Abstract
The purpose of this study was to explore relations between food craving, caloric intake, and body mass index (BMI) changes over the course of an 18-month weight loss trial. Two-hundred two obese adults (mean BMI = 34.9 kg/m2; mean age = 51.30 years, 92.2% White; 57.8% female) who participated in a behavioral weight loss trial completed measures of food craving, caloric intake, and BMI at baseline, 6 and 18 months. From baseline to 6 months, higher initial food cravings were associated with more gradual and less steep reductions in BMI. Additionally, the relation between changes in food craving and BMI changes varied by levels of change in caloric intake, such that BMI change and change in food cravings were positively associated at low levels of change in caloric intake, but were unrelated at average and high levels of change in caloric intake. Similarly, from baseline to 6 months and from 6 to 18 months, the relation between changes in food craving and BMI changes also varied by initial levels of caloric intake. Explicit clinical targeting of food craving management may be beneficial for individuals beginning weight loss programs, especially for those who report higher levels of food craving at baseline. Baseline caloric intake and change in calorie intake over time may serve as moderators of the relation between food cravings and BMI.
Keywords: Food craving, Calorie intake, Body mass index, Weight loss
Introduction
Approximately 37.7% of adults in the United States are currently obese (Flegal et al., 2016). Obesity is associated with major health consequences including heart disease, stroke, type 2 diabetes, and increased risk for certain types of cancer (Bray, 2004). Excessive weight gain is primarily attributed to a persistent positive energy balance where calories consumed exceed calories expended (Janssen et al., 2005). Given the importance of achieving a negative energy balance to lose weight, the most efficacious dietary interventions for obesity require restriction of high calorie foods (Dietary Guidelines for Americans, 2010). Therefore, identifying variables associated with overeating is key to facilitating weight loss.
Food craving has been identified as one possible precursor to overeating (Gendall et al., 1998), and is characterized by a strong motivation or desire to consume a particular food item (Weingarten & Elston, 1990). It has been differentiated from hunger, which is a more general desire for food (Batra et al., 2013). Cross-sectionally, there is evidence that food craving is associated with calorie overconsumption (Hill et al., 1991; Lafay et al., 2001; White & Grilo, 2005). Additionally, individuals whose weight falls in the overweight or obese body mass index (BMI) range report higher frequencies of food craving than individuals whose weight falls in the normal BMI range (Abilés et al., 2010; Chao et al., 2014; Franken & Muris, 2005). In a cross-sectional study of 646 adults, Chao et al. (2014) found a significant positive relation between food craving and BMI. They also found significant positive associations between cravings for specific calorie dense foods (e.g., sweets, high fat foods, carbohydrates, and fast foods) and actual consumption of those respective foods. Abilés et al. (2010) compared bariatric surgery patients to a normal weight control group and found that the bariatric surgery patients reported significantly higher levels of food craving than the normal-weight controls. In sum, the available literature demonstrates relationships between greater cravings, greater energy intake, and elevated BMI, with food cravings often proposed as the driver of the relationship.
Longitudinal evidence has also reported relationships between food cravings, energy intake, and BMI, with experimental evidence suggesting that caloric restriction is related to decreased food cravings and weight loss decreased food cravings (Anton et al., 2012; Martin et al., 2011). The experimental evidence suggests that changes in food intake may actually influence food cravings. One potential explanation for this seemingly paradoxical relation is that food cravings may be conditioned expressions of hunger (Gibson & Desmond, 1999). In other words, food cravings develop from repeated pairings of specific foods with hunger, with the reduction in hunger and experience of consuming the food potentially providing negative and/or positive reinforcement (i.e., removal of the aversive state of hunger, and/or the positive effects produced from actual consumption of the specific food). The food specific craving may then be a consequence of conditioned tolerance and/or incentive). When consumption of the food item is reduced from the diet, extinction occurs leading to a decrease in cravings and subsequent food intake (Gibson & Desmond, 1999). This suggests that food cravings interact with food intake, in a feed forward cycle. The food craving-intake interaction may cycle with the reintroduction of specific, initially craved foods. Specifically, reintroduction of these foods may then increase craving and consumption (increasing caloric intake), resulting in weight gain.
Indeed, Martin et al. (2006) measured changes in craving over a 12-week weight loss program and found that cravings decreased as a function of calorie reduction. Further, participants who were prescribed a very low calorie, supplement-based diet (1675–2093 kJ/d) decreased cravings to a greater degree than participants who were prescribed a traditional, food-based low calorie diet (4187–6280 kJ/d). However, there was no significant relation found between changes in food craving and weight loss. A limitation of this study was that it was a shorter-term program, so conclusions cannot be made about longitudinal patterns of relations between food craving and weight loss. A longer-term trial compared changes in food craving between individuals randomized to a low carbohydrate diet condition versus a low-calorie/low-fat diet condition. Data were collected at 6 time points over the course of 2 years. Results indicated that over time, participants randomized to the low-carbohydrate diet significantly reduced food cravings for carbohydrates, and participants randomized to the low-calorie/low-fat diet significantly reduced food cravings for high fat foods (Martin et al., 2011). One limitation of these findings was that relations between weight loss and food craving were only examined via correlational analyses at each time point, and patterns of the relationship between change in BMI and food craving over time were not examined. Further, dietary intake were not collected, so adherence to the dietary recommendations is unknown. The conditioned expression of hunger hypothesis may suggest that variations in baseline calorie intake and changes in caloric intake over time may affect the predictive validity of craving for changes in BMI.
The current study extends the literature by examining relations between food craving, caloric intake, and BMI changes over the course of an 18-month behavioral weight loss trial via structural equation modeling and latent growth curve modeling. This statistical approach allows for longitudinal analysis of patterns of change and interactions between changes in all three variables over the course of the trial (baseline, 6 and 18 months; Berlin et al., 2014). This study is the first to our knowledge to investigate the predictive validity of food craving at baseline on BMI outcomes over the course of a weight loss trial. Given the cross-sectional findings from the 2-year weight loss trial, we hypothesized that greater reductions in food cravings would be associated with greater decreases in BMI across each time point. We also hypothesized that initial calorie intake and changes in calorie intake over time would moderate the relationship between food craving and BMI.
Method
Participants
Eligible participants had a BMI between 27 and 45 kg/m2 and were between 21 and 65 years old. Overall, 202 individuals (mean BMI = 34.9 kg/m2; mean age = 51.30 years, 92.2% White; 57.8% female) participated in an 18-month behavioral obesity intervention. Exclusion criteria included heart problems, use of weight loss medications or participation in another weight loss program, bariatric surgery, pregnancy or planning to become pregnant, allergies to foods used in the study, consumed less than five different types of nutrient-dense, energy-dense foods, or could not walk two blocks. For more details on the institutional review board-approved clinical trial see Raynor et al. (2012). Participating individuals provided informed consent and then were randomly assigned to one of two interventions: (1) Lifestyle Condition (Lifestyle) including a traditional hypocaloric, low-fat (1200–1500 kcal/day, ≤30% kcal from fat) diet or (2) a Lifestyle + Limited Variety Condition (Lifestyle + LV) including a traditional hypocaloric, low-fat diet and a goal to limit variety of snack food consumption.
Intervention
Three components were common to both intervention groups: a cognitive behavioral intervention, a diet prescription (1200–1500 kcal/day, ≤30% kcal from fat), and a physical activity prescription (40 min/day, five times/week). Participants in the Lifestyle + LV group were also instructed to reduce the variety of non-nutrient dense, energy-dense foods in their diet to only two food types throughout the intervention period. The goal of the intervention was to help assist participants with developing a healthy lifestyle and to achieve at least a 10% weight loss. For the first 6 months, participants met weekly, and then twice a month from months 7 to 18.
Measures
Demographics and anthropometrics
Basic demographic information (e.g. gender, age, education level) was collected by self-report measure at baseline. Height was measured in millimeters at baseline using a stadiometer and weight was measured at baseline, 6 and 18 months in kilograms using a calibrated digital scale. Participants were instructed to wear light clothing and to remove shoes when they were being measured. BMI was calculated as weight in kilograms divided by height in meters squared.
Food Craving Inventory
The Food Craving Inventory (FCI) is a 28-item self-report measure assessing food cravings for different foods (White & Grilo, 2005; White et al., 2002). Five food craving scores pertaining to different food varieties (e.g., fats, sweets, carbohydrates, fast food fats, and total) can be derived from the measure. The total food craving score was used for the purpose of the current study. Test–retest (α = 0.86) and internal consistency analyses (α = 0.93) have demonstrated strong reliability for the total scale. Additionally, the FCI has demonstrated good content, concurrent, construct, and discriminant validity (White et al., 2002).
Dietary intake
Overall energy intake was obtained from three 24-h dietary recalls (2 weekdays and 1 weekend day) over the phone at each time point (e.g. baseline, 6 and 18 months). Interviewers were blind to intervention assignment and used the Nutrition Data System Software for Research developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN. Participants used 2-dimensional food shapes they were given to facilitate estimating portion sizes.
Analytic plan
Pearson correlations, latent growth modeling, and path analyses were conducted in order to examine the relations among changes in participant food craving, caloric intake, and BMI. Full information robust maximum likelihood estimation allowed for the modeling of multiple change processes with missing and non-normally distributed data (Little et al., 2014; Muthén & Muthén, 1998–2012).
First, linear, quadratic, and piecewise growth models (with residual variances fixed to zero for identification purposes when necessary) were evaluated separately for each variable of interest to characterize the nature of change. The goodness of fit for the growth models were evaluated using the Robust Chi Square statistic (χ2), where increases in values represent worse fit (Yuan & Bentler, 2000). However, the Chi square statistic is sensitive to sample size (Hu & Bentler, 1999), therefore the Comparative Fit Index (CFI) was also included. Values of ≥0.90 and ≥0.95 on the CFI represent an adequate and good model fit respectively (Hu & Bentler, 1999). The Root Mean Square Error of Approximation (RMSEA; MacCallum et al., 1996) statistic was also supplied as a population-based index that measures error of approximation (Browne & Cudeck, 1993). RMSEA values are interpreted in terms of fit as follows: good (<0.05), acceptable (0.05–0.08), and poor (>0.10; Hu & Bentler, 1999; MacCallum et al., 1996). The Standardized Root Mean Square Residual (SRMR) measures the overall difference between the observed and predicted correlations, with values less than 0.08 generally indicating good fit (Hu & Bentler, 1999).
In addition, linear growth models between the first and last time points were conducted to characterize the overall change from baseline to 18 months. Pending significant variability in the rates of change and initial values, factor scores from these models were exported and used with path analysis to decrease model complexity and facilitate model convergence. Two-way and three-way interactions among intercepts and slopes of relevant variables were tested, but higher-order interactions were removed from the final model if non-significant. Intervention group was not included in the model since there were no between group differences in weight loss (Raynor et al., 2012), food craving, or change in food craving [Wilks’ Lambda = 0.962, F(3, 200) = 2.619, p > 0.05]. All model analyses were conducted in Mplus 7.20 (Muthén & Muthén, 1998–2012).
Significant interactions were examined further using interaction plots with changes in the predictor represented as individuals increasing or decreasing on that specific variable plotted on the x-axis, changes in BMI plotted on the Y axis, and different lines representing the mean of the moderator, 1 SD above, and 1 SD below the mean. If interactions involved change variables, graphical depictions were presented using change values for “decreasers” (at the average value for those whose change scores were negative), “increasers” (at the average value for those who change scores were positive), at low (−1 SD), average, and high (+1 SD) levels of the moderator.
Results
Bivariate correlations are presented in Table 1 for initial and changes in variables from T1 to T4 and Table 2 for initial and changes in variables from T1 to T2. Similar relationships among variables were found from T1 to T4 and T1 to T2. Initial food craving was positively correlated with initial BMI. Initial food craving was positively correlated with initial calories and negatively correlated with change in food cravings and change in calories. Additionally, change in calories was positively associated with change in cravings.
Table 1.
Correlations of intercepts and slopes from T1 to T4
| 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|
| 1. Change in BMI | |||||
| 2. Initial BMI | −0.21* | ||||
| 3. Initial food cravings | −0.12 | 0.15* | |||
| 4. Initial calories | 0.03 | 0.09 | 0.21* | ||
| 5. Change in food craving | 0.12 | 0.01 | −0.63* | −0.05 | |
| 6. Change in calories | 0.07 | −0.10 | −0.23* | −0.69* | 0.15* |
Significant at the <0.05 p value
Table 2.
Correlations of intercepts and slopes from T1 to T2
| 1. | 2. | 3. | 4. | 5. | ||
|---|---|---|---|---|---|---|
| 1. Change in BMI | m = −0.64, SD = 0.36 | |||||
| 2. Initial BMI | −0.32* | m = 34.91, SD = 4.33 | ||||
| 3. Initial food cravings | 0.03 | 0.15* | m = 2.54, SD = 0.68 | |||
| 4. Initial calories | −0.02 | 0.09 | 0.21* | m = 201.34, SD = 62.99 | ||
| 5. Change in food craving | 0.08 | 0.04 | −0.51* | −0.05 | m = −0.06, SD = 0.11 | |
| 6. Change in calories | 0.08 | −0.12 | −0.05* | −0.79* | 0.18* | m = −10.67, SD = 9.41 |
Significant at the <0.05 p value
A piecewise model was found to be the best-fitting model for all the variables and intercepts and slopes from each of the growth models are presented in Table 3. Additionally, linear models examining changes from the first time point to the last are also included in Table 3. As reported previously (Buscemi et al., 2014), BMIs on average decreased (slope 1) in a linear manner from T1 (baseline) to T2 (6 months), but increased marginally from T2 (6 months) to T4 (18 months; slope 2). On average, the change from T1 to T4 is characterized by decreases in BMIs. Similarly, on average, changes in calories consumed decreased during the intervention from T1 to T2, but increased marginally from T2 to T4 with significant variability in these estimates. Overall, the change from T1 to T4 is characterized by average decreases in calories. Additionally, food craving decreased in a linear manner from T1 to T2 and there was no significant change after that initial decrease in food craving from T2 to T4, with significant variability in these estimates.
Table 3.
Latent growth curve models of changes in key variables
| Estimate | S.E. | Estimate/S.E. | p value | |
|---|---|---|---|---|
| BMI piecewise model results | ||||
| Intercept | 34.91 | 0.30 | 115.39 | <0.01 |
| Slope 1 | −0.64 | 0.03 | −25.12 | <0.01 |
| Slope 2 | 0.05 | 0.01 | 3.24 | <0.01 |
| Calories piecewise model results (divided by 100) | ||||
| Intercept | 20.13 | 0.43 | 47.08 | <0.01 |
| Slope 1 | −1.07 | 0.07 | −15.63 | <0.01 |
| Slope 2 | 0.15 | 0.03 | 5.72 | <0.01 |
| Food cravings piecewise model results | ||||
| Intercept | 2.54 | 0.05 | 54.41 | <0.01 |
| Slope 1 | −0.060 | 0.01 | −7.10 | <0.01 |
| Slope 2 | −0.01 | 0.01 | −1.70 | 0.09 |
| BMI Linear model baseline to post | ||||
| Intercept | 34.91 | 0.30 | 115.39 | <0.01 |
| Slope | −1.97 | 0.13 | −15.50 | <0.01 |
| Food cravings linear model baseline to post | ||||
| Intercept | 2.53 | 0.05 | 54.44 | <0.01 |
| Slope | −0.02 | 0.01 | −8.69 | <0.01 |
| Calories linear model baseline to post (divided by 100) | ||||
| Intercept | 20.13 | 0.43 | 47.08 | <0.01 |
| Slope | −0.26 | 0.02 | −11.36 | <0.01 |
BMI changes across active treatment: T1 to T2
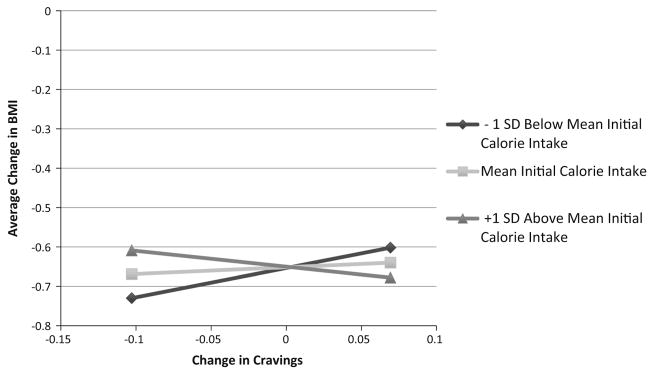
In the model examining BMI change across the weekly intervention phase, initial food craving score, the initial caloric intake by change in food craving interaction, and change in food craving by change in caloric intake interaction were significant predictors of linear BMI Change from T1 to T2 (see Table 4). More specifically, higher initial food cravings were associated with more gradual and less steep reductions in BMI (est. = 0.076, t = 2.304, p = 0.042). The relation between changes in food craving and BMI changes varied by level of initial caloric intake, such that BMI and food craving moved in tandem at low (−1 SD) initial levels of caloric intake (est. = 0.762, t = 1.942, p = 0.052), but this relation became weaker (and non-significant) at average (est. = 0.177, t = 0.661, p = 0.509), and high (+1 SD) levels of initial caloric intake (est. = −0.408, t = −1.113, p = 0.266). Figure 1 graphically presents the estimated BMI change values for “food craving decreasers” (at the average value for those who decreased food craving), “food craving increasers” (at the average value for those who increased food craving), at low (−1 SD), average, and high (+1 SD) levels of initial caloric intake.
Table 4.
Regression model results and associated changes in BMI from T1 to T2
| Estimate | S.E. | Est./S.E. | p value | |
|---|---|---|---|---|
| Changes in BMI from T1 to T2 predicted by | ||||
| Initial BMI | −0.03 | 0.01 | −4.65 | <0.01 |
| Initial food cravings | 0.08 | 0.04 | 2.03 | 0.04 |
| Initial calories | 0.01 | 0.01 | 0.82 | 0.41 |
| Change in food cravings | 0.18 | 0.27 | 0.66 | 0.51 |
| Change in calories | 0.08 | 0.05 | 1.78 | 0.08 |
| Initial calories × change in calories | −0.01 | 0.01 | −2.48 | 0.01 |
| Change in food cravings × change in calories | −0.93 | 0.34 | −2.69 | <0.01 |
| Initial calories × change in food cravings | −0.10 | 0.04 | −2.17 | 0.03 |
Fig. 1.
From baseline to 6 months, the relation between changes in craving and BMI changes varied by level of initial caloric intake, such that BMI and craving moved in tandem at low (−1 SD) initial levels of caloric intake (est. = 0.762, t = 1.942, p = 0.052), but this relation became weaker (and non-significant) at average (est. = 0.177, t = 0.661, p = 0.509), and high (+1 SD) levels of initial caloric intake (est. = −0.408, t = −1.113, p = 0.266). This line graph presents the estimated BMI change values for “craving decreasers” (at the average value for those who decreased craving), “craving increasers” (at the average value for those who increased craving), at low (−1 SD), average, and high (+1 SD) levels of initial caloric intake
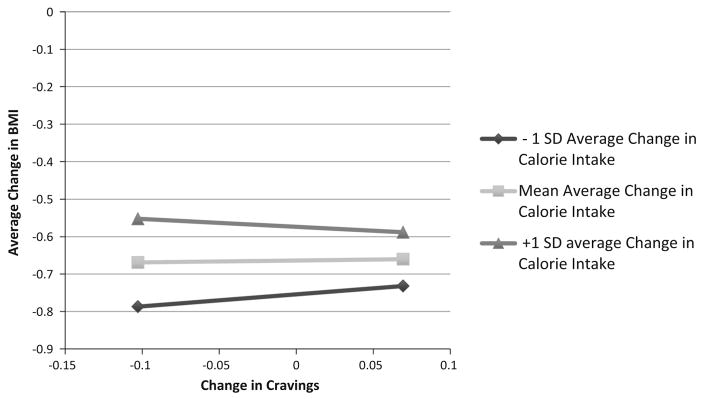
Additionally, results demonstrated that the relation between changes in food craving and BMI changes varied by levels of change in caloric intake, such that BMI change and change in food cravings moved in tandem at low levels of change in caloric intake (−1 SD below the average change; est. = 1.044, t = 2.740, p = 0.006), but were unrelated at average (est. = 7.17, t = 1.64, p = 0.10), and high levels of change in caloric intake (+1 SD above the average change; est. = 2.52, t = 0.52, p = 0.60). Figure 2 graphically presents the estimated BMI change values for “food craving decreasers” (at the average value for those who decreased food craving from T1 to T2), “food craving increasers” (at the average value for those who increased food craving from T1 to T2), at low (−1 SD), average, and high (+1 SD) levels of change in caloric intake.
Fig. 2.
From baseline to 6 months, the relation between changes in craving and BMI changes varied by levels of change in caloric intake, such that BMI change and change in cravings moved in tandem at low levels of change in caloric intake (−1 SD below the average change; est. = 1.044, t = 2.740, p = 0.006), but were unrelated at average (est. = 7.17, t = 1.64, p = 0.10), and high levels of initial caloric intake (+1 SD above the average change; est. = 2.52, t = 0.52, p = 0.60). This line graph presents the estimated BMI change values for “craving decreasers” (at the average value for those who decreased craving from T1 to T2), “craving increasers” (at the average value for those who increased craving from T1 to T2), at low (−1 SD), average, and high (+1 SD) levels of change in caloric intake
BMI changes across the entire trial: T1 to T4
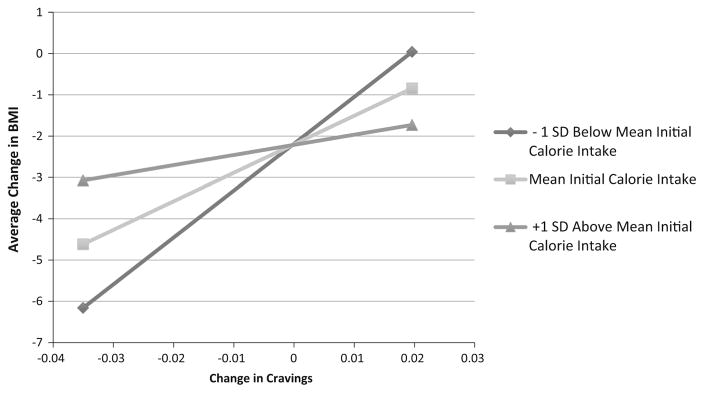
In the model examining BMI change across the trial, initial BMI and the initial caloric intake by change in food craving interaction were significant predictors of linear BMI Change from T1 to T4 (see Table 5). The relation between changes in food craving and BMI changes varied by level of initial caloric intake, such that BMI and food craving moved in tandem at low (−1 SD) initial levels of caloric intake (est. = 11.78, t = 2.446, p = 0.014), but unrelated at average (est. = 7.17, t = 1.64, p = 0.10), and high (+1 SD) levels of initial caloric intake (est. = 2.52, t = 0.52, p = 0.60). Figure 3 graphically presents the estimated BMI change values for “food craving decreasers” (at the average value for those who decreased food craving), “food craving increasers” (at the average value for those who increased food craving), at low (−1 SD), average, and high (+1 SD) levels of initial caloric intake.
Table 5.
Regression model results and associated changes in BMI from T1 to T4
| Estimate | S.E. | Est./S.E. | p value | |
|---|---|---|---|---|
| Changes in BMI from T1 to T4 predicted by | ||||
| Initial BMI | −0.08 | 0.03 | −2.85 | 0.004 |
| Initial food cravings | 0.29 | 0.21 | 1.39 | 0.17 |
| Change in food cravings | 7.17 | 4.36 | 1.64 | 0.10 |
| Initial calories | −0.01 | 0.02 | −0.51 | 0.60 |
| Change in calories | 0.47 | 0.61 | 0.77 | 0.44 |
| Initial calories × change in calories | −0.11 | 0.04 | −2.48 | 0.01 |
| Initial calories × change in food cravings | −0.79 | 0.37 | −2.17 | 0.03 |
Fig. 3.
From baseline to 18 months, the relation between changes in craving and BMI changes varied by level of initial caloric intake, such that BMI and Craving moved in tandem at low (−1 SD) initial levels of caloric intake (est. = 11.78, t = 2.446, p = 0.014), but unrelated at average (est. = 7.17, t = 1.64, p = 0.10), and high (+1 SD) levels of initial caloric intake (est. = 2.52, t = 0.52, p = 0.60). The line graph presents the estimated BMI change values for “craving decreasers” (at the average value for those who decreased craving), “craving increasers” (at the average value for those who increased craving), at low (−1 SD), average, and high (+1 SD) levels of initial caloric intake
Discussion
Food craving is believed to be an important factor in calorie overconsumption (Hill et al., 1991; Lafay et al., 2001; White & Grilo, 2005), with overconsumption leading to weight gain (Abilés, et al., 2010; Chao et al., 2014; Franken & Muris, 2005). In this frame work, cravings drive the relationship between intake and BMI. However, according to the conditioned expression of hunger conceptualization of food craving, cravings and intake interact, influencing BMI. Decreased caloric intake results in reduced cravings given the reduction of consumption of highly craved foods, which leads to reduction of the reinforcing value of those foods (Gibson & Desmond, 1999), further reducing energy intake. Our study extends previous research by including change in caloric intake (measured by a 24-h recall) in the analyses and investigating relations between food craving, caloric intake, and weight changes longitudinally to better understand how cravings and energy intake are related to each other and influence BMI.
Consistent with previous literature (Anton et al., 2012; Martin et al., 2006, 2011), diet restriction and food craving showed similar patterns of reduction during the active (weekly) treatment period. Importantly, from baseline to 6 months, higher levels of initial food craving predicted less steep declines in BMI. Elevated craving may portend a difficulty in decreasing the consumption of highly palatable, craved foods necessary for weight loss. In addition to the finding that higher levels baseline craving predicted less successful weight loss, we also found that initial caloric consumption and change in calorie consumption impacted the relation between food craving and BMI. Specifically, over the course of the trial, changes in BMI and food craving were positively associated at low initial levels of caloric intake, but were unrelated at average and high levels of initial caloric intake. Similarly, from baseline to 6 months, BMI change and change in food cravings were positively related at low levels of change in caloric intake, but were unrelated at average and high levels of change in caloric intake. Conceptualizing food craving as a conditioned response, it is possible that individuals with lower caloric intake at baseline had less of a reduction in caloric intake over time, thus leading to increased responsiveness to cravings. Additionally, those with less of a reduction in energy intake may be more susceptible to responding to increased cravings by consuming craved foods, influencing BMI. Results may suggest that a greater reduction in energy may be protective against responding to cravings due to extinction, whereas less of a reduction in energy decreases the opportunity for extinction. Although previous studies have demonstrated cross-sectional positive relations between increased levels of craving and BMI (Abilés et al., 2010; Chao et al., 2014; Franken & Muris, 2005), the finding that initial high levels of food craving may be associated with less successful weight loss is a novel contribution to the literature, with several important clinical implications. Namely, targeting food cravings clinically might be beneficial for individuals enrolled in weight loss programs who report higher levels of food craving at baseline. Acceptance-based interventions have shown promise in reducing food craving (Alberts et al., 2010; Forman et al., 2007, 2012; Hooper et al., 2012). Key intervention components of acceptance-based strategies include (1) normalizing cravings; (2) encouraging participants to accept thoughts about cravings rather than trying to change them; and (3) providing psychoeducation around the ability to accept cravings without acting on them. A second emerging clinical strategy for reducing cravings is episodic future thinking (EFT; Daniel et al., 2013). EFT is thought to reduce impulsivity and to increase the ability to delay gratification by emphasizing a more reinforcing future reward. Both of these strategies may be useful for clinicians working with individuals with high levels of baseline food craving at the start of a weight loss program.
This study has several limitations. First, the sample was primarily White, limiting our ability to generalize findings to other racial/ethnic minority groups. Second, our analyses were limited by the measures collected within the context of our study. There are several other variables that have been found to be associated with food craving that we were unable to include such as hunger, stress level, and impulsivity. Finally, we did not investigate relations between food cravings for specific food items and actual consumption of craved items (e.g., Chao et al., 2014).
Despite these limitations, this study contributes to the food craving and weight loss literature by examining longitudinal change patterns and interactions between food craving, calorie consumption, and BMI change in the context of a behavioral weight loss trial. This study was the first to provide support that initial food craving level may be an important factor to consider during weight loss. Results also highlight the impact of caloric intake on the relation between food craving and BMI, and suggest that greater caloric reduction may be protective against food cravings, and subsequently, BMI. Future studies should explore how these variables relate in more diverse samples. Additionally, future research should examine how explicitly targeting food craving affects overall weight loss in the context of a randomized controlled trial.
Acknowledgments
Funding was provided by National Institute of Diabetes and Digestive and Kidney Diseases (US) (Grant No. R01DK074721).
Footnotes
Compliance with ethical standards
Conflict of interest
Joanna Buscemi, Tiffany M. Rybak, Kristoffer S. Berlin, James G. Murphy and Hollie A. Raynor declare that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Abilés V, Rodríguez-Ruiz S, Abilés J, Mellado C, García A, Pérez de la Cruz A, et al. Psychological characteristics of morbidly obese candidates for bariatric surgery. Obesity Surgery. 2010;20:161–167. doi: 10.1007/s11695-008-9726-1. [DOI] [PubMed] [Google Scholar]
- Alberts HJ, Mulkens S, Smeets M, Thewissen R. Coping with food cravings. Investigating the potential of a mindfulness-based intervention. Appetite. 2010;55:160–163. doi: 10.1016/j.appet.2010.05.044. [DOI] [PubMed] [Google Scholar]
- Anton SD, Gallagher J, Carey VJ, Laranjo N, Cheng J, Champagne CM, et al. Diet type and changes in food craving following weight loss: Findings from the POUNDS LOST trial. Eating and Weight Disorders. 2012;17:e101–e108. doi: 10.1007/BF03325333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra P, Das SK, Salinardi T, Robinson L, Saltzman E, Scott T, et al. Relationship of cravings with weight loss and hunger. Results from a 6 month worksite weight loss intervention. Appetite. 2013;69:1–7. doi: 10.1016/j.appet.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Berlin KS, Parra GR, Williams NA. An introduction to latent variable mixture modeling (part 2): Longitudinal latent class growth analysis and growth mixture models. Journal of Pediatric Psychology. 2014;39:188–203. doi: 10.1093/jpepsy/jst085. [DOI] [PubMed] [Google Scholar]
- Bray GA. Medical consequences of obesity. Journal of Clinical Endocrinology and Metabolism. 2004;89:2583–2589. doi: 10.1210/jc.2004-0535. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–161. [Google Scholar]
- Buscemi J, Murphy JG, Berlin KS, Raynor HA. A behavioral economic analysis of changes in food-related and food-free reinforcement during weight loss treatment. Journal of Consulting and Clinical Psychology. 2014;82:659–669. doi: 10.1037/a0036376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao A, Grilo CM, White MA, Sinha R. Food cravings, food intake and weight status in a community-based sample. Eating Behaviors. 2014;15:478–482. doi: 10.1016/j.eatbeh.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel TO, Epstein LH, Stanton CM. The future is now: Reducing impulsivity and energy intake using episodic future thinking. Psychological Science. 2013;24:2339–2342. doi: 10.1177/0956797613488780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carroll MD. Trends in obesity among adults in the United States, 2005–2014. JAMA. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, Juarascio AS, Butryn ML, Herbert JD. Comparison of acceptance-based and standard cognitive-based coping strategies for craving sweets in overweight and obese women. Eating Behaviors. 2012;14:64–68. doi: 10.1016/j.eatbeh.2012.10.016. [DOI] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, McGrath KB, Herbert JD, Brandsma LL, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: An analog study. Behaviour Research and Therapy. 2007;45:2372–2386. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Franken IH, Muris P. Individual differences in reward sensitivity are related to food craving and relative body weight in healthy women. Appetite. 2005;45:198–201. doi: 10.1016/j.appet.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Gendall KA, Joyce PR, Sullivan PF, Bulik CM. Food cravers: Characteristics of those who binge. International Journal of Eating Disorders. 1998;23:353–360. doi: 10.1002/(sici)1098-108x(199805)23:4<353::aid-eat2>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Gibson EL, Desmond E. Chocolate craving and hunger state: Implications for the acquisition and expression of appetite and food choice. Appetite. 1999;32:219–240. doi: 10.1006/appe.1998.0207. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Weaver CF, Blundell JE. Food craving, dietary restraint and mood. Appetite. 1991;17:187–197. doi: 10.1016/0195-6663(91)90021-j. [DOI] [PubMed] [Google Scholar]
- Hooper N, Sandoz EK, Ashton J, Clarke A, McHugh L. Comparing thought suppression and acceptance as coping techniques for food cravings. Eating Behaviors. 2012;13:62–64. doi: 10.1016/j.eatbeh.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Janssen I, Katzmarzyk P, Boyce W, Vereecken C, Mulvihill C, Roberts C, et al. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obesity Reviews. 2005;6:123–132. doi: 10.1111/j.1467-789X.2005.00176.x. [DOI] [PubMed] [Google Scholar]
- Lafay L, Thomas F, Mennen L, Charles MA, Eschwege E, Borys JM, et al. Gender differences in the relation between food cravings and mood in an adult community: Results from the Fleurbaix Laventie Ville Sante study. International Journal of Eating Disorders. 2001;29:195–204. doi: 10.1002/1098-108x(200103)29:2<195::aid-eat1009>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Little TD, Jorgensen TD, Lang KM, Moore EWG. On the joys of missing data. Journal of Pediatric Psychology. 2014;39:151–162. doi: 10.1093/jpepsy/jst048. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130. [Google Scholar]
- Martin CK, McClearnon FJ, Chellino A, Correa JB. Handbook of behavior, food, and nutrition. New York: Springer; 2011a. Food cravings: A central construct in food intake behavior, weight loss, and the neurobiology of appetite behavior; pp. 741–755. [Google Scholar]
- Martin CK, O’Neil PM, Pawlow L. Changes in food cravings during low-calorie and very-low-calorie diets. Obesity (Silver Spring) 2006;14:115–121. doi: 10.1038/oby.2006.14. [DOI] [PubMed] [Google Scholar]
- Martin CK, Rosenbaum D, Han H, Geiselman P, Wyatt H, Hill J, et al. Change in food cravings, food preferences, and appetite during a low-carbohydrate and low-fat diet. Obesity (Silver Spring) 2011b;19:1963–1970. doi: 10.1038/oby.2011.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Raynor HA, Steeves EA, Hecht J, Fava JL, Wing RR. Limiting variety in non-nutrient-dense, energy-dense foods during a lifestyle intervention: A randomized controlled trial. American Journal of Clinical Nutrition. 2012;95:1305–1314. doi: 10.3945/ajcn.111.031153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary guidelines for Americans. 7. Washington, DC: U.S. Government Printing Office; 2010. Dec, [Google Scholar]
- Weingarten HP, Elston D. The phenomenology of food cravings. Appetite. 1990;15:231–246. doi: 10.1016/0195-6663(90)90023-2. [DOI] [PubMed] [Google Scholar]
- White MA, Grilo CM. Psychometric properties of food craving inventory among obese patients with binge eating disorder. Eating Behaviors. 2005;6:239–245. doi: 10.1016/j.eatbeh.2005.01.001. [DOI] [PubMed] [Google Scholar]
- White MA, Whisenhunt BL, Williamson DA, Greenway FL, Netemeyer RG. Development and validation of the food-food craving inventory. Obesity Research. 2002;10:107–114. doi: 10.1038/oby.2002.17. [DOI] [PubMed] [Google Scholar]
- Yuan K, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methdology. 2000;30:165–200. [Google Scholar]