Abstract
Purpose
We sought to identify icons to effectively communicate health harms of chemicals in cigarette smoke.
Methods
Participants were a convenience sample of 701 U.S. adults. A within-subjects online experiment explored the effects of icon semiotic type: symbolic (arbitrary, most abstract), indexical, and iconic (representative, most concrete). Outcomes were perceived representation, affect toward smoking, elaboration, perceived severity, and perceived effectiveness.
Results
For not-easy-to-visualize harms of cancer and addiction, symbolic icons received the highest ratings (all p<.001). For easy-to-visualize symptoms of heart attack/stroke, indexical icons received the highest ratings (all p<.001). For easy-to-visualize harm of reproductive organ damage, the iconic image did best (all p<.001). Icon type often had a larger impact among participants with higher health literacy.
Conclusions
Symbolic icons may be most effective for health effects not easily visualized. Iconic or indexical icons may be more effective for health effects attributable to specific body parts or symptoms.
Keywords: icons, pictograph, warning, cigarette, health effects
Introduction
Cigarette smoking remains the primary cause of preventable death and disease in the United States (U.S.) (United States Department of Health Human Services, 2014). Smoking causes an array of health problems including cardiovascular disease, cancer, respiratory disease, reproductive health harms, and addiction (Center for Disease Control and Prevention, 2016; United States Department of Health and Human Services, 2016). The harms from smoking are mainly due to the chemicals (sometimes called constituents) in smoke. These chemicals either exist naturally in tobacco, are added in production, or are produced in the burning of the cigarette (R. R. Baker, Massey, & Smith, 2004; Hecht, 2012; Wayne & Carpenter, 2009). At least 70 of the chemicals in cigarette smoke cause cancer (carcinogens), including acetaldehyde, benzene, benzo[a]pyrene, formaldehyde, and 1,3-butadiene. Other harmful chemicals, including arsenic, hydrogen cyanide, and acrolein are known to harm cardiovascular and respiratory health (Fowles & Dybing, 2003; Hecht, 2012; Hoffmann & Hoffmann, 2001; Rodgman & Perfetti, 2013; Talhout et al., 2011; United States Food and Drug Administration, 2012).
The Family Smoking Prevention and Tobacco Control Act, designed to protect public health, includes a requirement that the U.S. government inform the public about the harmful and potentially-harmful constituents (HPHCs) in tobacco products and cigarette smoke. This information is to be displayed in a format that is “understandable” and “not misleading to a lay person” (111th Congress of the United States of America, 2009). The mandate is challenging to fulfill given the public's limited knowledge of the many chemicals in cigarette smoke and the resulting health problems (Boynton et al., 2016; Hall, Ribisl, & Brewer, 2014; Moracco et al., 2016). One way to achieve this communication goal is through the use of simple visuals to clearly convey the general categories of harms at a glance. Adding visuals, such as icons, can improve the effectiveness of health communication, especially for people with lower literacy (Garcia-Retamero & Galesic, 2010; Houts, Doak, Doak, & Loscalzo, 2006; Katz, Kripalani, & Weiss, 2006). Illustrative visuals (icons or photographs) can improve lay audiences' understanding of health information and influence health behaviors indirectly through increased cognitive elaboration, perceived risk, and negative affect (Andrews, Netemeyer, Kees, & Burton, 2014; Evans et al., 2015; Houts et al., 2006; Meppelink, Smit, Buurman, & van Weert, 2015; Zikmund-Fisher et al., 2014). Yet, currently very little is known about what types of icons are most effective in representing specific concepts, such as health harms, to lay audiences (Nakamura & Zeng-Treitler, 2012; Zikmund-Fisher et al., 2014).
Peircean semiotics – the study of signs or processing of signs – offers a framework to link icons with salient mental representations and predictions of how images (including icons) will be processed and what thoughts they will provoke (Messaris, 1997; Moriarty, 2002). A sign is an “object that stands for another” in one's mind (Peirce, 1991, p. 141); signs can be represented more concretely or more abstractly depending on the choice of sign type. In the present study, we use Peirce's (1991) three classifications: iconic, indexical, and symbolic. With each type, the icons (the signifiers) evoke unique connections to the health effects they represent (the signified) for lay audiences (the interpretants). Iconic signs represent an object's likenesses (e.g., an image of flames to represent fire). The visual similarity of iconic visuals and the concrete objects they represent make them familiar and easy to interpret. Indexical signs represents a “correspondence of fact” or evidence that evokes thoughts of a physical connection or lived experience between the signifier and the signified without being a direct representation of it (e.g., smoke signaling there is fire). Finally, symbolic signs show “imputed character” or arbitrary representations (e.g., a fire fighter's hat to represent fire). Symbolic signs follow social conventions and rely on knowledge of learned social constructions, such as metaphors for interpretation (Peirce, 1991, p. 30). These categories are a taxonomy of visual communication that can aid analysis of its impact; these categories may overlap to some degree (Moriarty, 2002). Signs, and in this case icons, derive their meaning from the viewer's interpretation and that meaning may vary among individuals; a fire may symbolically represent danger to one individual and iconically represent the fire itself to another. However, our culturally shared meaning of visuals often allows signs to have shared interpretations, especially when accompanied by explicit, text-based information (e.g., labels).
With this semiotic perspective, our study developed and tested the possibility of differing effects of iconic icons (that are mimetic, i.e., look like what they represent), indexical icons (that are evidential and show the consequences), and symbolic icons (that are abstract or have meaning based on arbitrary learned social constructions) to communicate each of five categories of health effects of the chemicals in cigarette smoke to lay audiences. Developing simple imagery that represents each of these categories of health effects poses multiple challenges. The health effects of interest range from abstract diseases that are difficult to visualize in a single image (e.g., cancer, addiction) to those that are easily identified with an acute symptom or specific organ (e.g., heart attack, lung damage) to conditions that are concrete but best understood by the absence of something (e.g., infertility). Our exploratory study evaluated each of these three semiotic types of icons for their perceived representativeness as well as for how effective they were in influencing how participants thought and felt about each of the health effects.
Methods
Participants
In January 2016, we recruited 701 U.S. adults aged 18 or older using Amazon's Mechanical Turk (MTurk), an online survey platform that is increasingly used in social science and behavioral research (Buhrmester, Kwang, & Gosling, 2011; Casler, Bickel, & Hackett, 2013). The recruitment message invited both smokers and non-smokers to participate. Participants' average age was 34 years (range 19-70). The majority of participants (80.5%) reported their race as white (Table 1). Slightly more than half of participants (55.9%) had an associate's degree or higher. About a third (34.1%) identified as current smokers and most participants had a perfect health literacy score (52%) or missed one item (32%).
Table 1. Participant demographics.
| % (n) | |
|---|---|
|
| |
| Sex | |
| Female | 46.2 (324) |
| Male | 53.8 (377) |
| Sexual orientation | |
| Straight | 88.4 (620) |
| Gay or lesbian | 5.1 (36) |
| Bisexual | 6.4 (45) |
| Hispanic | |
| Yes | 8.3 (58) |
| No | 91.7 (643) |
| Race | |
| White | 80.5 (564) |
| Black | 6.6 (46) |
| American Indian or Alaska Native | 0.7 (5) |
| Asian | 9.3 (65) |
| Pacific Islander | 0.1 (1) |
| Other | 2.9 (20) |
| Education | |
| Less than high school | 2.0 (14) |
| High school degree or GED | 13.8 (97) |
| Some college | 11.6 (81) |
| Associate's degree | 10.4 (73) |
| Bachelor's degree | 37.7 (264) |
| Master's degree | 5.7 (40) |
| Professional degree | 1.3 (9) |
| Doctorate degree | 0.9 (6) |
| Current smoker | |
| No | 65.9 (462) |
| Yes | 34.1 (239) |
| Health literacy | |
| Perfect score | 51.8 (363) |
| Missed one or more | 48.2 (338) |
Note. n = 701.
Procedures
Icon development
The FDA used the five categories of health effects of smoking to inform the development of their list HPHCs, which are 1) cancers, 2) addiction, 3) heart attack and stroke, 4) permanent breathing problems, and 5) reproductive organ damage. With these categories in mind, we developed icons for five categories of health effects caused by chemicals in cigarette smoke. A professional designer created new and adapted existing icons using an iterative design process, generating a revised panel of icons weekly for 8 weeks. An advisory board of public health and health communications experts reviewed the icons weekly and suggested revisions. This process resulted in three final icons for each health effect (Figure 1). For each health effect category described above, we created one icon that aligned with each semiotic icon type – iconic (concrete, mimetic representations or likeness of the object), indexical (evidence of something), or symbolic (abstract meaning).
Figure 1. Health Effects of Cigarette Smoke Icons.
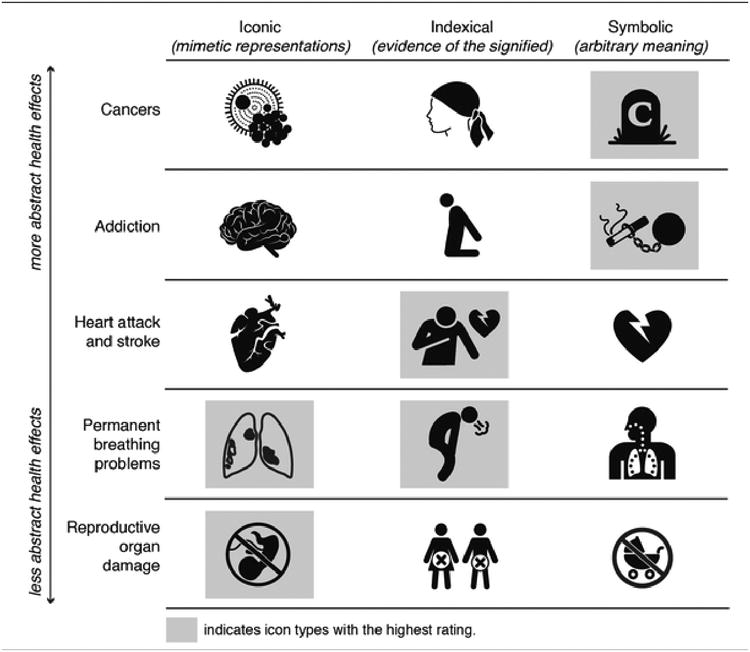
Icons for cancer were a cell invaded with cancer (iconic), a silhouette wearing a headscarf as evidence of losing one's hair (indexical), and a tombstone with a large letter “C” (symbolic). Addiction icons were an anatomical brain (iconic), a figure on their knees with hands behind the back (indexical), and a ball and chain attached to a cigarette (symbolic). Icons for heart attack and stroke, which focused on heart attacks, were an anatomical heart (iconic), a figure with one hand clutching the chest (indexical), and a heart with a lighting bolt through the center (symbolic). Permanent breathing problem icons were outlined lungs with spots (iconic), a figure coughing (indexical), and a figure with dotted airflow diagram (symbolic). Lastly, reproductive organ damage icons were a circle with line surrounding a fetus (iconic), male and female figures with “x's” over their reproductive organs (indexical), and a circle with line surrounding a baby carriage (symbolic). All icons appeared above text denoting the category (e.g., cancers) to increase the likelihood participants would interpret them as a representation of their respective health category.
Experimental procedures
Individuals participated in an online experiment with a section for each of the five health effect categories: 1) cancers, 2) addiction, 3) heart attack and stroke, 4) permanent breathing problems, and 5) reproductive organ damage. The sections appeared in a random order, with each participant eventually rating icons for all five health problems. In each section, participants viewed icons of all three types (iconic, indexical and symbolic), one at a time in a random order. Thus, in total, each participant viewed and rated 15 icons.
Following consent, the online questionnaire described the study as being about “icons, or pictures, that show the harms of smoking cigarettes,” along with an example of a danger icon (triangle with exclamation point) and brief description of the implied meaning (danger). Next, the participants were presented the first icon, shown underneath information that stated the health effect category (in bold) followed by text giving disease examples: cancers includes cancer of the lungs, bone, and pancreas; heart attack and stroke includes sudden death, heart damage, and blood clots; permanent breathing problems includes lung damage and lung disease; reproductive organ damage includes erectile dysfunction, spontaneous abortions, and birth defects. The exception was addiction, which had no disease examples listed. Participants received $4 upon study completion. The University of North Carolina Institutional Review Board approved the study.
Measures
For each icon, participants responded to 8 items that assessed perceived representation, affect, cognitive elaboration, perceived severity, and perceived effectiveness. Each item appeared directly below each icon on the same website page. After participants had responded to all questions for all three icons in a section, they selected which of the three icons they felt was best represented the health effect.
Perceived Representation
The survey assessed perceived representation with a single item for each icon, “This icon makes me think of cancers.” Response options ranged from “strongly disagree” (coded as 1) to “strongly agree” (5).
Affect
The survey assessed how each icon made participants feel about smoking using one item (Peters et al., 2006). The seven-point response scale ranged from “very bad” (coded as -3) to “very good” (3).
Cognitive Elaboration
The survey assessed how much each icon made participants think about the harmful effects of smoking (Brewer et al., 2016; Fathelrahman et al., 2010). The seven-point response scale ranged from “not at all” (coded as 0) to “quite a lot” (6).
Perceived Severity
The survey assessed perceived severity with this question, “How much would having the health problem shown by this icon affect your life?” (Brewer et al., 2011; Brewer et al., 2016). The seven-point response scale ranged from “not at all” (coded as 0) to “quite a lot” (6).
Perceived Effectiveness
The survey assessed perceived effectiveness with three previously developed items: “This icon makes smoking seem unpleasant to me;” “This icon makes me concerned about the harmful effects of smoking;” and “ This icon discourages me from wanting to smoke” (Boynton et al., 2016). The five-point response scale ranged from “strongly disagree” (coded as 1) to “strongly agree” (5).
Icon Choice
At the end of each experiment, participants chose “the icon that best represents [health effect] caused by smoking” by clicking on one of the three icons (iconic, indexical, or symbolic) they saw previously; icon order was randomized.
Open-ended Evaluation
After the experiments were complete, participants saw three randomly selected icons, one from each icon type. For each icon, they gave open-ended responses to the question, “What do you think of when you see this icon?”
Covariates
To assess current smoking status, the survey used two items from the Behavioral Risk Factor Surveillance System (Centers for Disease Control and Prevention, 2013). We defined current smokers as people who have smoked at least 100 cigarettes in their lifetime (i.e., five packs) and smoke every day or some days. Health literacy was assessed with a reading comprehension portion (passage B) of the Short Test of Functional Health Literacy (D. Baker, Williams, Parker, Gazmarian, & Nurss, 1999). A modified cloze procedure omitted every fifth to seventh word of sentences at a 10th grade reading level. Participants selected the word that best fit the missing space from four options. Participants were divided into perfect scores of health literacy (20 correct) and those that missed one or more item (19 or less correct).
Data Analysis
For each health topic section, we conducted a multivariate analysis of variance (MANOVA) in order to correct for multiple tests (Stevens, 2007). Predictor variables were icon type (iconic vs. indexical vs. symbolic), smoking status, and health literacy. Outcomes were perceived representation, affect, cognitive elaboration, and perceived severity, and perceived effectiveness. Because all MANOVAs were statistically significant (p<.001), we conducted repeated measures univariate analyses of variance (ANOVA) for each outcome, using Greenhouse-Geisser adjusted F tests for main effects and interactions between icon type and smoking status or health literacy (Stevens, 2007). For statistically significant F-tests, we conducted post-hoc pairwise comparisons with Bonferroni corrections.
Results
Icon type affected all outcomes in each of the 5 sections in the experiment (all p<.001).
Cancers
For cancers, perceived representativeness was highest for the symbolic icon, the tombstone with the letter “C,” (M = 3.55, SD = 1.33). Ratings of this icon were higher than for the other two icons – iconic, a cancer cell, (M = 2.59, SD = 1.39) or indexical, the person with the headscarf, (M = 2.99, SD = 1.44) (p<.001 for each). The symbolic cancers icon also elicited more negative affect toward smoking, greater cognitive elaboration, greater perceived severity of cancer, and was perceived as more effective compared to the iconic and indexical icons (all p<.001).
When given all three icons side-by-side, participants also most often selected the symbolic icon as the most representative of cancers (Table 3). Participants' open-ended responses described the symbolic cancers icon as making them think, “smoking can lead to cancer that can lead to an early death,” and “I see myself dead in a grave if I don't stop smoking!”
Table 3. Icon Selected as Most Representative.
| 1. Iconic | 2. Indexical | 3. Symbolic | |
|---|---|---|---|
|
|
|||
| Cancers | 15% | 21% | 64% |
| Addiction | 2% | 2% | 96% |
| Heart attack and stroke | 13% | 78% | 8% |
| Permanent breathing problems | 43% | 46% | 11% |
| Reproductive organ damage | 59% | 35% | 6% |
Note. Shading indicates icon types selected as most representative. n = 701.
Addiction
Addiction, another abstract health effect, had a similar pattern of effects as cancers. The perceived representativeness was highest for the symbolic icon for addiction, a ball and chain connected to a cigarette, (M = 4.55, SD = .72). The symbolic icon was rated higher than the images that were iconic, brain (M = 2.47, SD = 1.33), or indexical, person kneeling with hands behind back, (M = 2.38, SD = 1.35), (p<.001 for each). The symbolic icon also had higher ratings for negative affect toward smoking, increased cognitive elaboration, and higher perceived severity for addiction, and perceived effectiveness of the icon compared to the other icon types (all p<.001).
The symbolic icon was overwhelmingly selected as the icon choice most representative of addiction in the side-by-side comparison. Participants reported, in their open-ended responses, the symbolic addiction icon made them think of “being chained down by nicotine addiction” and “smoking weighing me down as if I were chained to a ball and it is something that I won't be able to escape from.”
Heart Attack and Stroke
Heart attack and stroke elicited highest ratings for the indexical icon, a figure with one hand clutching the chest, (M = 4.50, SD = .77). This icon was rated higher on representation than the iconic, anatomical heart, (M = 3.71, SD = 1.22) or symbolic, heart with a lighting bolt, (M = 3.78, SD = 1.15) icons (p<.001 for each). The indexical icon also elicited more negative affect toward smoking, greater elaboration, increased perceived severity of heart attack and stroke, and was perceived as more effective than the iconic or symbolic icons (all p<.001).
Over three-quarters of participants selected the indexical icon as the icon of choice for heart attack and stroke in the side-by-side comparison. Participants' open-ended responses described the indexical icon making them think of a man “grabbing his heart because he is having a stroke” or “having a heart attack,” as well as thinking about, “the pain of a heart attack.”
Permanent Breathing Problems
Permanent breathing problems was the only health effect category without a clearly preferred semiotic icon type. The iconic icon, outlined lungs with spots, (M = 4.15, SD = .96) and indexical icon, figure coughing, (M = 4.04, SD = 1.05) were both perceived as more representative of permanent breathing problems than the symbolic icon, a figure with a dotted airflow diagram (M = 3.45, SD = 1.27) (p<.001 for each). Both the iconic and indexical icons elicited greater negative affect toward smoking, cognitive elaboration, perceived severity, and overall perceived effectiveness compared to the symbolic icon (p<.001 for all).
Mirroring these results, participants were split in their preference for the iconic and indexical versions when given the side-by-side comparison for icon choice. Participants thought of direct damage and health consequences with the iconic icon, and commented that it made them think of “the damage smoking would do my lungs and how that would affect my health and quality of life” and “my lungs getting clogged up with tars and possibly cancer.” Similarly, health consequences were salient to participants with the indexical icon, with participants thinking of “the limitations smoking would cause in my life because of the difficulty breathing,” and how someone couldn't “go about their daily lives due to the effects of smoking on lung function.”
Reproductive Organ Damage
For reproductive organ damage, ratings were highest for the iconic representation, a circle with line surrounding a fetus, (M = 3.99, SD = 1.16). The iconic image was more representative than the indexical, male and female figures with “x's” over their reproductive organs, (M = 3.76, SD = 1.23) or symbolic, a circle with line surrounding a baby carriage, (M = 3.26, SD = 1.34) icons (p<.001 for each). The iconic icon also elicited more negative affect, greater cognitive elaboration, perceived severity of reproductive organ damage, and perceived effectiveness of the icon compared to the indexical or symbolic icon (p<.001 for all).
The majority of participants also selected the iconic type in the side-by-side comparison. When they saw the iconic icon, participants thought about “my genitals not working properly,” “either miscarriages or not being able to conceive,” and “fetus damages and a baby with defects for life.”
Moderators
Icon type often had a larger impact among participants with perfect health literacy (n = 363) than among people with lower health literacy (n = 338). We summarize findings for 10 of 25 analyses where this difference was present (interactions p<.05; Table 4). The impact of icon type remained statistically significant in analyses stratified by health literacy (all p<.05). For addiction icons, perfect literacy participants had effect sizes as measured by partial eta squared that ranged from .46 to .63 across four outcomes, whereas lower health literacy participants had effect sizes that ranged from .21 to .52. The same pattern held for heart attack and stroke icons (range across two items, .20-.21 vs. .14-.16) and permanent breathing problem icons (range across four items, .17-.20 vs. .06-.09). Health literacy did not moderate the impact of cancer and reproductive organ damage icons. Smoking status did not moderate the effects of icon type for any outcome or health effect category.
Table 4. Impact of Semiotic Icon Type by Health Literacy Score.
| Perfect health literacy | Lower health literacy | |||||
|---|---|---|---|---|---|---|
| F value |
|
F value |
|
|||
| Addiction | ||||||
|
| ||||||
| Perceived representation | 618 | .63 | 349 | .51 | ||
| Affect | 308 | .46 | 89 | .21 | ||
| Cognitive elaboration | 572 | .61 | 359 | .52 | ||
| Perceived effectiveness | 470 | .57 | 294 | .47 | ||
|
| ||||||
| Heart attack and stroke | ||||||
|
| ||||||
| Perceived representation | 92.59 | .20 | 53 | .14 | ||
| Cognitive elaboration | 97.91 | .21 | 64 | .16 | ||
|
| ||||||
| Permanent breathing problems | ||||||
|
| ||||||
| Perceived representation | 71.09 | .17 | 26 | .07 | ||
| Affect | 71.62 | .17 | 21 | .06 | ||
| Cognitive elaboration | 92.49 | .20 | 25 | .07 | ||
| Perceived effectiveness | 91.71 | .20 | 31 | .09 | ||
Note. Table shows effect sizes for the 10 of 25 analyses where icon type interacted with health literacy. All F values for RM MANOVAs and univariate analyses are significant at p < .001.
Discussion
Communicating the health risks posed by exposure to chemicals in cigarette smoke in a way that is understandable and not misleading to lay audiences is a critical goal for tobacco control. We found systematic preferences for icon type that varied across health effects. When the health effect was attributable to a specific body part or easy-to-visualize symptom (e.g., heart attack and stroke), people preferred the iconic (concrete, direct representation) or indexical (evidential) icons. Conversely, people preferred symbolic (abstract) icons when the health effect could not be easily visualized or was not associated with a single, concrete representation (i.e., cancer, addiction). People consistently rated the preferred representative icons for each health effect as more effective and evaluated them as having a greater impact on thoughts and feelings. In other words, for an icon to be effective at communicating health harms of a risk behavior – by eliciting greater affect, elaboration, and perceived severity – it must also be representative of the health effect to the target audience. The present results suggest that icon effectiveness may be maximized by matching the abstractness of the icon with the abstractness of the health effect.
The preference for the iconic and indexical icons with illustrated figures conforms to prior research that anthropomorphic icons are more effective than graphical shapes for processing risk information (Zikmund-Fisher et al., 2014). It is possible that individuals are able to view themselves in these images; an example of “amplification through simplification” where the simple nature of icons, illustrations, or comics increases the perceived relevance of graphic medicine (Green & Myers, 2010; McCloud, 1993). Our findings also extend this prior research by showing that when the health effects were abstract or not associated with one specific visual representation, the symbolic icons more perceived as more representative and effective. These icons relied on metaphorical interpretations to communicate the health effect, metaphors that individuals continuously rely upon to understand complex phenomenon, such as health or disease (Lakoff & Johnson, 1980; Palmer-Wackerly & Krieger, 2015). Thus, it may be that individuals were easily able to connect the symbolic icons to their own lay theories of health to interpret the intended meaning (Sopory, 2005).
Icons must evoke a single concept or idea among viewers to effectively communicate information at a glance. Unlike explicit conventions used for language (e.g., syntax, semantics), however, visuals do not have pre-established codes to ensure systematic interpretation (Nakamura & Zeng-Treitler, 2012). Thus, to reduce ambiguity for the interpretation of these icons, we relied on the predictive mechanisms of Peircean semiotics in this exploratory study, along with pairing the visuals with explicit text labels for each health category. We found that individuals connect ideas about a disease to its representation via predictable pathways – iconic representations linked to concrete objects, indexes linked to evidence of the health effect or symptoms, and abstract symbols linked to social constructions of a health effect. Given these consistent findings, semiotics should be considered as a useful theoretical framework to guide icon development for health communication materials. Semiotics informs how individuals interpret icons.
The findings have direct practical implications for the design and development of tobacco control communication. The same distinct pattern for affective and cognitive evaluations of the icons was detected with the single icon choice item. When participants were given the side-by-side comparison of the icons, they made the same selections (with comparable effect sizes) as when asked about the individual icons. Icon choice was the last item of each health effect segment; thus, we do not know if there are effects of participants either using earlier items to clarify their thinking or transitioning to answering all items heuristically (generally good or bad). However, this distinct pattern indicates that simply asking a large group of people their preference could be a fruitful and efficient way to select visuals. From a methodological standpoint, these results suggest that researchers can ask the simpler choice question (which icon best represents the health effect?) rather than asking participants a long series of process-oriented questions. One caveat is that, because the “choice questions” came after lengthy evaluation of the relevant icons, additional research may be needed to establish whether the choice questions on their own lead to the same conclusion. Furthermore, researchers and practitioners should consider the advantages of crowdsourcing for icon development. Using a crowd-sourcing platform, such as MTurk, allows for an effective and inexpensive approach to detect shared preferences and interpretations of designs among large-scale lay audiences (Yu, Willis, Sun, & Wang, 2013).
This study provides a theory-based process for predicting how icons will be interpreted and what thoughts will be evoked – whether this is a successful match for the intended meaning will be context specific as findings are tied to the specific visuals used. Moreover, it is unlikely that one semiotic type will always be preferred given the inherently subjective (and implicit) nature of visual communication of icons. Additionally, people may have interpreted the icons with our health effect labels differently than they would have if no text had appeared with them. In practice, however, all icons likely need some explanatory text to increase the likelihood they will be decoded as intended.
Our findings may be specific to the convenience sample we recruited. The survey did not assess prior knowledge of the health harms of cigarette smoke prior to icon exposure because we were concerned that doing so would have influenced interpretations of the health effect categories. Replication with diverse and representative samples can establish the generalizability of our findings.
While our study design allowed for insights into perceived effectiveness of these icons, the ultimate interest of tobacco control is to measure the ability of these icons to aid communications in affecting tobacco use behavior to benefit public health. Future research should explore whether the presence of these icons, as additions to text labels of the health consequences of smoking and within larger message designs linking chemicals to specific harms, improves understanding or acceptance of tobacco control messages. Lastly, although we developed and tested these visuals for tobacco disclosures, researchers could consider applications of Peircian semiotics to aid in the development of pictorial warnings that meet legal requirements. People may perceive images as more factual if they are iconic (true representations, such as damaged organs) or indexical (showing the evidence of a disease, such as an individual experiencing symptoms), rather than symbolic (based on arbitrary or learned associations). Semiotic studies could also examine if a large majority of the public generally agrees whether a specific visual (the signifier) stands for a health harm (the signified).
Conclusion
Our findings contribute new insights for icon development for health communication, a process that is often anecdotal rather than informed by theory. Using semiotics as a framework to anticipate how people would interpret icons, we found systematic preferences detectable through cognitive and affective responses, as well as through simple preference selection. For communicating harms caused by cigarette smoke, health effects not easily visualized were best represented with symbolic icons. Health effects linked to a specific organ or observable symptom were best represented with iconic and indexical icons, respectively.
Table 2. Impact of Semiotic Icon Type.
| 1. | 2. | 3. | Pairwise Comparisons | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Iconic M (SD) | Indexical M (SD) | Symbolic M (SD) | F |
|
1-2 | 1-3 | 2-3 | ||
| Cancers | |||||||||
|
| |||||||||
| Perceived representation | 2.59 (1.39) | 2.99 (1.44) | 3.55 (1.33) | 107 | .13 | ** | ** | ** | |
| Affect | -.76 (1.17) | -.91 (1.23) | -1.54 (1.32) | 102 | .13 | * | ** | ** | |
| Cognitive elaboration | 2.22 (1.97) | 2.57 (1.06) | 3.81 (1.94) | 178 | .20 | ** | ** | ** | |
| Perceived severity | 3.65 (2.28) | 3.83 (2.20) | 4.63 (1.84) | 82 | .11 | ** | ** | ||
| Perceived effectiveness | 2.70 (1.34) | 2.91 (1.36) | 3.73 (1.25) | 156 | .19 | * | ** | ** | |
|
| |||||||||
| Addiction | |||||||||
|
| |||||||||
| Perceived representation | 2.47 (1.33) | 2.38 (1.35) | 4.55 (.72) | 938 | .57 | ** | ** | ||
| Affect | -.52 (1.04) | -.65 (1.06) | -1.89 (1.40) | 336 | .33 | * | ** | ** | |
| Cognitive elaboration | 2.00 (1.88) | 1.96 (1.88) | 4.80 (1.30) | 910 | .57 | ** | ** | ||
| Perceived severity | 3.09 (2.03) | 3.01 (2.07) | 4.67 (1.46) | 312 | .31 | ** | ** | ||
| Perceived effectiveness | 2.49 (1.27) | 2.52 (1.30) | 4.25 (.85) | 744 | .52 | ** | ** | ||
|
| |||||||||
| Heart attack and stroke | |||||||||
|
| |||||||||
| Perceived representation | 3.71 (1.22) | 4.50 (.77) | 3.78 (1.15) | 143 | .17 | ** | ** | ||
| Affect | -1.29 (1.35) | -1.85 (1.38) | -1.32 (1.29) | 65 | .09 | ** | ** | ||
| Cognitive elaboration | 3.60 (1.87) | 4.75 (1.47) | 3.73 (1.77) | 159 | .19 | ** | ** | ||
| Perceived severity | 4.52 (1.79) | 5.13 (1.39) | 4.54 (1.75) | 71 | .09 | ** | ** | ||
| Perceived effectiveness | 3.60 (1.25) | 4.28 (.94) | 3.65 (1.19) | 134 | .16 | ** | ** | ||
|
| |||||||||
| Permanent breathing problems | |||||||||
|
| |||||||||
| Perceived representation | 4.15 (.96) | 4.04 (1.05) | 3.45 (1.27) | 91 | .12 | ** | ** | ||
| Affect | -1.71 (1.29) | -1.62 (1.29) | -1.05 (1.31) | 81 | .10 | ** | ** | ||
| Cognitive elaboration | 4.43 (1.50) | 4.27 (1.61) | 3.40 (1.86) | 106 | .13 | ** | ** | ||
| Perceived severity | 4.86 (1.47) | 4.71 (1.57) | 4.23 (1.81) | 56 | .08 | * | ** | ** | |
| Perceived effectiveness | 4.15 (.95) | 4.05 (1.01) | 3.44 (1.23) | 114 | .14 | ** | ** | ||
|
| |||||||||
| Reproductive organ damage | |||||||||
|
| |||||||||
| Perceived representation | 3.99 (1.16) | 3.76 (1.23) | 3.26 (1.34) | 91 | .12 | ** | ** | ** | |
| Affect | -1.78 (1.31) | -1.33 (1.33) | -1.15 (1.36) | 75 | .10 | ** | ** | * | |
| Cognitive elaboration | 4.26 (1.81) | 3.55 (1.90) | 3.24 (1.95) | 109 | .14 | ** | ** | * | |
| Perceived severity | 4.12 (1.99) | 3.89 (1.93) | 3.54 (2.06) | 41 | .06 | * | ** | ** | |
| Perceived effectiveness | 3.96 (1.16) | 3.56 (1.24) | 3.31 (1.30) | 103 | .13 | ** | ** | ** | |
Note. Shading indicates icon types with the highest rating. n = 701. All F values for RM MANOVAs and univariate analyses are significant at p < .001. All items had 5-point scale with higher scores indicating higher amounts of the construct. Affect was the exception and ranged from -3 to 3 on a 7-point scale.
p < .05,
p < .001
Acknowledgments
Research reported in this publication was supported by grant number P50CA180907-03S1 from the National Cancer Institute and FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
References
- Family Smoking Prevention and Tobacco Control Act. Public Law 111–31, 123 Statute 1776. 2009 Jun 22; [Google Scholar]
- Andrews JC, Netemeyer RG, Kees J, Burton S. How graphic visual health earnings affect young smokers' thoughts of quitting. Journal of Marketing Research. 2014;51:165–183. [Google Scholar]
- Baker D, Williams M, Parker R, Gazmarian J, Nurss J. Development of a brief test to measure functional health literacy. Patient Education & Counseling. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Baker RR, Massey ED, Smith G. An overview of the effects of tobacco ingredients on smoke chemistry and toxicity. Food and Chemical Toxicology. 2004;42:53–83. doi: 10.1016/j.fct.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Boynton MH, Agans RP, Bowling JM, Brewer NT, Sutfin EL, Goldstein AO, Noar SM, Ribisl KM. Understanding how perceptions of tobacco constituents and the FDA relate to effective and credible tobacco risk messaging: A national phone survey of U.S. adults, 2014–2015. BMC Public Health. 2016;16:1–13. doi: 10.1186/s12889-016-3151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith JS. Longitudinal predictors of HPV vaccine initiation among adolescent girls in a high-risk geographic area. Sexually Transmitted Diseases. 2011;38:197. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Hall MG, Noar SM, Parada H, Stein-Seroussi A, Bach LE, Hanley S, Ribisl KM. Effect of pictorial cigarette pack warnings on changes in smoking behavior: A randomized clinical trial. JAMA Internal Medicine. 2016;176:905–912. doi: 10.1001/jamainternmed.2016.2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Casler K, Bickel L, Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon's MTurk, social media, and face-to-face behavioral testing. Computers in Human Behavior. 2013;29(6):2156–2160. [Google Scholar]
- Center for Disease Control and Prevention. Fact sheets: Smoking and tobacco use. 2016 Retrieved from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2013 Retrieved from https://www.cdc.gov/brfss/questionnaires/pdf-ques/2013brfss_english.pdf.
- Evans AT, Peters E, Strasser AA, Emery LF, Sheerin KM, Romer D. Graphic warning labels elicit affective and thoughtful responses from smokers: Results of a Randomized Clinical Trial. PLoS ONE. 2015;10:e0142879. doi: 10.1371/journal.pone.0142879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathelrahman AI, Omar M, Awang R, Cummings KM, Borland R, Samin ASBM. Impact of the new Malaysian cigarette pack warnings on smokers' awareness of health risks and interest in quitting smoking. International Journal of Environmental Research and Public Health. 2010;7:4089–4099. doi: 10.3390/ijerph7114089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowles J, Dybing E. Application of toxicological risk assessment principles to the chemical constituents of cigarette smoke. Tobacco Control. 2003;12:424–430. doi: 10.1136/tc.12.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Retamero R, Galesic M. Who proficts from visual aids: Overcoming challenges in people's understanding of risks. Social Science & Medicine. 2010;70:1019–1025. doi: 10.1016/j.socscimed.2009.11.031. [DOI] [PubMed] [Google Scholar]
- Green MJ, Myers KR. Graphic medicine: Use of comics in medical education and patient care. British Medical Journal. 2010;340:574–577. doi: 10.1136/bmj.c863. [DOI] [PubMed] [Google Scholar]
- Hall MG, Ribisl KM, Brewer NT. Smokers' and nonsmokers' beliefs about harmful tobacco constituents: Implications for FDA communication efforts. Nicotine & Tobacco Research. 2014;16:343–350. doi: 10.1093/ntr/ntt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht SS. Research opportunities related to establishing standards for tobacco products under the Family Smoking Prevention and Tobacco Control Act. Nicotine & Tobacco Research. 2012;14:18–28. doi: 10.1093/ntr/ntq216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann D, Hoffmann I. The changing cigarette: Chemical studies and bioassays. Smoking and Tobacco Control Monograph. 2001;13:159–192. [Google Scholar]
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Education and Counseling. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Katz MG, Kripalani S, Weiss BD. Use of pictorial aids in medication instructions: A review of the literature. American Journal of Health-System Pharmacy. 2006;63:2391–2397. doi: 10.2146/ajhp060162. [DOI] [PubMed] [Google Scholar]
- Lakoff G, Johnson M. Metaphors we live by. Chicago, IL: University of Chicago Press; 1980. [Google Scholar]
- McCloud S. Understanding comics: The invisible art. New York: Harper Collins Publishers Inc; 1993. [Google Scholar]
- Meppelink CS, Smit EG, Buurman BM, van Weert JC. Should we be afraid of simple messages? The effects of text difficulty and illustrations in people with low or high health literacy. Health Communication. 2015;30:1181–1189. doi: 10.1080/10410236.2015.1037425. [DOI] [PubMed] [Google Scholar]
- Messaris P. Visual persuasion: The role of images in advertising. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- Moracco KE, Morgan JC, Mendel J, Teal R, Noar SM, Ribisl KM, Brewer NT. “My first thought was croutons”: Perceptions of cigarettes and cigarette smoke constituents among adult smokers and nonsmokers. Nicotine & Tobacco Research. 2016;18:1566–1574. doi: 10.1093/ntr/ntv281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriarty S. The symbiotics of semiotics and visual communication. Journal of Visual Literacy. 2002;22:19–28. [Google Scholar]
- Nakamura C, Zeng-Treitler Q. A taxonomy of representation strategies in iconic communication. International Journal of Human-Computer Studies. 2012;70:535–551. doi: 10.1016/j.ijhcs.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer-Wackerly AL, Krieger JL. Dancing around infertility: The use of metaphors in a complex medical situation. Health Communication. 2015;30:612–623. doi: 10.1080/10410236.2014.888386. [DOI] [PubMed] [Google Scholar]
- Peirce CS. Peirce on signs: Writing on semiotic. Chapel Hill: University of North Carolina Press; 1991. [Google Scholar]
- Peters E, Västfjäll D, Slovic P, Mertz C, Mazzocco K, Dickert S. Numeracy and decision making. Psychological Science. 2006;17:407–413. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- Rodgman A, Perfetti TA. The chemical components of tobacco and tobacco smoke. Boca Raton, Florida: CRC press; 2013. [Google Scholar]
- Sopory P. Metaphor in formative evaluation and message design: An application to relationships and alcohol use. Health Communication. 2005;17:149–172. doi: 10.1207/s15327027hc1702_3. [DOI] [PubMed] [Google Scholar]
- Stevens JP. Intermediate statistics: A modern approach. 3rd. New York, NY: Routledge; 2007. [Google Scholar]
- Talhout R, Schulz T, Florek E, Van Benthem J, Wester P, Opperhuizen A. Hazardous compounds in tobacco smoke. International Journal of Environ Research and Public Health. 2011;8:613–628. doi: 10.3390/ijerph8020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Nicotine addiction and your health. 2016 Retrieved from http://betobaccofree.hhs.gov/health-effects/nicotine-health/
- United States Department of Health Human Services. Atlanta, GA: 2014. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Retrieved from http://www.surgeongeneral.gov/library/reports/50-years-of-progress/exec-summary.pdf. [Google Scholar]
- United States Food and Drug Administration. Harmful and potentially harmful constituents in tobacco products and tobacco smoke: Established list. 2012 Retrieved from http://www.fda.gov/TobaccoProducts/GuidanceComplianceRegulatoryInformation/ucm297786.htm.
- Wayne GF, Carpenter CM. Tobacco industry manipulation of nicotine dosing. Nicotine Psychopharmacology. 2009;192:457–485. doi: 10.1007/978-3-540-69248-5_16. [DOI] [PubMed] [Google Scholar]
- Yu B, Willis M, Sun P, Wang J. Crowdsourcing participatory evaluation of medical pictograms using Amazon Mechanical Turk. Journal of Medical Internet Research. 2013;15:e108. doi: 10.2196/jmir.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zikmund-Fisher BJ, Witteman HO, Dickson M, Fuhrel-Forbis A, Kahn VC, Exe NL, Valerio M, Holtzman L, Scherer L, Fagerlin A. Blocks, ovals, or people? Icon type affects risk perceptions and recall of pictographs. Medical Decision Making. 2014;34:443–453. doi: 10.1177/0272989X13511706. [DOI] [PMC free article] [PubMed] [Google Scholar]


