Abstract
Objective
Childhood sexual abuse (CSA) is a critical global health issue associated with poor psychosocial outcomes. Individuals with CSA histories are at risk for drug use, which is a growing problem in the Western Cape of South Africa. The present study of methamphetamine users in this region examined whether substance use coping, a contextually relevant type of avoidance-based coping, mediates the relation between CSA and depressive symptoms.
Method
Participants included 161 men and 108 women seeking treatment for methamphetamine use. Participants completed a computer-assisted survey and a face-to-face interview with clinic staff to evaluate history of CSA, current substance use severity and coping, and current depressive symptoms.
Results
Nearly a third of participants reported a history of CSA, and the average methamphetamine useseverity score exceeded the threshold of high risk. A history of CSA was significantly associated with higher substance use coping and more depression symptoms. Substance use coping was a significantmediator of the association between CSA and depression symptoms.
Conclusions
In this study of high-risk methamphetamine users, substance use coping emerged as a common means of managing stress, especially for those with a history of CSA, which was further linked to depressive symptoms. These findings underscore the potential benefit of integrating coping interventions and mental health treatment into substance abuse treatment programs, particularly for those with a history of childhood abuse and violence.
Keywords: South Africa, methamphetamine, coping, childhood sexual abuse, depression
Childhood sexual abuse (CSA) is a human rights issue of global proportions. Reported prevalence of CSA worldwide is approximately one in eight (Stoltenborgh, van Ijzendoorn, Euser, & Bakermans-Kranenburg, 2011), with higher rates in sub-Saharan Africa (Andersson et al., 2012). In South Africa, 17.7% of males and 18.3% of females have experienced forced or coerced sex by age 16 (Andersson et al., 2012). The experience of widespread poverty in sub-Saharan Africa may place children at high risk of sexual abuse, as CSA has been linked with insufficient food in the home and lower levels of education (Andersson et al., 2012; Madu & Peltzer, 2000). Also of critical concern in this region isthe increasing use of methamphetamine, a highly addictive psychostimulant that causes both physical and psychological harm (Darke, Kay, McKetin, & Duflou, 2008). Over the past 30 years, expansion of drug trafficking routes has led to dramatic increases in drug use across Africa, with the highest reported consumption of methamphetamine in South Africa (United Nations Office on Drugs and Crime, 2011; Mbwambo et al., 2012). Since 2000, peri-urban (“township”) communities in the Western Cape have seen a sharp rise in use of methamphetamine, which is known locally as tik (Plüddemann, Myers, & Parry, 2008; Plüddemann, Flisher, McKetin, Parry, & Lombard, 2010). Many South African individuals living in poverty begin to use methamphetamine due to boredom resulting from a lack of employment opportunities, and others becoming involved in distribution as a method of income generation (Hobkirk, Watt, Myers, Skinner, & Meade, 2016). Therefore, the high rates of poverty in this area may contribute to both CSA and substance use (Singer et al., 2006). Furthermore, several studies have documented an association between CSA and substance use in South African populations (Jewkes, Dunkle, Nduna, Jama, & Puren, 2010; King et al., 2004; Meade et al., 2012).
CSA often leads to poor psychological outcomes, including depression and PTSD, that may persist throughout adolescence and adulthood in South African populations (Brown et al., 2009; Carey, Walker, Rossouw, Seedat, & Stein, 2008; Collings, 1995; Jewkes et al., 2010). Several studies have also documented an association between CSA and substance use in South African populations (Jewkes et al., 2010; King et al., 2004; Meade et al., 2012). Individuals may turn to substances, such as methamphetamine, to cope with the traumatic stress that mayresultfrom CSA (Leeies, Pagura, Sareen, & Bolton, 2010; Robinson, Sareen, Cox, & Bolton, 2011; Ullman, Relyea, Peter-Hagene, & Vasquez, 2013). Coping through the use of substances is an avoidance-based strategy that aligns with the self-medication hypothesis, which proposes that substances are used to reduce painful negative affect (Khantzian, 1997); however, avoidance-based coping strategies often have negative psychosocial effects in the long term (Roth & Cohen, 1986). Broadly, the use of avoidance-based coping strategies has been linked with higher rates of depression, more rapid progression of depressive symptoms, and general psychological distress (Min, Farkas, Minnes, & Singer, 2007; Morris, Kouros, Fox, Rao, & Garber, 2014). Previous studies have found varying effects of gender on coping outcomes. In some studies, women exhibiting avoidance-based coping have shown poorer psychological outcomes than men, including more severe depressive symptoms (Kort-Butler, 2009; Nummer & Seiffge-Krenke, 2001), while others have found that avoidance in men leads to higher rates of both alcohol use and suicidal ideation (Woodhead, Cronkite, Moos, & Timko, 2014).
In the Western Cape, methamphetamine use may be a common form of avoidance-based coping, due to the high levels of poverty and the widespread availability of the substance (Andersson et al., 2012; Hobkirk et al., 2016; Watt et al., 2014; Western Cape Government, 2015). Chronic methamphetamine use may even strengthen the pattern of avoidant coping, as it compromises neurocognitive capacity and increases prioritization of immediate gratification over long-term goals (Hoffman et al., 2006). Coping behaviors are believed to act as mediators in the relation between the experience of stress and an individual's emotional outcome (Lazarus, 1999). Previous research has found avoidant coping strategies (e.g., denial and mental or behavioral disengagement) to mediate the relation between victimization (i.e., childhood abuse and intimate partner violence) and psychological distress (Calvete, Corral, & Estevez, 2008; Choi et al., 2015; Johnson & Kenkel, 1991; Min et al., 2007). Therefore, we propose a model wherein CSA elicits traumatic stress that is temporarily alleviated through self-medication, and wherein this maladaptive coping strategy leads to poor trauma resolution and ultimately depressive symptomology. Few studies have examined the role of avoidant coping among South African samples; however, two recent studies have found substance use coping to contribute to depression and addiction among survivors of interpersonal violence in the Western Cape (Choi et al., 2015; Hobkirk et al., 2015). No study to date has examined the pathway from CSA to depressive symptoms through substance use coping among treatment seeking methamphetamine users in the area, which may provide insights into the needs of substance use treatment programs in the region.
In the present study, wehypothesize that substance use coping mediates the association between CSA and depression. Based on prior literature on gender differences in coping behaviors and outcomes, we hypothesize that gender will moderate the relation among CSA, substance use coping, and depression.
Methods
Setting
This study was conducted in two peri-urban townships in Cape Town: Mitchells Plain and Delft. The population of Mitchells Plain is approximately 300,000, which is twice as large as the population of Delft. The majority of the residents of Mitchells Plain are Coloured, while Delft's population consists of approximately equal proportions of Coloured and Black African residents (these terms originate from the Apartheid era and are still used as demographic markers referring to people of mixed versus African ancestry, respectively; Statistics South Africa, 2013, 2013a). Both townships have high rates of poverty, school dropout, unemployment, and substance-related crime (Plüddemann et al., 2010; Western Cape Government, 2015). In the past decade, the City of Cape Town has opened a city-funded outpatient drug rehabilitation center in each township, and both have since been certified by the UCLA-based Matrix Institute. The Matrix clinics provide a 16-week treatment program, which includes recovery skills training, family education, and relapse prevention, followed by continuing social support for those who complete the program. All services are free and open to the public (City of Cape Town, 2010, 2012).
Participants
The sample included methamphetamine users who presented for substance abuse treatment at the Matrix clinics in Mitchells Plain and Delft. The clinics accept patients on a “walk-in” basis. Clinic staff administered an initial screening to determine eligibility for the study. Inclusion criteria were: ≥ 18 years of age, self-reported methamphetamine use in the past 3 months, and ability to provide informed consent. Eligible subjects were informed that participation in this study would not affect their treatment at the Matrix clinic.
Procedures
After providing written consent, participants completed a 30- to 50-minuteaudio computer-assisted self-interview (ACASI) to assess clinical and behavioral measures. This tool measured childhood trauma, depressive symptoms, and substance use coping behaviors. The survey was programmed using QDS™ 2.6 software (NOVA Research Company, Bethesda, MD, US), and was offered in English, Afrikaans, and Xhosa. Clinic staff conducted a face-to-face clinical interview that measured demographic data and patterns and severity of substance use. Participants were compensated with a gift bag valuing $5. All procedures were approved by the Duke University Health System Institutional Review Board and the University of Cape Town Human Research Ethics Committee.
Measures
Methamphetamine use characteristics
The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) assessed patterns and severity of methamphetamine use (World Health Organization, 2010). Participants were asked to report frequency of methamphetamine use, cravings, and problems related to use in the past three months, as well as total number of prior quit attempts. According to the guidelines of the screening test, a specific substance involvement (SSI) score was calculated for methamphetamine to determine the risk level associated with use. A score of 4 or above indicates moderate risk, which suggests that the individual has the potential for dependence and future health problems. A score of 27 or above indicates high risk, which suggests that the individual may be experiencing “health, social, financial, legal and relationship problems as a result oftheir substance use” (WHO 2010). Across both high- and low-income countries, this tool has demonstrated high internal reliability (α = 0.89) and high discriminative validity between moderate- and high-risk scores (Humeniuk et al., 2008). In this study, the six items used to calculate SSI for methamphetamine were found to have moderate internal reliability (α = 0.63).
Childhood sexual abuse
CSA was measured using three items from the 5-item sexual abuse subscale of the Childhood Trauma Questionnaire (CTQ; Bernstein et al., 1994): (1) Did anyone try to touch you or make you touch them in a sexual way? (2) Did anyone threaten you unless you did something sexual? (3) Did anyone force you to have sexual intercourse? For brevity, two items from the original subscale were excluded, and responses were either yes or no. Participants were considered to have experienced CSA if they endorsed one or more of the items. The three-item scale was found to have high internal reliability (α = 0.80).
Depressive symptoms
The nine-item Patient Health Questionnaire (PHQ-9) assessed symptoms indicative of depression (Kroenke, Spitzer, & Williams, 2001). Participants rated how often they had experienced each of the nine symptoms over the past two weeks (0 = not at all; 1 = several days; 2 = more than half of the days; 3 = nearly every day), and the ratings were summed for a composite score from 0 to 27. Cutoffs of 5, 10, 15, and 20 were used to approximate the lower boundaries of mild, moderate, moderately severe, and severe depressive symptoms, respectively. These cutoffs have high sensitivity and specificity in predicting likelihood of a major depression diagnosis (Kroenke et al., 2001), and the scale has been validated for use in primary care settings in South Africa (Cholera et al., 2014). This scale had high internal consistency in the current sample (α = 0.88).
Substance use coping
The four substance-related items of the COPE Inventory assessed participants' responses to stress (Carver, Scheier, & Weintraub, 1989). Participants were asked to read brief statements about coping, such as ‘When I am under a lot of stress or I feel bad about past events, I use alcohol or drugs to make myself feel better,’ and to rate how often they endorse each one (1 = never or rarely; 2 = occasionally; 3 = often; 4 = almost always). Ratings were summed for a composite score from 4 to 16, with higher scores indicating more frequent usage of substance use coping. This subscale had high internal consistency in the current sample (α = 0.88).
Data analysis
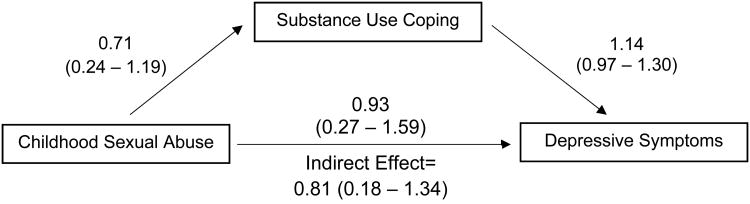
Analyses were conducted using SPSS Statistics version 22 (IBM Corp., 2013). Descriptive statistics were conducted to describe the sample, and chi-square analyses, t-tests, and Pearson correlations examined associations between relevant variables. Linear regression was used to determine if substance use coping mediated the association between CSA and depressive symptoms. To test if the association of childhood sexual abuse and depressive symptoms were mediated by substance use coping, we used model 4 of the PROCESS macro (version 2.13) for SPSS (www.processmacro.org). To examine gender as a potential moderator of this model, moderated mediation was tested using model 7 of the PROCESS macro. The PROCESS macro uses bootstrapping with 1000 iterations to determine a 95% confidence interval foreach unstandardized regression coefficient as well as the indirect effect of CSA on depression through substance use coping. In our analysis, CSA was measured by the CTQ, substance use coping was measured by the brief COPE, and depressive symptoms weremeasured by the PHQ-9 (see Figure 1). Given that this is a cross-sectional study with the potential for reverse causal effects, model 4 of the PROCESS macro was again used to test for mediation with substance use coping as the outcome and depression as the mediator.
Figure 1.
Mediation model of the indirect effect of childhood sexual abuse on depressive symptoms through substance use coping. Unstandardized regression coefficients and 95% confidence intervals are presented for each path.
Results
The sample included 269 treatment-seeking methamphetamine users, 60% of whom were men (see Table 1). The average age was 28.4 years (SD = 6.14) and ranged from 18 to 54. The majority of the sample identified with the apartheid-derived demographic category of “Coloured”, while less than 5% identified as Black African. The majority of the sample (89%) reported usingmethamphetamine at least weekly in the past three months, and 83% reported problems related to use in the past 3 months. The average substance risk severity score for methamphetamine use was 29.5 (SD = 8.59), which exceeds the threshold of high risk. Participants reported using alcohol (54%), marijuana (60%), opioids (e.g., heroin) (13%), and other illicit substances (e.g., mandrax) (45%) in the past 3 months.
Table 1. Participant characteristics across childhood sexual abuse.
| Variable | Childhood Sexual Abuse(n = 81) | No Childhood Sexual Abuse(n = 188) | X2 or t |
|---|---|---|---|
| Demographics | |||
| Age | 28.30 (5.66) | 28.38 (6.35) | 0.10 |
| Female gender | 49 (61%) | 59 (31%) | 19.96*** |
| Highest grade level | 9.57 (2.02) | 9.61 (1.88) | 0.15 |
| Unemployed | 67 (82.7%) | 155 (82.4%) | 0.01 |
| Methamphetamine-related Characteristics | |||
| Weeklyor more methamphetamine use | 73 (90.1%) | 164 (88.2%) | 0.22 |
| Any methamphetamine-related problems | 70 (89.7%) | 150 (80.6%) | 3.28 |
| Prior unsuccessful quit attempts | 76 (93.8%) | 164(87.2%) | 2.56 |
| Methamphetamine involvement score | 30.52(6.88) | 29.06(9.21) | 1.28 |
| High-risk methamphetamine use (SSI ≥ 27) | 63 (77.8%) | 136 (72.3%) | 0.87 |
| Depression | |||
| PHQ-9 total score | 14.60 (6.87) | 11.07 (6.79) | 0.60 |
| Above threshold of moderate severity (≥15) | 39 (48.1%) | 58 (30.9%) | 7.34** |
| Substance Use Coping | |||
| COPE total score | 11.51 (3.86) | 9.89 (3.77) | 3.19** |
| To make myself feel better | 3.00 (1.04) | 2.62 (1.13) | 2.61** |
| To try to lose myself for a while | 2.74 (1.08) | 2.31 (1.12) | 2.90** |
| To think less about stress/past events | 2.91 (1.05) | 2.48 (1.14) | 2.95** |
| To help me get through it | 2.85 (1.06) | 2.48 (1.14) | 2.48* |
Note
p<.05;
p<.01;
p<.001.
The mean depressive symptom score was 12.1 (SD = 6.99), and over a third of participants exceeded the threshold for moderate depressive symptom severity (≥ 15). The average substance use coping score was 10.4 (SD = 3.86). The level of substance use coping was not related to the severity of methamphetamine use risk (X2(1) = 3.34, p = .07), with only 51% of participants in the high-risk group also reporting high levels of substance use coping. There were no significant differences in depressive symptoms or substance use coping across gender [t(267) = 0.60, p = .55 and t(267) = 0.48, p = .63, respectively].
Almost a third of participants reported a history of CSA, including 20% of men and 45% of women. Women were significantly more likely to endorse each of the three CSA items: being touched in a sexual way (X2(1) = 17.06, p< .001), threatened unless I did something sexual (X2(1) = 12.25, p < .01), and forced sexual intercourse (X2(1) = 9.99, p< .01). While CSA was not associated with severity of methamphetamine use risk, it was associated with a higher frequency of substance use coping and depressive symptoms (see Table 1). Correlations among the primary study variables are displayed in Table 2.
Table 2. Bivariate correlations among study variable total scores.
| Variable | Childhood Sexual Abuse | Substance Use Coping |
|---|---|---|
| Substance Use Coping | .180** | - |
| Depressive Symptoms | .243*** | .651** |
Note.
p<.05;
p<.01;
p<.001.
For the mediation analysis, the indirect effect of CSA on depressive symptoms through substance use coping was significant with a 95% confidence interval that did not include 0. Figure 1 shows the unstandardized regression coefficients and 95% confidence intervals of each path in the model. The indirect effect of CSA on depressive symptoms through substance use coping was 0.81, and statistically significant with a 95% confidence interval of 0.18 - 1.34. Gender was not a significant moderator of the mediation analysis (interaction B = 0.11, p = .824).The second mediation model with depression as the mediator and substance use coping as the outcome variable showed a significant indirect effect (0.62 [0.34 – 0.95]), suggesting that reverse causal effects exist for the current model.
Discussion
In this sample of adult methamphetamine users entering substance abuse treatment in South Africa, CSA was associated with more self-reported substance use coping and depressive symptoms. Analyses revealed that substance use coping mediated the link between CSA and depressive symptoms. The rates of CSA in the current sample were similar to those found in a community sample of methamphetamine users in this region (Watt, Kimani, Skinner, & Meade, 2015). This consistently high rate of CSA among South African drug users underscores the importance of assessing trauma in patients presenting for substance abuse treatment, as an access point to trauma-related care. In the current study, the rates of CSA for women were over two times higher than those found among women in the general South African population, while the rates for men were similar to the general population (Andersson et al., 2012). Although women reported a higher prevalence of CSA than men, gender did not moderate the current mediation model.
Given the high comorbidity and overlapping time course of CSA, substance use coping, and depression, other models may also explain their association. Among the current sample, an alternative model consistent with the self-medication hypothesis, such that depression mediatesthe link between CSA and substance use coping, was also supported, albeit with a smaller indirect effect size than our hypothesized model (Khantzian, 1997). Thus, it seems likely that depression is both a cause and a consequence of substance use coping, and therefore should be assessed for and treated at all stages in this continuum. Longitudinal research is needed to ascertain the temporal progression of substance use coping and depression after a traumatic experience.
Coping interventions that have been effective in reducing trauma-related sequelae could provide individuals with better skills for managing stress relating to prior trauma experiences, such as CSA (Kiser, Donohue, Hodgkinson, Medoff, & Black, 2010; Salloum & Overstreet, 2012; Sikkema et al., 2013; Tol et al., 2008). The association between CSA, substance use coping and depressive symptoms suggests that methamphetamine users could benefit from such programs. Coping interventions teach individuals to more accurately appraise stressors in order to choose more effective methods of coping, and such interventions could be targeted specifically to address trauma-related stressors. As social support is an important factor in approach-based coping, training programs should be accompanied by initiatives to reduce community-based stigma against abuse survivors. Many organizations worldwide, including the United Nations, Amnesty International, and CARE, have implemented educational media campaigns to improve public treatment of women with histories of sexual abuse (Amnesty International, 2015; CARE, 2013; United Nations, 2013). Our results suggest that these efforts should be continued and expanded to include men. Improving public awareness of the prevalence and consequences of CSA for both men and women may reduce stigma, thereby creating more opportunities for individuals to employ approach-based coping strategies. Integrated treatment models that address both trauma-related stress and substance use have shown preliminary success in several recent effectiveness trials (Swopes, Davis, & Scholl, 2015; Wolff et al., 2015) andrandomized controlled trials (Mills et al., 2012; van Dam, Ehring, Vedel, & Emmelkamp, 2013), and may be effective in this setting.
Future research would benefit from examining the influence of other potentially traumatic experiences on psychological outcomes. The focus on CSA may have limited the scope of the present study, given that individuals who use substances to cope may be responding to a broad range of stressors that continue into adulthood, which would further complicate the temporal relation with psychological outcomes. Substance use, and the lifestyle that often accompanies it, is associated with a range of new stressors, such as intimate partner violence, criminal behavior, and poverty. For example, for women in the context of poverty, sex trading is a common means of acquiring more drugs, and it is associated with violence against women and HIV risk (Watt et al., 2015). Thus, the depressive symptoms explored in this study may be the result of a broader range of potentially traumatic experiences, not only CSA. The experience of other forms of child maltreatment, such as physical abuse or neglect, might contribute to both substance use coping and depression. Previous studies have suggested that in cases of poly-victimization, focusing on a single type of maltreatment overestimates the direct relation with posttraumatic outcomes (Collings, Pennings, & Valjee, 2014; Turner, Finkelhor, & Ormrod, 2010). In this study, poly-victimization might account for a significant portion of the association between CSA, substance use coping, and depression, thereby reducing the significance of CSA as an independent factor.
The findings also link substance abuse to depression, which suggests that individuals may benefit from programs that integrate depression and substance use treatment. Several recent studies have demonstrated the effectiveness of such models (Morley et al., 2016; Wüsthoff, Waal, & Gråwe, 2014), and one randomized controlled trial has found success in simultaneously treating trauma, substance use, and depression (Danielson et al., 2012). Given that all participants in this study were currently seeking substance use treatment, integrated models such as these could help individuals in need of trauma-related and/or depression treatment access care, through existing treatment centers for substance abuse like the Matrix clinics. Future studies should explore the relationship among trauma, substance use coping, and other psychological outcomes, such as anxiety or traumatic stress disorder, in order to further inform such integrated models.
This study has several noteworthy limitations, with implications for future research. First, due to the primary focus on drug use, this study examined only a small subset of coping behaviors. A more comprehensive assessment of multiple types of approach- and avoidance-based coping strategies could provide insight into the proposed mediationmodels. In addition, when participants reported their coping behavior, they were not asked to indicate with what stressor they were coping. Increasing the breadth and specificity of the coping assessment would improve future studies.
Additionally, this sample may not accurately represent the entire methamphetamine-using population of this region. Black Africans were under-represented as compared to the demographics of the two townships, but it has been suggested that methamphetamine use is less prevalent among Black Africans in this setting (Dada et al., 2015). More notably, the sample included only methamphetamine users that were currently seeking treatment. Seeking substance use treatment is itself a form of approach-based coping, and the large majority of methamphetamine users in this setting do not seek treatment (Meade et al., 2015). Therefore, these results may not generalize to the larger population of methamphetamine users.
In conclusion, given the high prevalence of CSA among methamphetamine users and its relation to both substance use and depressive symptoms, publicly-available substance abuse treatment centers may provide an opportunity to identify individuals who might benefit from trauma-focused coping interventions. Our findings call for interventions that improve coping skills at the individual level and increase public awareness at the societal level. Future research should aim to explore other stressors and other coping behaviors that contribute to the pathway to depression. Through integration of trauma-related coping and depression treatmentswith existing substance use treatment programs, we see a potential opportunity to empower methamphetamine users to more effectively cope with past trauma and achieve superior psychological outcomes.
Acknowledgments
This study was funded by the Duke University Center for AIDS Research (P30-AI0645180), with additional support from the National Institute on Drug Abuse (K23-DA028660, R03-DA033828, F32-DA038519). An Atlantic Coast Conference Inter-Institutional Academic Collaborative Fellowship from Duke University and a Bains Family Independent Research Grant from the Duke Global Health Institute provided the first author (MKB) with funds for travel and living expenses in South Africa. We thank Dr. Hetta Gouse, Daniella Cordero, and Ryan Lion for their assistance with data collection and management. We also thank Mr. Warren Burnhams, Ms. Sadieqa Barodien, and the Matrix clinic staff for their assistance with participant recruitment and interviewing. This analysis was conducted as part of an undergraduate honors thesis by the first author (MKB).
References
- Amnesty International. Violence against women: End the cycle of violence. 2015 http://www.amnestyusa.org/our-work/issues/women-s-rights/violence-against-women.
- Andersson N, Paredes-Solís S, Milne D, Omer K, Marokoane N, Laetsang D, Cockcroft A. Prevalence and risk factors for forced or coerced sex among school-going youth: National cross-sectional studies in 10 southern African countries in 2003 and 2007. BMJ Open. 2012;2(2) doi: 10.1136/bmjopen-2011-000754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. http://dx.doi.org/10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Brown DW, Riley L, Butchart A, Meddings DR, Kann L, Phinney-Harvey A. Exposure to physical and sexual violence and adverse health behaviours in African children: Results from the Global School-based Student Health Survey. Bulletin of the World Health Organization. 2009;87:447–455. doi: 10.2471/BLT.07.047423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvete E, Corral S, Estevez A. Coping as a mediator and moderator between intimate partner violence and symptoms of anxiety. Violence Against Women. 2008;14(8):886–904. doi: 10.1177/1077801208320907. [DOI] [PubMed] [Google Scholar]
- CARE. CARE's work to end gender-based violence. 2013 http://www.care.org/impact/stories/cares-work-end-gender-based-violence.
- Carey PD, Walker JL, Rossouw W, Seedat W, Stein DJ. Risk indicators and psychopathology in traumatized children and adolescents with a history of sexual abuse. European Child and Adolescent Psychiatry. 2008;17:93–98. doi: 10.1007/s00787-007-0641-0. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. http://dx.doi.org/10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Choi KW, Sikkema KJ, Velloza J, Marais A, Jose C, Stein DJ, Joska JA. Maladaptive coping mediates the influence of childhood trauma on depression and PTSD among pregnant women in South Africa. Archives of Women's Mental Health. 2015;18(5):731–738. doi: 10.1007/s00737-015-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cholera R, Gaynes BN, Pence BW, Bassett J, Qangule N, Macphail C, Miller WC. Validity of the Patient Health Questionnaire-9 to screen for depression in a high-HIV burden primary healthcare clinic in Johannesburg, South Africa. Journal of Affective Disorders. 2014;167:160–166. doi: 10.1016/j.jad.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- City of Cape Town. Tafelsig Matrix treatment clinic internationally certified as a ‘programme of excellence’ [Press release] 2010 https://www.capetown.gov.za/en/MediaReleases/Pages/TafelsigMatrixtreatmentclinicinternationallycertifiedasaprogrammeofexcellence.aspx.
- City of Cape Town. City's Delft South Matrix clinic to receive certificate of excellence in recognition of its rehabilitation programmes. 2012 https://www.capetown.gov.za/en/achievementsandawards/Pages/CityDelftSouthMatrixClinreceiveCertofExcel.aspx.
- Collings SJ. The long-term effects of contact and noncontact forms of child sexual abuse in a sample of university men. Child Abuse & Neglect. 1995;19(1):1–6. doi: 10.1016/0145-2134(94)00098-F. [DOI] [PubMed] [Google Scholar]
- Collings SJ, Pennings SL, Valjee SR. Lifetime poly-victimization and posttraumatic stress disorder among school-going adolescents in Durban, South Africa. Journal of Psychiatry. 2014;17(5):133–137. doi: 10.4172/psychiatry.1000133. [DOI] [Google Scholar]
- Dada S, Burhams NH, Williams Y, Erasmus J, Parry C, Bhana A, Fourie D. Alcohol & Drug Abuse Research Unit. Medical Research Council; Cape Town, South Africa: 2015. Monitoring alcohol, tobacco and drug abuse treatment admissions in South Africa (July-December 2014) [Google Scholar]
- Danielson CK, McCart MR, Walsh K, de Arellano MA, White D, Resnick HS. Reducing substance use risk and mental health problems among sexually assaulted adolescents: A pilot randomized controlled trial. Journal of Family Psychology. 2012;26(4):628–635. doi: 10.1037/a0028862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug and Alcohol Review. 2008;27:253–262. doi: 10.1080/09595230801923702. [DOI] [PubMed] [Google Scholar]
- Hobkirk AL, Watt MH, Green KT, Beckham JC, Skinner D, Meade CS. Mediators of interpersonal violence and drug addiction severity among methamphetamine users in Cape Town, South Africa. Addictive Behaviors. 2015;42:167–171. doi: 10.1016/j.addbeh.2014.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobkirk AL, Watt MH, Myers B, Skinner D, Meade CS. A qualitative study of methamphetamine initiation in Cape Town, South Africa. International Journal of Drug Policy. 2016;30:99–106. doi: 10.1016/j.drugpo.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman WF, Moore M, Templin R, McFarland B, Hitzermann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology. 2006;188:162–170. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikam J, Simon S. Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South Africa youth. Child Abuse & Neglect. 2010;34:833–841. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BK, Kenkel MB. Stress, coping, and adjustment in female adolescent incest victims. Child Abuse & Neglect. 1991;15(3):293–305. doi: 10.1016/0145-2134(91)90073-M. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King G, Flisher AJ, Noubary F, Reece R, Marais A, Lombard C. Substance abuse and behavioral correlates of sexual assault among South African adolescents. Child Abuse & Neglect. 2004;28(6):683–696. doi: 10.1016/j.chiabu.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Kiser LJ, Donohue A, Hodgkinson S, Medoff D, Black MM. Strengthening family coping resources: The feasibility of a multifamily group intervention for families exposed to trauma. Journal of Traumatic Stress. 2010;23(6):802–806. doi: 10.1002/jts.20587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kort-Butler LA. Coping styles and sex differences in depressive symptoms and delinquent behavior. Journal of Youth and Adolescence. 2009;38:122–136. doi: 10.1007/s10964-008-9291-x. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS. Stress and coping: A new synthesis. New York, NY: Springer; 1999. [Google Scholar]
- Leeies M, Pagura J, Sareen J, Bolton JM. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depression and Anxiety. 2010;27(8):731–736. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Madu SN, Peltzer K. Risk factors and child sexual abuse among secondary school students in the Northern Province (South Africa) Child Abuse & Neglect. 2000;24(2):259–268. doi: 10.1016/s0145-2134(99)00128-3. [DOI] [PubMed] [Google Scholar]
- Mbwambo J, McCurdy SA, Myers B, Lambdin B, Kilonzo GP, Kaduri P. Drug trafficking, use, and HIV risk: The need for comprehensive interventions. SAHARA-J: Journal of Social Aspects of HIV/AIDS. 2012;9(3):154–159. doi: 10.1080/17290376.2012.743832. [DOI] [PubMed] [Google Scholar]
- Meade CS, Watt MH, Sikkema KJ, Deng LX, Ranby KW, Skinner D, Kalichman SC. Methamphetamine use is associated with childhood sexual abuse and HIV sexual risk behaviors among patrons of alcohol-serving venues in Cape Town, South Africa. Drug and Alcohol Dependence. 2012;126(1-2):232–239. doi: 10.1016/j.drugalcdep.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Towe SL, Watt MH, Lion RR, Myers B, Skinner D, Pieterse D. Addiction and treatment experiences among active methamphetamine users recruited from a township community in Cape Town, South Africa: a mixed-methods study. Drug and Alcohol Dependence. 2015;152:79–86. doi: 10.1016/j.drugalcdep.2015.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min M, Farkas K, Minnes S, Singer LT. Impact of childhood abuse and neglect on substance abuse and psychological distress in adulthood. Journal of Traumatic Stress. 2007;20(5):833–844. doi: 10.1002/jts.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley KC, Baillie A, Leung S, Sannibale C, Teesson M, Haber PS. Is specialized integrated treatment for comorbid anxiety, depression and alcohol dependence better than treatment as usual in a public hospital setting? Alcohol and Alcoholism. 2016;51(4):402–409. doi: 10.1093/alcalc/agv131. [DOI] [PubMed] [Google Scholar]
- Morris MC, Kouros CD, Fox KR, Rao U, Garber J. Interactive models of depression vulnerability: The role of childhood trauma, dysfunctional attitudes, and coping. British Journal of Clinical Psychology. 2014;53:245–263. doi: 10.1111/bjc.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nummer G, Seiffge-Krenke I. Can differences in stress perception and coping explain sex differences in depressive symptoms in adolescents? Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2001;29(2):89–97. doi: 10.1024//1422-4917.29.2.89. [DOI] [PubMed] [Google Scholar]
- Plüddemann A, Myers BJ, Parry CD. Surge in treatment admissions related to methamphetamine use in Cape Town, South Africa: Implications for public health. Drug and Alcohol Review. 2008;27(2):185–189. doi: 10.1080/09595230701829363. [DOI] [PubMed] [Google Scholar]
- Plüddemann A, Flisher AJ, McKetin R, Parry C, Lombard C. Methamphetamine use, aggressive behavior and other mental health issues among high-school students in Cape Town, South Africa. Drug and Alcohol Dependence. 2010;109:14–19. doi: 10.1016/j.drugalcdep.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: A longitudinal investigation. Archives of General Psychiatry. 2011;68(8):800–807. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- Roth S, Cohen LJ. Approach, avoidance, and coping with stress. American Psychology. 1986;41(7):813–819. doi: 10.1037//0003-066x.41.7.813. http://dx.doi.org/10.1037/0003-066X.41.7.813. [DOI] [PubMed] [Google Scholar]
- Salloum A, Overstreet S. Grief and trauma intervention for children after disaster: Exploring coping skills versus trauma narration. Behaviour Research and Therapy. 2012;50:169–179. doi: 10.1016/j.brat.2012.01.001. [DOI] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 Jun; URL: http://quantpsy.org/
- Sikkema KJ, Ranby KW, Meade CS, Hansen NB, Wilson PA, Kochman A. Reductions in traumatic stress following a coping intervention were mediated by decreases in avoidant coping for people living with HIV/AIDS and childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2013;81(2):274–283. doi: 10.1037/a0030144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science & Medicine. 2006;63(8):2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics South Africa. City of Cape Town - 2011 Census Suburb Delft 2013 [Google Scholar]
- Statistics South Africa. City of Cape Town - 2011 Census Suburb Mitchells Plain 2013a [Google Scholar]
- Statistics South Africa. South Africa's young children: Their family and home environment, 2012 2013b [Google Scholar]
- Stoltenborgh M, van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ. A global perspective on child sexual abuse: Meta-analysis of prevalence around the world. Child Maltreatment. 2011;16(2):79–101. doi: 10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- Swopes RM, Davis JL, Scholl JA. Treating substance abuse and trauma symptoms in incarcerated women: An effectiveness study. Journal of Interpersonal Violence. 2015 doi: 10.1177/0886260515587668. [DOI] [PubMed] [Google Scholar]
- Tol WA, Komproe IH, Susanty D, Jordans MJ, Macy RD, De Jong JT. School-based mental health intervention for children affected by political violence in Indonesia: A cluster randomized trial. Journal of the American Medical Association. 2008;200(6):655–662. doi: 10.1001/jama.300.6.655. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. American Journal of Preventive Medicine. 2010;38(3):323–330. doi: 10.1016/j.amepre.1009.11.012. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Relyea M, Peter-Hagene L, Vasquez AL. Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive Behaviors. 2013;38(6):2219–2223. doi: 10.1016/j.addbeh.2013.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. UNiTE to end violence against women. 2013 http://www.un.org/en/women/endviolence/
- United Nations Office on Drugs and Crime. World Drug Report 2014. Vienna, Austria: United Nations; 2014. [Google Scholar]
- van Dam D, Ehring T, Vedel E, Emmelkamp PM. Trauma-focused treatment for posttraumatic stress disorder combined with CBT for severe substance use disorder: A randomized controlled trial. BMC Psychiatry. 2013;13(172) doi: 10.1186/1471-244X-13-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Meade CS, Kimani S, McFarlane JC, Choi KW, Skinner D, Sikkema KJ. The impact of methamphetamine (“tik”) on a peri-urban community in Cape Town, South Africa. The International Journal on Drug Policy. 2014;25(2):219–225. doi: 10.1016/j.drugpo.2013.10.007. http://dx.doi.org/10.1016/j.drugpo.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Kimani SM, Skinner D, Meade CS. Nothing is free: A qualitative study of sex trading among methamphetamine users in Cape Town, South Africa. Archives of Sexual Behavior. 2015;45(4):923–933. doi: 10.1008/s10508-014-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Western Cape Government. Report on the Western Cape Policing Needs and Priorities: 2014/2015. Western Cape, South Africa: Hanekom et al; 2015. [Google Scholar]
- Wolff N, Huening J, Shi J, Frueh BC, Hoover DR, McHugo G. Implementation and effectiveness of integrated trauma and addiction treatment for incarcerated men. Journal of Anxiety Disorders. 2015;30:66–80. doi: 10.1016/j.janxdis.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong FY, Huang ZJ, DiGangi JA, Thompson EE, Smith BD. Gender differences in intimate partner violence on substance abuse, sexual risks, and depression among a sample of South Africans in Cape Town, South Africa. AIDS Education & Prevention. 2008;20(1):56–64. doi: 10.1521/aeap.2008.20.1.56. [DOI] [PubMed] [Google Scholar]
- Woodhead EL, Cronkite RC, Moos RH, Timko C. Coping strategies predictive of adverse outcomes among community adults. Journal of Clinical Psychology. 2014;70(12):1183–1195. doi: 10.1002/jclp.21924. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The alcohol, smoking and substance involvement screening test (ASSIST) Geneva, Switzerland: Humeniuk et al; 2010. [Google Scholar]
- Wüsthoff LE, Waal H, Gråwe RW. The effectiveness of integrated treatment in patients with substance use disorders co-occurring with anxiety and/or depression - A group randomized trial. BMC Psychiatry. 2014;14:67–78. doi: 10.1186/1471-244X-14-67. http://www.biomedcentral.com/1471-244X/14/67. [DOI] [PMC free article] [PubMed] [Google Scholar]