumatic event, narrowly focusing on the cancer experience, personal growth involves seeing oneself as developing through time and thereby realizing personal potential (van Dierendonck 2004), unrelated to cancer. It may be that MCGP-CS focuses on sense of meaning placed in a broader context of one’s personal narrative, and thus addressed personal growth rather than PTG. Further (qualitative) research is needed to examine this effect of MCGP-CS on personal growth.
When compared to CAU, it is clear that MCGP-CS is efficacious in improving the primary outcome measure personal meaning post-intervention. No differences were found on personal meaning when MCGP-CS and SGP were compared with each other directly, however, the analyses showed that on the primary outcome measure, only MCGP-CS was effective (as compared to CAU). With respect to secondary outcomes, several improvements were measured until the six-month follow-up. MCGP-CS was equally effective compared to SGP on personal meaning, but more effective on personal growth and environmental mastery, also in the longer-term. When compared to CAU, SGP only had a positive effect on goal-orientedness, and only post-intervention. These findings indicate that in comparison to CAU, MCGP-CS is more efficacious than SGP, which implicates that a meaning-focused approach is more successful than traditional supportive group psychotherapy. Meaning-focused coping might be more effective than other coping strategies, in improving positive psychological outcomes, as well as symptom-related outcomes. Possibly, because it affects the identity of the patients, placing the disease in a broader context of their life’s narrative and their personal meaning. Future research should look into the working mechanisms of meaning-focused coping and MCGP(-CS).
Important strengths of this study were the specific focus on cancer survivors, a large sample size with various types of cancer diagnoses, and high treatment adherence. Furthermore, a strength of MCGP-CS is that it was developed based on both theoretical and empirical knowledge, as well as on input from cancer survivors and clinical experts (van der Spek, Vos, et al. 2014). A limitation of this study was that no clear cut-off scores or minimal important difference (MID) criteria are available regarding the primary outcome measure personal meaning, and the secondary outcome measures psychological well-being and mental adjustment to cancer. Future research is needed to define cut-off scores and MIDs that may help to identify cancer survivors who might benefit most from MCGP-CS. Also, when interpreting the results of the linear mixed model analyses of the secondary outcome measures, it should be borne in mind that the use of multiple comparisons might only have led to significant results by chance. There is no clear consensus on whether this should be corrected, and a correction might have led to less efficient estimates. Therefore we did not perform a correction, and for every 20 true null hypotheses we expect one to be falsely rejected (Gelman, Hill, and Yajima 2012). However, with respect to the post-hoc analyses, Bonferroni corrections were applied. Another limitation is that patients and therapists in the study could not be blinded which may have caused bias. Also, MCGP-CS and SGP were supervised by the same therapists, this incorporates a risk of bleed across conditions; however, no indication for this was found in the evaluation of treatment integrity. Finally, it is important to note that allegiance bias is a risk in this type of research (e.g. Leykin & DeRubeis, 2009). However, several measures were taken to minimize this risk. For instance, the randomization was carried out by an independent researcher, using a random number table, and an independent researcher (BW) performed the first statistical analyses.
Despite the study limitations, this study provides evidence on the efficacy of MCGP-CS to improve personal meaning, psychological well-being, and mental adjustment to cancer, and to reduce psychological distress and depressive symptoms in the long run. Given that dealing with the aftermath of cancer is both a psychological and an existential challenge for many survivors, an evidence based intervention such as MCGP-CS, that addresses and successfully affects both these aspects, is an important addition to psycho-oncological health care.
Footnotes
Trial registration: NTR3571
References
- Brenner H. Long-term survival rates of cancer patients achieved by the end of 20th century: a period analysis. Lancet. 2002;2002:1131–1135. doi: 10.1016/S0140-6736(02)11199-8. [DOI] [PubMed] [Google Scholar]
- Breitbart WS. Spirituality and meaning in supportive care: spirituality and meaning-centered group psychotherapy interventions in advanced cancer. Supportive Care in Cancer. 2002;10:272–280. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- Breitbart WS, Poppito S. Meaning-Centered Group Psychotherapy for patients with advanced cancer. New York: Oxford University Press; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbart WS, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-Centered Group Psychotherapy: An Effective Intervention for Improving Psychological Well-Being in Patients With Advanced Cancer. Journal of Clinical Oncology. 2015;33:749–54. doi: 10.1200/JCO.2014.57.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, Harlos M. Effect of Dignity Therapy on Distress and End-of-Life Experience in Terminally Ill Patients: A Randomised Controlled Trial. The Lancet Oncology. 2011;12:753–62. doi: 10.1016/S1470-2045(11)70153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. London: Routledge; 1977. [Google Scholar]
- Gelman A, Hill J, Yajima M. Why We (Usually) Don’t Have to Worry About Multiple Comparisons. Journal of Research on Educational Effectiveness. 2012;5:189–211. [Google Scholar]
- Hoffman KE, McCarthy EP, Recklitis CJ, Ng AK. Psychological Distress in Long-term Survivors of Adult-Onset Cancer Results From a National Survey. Archives of Internal Medicine. 2009;14:1274–1281. doi: 10.1001/archinternmed.2009.179. [DOI] [PubMed] [Google Scholar]
- Jaarsma TA, Pool G. Posttraumatic Growth Inventory: Dutch Version. Groningen: Noordelijk Centrum Voor Gezondheidsvraagstukken; 2003. [Google Scholar]
- Jaarsma TA, Pool G, Ranchor AV, Sanderman R. The Concept and Measurement of Meaning in Life in Dutch Cancer Patients. Psycho-Oncology. 2007;16:241–48. doi: 10.1002/pon.1056. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Bloch S, Smith GC, Miach P, Clarke DM, Ikin J, Love A, Ranieri N, McKenzie D. Cognitive-Existential Group Psychotherapy for Women with Primary Breast Cancer: A Randomised Controlled Trial. Psycho-Oncology. 2003;12:532–46. doi: 10.1002/pon.683. [DOI] [PubMed] [Google Scholar]
- Lee V. The Existential Plight of Cancer: Meaning Making as a Concrete Approach to the Intangible Search for Meaning. Supportive Care in Cancer. 2008;16:779–85. doi: 10.1007/s00520-007-0396-7. [DOI] [PubMed] [Google Scholar]
- Lee V, Cohen SR, Edgar L, Laizner AM, Gagnon AJ. Meaning-Making Intervention during Breast or Colorectal Cancer Treatment Improves Self-Esteem, Optimism, and Self-Efficacy. Social Science & Medicine. 2006;62:3133–45. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- LeMay K, Wilson KG. Treatment of Existential Distress in Life Threatening Illness: A Review of Manualized Interventions. Clinical Psychological Review. 2008;28:472–93. doi: 10.1016/j.cpr.2007.07.013. [DOI] [PubMed] [Google Scholar]
- Lethborg C, Aranda S, Cox S, Kissane D. To What Extent Does Meaning Mediate Adaptation to Cancer? The Relationship between Physical Suffering, Meaning in Life, and Connection to Others in Adjustment to Cancer. Palliative Supportive Care. 2007;5:377–88. doi: 10.1017/s1478951507000570. [DOI] [PubMed] [Google Scholar]
- Leykin Y, DeRubeis RJ. Allegiance in Psychotherapy Outcome Research: Separating Association From Bias. Clinical Psychological Science and Practice. 2009;16:54–65. [Google Scholar]
- McClain CS, Rosenfeld B, Breitbart W. Effect of Spiritual Well-Being on End-of-Life Despair in Terminally-Ill Cancer Patients. Lancet. 2003;361:1603–7. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A. Cancer treatment and survivorship statistics, 2016. CA: A Cancer Journal for Clinicians. 2016 doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- Park CL, Edomondson D, Fenster JR, Blank TO. Meaning Making and Psychological Adjustment Following Cancer: The Mediating Roles of Growth, Life Meaning, and Restored Just-World Beliefs. Journal of Consulting and Clinical Psychology. 2008:863–75. doi: 10.1037/a0013348. [DOI] [PubMed] [Google Scholar]
- Park CL. Making Sense of the Meaning Literature: An Integrative Review of Meaning Making and Its Effects on Adjustment to Stressful Life Events. Psychological Bulletin. 2010;136:257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Payne DK, Vroom P, Phil M. Supportive Group Psychotherapy: A Group Intervention for Cancer Patients. New York: Memorial Sloan-Kettering Cancer Center; 2009. [Google Scholar]
- Richards MA, Stockton D, Bapp P, Coleman MP. How many deaths have been avoided through improvements in cancer survival? British Medical Journal. 2000;320:895–898. doi: 10.1136/bmj.320.7239.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santin O, Murray L, Prue G, Gavin A, Gormley G, Donnelly M. Self-reported psychosocial needs and health-related quality of life of colorectal cancer survivors. European Journal of Oncology Nursing. 2015;19:336–342. doi: 10.1016/j.ejon.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Spira J. Supportive-Expressive Group Therapy: A Treatment Manual of Psychosocial Intervention for Women with Recurrent Breast Cancer. Stanford, CA: Stanford University School of Medicine; 1991. [Google Scholar]
- Spinhoven P. A Validation Study of the Hospital Anxiety and Depression Scale (HADS) in Different Groups of Dutch Subjects. Psychological Medicine. 1997;27:363–70. doi: 10.1017/s0033291796004382. [DOI] [PubMed] [Google Scholar]
- ten Klooster PM, Weekers AM, Eggelmeijers F, Van Woerkom JM, Drossaert CHC, Taal E, Baneke JJ, Rasker JJ. Optimisme En/of Pessimisme: Factorstructuur van de Nederlandse Life Orientation Test-Revised. Psychologie En Gezondheid. 2010;38:89–100. [Google Scholar]
- Thewes B, Butow P, Girgis A, Pendlebury S. The psychosocial needs of breast cancer survivors; A qualitative study of the shared and unique needs of younger versus older survivors. Psycho-Oncology. 2004;13:177–189. doi: 10.1002/pon.710. [DOI] [PubMed] [Google Scholar]
- Tomich PL, Helgeson VS. Five Years Later: A Cross-Sectional Comparison of Breast Cancer Survivors with Healthy Women. Psycho-Oncology. 2002;11:154–69. doi: 10.1002/pon.570. [DOI] [PubMed] [Google Scholar]
- van der Spek N, van Uden-Kraan CF, Vos J, Breitbart W, Tollenaar RAEM, van Asperen CJ, Cuijpers P, Verdonck-de Leeuw IM. Meaning-Centered Group Psychotherapy in Cancer Survivors: A Feasibility Study. Psycho-Oncology. 2014;23:827–831. doi: 10.1002/pon.3497. [DOI] [PubMed] [Google Scholar]
- van der Spek N, Vos J, van Uden-Kraan CF, Breitbart W, Cuijpers P, Knipscheer-Kuipers K, Willemsen V, Tollenaar RAEM, van Asperen CJ, Verdonck-de Leeuw IM. Effectiveness and Cost-Effectiveness of Meaning-Centered Group Psychotherapy in Cancer Survivors: Protocol of a Randomized Controlled Trial. BMC Psychiatry. 2014;14:22. doi: 10.1186/1471-244X-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Spek N, Vos J, van Uden-Kraan CF, Breitbart W, Tollenaar RAEM, Cuijpers P, Verdonck-de Leeuw IM. Meaning Making in Cancer Survivors: A Focus Group Study. PLoS ONE. 2013;8:e76089. doi: 10.1371/journal.pone.0076089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dierendonck D. The Construct Validity of Ryff’s Scales of Psychological Well-Being and Its Extension with Spiritual Well-Being. Personality and Individual Differences. 2004;36:629–43. [Google Scholar]
- Watson M, Greer S, Young J, Inayat Q, Burgess C, Robertson B. Development of a Questionnaire Measure of Adjustment to Cancer: The MAC Sca1e. Psychological Medicine. 1988;18:203–9. doi: 10.1017/s0033291700002026. [DOI] [PubMed] [Google Scholar]
- Wong P. In: The Human Quest for Meaning. 2nd. Wong Paul TP., editor. New York: Routledge, Taylor & Francis Group; 2010. [Google Scholar]
- Yalom ID. Existential psychotherapy. Basic Books 1980;1 [Google Scholar]
- Yalom ID, Greaves C. Group Therapy with the Terminally Ill. Americam Journal of Psychiatry. 1977;134:396–400. doi: 10.1176/ajp.134.4.396. [DOI] [PubMed] [Google Scholar]
- Young MA, Halper IS, Clark DC, Scheftner W, Fawcett J. An Item-Response Theory Evaluation of the Beck Hopelessness Scale. Cognitive Therapy and Research. 1992;16:579–87. [Google Scholar]
- Zika S, Chamberlain K. On the Relation between Meaning in Life and Psychological Well-Being. British Journal of Psychology. 1992;83:133–45. doi: 10.1111/j.2044-8295.1992.tb02429.x. [DOI] [PubMed] [Google Scholar]
- Zoellner T, Rabe S, Karl A, Maercker A. Post-Traumatic Growth as Outcome of a Cognitive-Behavioural Therapy Trial for Motor Vehicle Accident Survivors with PTSD. Psychology and Psychotherapy. 2011;84:201–13. doi: 10.1348/147608310X520157. [DOI] [PubMed] [Google Scholar]


