Case Description
An 89 year-old woman with hypertension, hyperlipidemia, stroke, deep venous thrombosis, and atrial fibrillation presented with four days of right eye (OD) redness and swelling, and intermittent diplopia. An ophthalmologic evaluation revealed visual acuity 20/50 OD. There was limited abduction OD, right upper and lower lid erythema and edema, conjunctival injection. Funduscopic examination was unremarkable. ESR and CRP were normal. Follow-up ophthalmologic exam two weeks later showed visual acuity decreased to 20/70 OD with increased right orbital congestion, exophthalmos (25mm OD and 21mm OS), and worsening limitation of ductions OD. An MRI/MRA of her head demonstrated fusiform dilatation of the cavernous segment of the right internal carotid artery (ICA) with asymmetric enhancement of the right cavernous sinus and an enlarged right superior ophthalmic vein (SOV) consistent with arterialized flow from a carotid-cavernous sinus fistula (CCF).
The patient was urgently referred to neuro-interventional radiology for diagnostic angiography and embolization of the CCF. The cerebral angiogram showed a right direct (Barrow type A) CCF, with rapid enhancement of the right cavernous sinus and right superior ophthalmic vein. A 7 mm fusiform aneurysm of the right cavernous internal carotid artery was found to be the likely cause of the CCF (Figure 1A). Transarterial access of the fistula for coil embolization was unsuccessful.
Figure 1.
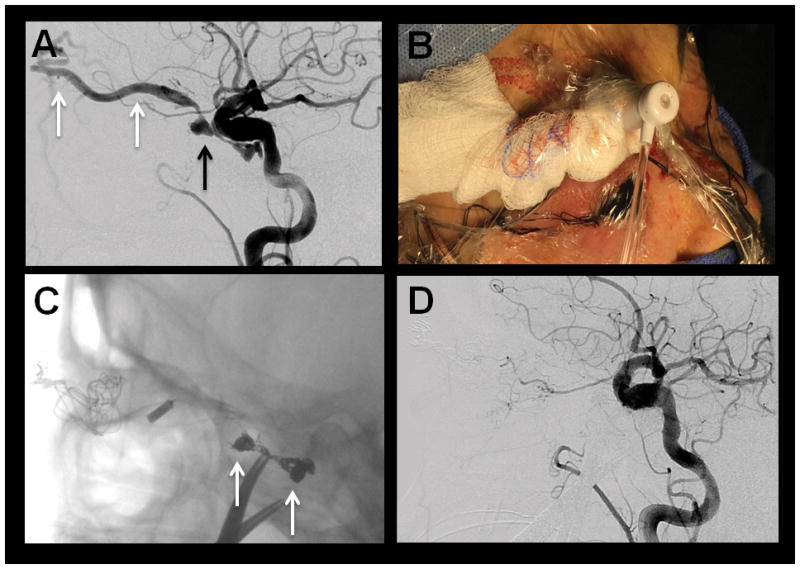
(A) Pre-treatment DSA, lateral magnified view, right common carotid artery injection, showing early, rapid opacification of the right cavernous sinus (black arrow) and right superior ophthalmic vein (white arrows) consistent with a direct carotid-cavernous fistula. There is also fusiform dilatation of the cavernous right ICA representing dysplasia with an aneurysm. (B) Photograph showing the direct access provided to the right superior ophthalmic vein for coil embolization (C) Unsubtracted lateral magnified view angiography after coil embolization of the carotid-cavernous fistula showing a coil basket (white arrows) within the right cavernous sinus. (D) DSA, lateral magnified view, right common carotid injection, after coil embolization showing complete closure of the carotid-cavernous fistula without evidence of residual arteriovenous shunting.
Repeat ophthalmologic exam demonstrated continued worsening of her visual acuity to 20/400 OD, elevated intraocular pressure (IOP) in the right eye (24mmHg), a relative afferent pupillary defect and complete limitation of ductions OD. External exam revealed worsening right upper and lower lid edema and erythema, proptosis, and conjunctival injection with corkscrew vessel tortuosity (Figure 2A). Goldmann visual field testing revealed 360 degree significant peripheral constriction. Four days after her initial angiography, the patient underwent coil embolization of her right direct CCF via direct access of the right superior ophthalmic vein provided by the Ophthalmic Plastic Surgery Service (Figure 1B–C). Complete closure of the CCF was demonstrated without residual arteriovenous shunting (Figure 1D).
Figure 2.
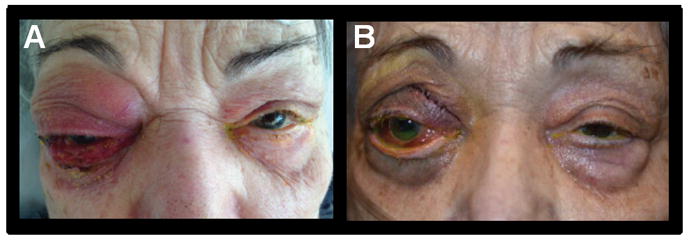
(A) Photograph pre-intervention demonstrating severe right orbital edema and erythema and proptosis. (B) Photograph 8 days after fistula embolization.
Post-operatively, her visual acuity, intraocular pressure, congestion, chemosis, lid edema and extraocular eye movements have improved substantially (Figure 2B).
Discussion
Carotid-cavernous fistulas arise from abnormal connections between the carotid arteries and the cavernous sinus.1 These acquired vascular malformations disrupt the cavernous sinus, an intricate anatomic site of cerebral venous drainage, through which the internal carotid artery and cranial nerves III, IV, V1, V2, and VI traverse.
CCFs are classified based on hemodynamics (high flow or low flow), etiology (spontaneous or traumatic) and angiographic anatomy (direct or indirect).1–3 The angiographic classification by Barrow and colleagues divides CCFs into four types (A, B, C, and D). Type A CCF are direct connections between the cavernous ICA and the cavernous sinus. Types B, C, and D CCF are indirect connections between the cavernous sinus and branches of the ICA (Type B), branches of the external carotid artery (Type C), and branches of the ICA and external carotid artery (Type D).1
Type A, or direct carotid-cavernous fistula, are the most frequent type of CCF.4 Trauma is the most common cause of direct CCFs and accounts for the higher prevalence in young men.3,4 Traumatic CCF are usually unilateral, but can occur bilaterally in 2% of patients.3,4 Less frequently, spontaneous direct CCFs occur due to rupture of a cavernous carotid aneurysm (as in our patient) or rupture of a weakened carotid wall in patients with connective tissue diseases such as fibromuscular dysplasia or Ehlers-Danlos.3–4 Iatrogenic causes of Type A CCFs include transphenoidal surgery and endovascular procedures.4 The majority of Type A CCFs are high flow lesions, with acute onset of symptoms, and low likelihood of resolving spontaneously.3,4
Type B, C and D carotid-cavernous fistulas are indirect or dural fistulas. Indirect CCFs are more often spontaneous and infrequently traumatic.3–5 They are more common in elderly women.3–5 The precise spontaneous mechanism is unknown but may be related to venous thrombosis in the cavernous sinus or weakening of the arterial wall from predisposing factors such as hypertension, atherosclerosis or connective tissue diseases.3–5 Indirect CCFs are low flow lesions, with insidious symptom onset, and high likelihood of spontaneous resolution.3–6
In carotid-cavernous fistulas arterialized blood is shunted into the venous system leading to venous hypertension.3,4 The clinical symptoms depend in large part on the venous drainage route, and available collaterals.3,4 Patients with direct CCFs classically present with sudden onset of the clinical triad of chemosis, proptosis, and bruit.3,6 Other common clinical findings include headache, diplopia, ophthalmoplegia, and decreased visual acuity.2–4,6 Less common findings include intracerebral hemorrhage, subarachnoid hemorrhage and external hemorrhage, such as epistaxis.2–4,6 Patients with indirect CCFs have a more insidious onset of symptoms and the clinical course is often relapsing-remitting, making diagnosis difficult.2–6 Chronic conjunctival injection, proptosis, glaucoma and chemosis are common.2–4,6
The diagnosis of CCF is made by neuroanatomic and neurovascular imaging. First line modalities include computed tomography (CT) and CT angiogrography (CTA) or magnetic resonance (MR) and MR angiography (MRA) of the brain. Signs of CCF detected with non-invasive imaging include proptosis, dilatation of the superior ophthalmic vein (SOV), extraocular muscle enlargement, ipsilateral cavernous sinus enlargement, and skull fracture.2–4,6 Digital subtraction angiography (DSA) is the gold standard in the diagnosis of CCF and must be performed prior to any potential intervention.3–4
The main goal in the treatment of CCFs is to preserve flow in the ICA while occluding the fistula.2,6 Clinical indications for emergent treatment include progressive ptosis, visual decline, hemorrhage (intracranial or external) and increased intracranial pressure.7 Angiographic signs for emergent treatment include cavernous sinus varix, pseudoaneurysm, cortical venous drainage and thrombosis of distal venous pathways.7
Conservative management is an option for some low risk, low flow, indirect CCFs. External manual compression of the ipsilateral carotid artery and contralateral jugular vein, several times per day over several weeks, achieves cure in approximately 30% of patients.6,8 Surgical management is limited to cases when endovascular approaches are not possible or not effective due to the increased morbidity associated with the open management.2–4 Stereotactic radiosurgery is an option for low flow, indirect CCFs, with high success rates of 75% – 91%, however, the long time to successful treatment limits the utility of this approach.2,4
Endovascular management is the current treatment modality of choice for CCFs.2–4 Transarterial embolization is the preferred access method for direct CCFs and transvenous embolization is preferred for indirect CCFs.4 In the transarterial approach, a microcatheter is passed through the fistula into the cavernous sinus and coils and/or embolic agents, such as Onyx (Covidien, Ireland), are placed in the cavernous sinus.4,6 In the transvenous approach, the cavernous sinus is most commonly accessed through the inferior petrosal sinus.4 Direct cannulation of the superior ophthalmic vein (SOV) is occasionally needed when more standard approaches are not possible.2,4 Cure rates after endovascular repair of CCFs approximate 80%.2
In summary, carotid cavernous fistulas are a rare but treatable cause of orbital injury and vision loss. Endovascular embolization of CCFs with coiling or liquid agents is the treatment modality of choice. With appropriate treatment, progressive resolution of symptoms is expected in most patients.
Take Home Points.
Carotid cavernous fistulas (CCFs) are a rare but potentially devastating cause of orbital symptoms, visual loss and periocular disfigurement.
CCF patients typically present with proptosis, elevated intraocular pressure, prominent tortuous conjunctival vessels and sometimes headache.
Endovascular treatment is the modality of choice for CCFs. Prompt treatment can prevent further complications of CCFs and lead to complete resolution of symptoms.
Footnotes
Disclosures: none
Funding Sources: none
References
- 1.Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985;62:248–256. doi: 10.3171/jns.1985.62.2.0248. [DOI] [PubMed] [Google Scholar]
- 2.Ellis JA, Goldstein H, Connolly ES, Meyers PM. Carotid-cavernous fistulas. Neurosurg Focus. 2012;32:E9. doi: 10.3171/2012.2.FOCUS1223. [DOI] [PubMed] [Google Scholar]
- 3.Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol. 2013;5:143–55. doi: 10.4329/wjr.v5.i4.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zanaty M, Chalouhi N, Tjoumakaris SI, Hasan D, Rosenwasser RH, Jabbour P. Endovascular treatment of carotid-cavernous fistulas. Neurosurg Clin N Am. 2014;25:551–63. doi: 10.1016/j.nec.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Miller NR. Diagnosis and management of dural carotid-cavernous sinus fistulas. Neurosurg Focus. 2007;23:E13. doi: 10.3171/FOC-07/11/E13. [DOI] [PubMed] [Google Scholar]
- 6.Gemmete JJ, Ansari SA, Gandhi DM. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol. 2009;29:62–71. doi: 10.1097/WNO.0b013e3181989fc0. [DOI] [PubMed] [Google Scholar]
- 7.Halbach VV, Hieshima GB, Higashida RT, Reicher M. Carotid cavernous fistulae: indications for urgent treatment. American Journal of Roentgenology. 1987;149:587–593. doi: 10.2214/ajr.149.3.587. [DOI] [PubMed] [Google Scholar]
- 8.Higashida RT, Hieshima GB, Halbach VV, Bentson JR, Goto K. Closure of carotid cavernous sinus fistulae by external compression of the carotid artery and jugular vein. Acta Radiol Suppl. 1986;369:580–3. [PubMed] [Google Scholar]


