Abstract
Background
Despite the temporal increase in cesarean deliveries, the extent to which maternal age, period, and maternal birth cohorts may have contributed to these trends remains unknown.
Methods
We performed an analysis of 123 million singleton deliveries in the US (1979-2010). We estimated rate ratio (RR) with 95% confidence interval (CI) for primary and repeat cesarean deliveries. We examined changes in cesarean rates with weighted Poisson regression models across three time-scales: maternal age, year of delivery, and birth cohort (mother’s birth year).
Results
The primary cesarean rate increased by 68% (95% confidence interval (CI) 67%, 69%) between 1979 (11.0%) and 2010 (18.5%). Repeat cesarean deliveries increased by 178% (95% CI 176, 179) from 5.2% in 1979 to 14.4% in 2010. Cesarean rates increased with advancing age. Compared to 1979, the RR for the period effect in primary and repeat cesarean deliveries increased up to 1990 fell to a nadir at 1993 and began to rise thereafter. A small birth cohort effect was evident, with women born prior to 1950 at increased risk of primary cesarean; no cohort effect was seen for repeat cesarean deliveries. Adjustment for maternal BMI had a small effect on these findings. Period effects in primary cesarean were explained by a combination of trends in obesity and chronic hypertension as well as demographic shifts over time.
Conclusions
Maternal age and period appear to have important contributions to the temporal increase in the cesarean rates, although the effect of parity on these associations remains undetermined.
Keywords: Age-period-cohort analysis, Cesarean delivery, Primary cesarean, Repeat cesarean, Cesarean indications, Ischemic placental disease, Temporal trends, Obesity
Introduction
Nearly one in three infants today is delivered by cesarean, making the surgery one of the most common procedures in the US. The rate of cesarean delivery has increased in most industrialized countries with the rate rising in the US from 5.5% in 19701 to 32.2% in 20142,3– a relative increase of 500% in the ensuing four decades. Encouragement from the American Congress of Obstetricians and Gynecologists to promote vaginal deliveries following cesarean in the late 1980s4 led to a decline in the cesarean delivery rate between 1989 and 1995 (and a concurrent increase in the rate of vaginal birth after cesarean). However, amidst concerns for maternal and adverse perinatal outcomes associated with the low cesarean rate,5,6 especially among high-risk women, the cesarean rate began to rise again. A variety of maternal and fetal factors have been implicated in the rising cesarean rates of both primary and repeat cesarean deliveries, including non-reassuring fetal status, ischemic placental disease7,8 (preeclampsia, intrauterine growth restriction, and placental abruption), fetal malpresentation, and complications of labor.9 A prior cesarean delivery is the chief indication for a repeat cesarean.
Despite extensive research, important factors in the increasing cesarean delivery rate remain unexplored. These include (i) an evaluation of the extent to which primary and repeat cesarean deliveries have increased at the population-level in the US; (ii) how indications for cesarean deliveries have changed temporally, and how such changes may have affected primary and repeat cesarean delivery rates; and (iii) the role maternal birth cohorts may have played in these trends. To address these shortcomings, we performed an age-period-cohort (APC) analysis. An APC analysis is a simultaneous examination of how changes in three time-related factors – maternal age, period (year of occurrence of cesarean) and maternal birth cohort (maternal birth year) – affect changes in an outcome. Temporal changes in cesarean delivery rates are the object of many studies,10-14 as is maternal age.11 An examination of the effects of maternal birth cohorts has been neglected, but can provide important insights to understand the profile of cesarean deliveries. For instance, if the cesarean delivery rate changes by maternal age across birth cohorts, this may provide important clues to how a woman’s early life exposures and her age at delivery (an interaction) shape cesarean risk.
The objectives of this paper are to delineate, through an APC analysis, the effects of maternal age, period and birth cohort on trends in both primary and repeat cesarean deliveries in the US, as well as cesarean trends based on the underlying indications. Given the surge in obesity prevalence in the US over the last two decades, we hypothesized that birth cohort may have contributed to these trends. We address these objectives in a population-based study of over 123 million singleton births in the US.
Methods
The National Hospital Discharge Survey (NHDS)
We designed a retrospective cohort analysis utilizing the NHDS data between 1979 and 2010 to examine how age, period and birth cohorts have affected the changes in overall and primary and repeat cesarean deliveries in the US. The NHDS data was assembled by the US Centers for Disease Control and Prevention. These data are based on hospitalizations from short-stay (<30 days) hospitals, and non-federal general and specialty hospitals. The data included in the survey is representative sample of hospital discharges in the 50 states and the District of Columbia. Since the NHDS data are completely de-identified and publicly available, no ethics approval was sought.
Between 1979 and 1987, the NHDS data collection was based on a two-stage stratified sampling design and since 1988, a modified three-stage design.15,16 The number of hospitals surveyed each year ranged between 400 and 558 and included roughly 181,000 to over 300,000 hospital discharges each year. Since 2008, the number of hospitals chosen was reduced to 200 to 300 hospitals. The NHDS data includes a sampling weight and when these weights are incorporated during statistical analyses, the data generalize to all in-patient hospitalizations leading to a delivery in the US.
Indications for cesarean deliveries
The NHDS does not record the indications for cesarean deliveries. Instead, we identified maternal and fetal conditions that may presumably have led to a cesarean. These indications were broadly classified as (i) non-reassuring fetal status; (ii) ischemic placental disease that included preeclampsia, fetal growth restriction, and placental abruption; (iii) malpresentation that included breech and transverse lie; and (iv) labor complications that included arrest of labor (abnormal uterine forces, disproportion) and suspected fetal macrosomia. For repeat cesarean deliveries, we additionally examined previous cesarean delivery as an indication. All diagnoses and procedures in the NHDS were coded based on the International Classification of Disease, 9th revision, Clinical Modification (ICD9-CM) and codes to define the indications are shown in eTable 1. The NHDS lacked data on parity, so whether APC trends differ between women with primary cesarean delivery in their first versus other pregnancies remains a limitation.
Age-Period-Cohort Analysis
Through an APC methodology, we examined temporal changes in rates of primary and repeat deliveries. Age, period, and birth cohort effects were modeled, in single years, through a Poisson regression. One of the challenges of an APC analysis is the “identifiability” issue since APC effects are perfectly collinear (cohort=period-age);17,18 this complicates the estimation of parameters in the models. Specifically, constraints need to be placed on the model and assumptions need to be made about the underlying relationships among APC factors in order to estimate the parameters in the model.
To address the identifiability problem, we adopted a classical approach common in epidemiologic studies of health outcomes.19 In this approach, we iteratively fit model parameters and assessed model fit through a series of constraints. First, an age parameter was included in the model. Then, an overall linear trend in cesarean delivery rates was included; this linear trend cannot be uniquely attributed to either period or cohort effects, but rather to the sum of the linear component of period and cohort effects. We refer to this estimate as the “drift” parameter. We then assessed deviations from linearity that can be uniquely attributed to the period and cohort effects; we refer to this as the “curvature” effect. These parameter estimates can be interpreted as the direction and magnitude of the change in the linear trend by period and cohort. We determined all models a priori and sequentially fit them beginning with age only, and then adding drift and subsequently period and cohort independently and in combination. Non-linear APC effects on cesarean deliveries were modeled as flexible smooth functions based on natural splines with 6 knots each for age, period and birth cohorts. The APC modeling was performed using the “apc.fit” function in the “Epi” package20 in the R programming language (version 3.1.1; Vienna, Austria).
Sensitivity analyses
We carried out four sets of sensitivity analyses. First, we examined if the APC effects on primary and repeat cesarean deliveries differed between black and white women; this was conducted as a sensitivity analysis since 23.3% of deliveries had missing data on race in the NHDS. Second, since cesarean deliveries have been increasing overall as well as among women considered “low-risk”,21 we examined APC effects for primary cesarean delivery in low-risk women. We identified the subset of low-risk women as those without non-reassuring fetal status, malpresentation, ischemic placental disease, long labor, abnormal labor, cord complications, failed medical or mechanical induction, disproportion, or placenta previa or vasa previa. In addition, we also excluded women that delivered at preterm gestational age (<37 weeks).
Third, given that all APC models are subject to criticism due to unverifiable assumptions in order for model identification,22 assessment of the robustness of results across different types of models provides reassurance that results are unbiased to model constraints. We assessed APC effects for primary and repeat cesarean deliveries using the hierarchical APC model23 which uses a cross-classified random effects approach. Using a general form of a Poisson regression model, we first fit a “within” model, with cesarean rates predicted by an intercept, age as a categorical scalar variable, and an error term. Then, period and cohort were modeled as random effects in a “between” model, predicting the intercept of the “within” model. The central difference between our primary approach and the hierarchical APC model is the way in which we parameterize period and cohort estimates; in the primary approach, period and cohort estimates are first derivatives of the linear trend. In the hierarchical approach, period and cohort estimates are random intercept effects of a regression model with age and other covariates as fixed effects.
Fourth, given the temporal increase in rates of overweight and obesity in the US (obesity rates has increased from 18.0% in 1971 to 38.6% in 2010) and maternal body-mass index (BMI) being strongly associated with cesarean deliveries,24 we determined the extent to which maternal obesity explained the APC effects on cesarean delivery. Specifically, we included parameters for the prevalence of obesity by cohort as well as period based on data from National Health and Nutrition Examination Survey data. In order to adjust for other observed confounders, maternal race, chronic hypertension, marital status and region of hospital were included as well. For each variable, we estimated the population average for each birth cohort (across years) and for each year (across cohort). These estimates were entered as covariates in the “between” model in the cross-classified random effects model to determine whether variation in obesity rates over time and birth cohort explain observed period and cohort trends after adjusting for confounding.
Results
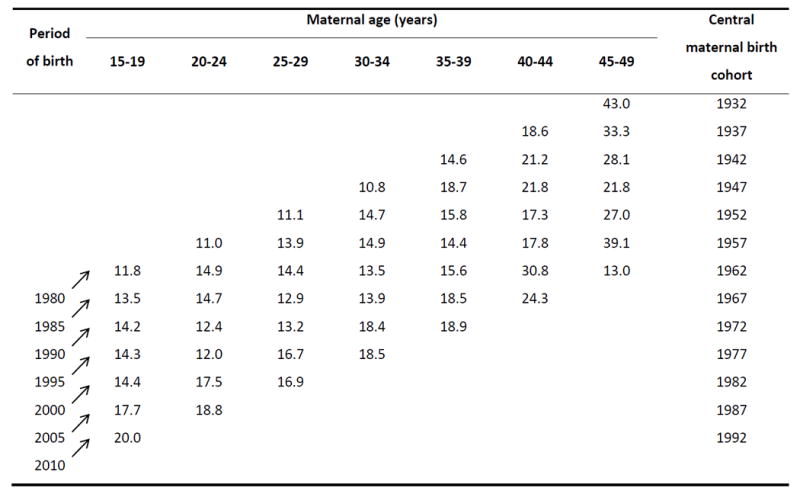
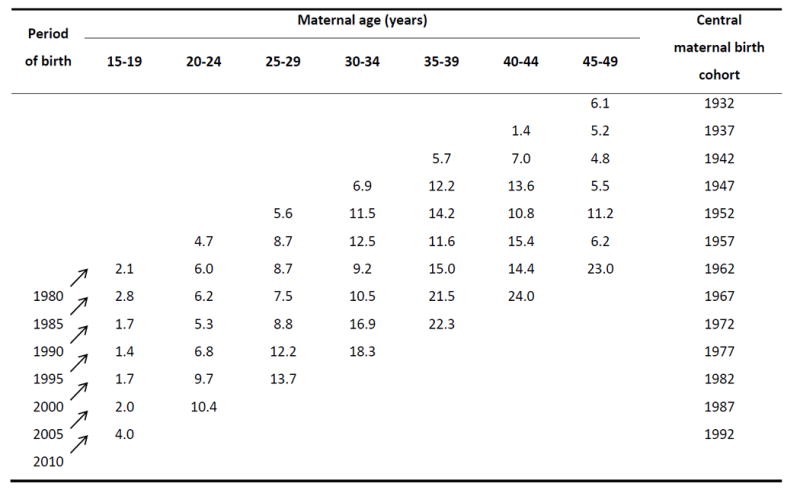
Over the 31-year period (1979-2010), there were 123,484,399 (weighted) hospitalizations in the US that resulted in a singleton delivery. Overall, the primary cesarean rate increased by 68% (95% confidence interval (CI) 67%, 69%) between 1979 (11.0%) and 2010 (18.5%). Repeat cesarean deliveries increased by 178% (95% CI 176, 179) from 5.2% in 1979 to 14.4% in 2010. The distribution of primary cesarean delivery rates by age, selected periods and birth cohorts are shown in Table 1 (the corresponding number of deliveries for primary and repeat cesarean deliveries are shown in eTables 2 and 3, respectively). Within each period, the primary cesarean delivery rates were higher among older than younger women. For instance, in 1980, the rate was 11.8% among 15 to 19-year old women, and increased to 43.0% in women over 45 years. Rates of repeat cesarean deliveries for each period increased linearly with advancing age, but this increase was evident only up to 35 to 39 years (Table 2). We examined changes in the prevalence rates for the indications for cesarean deliveries (Table 3). The rates for most indications increased sharply between 1980 and 2010.
Table 1.
Primary cesarean delivery rates (%) by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
|
Table 2.
Repeat cesarean delivery rates (%) by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
|
Table 3.
Rates of indications for cesarean delivery in 1980, 1990, 2000 and 2010 in the United States and relative change in rates in 1990, 2000 and 2010 with reference to the rate in 1980
| Indications for cesarean delivery | 1980 (n=3,712,473) | 1990 (n=3,965,699) | 2000 (n=3,665,629) | 2010 (n=3,866,303) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| % | RR (95% CI) | % | RR (95% CI) | % | RR (95% CI) | % | RR (95% CI) | |
| Non-reassuring fetal status | 1.7 | 1.00 (Ref) | 8.8 | 5.19 (5.15, 5.23) | 10.3 | 6.07 (6.02, 6.13) | 12.9 | 7.63 (7.57, 7.69) |
| Ischemic placental disease | 4.5 | 1.00 (Ref) | 5.8 | 1.29 (1.28, 1.30) | 8.2 | 1.83 (1.82, 1.84) | 9.7 | 2.15 (2.14, 2.16) |
| Hypertensive disorders1 | 3.6 | 1.00 (Ref) | 4.3 | 1.19 (1.18, 1.20) | 6.2 | 1.73 (1.72, 1.75) | 6.9 | 1.92 (1.91, 1.94) |
| Fetal growth restriction | 0.3 | 1.00 (Ref) | 0.9 | 2.69 (2.64, 2.75) | 1.4 | 4.22 (4.13, 4.30) | 2.3 | 6.70 (6.58, 6.83) |
| Placental abruption | 0.7 | 1.00 (Ref) | 0.9 | 1.24 (1.22, 1.26) | 0.9 | 1.28 (1.26, 1.30) | 1.0 | 1.39 (1.37, 1.41) |
| Malpresentation | 3.3 | 1.00 (Ref) | 4.0 | 1.23 (1.22, 1.24) | 4.7 | 1.42 (1.41, 1.43) | 4.5 | 1.36 (1.35, 1.37) |
| Breech presentation | 3.0 | 1.00 (Ref) | 2.9 | 0.99 (0.98, 0.99) | 2.8 | 0.93 (0.92, 0.94) | 2.8 | 0.94 (0.93, 0.94) |
| Transverse lie | 0.2 | 1.00 (Ref) | 0.5 | 2.01 (1.96, 2.06) | 0.6 | 2.67 (2.60, 2.74) | 0.5 | 2.22 (2.16, 2.27) |
| Other malpresentation | 0.1 | 1.00 (Ref) | 0.7 | 6.41 (6.20, 6.63) | 1.3 | 12.41 (12.02, 12.82) | 1.2 | 11.50 (11.14, 11.88) |
| Labor complications | 6.8 | 1.00 (Ref) | 12.3 | 1.81 (1.80, 1.82) | 13.1 | 1.94 (1.93, 1.95) | 12.4 | 1.84 (1.83, 1.85) |
| Arrest of labor | 6.7 | 1.00 (Ref) | 11.4 | 1.71 (1.70, 1.72) | 11.1 | 1.66 (1.65, 1.67) | 10.5 | 1.57 (1.56, 1.58) |
| Macrosomia | 0.1 | 1.00 (Ref) | 1.0 | 14.77 (14.20, 15.37) | 2.4 | 34.80 (33.46, 36.19) | 2.4 | 34.84 (33.50, 36.23) |
| Prior cesarean | 5.1 | 1.00 (Ref) | 10.6 | 2.08 (2.07, 2.09) | 12.0 | 2.35 (2.34, 2.37) | 15.8 | 3.10 (3.09, 3.12) |
| Low-risk deliveries2 | 81.1 | 1.00 (Ref) | 60.5 | 0.75 (0.74, 0.75) | 53.1 | 0.66 (0.65, 0.66) | 50.7 | 0.63 (0.62, 0.63) |
Hypertensive disorders include gestational hypertension, mild and severe preeclampsia, eclampsia or superimposed preeclampsia
Low risk deliveries include women without any of the indications for primary cesarean deliveries and women that delivered at term RR, risk ratio; CI confidence interval
Age-Period-Cohort Models
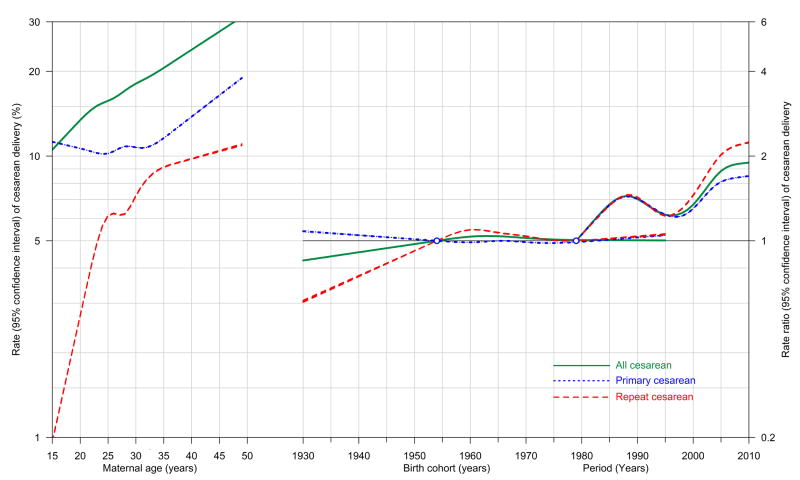
We modeled APC effects for cesarean deliveries based on Poisson regression (Fig 1), and the fit of the models are shown in eTable 4. Age was strongly associated with increased rates of both primary and repeat cesarean deliveries. The rate of primary cesarean delivery for women born in 1954 was fairly stable in women up to 35 years (around 11%), and increased sharply thereafter. In contrast, the rate of repeat cesarean delivery increased sharply between 20 and 37 years and began to decline slightly thereafter. The RR for both primary and repeat cesarean deliveries increased between 1979 and 1987, fell to a nadir in 1997 and increased thereafter. We observed a small birth cohort effect on repeat cesarean deliveries, in that women born between 1930 and 1950 had a lower risk of repeat cesarean deliveries and, to a lesser extent primary cesarean deliveries. No birth cohort effect was seen among women born after 1950.
Figure 1.
Age-period-cohort effects on all cesarean and primary and repeat cesarean deliveries. Rates with 95% confidence intervals are shown on the left vertical axis for maternal age, and risk ratios with 95% confidence intervals on the right vertical axis for period (1979 as the reference period) and birth cohort (1954 as the reference cohort): United States, 1979-2010
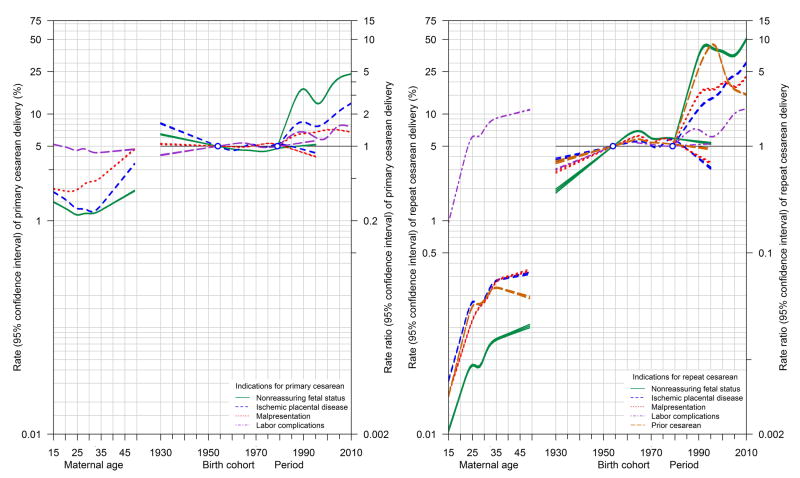
APC effects for primary and repeat cesarean deliveries based on indications are shown in figure 2. With the exception of labor complications, primary cesarean delivery rates for all other indications showed a consistent age effect with rates increasing after age 35 years. Among younger women (up to 35 years), the rates were either stable or declined slightly. For labor complications, no age effect was evident for primary cesarean deliveries. Trends in primary cesarean delivery for ischemic placental disease and, to a lesser extent, for non-reassuring fetal status, showed a small birth cohort effect with women born between 1930 and 1950 at increased risk. Primary cesarean deliveries showed a strong period effect for all indications, with increased risk with advancing period (compared to the 1979 period).
Figure 2.
Age-period-cohort effects on indication-specific primary (left panel) and repeat (right panel) cesarean deliveries. Rates with 95% confidence intervals are shown on the left vertical axis for maternal age, and risk ratios with 95% confidence intervals on the right vertical axis for period (1979 as the reference period) and birth cohort (1954 as the reference cohort): United States, 1979-2010
APC effects on repeat cesarean deliveries (Figure 2, right panel) demonstrated strong age and period effects. The rate of repeat cesarean deliveries increased sharply for all indications up to 40 years and plateaued thereafter. The risk ratios for period effects showed a steep increase for repeat cesarean deliveries based on all indications.
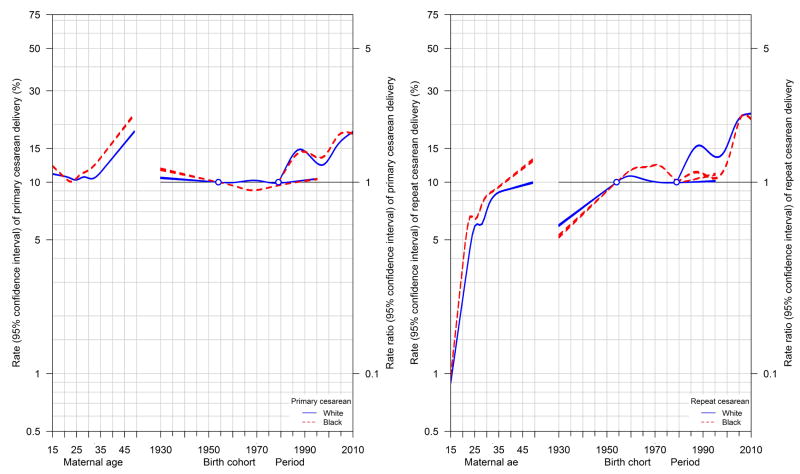
Race-specific APC effects on cesarean delivery
We examined APC effects on primary and repeat cesarean deliveries among white and black women (Figure 3). The overall patterns for APC effects on both primary and repeat cesarean deliveries were similar between white and black women. However, the absolute rates of primary and repeat cesarean deliveries based on maternal age were slightly higher among black than white women. Period effects for primary cesarean deliveries were also similar for black and white women, but no period effect was evident for black women for repeat cesarean deliveries until 1995 and began to increase thereafter. No birth cohort effect was evident.
Figure 3.
Age-period-cohort effects on primary (left panel) and repeat (right panel) cesarean deliveries among white and black women. Rates with 95% confidence intervals are shown on the left vertical axis for maternal age, and risk ratios with 95% confidence intervals on the right vertical axis for period (1979 as the reference period) and birth cohort (1954 as the reference cohort): United States, 1979-2010
Associations between obesity and APC effects of cesarean delivery
In eFigure 1 we provide estimates of APC effects based on multi-level cross-classified random effects models. Overall age, period, and cohort effects were consistent between modeling strategies. The resulting estimates extend the principal analyses for both primary and repeat cesarean deliveries, and demonstrate that the period effect is explained by the covariates included in the model.
In the eTable 5 we provide estimates of the extent to which period- and cohort-specific covariates explain the observed period and cohort effects. Model 2 shows that period-specific obesity is associated with the period effect in primary cesareans (β=0.02, 95% CI 0.01, 0.02). When race, chronic hypertension, marital status, and region of delivery into the model, obesity was no longer associated with changes in the primary cesarean delivery rates, and that set of covariates explain all between-period variation in primary cesarean. However, despite adjustment for these confounders, strong between cohort variation remained. These general findings were also consistent for repeat cesarean deliveries. Period trends in gestational hypertension is associated with primary cesarean (β=-0.04, 95% CI –0.08, 0.00). When repeat cesarean was examined (eTable 5), the results were consistent. Period-specific obesity was associated with the period effect (β=0.04, 95% CI 0.02, 0.07), but cohort-specific obesity was not associated with the cohort effect (β=0.03, 95% CI –0.04, 0.09). Race, chronic hypertension, marital status, and hospital region together explained the period effect in repeated cesarean, but there remains unexplained variation in the cohort effect.
Cesarean trends among low-risk women
We examined APC effects on primary cesarean deliveries among low-risk women. The effects of age, period, and birth cohort on primary cesarean deliveries in low-risk women (eFigure 2) were consistent with the overall patterns, although rates with respect to age were attenuated.
Discussion
Cesarean delivery rates in the US and western societies have increased several fold over the last three decades, with an estimated 1.3 million women undergoing this surgical procedure every year in the US alone. This study shows a steep temporal increase in both primary and repeat cesarean deliveries in the US over three decades (1979-2010) closely associated with higher maternal age with a small effect of maternal birth cohorts restricted to women born before the 1950s. The overall APC patterns both for primary and repeat cesarean deliveries were similar for black and white women although black women demonstrated higher age-specific rates than white women. These data show that maternal obesity explains, at least in part, period trends in primary and repeat cesarean; demographics and comorbidity explain the remainder of the period effect, but there remains substantial variance across cohorts unexplained by known risk factors.
Limitations of the study
A few limitations need to be addressed. Importantly, whether APC effects are differentially associated with cesarean deliveries by parity11,25 remains unknown (i.e., whether APC effects are different for primary cesarean deliveries in primiparous women versus first cesarean in multiparous women). Parity remains a strong determinant of a woman’s risk for a primary cesarean. The total fertility rate (the number of births) in the US has been on the decline over the past four decades (3.7 in 1960 to 1.9 in 2014),26 but the proportion of births to nulliparous women has been increasing. Therefore, it is likely that a 35-year-old woman delivering in 2010 is relatively more likely to be nulliparous than a 35-year-old woman delivering in 1979.
Unfortunately, some confounding factors are either unavailable or are poorly recorded in the NHDS data. Second, there is substantial variation in cesarean delivery rates across states, as well as by hospital and providers27 which remain unaccounted for in this analysis.
Strengths of the study
This population-based study of trends in cesarean deliveries over three decades in the US is the largest with over 123 million (weighted) hospitalizations associated with a singleton delivery. The large study size permitted us to examine trends separately by race, and for primary and repeat cesarean deliveries and within those sub-groups, an evaluation of indication-specific trends. Finally, we were able to demonstrate that period effects on cesarean deliveries are predominantly explained by obesity, race, chronic hypertension, marital status, and region of delivery, whereas cohort variation remains unaccounted for with the available covariates in our data.
Interpretation of the findings
We show that maternal age and period were strongly associated with increasing cesarean delivery rates in the US. Increasing cesarean delivery rates in relation to advanced maternal age have been reported in other studies.28-30 This increased risk is likely a result of higher rates of medical and obstetrical complications as well as higher risks for labor abnormalities among older women.12 The effect of advanced maternal age was consistent across most of the indications for primary and repeat cesarean deliveries.
In a recent study, Barber and colleagues9 reported that non-reassuring fetal status (32%), labor arrest disorders (16%), multiple gestation (16%), and preeclampsia (10%) were the chief indications that contributed to the increase in the primary cesarean delivery rate. They also reported that the cesarean delivery rates for labor disorders did not increase during the period of their study (2003-07).9 These findings are at variance with our data since both primary and repeat cesarean delivery rates do show a temporal increase among women with labor complications.
While major obstetrical initiatives such as the effort to increase trial of labor after cesarean delivery play a clear role in the trends demonstrated in these analyses, we were unable to evaluate other important factors. Elective cesarean deliveries,31,32 ethical concerns emanating from elective cesarean deliveries,33 cesarean on maternal request,34 and the growing concerns for malpractice litigations leading to lower threshold for interventions by obstetricians35-37 in the setting of high-risk pregnancies38 are likely to have contributed to the APC effects. We focused on broad categories for indications, and estimate the APC effects on cesarean deliveries within these categories. Therefore, our data allow interpretation only at the population level and as a characterization of APC effects on trends in cesarean deliveries.
Conclusions
We document an impressive temporal increase in primary and repeat cesarean deliveries in the US over three decades. Maternal age appears to be strongly associated with this trend, with women of advanced age at highest risk. In contrast, the role of cohorts (women being born at the same time) appears small, suggesting that it is clinical practice patterns and age related factors, as opposed to specific environmental exposures, that may be responsible for increased cesarean deliveries. Whether these changes in rates of cesarean deliveries have had an impact on secular change in adverse perinatal outcomes remain undetermined, and is a topic worthy of pursuit.
Supplementary Material
eFigure 1 Age, period, and cohort effects in cesarean rates based on cross-classified random effects model
eFigure 2 Age-period-cohort effects on primary (left panel) and repeat (right panel) cesarean deliveries in low-risk women. Rates with 95% confidence intervals are shown on the left vertical axis for maternal age, and risk ratios with 95% confidence intervals on the right vertical axis for period (1979 as the reference period) and birth cohort (1954 as the reference cohort): United States, 1979-2010
eTable 1 ICD9-Clinical Modification codes for variables in this study
eTable 2 Number of primary cesarean deliveries by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
eTable 3 Number of repeat cesarean deliveries by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
eTable 4 Comparison of age-period-cohort models based on weighted Poisson regression for cesarean delivery rates: United States, 1980 to 2010
eTable 5 Effect of covariates on explaining the between-period and between-birth cohort variation in primary and repeat cesarean delivery: United States, 1979-2010
Acknowledgments
Funding: None
Footnotes
Author contributions:
Investigators responsible for the data include Dr. Ananth and Ms. Lavery.
Study concept and design: Dr. Ananth.
Analysis of data: Ms. Lavery and Dr. Ananth.
Interpretation of data: All authors.
Drafting of the manuscript: Dr. Ananth.
Critical revision of the manuscript for important intellectual content: All authors.
Administrative, technical, or material support: Dr. Ananth.
Ms. Lavery takes responsibility for the accuracy of the data analysis.
Conflict of interest: None of the authors report any conflict of interest to disclose
Data availability: The National Hospital Discharge Survey (NHDS) data is publicly available in deidentified form
References
- 1.Placek PJ, Taffel SM. Trends in cesarean section rates for the United States, 1970--78. Public Health Rep. 1980;95(6):540–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Matthews TJ. Births: Final Data for 2014. Natl Vital Stat Rep. 2015;64(12):1–64. [PubMed] [Google Scholar]
- 3.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65. [PubMed] [Google Scholar]
- 4.ACOG Practice Bulletin #54: vaginal birth after previous cesarean. Obstet Gynecol. 2004;104(1):203–12. [PubMed] [Google Scholar]
- 5.Sachs BP, Kobelin C, Castro MA, Frigoletto F. The risks of lowering the cesarean-delivery rate. N Engl J Med. 1999;340(1):54–7. doi: 10.1056/NEJM199901073400112. [DOI] [PubMed] [Google Scholar]
- 6.Smith GC, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA. 2002;287(20):2684–90. doi: 10.1001/jama.287.20.2684. [DOI] [PubMed] [Google Scholar]
- 7.Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynecol. 2006;195(6):1557–63. doi: 10.1016/j.ajog.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Ananth CV, Vintzileos AM. Medically indicated preterm birth: recognizing the importance of the problem. Clin Perinatol. 2008;35(1):53–67. doi: 10.1016/j.clp.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Declercq E, Menacker F, MacDorman M. Rise in “no indicated risk” primary caesareans in the United States, 1991-2001: cross sectional analysis. BMJ. 2005;330(7482):71–2. doi: 10.1136/bmj.38279.705336.0B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Declercq E, Menacker F, MacDorman M. Maternal risk profiles and the primary cesarean rate in the United States, 1991-2002. Am J Public Health. 2006;96(5):867–72. doi: 10.2105/AJPH.2004.052381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gregory KD, Curtin SC, Taffel SM, Notzon FC. Changes in indications for cesarean delivery: United States, 1985 and 1994. Am J Public Health. 1998;88(9):1384–7. doi: 10.2105/ajph.88.9.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menacker F. Trends in cesarean rates for first births and repeat cesarean rates for low-risk women: United States, 1990-2003. Natl Vital Stat Rep. 2005;54(4):1–8. [PubMed] [Google Scholar]
- 14.Ananth CV, Vintzileos AM. Trends in cesarean delivery at preterm gestation and association with perinatal mortality. Am J Obstet Gynecol. 2011;204(6):505 e1–8. doi: 10.1016/j.ajog.2011.01.062. [DOI] [PubMed] [Google Scholar]
- 15.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2007;(165):1–209. [PubMed] [Google Scholar]
- 16.Kozak LJ, Owings MF, Hall MJ. National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2004;(156):1–198. [PubMed] [Google Scholar]
- 17.Clayton D, Schifflers E. Models for temporal variation in cancer rates. I: Age-period and age-cohort models. Stat Med. 1987;6(4):449–67. doi: 10.1002/sim.4780060405. [DOI] [PubMed] [Google Scholar]
- 18.Holford TR. Analysing the temporal effects of age, period and cohort. Stat Methods Med Res. 1992;1(3):317–37. doi: 10.1177/096228029200100306. [DOI] [PubMed] [Google Scholar]
- 19.Carstensen B. Age-period-cohort models for the Lexis diagram. Stat Med. 2007;26(15):3018–45. doi: 10.1002/sim.2764. [DOI] [PubMed] [Google Scholar]
- 20.Carstensen B, Plummer M, Laara E, Hills M. Epi: A package for statistical analysis in epidemiology (R package version 1.1.34) [20 April 2012]; http://CRAN.R-project.org/package=Epi.
- 21.Bailit JL, Love TE, Mercer B. Rising cesarean rates: are patients sicker? Am J Obstet Gynecol. 2004;191(3):800–3. doi: 10.1016/j.ajog.2004.01.051. [DOI] [PubMed] [Google Scholar]
- 22.Keyes KM, Utz RL, Robinson W, Li G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971-2006. Soc Sci Med. 2010;70(7):1100–8. doi: 10.1016/j.socscimed.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang Y, Land K. Mixed Effects Models: Hierarchical APC-Cross-Classified Random Effects Models (HAPC-CCREM), Part I: The Basics. In: Yang Y, Land K, editors. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. New York, NY: Chapman & Hall/CRC Interdisciplinary Statistics; 2013. [Google Scholar]
- 24.Getahun D, Kaminsky LM, Elsasser DA, Kirby RS, Ananth CV, Vintzileos AM. Changes in prepregnancy body mass index between pregnancies and risk of primary cesarean delivery. Am J Obstet Gynecol. 2007;197(4):376, e1–7. doi: 10.1016/j.ajog.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201(4):422, e1–7. doi: 10.1016/j.ajog.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 26.United Nations. United Nations, ed: Demographic Profiles. II. New York, NY: 2015. World Population Prospects: The 2015 Revision. [Google Scholar]
- 27.Kozhimannil KB, Arcaya MC, Subramanian SV. Maternal Clinical Diagnoses and Hospital Variation in the Risk of Cesarean Delivery: Analyses of a National US Hospital Discharge Database. PLoS Med. 2014;11(10):e1001745. doi: 10.1371/journal.pmed.1001745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ford J, Grewal J, Mikolajczyk R, Meikle S, Zhang J. Primary cesarean delivery among parous women in the United States, 1990-2003. Obstet Gynecol. 2008;112(6):1235–41. doi: 10.1097/AOG.0b013e31818ce092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joseph KS, Young DC, Dodds L, O’Connell CM, Allen VM, Chandra S, Allen AC. Changes in maternal characteristics and obstetric practice and recent increases in primary cesarean delivery. Obstet Gynecol. 2003;102(4):791–800. doi: 10.1016/s0029-7844(03)00620-3. [DOI] [PubMed] [Google Scholar]
- 30.Menacker F, Declercq E, MacDorman MF. Cesarean delivery: background, trends, and epidemiology. Semin Perinatol. 2006;30(5):235–41. doi: 10.1053/j.semperi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, Moawad AH, Caritis SN, Meis PJ, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O’Sullivan MJ, Sibai BM, Langer O, Thorp JM, Ramin SM, Mercer BM Eunice Kennedy Shriver NM-FMUN. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–20. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meikle SF, Steiner CA, Zhang J, Lawrence WL. A national estimate of the elective primary cesarean delivery rate. Obstet Gynecol. 2005;105(4):751–6. doi: 10.1097/01.AOG.0000157435.67138.78. [DOI] [PubMed] [Google Scholar]
- 33.Minkoff H, Powderly KR, Chervenak F, McCullough LB. Ethical dimensions of elective primary cesarean delivery. Obstet Gynecol. 2004;103(2):387–92. doi: 10.1097/01.AOG.0000107288.44622.2a. [DOI] [PubMed] [Google Scholar]
- 34.Mazzoni A, Althabe F, Liu NH, Bonotti AM, Gibbons L, Sanchez AJ, Belizan JM. Women’s preference for caesarean section: a systematic review and meta-analysis of observational studies. BJOG. 2011;118(4):391–9. doi: 10.1111/j.1471-0528.2010.02793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Minkoff H. Fear of litigation and cesarean section rates. Semin Perinatol. 2012;36(5):390–4. doi: 10.1053/j.semperi.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 36.Murthy K, Grobman WA, Lee TA, Holl JL. Association between rising professional liability insurance premiums and primary cesarean delivery rates. Obstet Gynecol. 2007;110(6):1264–9. doi: 10.1097/01.AOG.0000287294.89148.23. [DOI] [PubMed] [Google Scholar]
- 37.Leitch CR, Walker JJ. The rise in caesarean section rate: the same indications but a lower threshold. Br J Obstet Gynaecol. 1998;105(6):621–6. doi: 10.1111/j.1471-0528.1998.tb10176.x. [DOI] [PubMed] [Google Scholar]
- 38.Dubay L, Kaestner R, Waidmann T. The impact of malpractice fears on cesarean section rates. J Health Econ. 1999;18(4):491–522. doi: 10.1016/s0167-6296(99)00004-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1 Age, period, and cohort effects in cesarean rates based on cross-classified random effects model
eFigure 2 Age-period-cohort effects on primary (left panel) and repeat (right panel) cesarean deliveries in low-risk women. Rates with 95% confidence intervals are shown on the left vertical axis for maternal age, and risk ratios with 95% confidence intervals on the right vertical axis for period (1979 as the reference period) and birth cohort (1954 as the reference cohort): United States, 1979-2010
eTable 1 ICD9-Clinical Modification codes for variables in this study
eTable 2 Number of primary cesarean deliveries by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
eTable 3 Number of repeat cesarean deliveries by maternal age, period (every fifth year), and central maternal birth cohorts in the United States, 1980 to 2010
eTable 4 Comparison of age-period-cohort models based on weighted Poisson regression for cesarean delivery rates: United States, 1980 to 2010
eTable 5 Effect of covariates on explaining the between-period and between-birth cohort variation in primary and repeat cesarean delivery: United States, 1979-2010