Abstract
Background
A patellar dislocation is a common knee injury in the young, athletic patient population. Recent trends indicate that the use of long-term nonoperative treatment is decreasing, and surgical intervention is more commonly recommended for those patients who fail initial nonoperative management with recurrent patellar dislocations. Medial patellofemoral ligament (MPFL) reconstruction has become increasingly utilized in this regard.
Purpose
To evaluate outcomes, particularly return to sports and its relationship to postoperative instability, of isolated MPFL reconstruction for the treatment of recurrent patellar dislocations.
Study Design
Systematic review and meta-analysis.
Methods
A review of the current literature was performed using the terms “medial patellofemoral ligament reconstruction” and “MPFL reconstruction” in the electronic search engines PubMed and EBSCOhost (CINAHL, MEDLINE, SPORTDiscus) on July 29, 2015, yielding 1113 abstracts for review. At the conclusion of the search, 14 articles met the inclusion criteria and were included in this review of the literature. Means were calculated for population size, age, follow-up time, and postoperative Tegner scores. Pooled estimates were calculated for postoperative Kujala scores, return to play, total risk of postoperative instability, risk of positive apprehension sign, and risk of reoperation.
Results
The mean patient age associated with MPFL reconstruction was 24.4 years, with a mean postoperative Tegner score of 5.7. The pooled estimated mean postoperative Kujala score was 85.8 (95% CI, 81.6–90.0), with 84.1% (95% CI, 71.1%–97.1%) of patients returning to sports after surgery. The pooled total risk of recurrent instability after surgery was 1.2% (95% CI, 0.3%–2.1%), with a positive apprehension sign risk of 3.6% (95% CI, 0%–7.2%) and a reoperation risk of 3.1% (95% CI, 1.1%–5.0%).
Conclusion
A high percentage of young patients return to sports after isolated MPFL reconstruction for chronic patellar instability, with short-term results demonstrating a low incidence of recurrent instability, postoperative apprehension, and reoperations.
Keywords: MPFL reconstruction, medial patellofemoral ligament, patellar reconstruction, patellar instability
A patellar dislocation is one of the most common acute knee disorders in children and adolescents.39,43,44,55,56,63 The incidence of dislocations among pediatric patients is estimated at 43 per 100,000, with a peak incidence for patients of all ages occurring at age 15 years.44,55 The clinical presentation includes frequent “giving way” episodes, swelling, restricted knee range of motion (ROM), and limited functional activities.2,63 These injuries are associated with significant morbidity such as recurrent instability and patellofemoral osteoarthritis and can lead to physical activity modifications and declines in physical capacity.2,31,56,58 Long-term negative outcomes could potentially be associated with declines in physical fitness and psychosocial coping levels in these young patients who are isolated from their peers.37,67
Nonoperative treatment was long considered the standard of care for patellar dislocations.4,6,74 Currently, surgical treatment is recommended for recurrent patellar instability, osteochondral fractures with loose bodies, and failed nonoperative measures of functional rehabilitation.62 The selection of appropriate surgical procedures is dependent on the underlying pathophysiology of patellar instability, which is often anatomic in nature. There is a clear association between lateral patellar dislocations and medial soft tissue injuries.42 To address the pathological changes associated with patellar instability, medial patellofemoral ligament (MPFL) reconstruction is frequently recommended. 38 Since Ellera Gomes15 reported that MPFL reconstruction is the preferred surgical treatment for recurrent patellar instability, this procedure has been implemented on a large scale both in isolation and in combination with other procedures to correct soft tissue imbalance or bony malalignment.65 Recently, investigators have reported that isolated MPFL reconstruction may yield better postoperative outcomes in patients without significant anatomic abnormalities when compared with combined procedures.17
After surgery, clinicians have traditionally utilized time, ROM, strength, and subjective measures as guidelines for return-to-sports criteria.2,8,25,68 In a review by Fisher et al,19 77.3% of athletes returned to sports at their preinjury level after MPFL reconstruction. Recent reviews by Tompkins and Arendt69 and Matic et al33 have reported redislocation and failure rates of 1% and 6.6%, respectively, after MPFL reconstruction. However, because of the wide variety of concomitant procedures that are often performed with MPFL reconstruction, as well as the variability in reported outcome measures, many previous reviews have evaluated heterogeneous populations.69 Consequently, it is difficult to draw conclusions relative to the efficacy of the various surgical treatments for patellar instability.
To our knowledge, there are currently no published studies that systematically evaluate both subjective and clinical outcomes after true isolated MPFL reconstruction for the treatment of recurrent patellar instability. The purpose of the current systematic review was to summarize the existing knowledge of the treatment of patellar instability with isolated MPFL reconstruction, including patient selection criteria and outcomes associated with this procedure, specifically recurrent instability and return to sports.
METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed when conducting and reporting this review and meta-analysis.
Literature Search
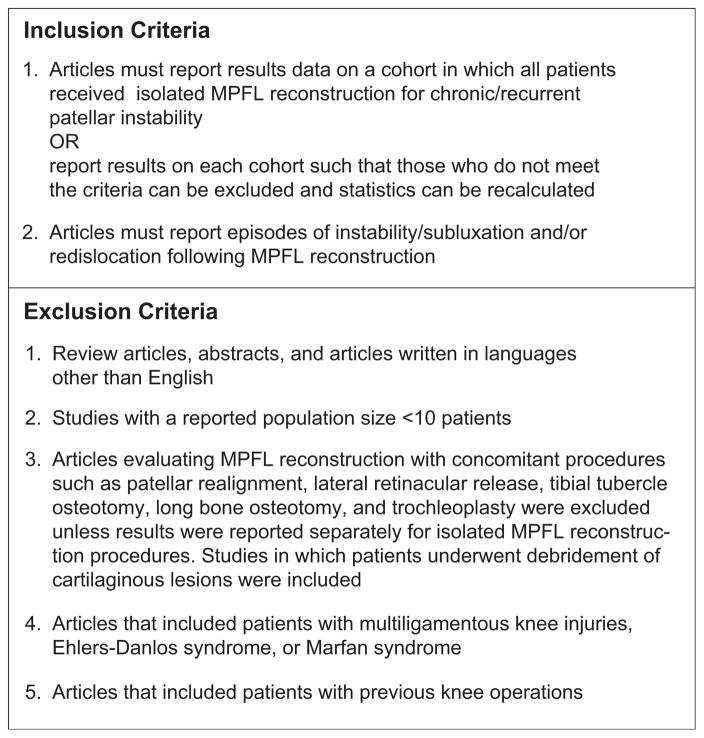
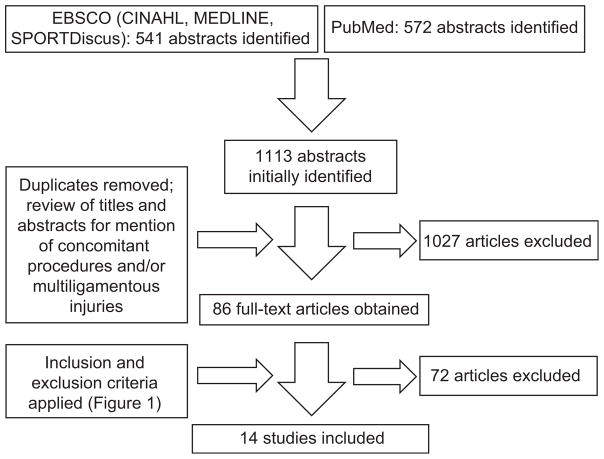
A systematic review of the current literature was performed on July 29, 2015, using the terms “medial patellofemoral ligament reconstruction” and “MPFL reconstruction” in the electronic search engines PubMed and EBSCOhost (CINAHL, MEDLINE, SPORTDiscus). The searches were limited to articles written in English, and they yielded 1113 abstracts for review. The full text of an article was obtained if the title and abstract discussed MPFL reconstruction without the mention of concomitant surgical procedures, multiligamentous damage, Ehlers-Danlos syndrome, or Marfan syndrome. The inclusion and exclusion criteria described in Figure 1 were applied to 86 full-text articles.
Figure 1.
Inclusion and exclusion criteria for the literature review. MPFL, medial patellofemoral ligament.
The references listed in recent reviews were also examined to determine the potential for inclusion.16,19,33,53,62,69,75 In addition to the electronic searches, experts in the field were contacted for further article suggestions and to attempt to identify pertinent unpublished studies. Corresponding authors of articles were contacted for additional information as needed. References from the included articles were also reviewed to ensure that all articles meeting inclusion criteria were identified. At the conclusion of the search, 14 articles met the inclusion criteria and were included in this review of the literature. A summary of the literature search process can be seen in Figure 2.
Figure 2.
PRISMA flowchart of the literature search process.
Risk of Bias Assessment
The Physiotherapy Evidence Database (PEDro) scale and a modified Downs and Black14 checklist were utilized to measure the methodological quality of the included studies. The PEDro scale is used to assess the quality of randomized controlled trials’ methods, while the modified Downs and Black14 checklist is appropriate for rating non-randomized studies. The Downs and Black14 checklist was modified to include only criteria that were relevant to evaluating potential sources of bias in the included studies. This resulted in a checklist of 11 items. Each study was independently assessed by 2 people, and any disagreements were resolved by arbitration and consensus. The results of these assessments are shown in Tables 1 and 2.
TABLE 1.
Levels of Evidence and PEDro Scores for All Included Studiesa
| Study | Level of Evidence | PEDro Scale Itemsb
|
Total Score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| Astur et al1 | 1b | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Csintalan et al11 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| Deie et al12 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Ellera Gomes15 | 4 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Feller et al17 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Fink et al18 | 4 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Goyal22 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Kang et al27 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| Matthews and Schranz34 | 1b | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Mulliez et al40 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Panagopoulos et al45 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Panni et al46 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Wagner et al71 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| Witonski et al73 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
The Physiotherapy Evidence Database (PEDro) scale is optimal for evaluating randomized controlled trials; therefore, it should be interpreted with caution in the studies included here, as they are nonrandomized. PEDro criterion 1 is not counted toward the total score according to the Physiotherapy Evidence Database guidelines.
Scale items: 1 = eligibility criteria specified; 2 = random allocation of participants; 3 = allocation concealed; 4 = similar groups at baseline; 5 = blinding of participants; 6 = blinding of intervention providers; 7 = blinding of outcome assessors; 8 = outcomes obtained from 85% of participants; 9 = use of intent-to-treat analysis if protocol violated; 10 = between-group statistical comparison; and 11 = point measures and measures of variability. “1” indicates a “yes” score, and “0” indicates a “no” score.
TABLE 2.
| Study | Modified Downs and Black14 Checklist Itemsb
|
Total Score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 6 | 7 | 10 | 11 | 12 | 16 | 18 | 27 | ||
| Astur et al1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 8 |
| Csintalan et al11 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 8 |
| Deie et al12 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Ellera Gomes15 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 7 |
| Feller et al17 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Fink et al18 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Goyal22 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 10 |
| Kang et al27 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 9 | |
| Matthews and Schranz34 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 8 |
| Mulliez et al40 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 9 |
| Panagopoulos et al45 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Panni et al46 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Wagner et al71 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 7 |
| Witonski et al73 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 8 |
Only criteria relevant to the included studies were used here; therefore, several criteria were excluded, yielding a checklist of 11 items with a maximum total of 11.
Included checklist items: 1 = clear aim; 2 = outcomes described; 3 = participants described; 6 = main findings clearly described; 7 = estimates of random variability; 10 = probability values reported; 11 = subjects asked to participate in the study represent the source population; 12 = subjects who were included in the study represent the population from which they were recruited; 16 = planned data analysis; 18 = appropriate statistics; and 27 = power calculation. “1” indicates a “yes” score, and “0” indicates a “no” score.
Level of Evidence Method
The Centre for Evidence-Based Medicine’s level of evidence was used to evaluate the quality of the current analysis. The level of evidence assesses research design quality. Levels of evidence for each study can be seen in Table 1.
Data Extraction
The population size was harvested from each study as well as means/medians and ranges for population age and follow-up time. Preoperative and postoperative Tegner and Kujala scores were extracted. The rate at which patients returned to preinjury or higher levels of sports participation was collected. Rates of redislocations and recurrent instability (if reported) were noted, as were rates of positive apprehension signs and reoperations. The following terms were defined as recurrent instability: “postoperative subluxation” and “recurrent patellar instability.” 40 All episodes of redislocations and recurrent instability were combined to calculate the total rate of recurrent instability for a particular study.
Statistical Analysis
Means were calculated for population size, age, follow-up time, and postoperative Tegner scores. Means were calculated using all available data. If a study did not report a specific statistic, it was not included in the calculation of the mean for that respective statistic. If not provided by authors, risks were calculated by using the number of occurrences of an event of interest divided by the number of patients (for return to play) or knees (for redislocations, recurrent instability, positive apprehension signs, and reoperations) in the population. All episodes of redislocations and recurrent instability (subluxations) were added to calculate the total rate of recurrent instability for a particular study. No patients were counted twice in this calculation, as only 1 study71 reported a single incidence of a redislocation, and this study did not report the incidence of subluxations. Postoperative Kujala scores, return to play, total risk of recurrent instability, risk of positive apprehension sign, and risk of reoperation were analyzed using a random-effects proportion meta-analysis (weighted for individual study size) using OpenMeta[Analyst] (Centre for Evidence-Based Medicine). Individual study means and pooled estimates of postoperative Kujala scores for individual studies were summarized in a forest plot for all studies that reported means ± SDs for this metric. Proportions of return to play, recurrent instability, positive apprehension sign, and reoperation for individual studies and pooled estimates were also summarized in forest plots for all studies that reported these data.
Summary of Included Studies
Astur et al
Astur et al1 published a single-surgeon case series (n = 58) comparing the results of MPFL reconstruction using either endobutton or anchor graft fixation at 2- and 5-year follow-up. As the purpose of this review is not to comment on the specific techniques utilized in reconstruction, results are reported on the investigators’ entire cohort. There were no instances of patellar instability at both 2 and 5 years after reconstruction. Authors reported 6 postoperative complications in their cohort, 3 of which required reoperation (5.2%). The mean Kujala score was 79.6 at 5-year follow-up. No data were provided on patients’ sports participation.
Csintalan et al
Csintalan et al11 conducted a case series (n = 49; 56 knees) of patients who underwent MPFL reconstruction with a doubled semitendinosus graft and reported their results with a follow-up of 4.3 years. There were no redislocations in the study population. Recurrent subluxations occurred at a rate of 10.7%, while the apprehension sign was positive in 12.5% of knees. Reoperation was required in 3.6% of knees: one because of painful hardware and one because of stiffness. Function was assessed via Tegner scores and a single-legged hop test for distance. Preinjury and postoperative mean Tegner scores were 6.1 and 5.6, respectively. The majority of participants were able to hop >75% of the distance with the involved limb compared with the uninvolved limb, with 19 patients >90% and 11 patients from 76% to 89%. However, only 39 of 56 operated knees underwent hop testing as bilateral surgeries were excluded, and some patients were unable or refused to perform the test.
Deie et al
Deie et al12 reported results from a case series (n = 29; 31 knees) in which patients underwent anatomic MPFL reconstruction with a cylindrical bone plug and a semitendinosus tendon graft. There were no redislocations after reconstruction and rehabilitation in the population. The mean Kujala score for the population was 94.5, and all patients in the study population returned to their preinjury level of competition in high-risk sports such as tennis and volleyball. The apprehension sign remained positive in 1 knee (3.2% of population), and this knee subsequently underwent lateral retinacular reconstruction (3.2% reoperation rate). The authors noted that this patient had severe dysplasia of the femoral condyle and osteoarthritis before surgery, and they noted that he/she might be better suited for a combined procedure rather than isolated MPFL reconstruction.
Ellera Gomes
Ellera Gomes15 published results (n = 12) comparing rigid and dynamic approaches to MPFL reconstruction using an adductor magnus tendon graft and a split half semitendinosus graft, respectively. Results from the half semitendinosus tendon graft group alone are reported in this review, as the adductor magnus tendon graft group underwent concomitant lateral retinacular release. No redislocations or subluxations occurred during the period between reconstruction and follow-up (minimum of 30 months). No data on reoperations were reported, although it was noted that no patients had any hematomas, infections, or thromboembolic events. All 8 athletes in this group returned to recreational sports after reconstruction and rehabilitation. Descriptions of the sports to which patients returned were not reported.
Feller et al
Feller et al17 published results from an observational study (n = 31) comparing isolated MPFL reconstruction to a combined procedure involving both reconstruction and an additional stabilization procedure at a minimum of 1 year after surgery. All of the isolated reconstructions were performed with either a semitendinosus or gracilis graft (if the gracilis was large enough). No patients in the isolated MPFL reconstruction group suffered a redislocation or subluxation, and there were no reoperations. The patients returned to sports after isolated surgery at a rate of 80.8%, with 65.4% returning to “strenuous” sports and 15.4% returning to “moderate” sports. Unfortunately, descriptions of these sports were not defined by the authors. A majority of the patients who resumed sports participation did so at a high frequency, with 90.5% of those who returned participating in sports at least weekly. The questionnaire regarding return to sports activities was not completed by 5 patients, although these patients’ clinical follow-up data (all ≥1 year) were collected and used to calculate rates of recurrent patellar instability.
Fink et al
Fink et al18 reported on a case series of patients (n = 17) who underwent isolated MPFL reconstruction with a quadriceps tendon graft at 12 months’ follow-up. There were no postoperative complications or redislocations, and no patients underwent reoperations. The mean postoperative Kujala score was 89.2. The mean preoperative and postoperative Tegner scores were 4.8 and 5.0, respectively. Data were not provided on sports participation.
Goyal
A case series (n = 32) published by Goyal22 reported the outcomes of MPFL reconstruction using a graft made from the superficial slip of the quadriceps tendon. No patients suffered redislocations or subluxations postoperatively, and there were no reoperations at a mean of 38 months’ follow-up. The mean postoperative Kujala score was 91.3 for the population. Postoperative activity levels were not assessed, and data on return-to-play rates were not reported.
Kang et al
Kang et al27 reported a case series (n = 45) of patients who underwent MPFL reconstruction with a horizontal Y-shaped semitendinosus graft. There were no redislocations or subluxations sustained during follow-up. In addition, no postoperative complications were observed, and no patients had positive apprehension signs after reconstruction. The mean postoperative Kujala score was 90.9. Sports participation was not considered in this study.
Matthews and Schranz
Matthews and Schranz34 published results from a case series (n = 21; 25 knees) of patients who underwent MPFL reconstruction with either a semitendinosus or gracilis autograft. No redislocations were observed in the population, but 1 patient was lost to follow-up. The reoperation rate was 28.0%, with 5 patients requiring manipulation under anesthesia to regain adequate ROM of knee flexion. The mean postoperative Kujala and Tegner scores were 87.0 and 4.4, respectively. While no data were provided on how many patients participated in sports before the injury, 3 patients were playing competitive sports at follow-up. The length of follow-up ranged from 3 to 87 months. The incidence of redislocations increased with time after surgery,23 so the lack of redislocations in this population may not be an accurate representation of global redislocation rates because of the variability in follow-up times.
Mulliez et al
Mulliez et al40 conducted a prospective cohort study (n = 86; 91 knees) and published results comparing isolated MPFL reconstruction to a combined procedure involving reconstruction and tibial tuberosity transfer. Reconstructions were performed with gracilis autografts unless the size of the gracilis was not adequate, in which case the semitendinosus was harvested as a graft source. No redislocations were noted in those patients who underwent isolated MPFL reconstruction. The mean postoperative Kujala score was 74.7, which is the lowest absolute score in the studies included in this review. Complications such as recurrent instability and reoperations were not reported or were given as total population rates, which included the group that underwent combined surgery. As these rates are not specific to isolated MPFL reconstruction, they are not included here.
Panagopoulos et al
Panagopoulos et al45 published their results from a case series (n = 25) of patients who underwent MPFL reconstruction with a semitendinosus autograft at a mean follow-up of 13 months. No patients sustained an episode of a redislocation during follow-up. The mean postoperative Tegner and Kujala scores were 7.7 and 89.0, respectively. Data on both recurrent instability and reoperations were not reported; however, 1 patient in the cohort did sustain a patellar fracture. The majority of the text was dedicated to reviewing the literature and the surgical technique utilized for MPFL reconstruction in this population. Thus, in-depth methods and discussion sections relative to the surgical outcomes reported are unavailable.
Panni et al
Panni et al46 conducted a case series (n = 45; 48 knees) of patients who underwent MPFL reconstruction with a semitendinosus autograft using a divergent 2-tunnel technique with a minimum 2-year follow-up. There were no redislocations observed in the cohort after surgery and rehabilitation. The incidence of postoperative subluxations in the population was not reported. One patient sustained a displaced patellar fracture after direct trauma at 4 months postoperatively, which was surgically corrected, indicating that the study population had a reoperation rate of 2.2%. The mean postoperative Kujala score was 86.8 for the total population; however, 4 patients with significant (Outerbridge stage 4) chondral damage may have decreased this figure, as the mean score in this subset was 45.7. After postoperative rehabilitation, 64% of patients returned to sports at their preinjury level of competition (21 patients to recreational sports, 8 to regional or national-level sports). Additionally, of the patients who returned to a reduced level of sports or changed sports, 16% did so for reasons unrelated to their MPFL reconstruction, and the remaining 20% did so because they did not feel as though reconstruction improved their function to an appropriate level.
Wagner et al
Wagner et al71 published a case series (n = 50) in which patients underwent MPFL reconstruction with a gracilis autograft with a minimum follow-up of 12 months. One redislocation occurred after surgery, for a redislocation rate of 2%. Subluxations and subjective instability were not reported. The reoperation rate within the population was 4.0%, with 2 patients requiring operative revision. The mean postoperative Kujala score for the population was 87.0, and 80% of patients returned to the same or greater level of sports activity relative to their preinjury sports activity.
Witonski et al
Witonski et al73 reported a case series (n = 10) of patients who underwent MPFL reconstruction using the medial strip of the autologous patellar tendon as a graft with a minimum 2-year follow-up. No redislocations or deterioration of knee function were observed after reconstruction. No instances of reoperation were reported. The mean postoperative Kujala score for the population was 84.4. Data regarding sports participation were not reported by the authors, and the relatively small sample size makes it difficult to draw global conclusions from this study alone.
RESULTS
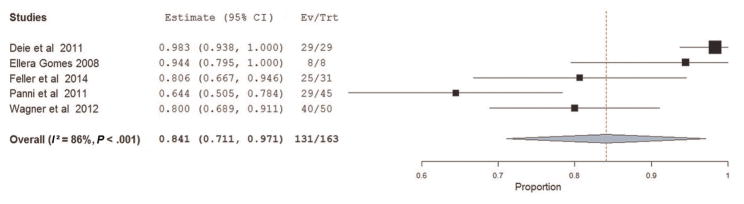
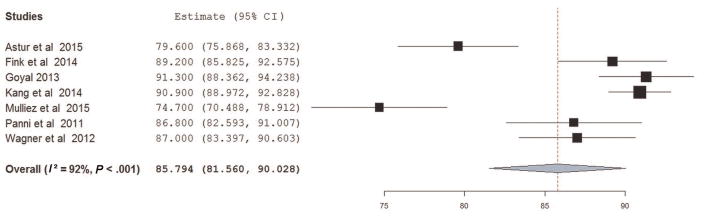
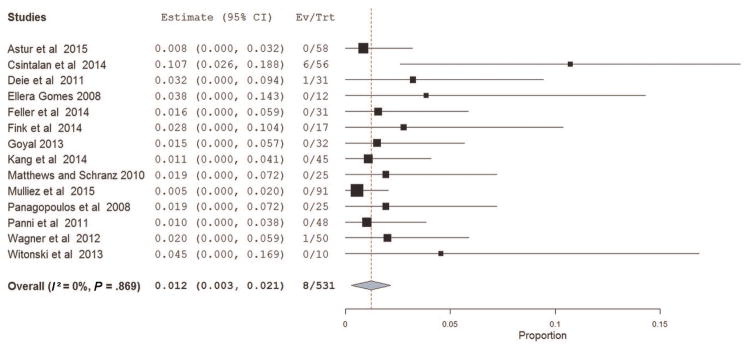
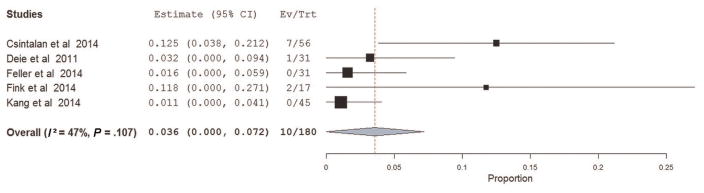
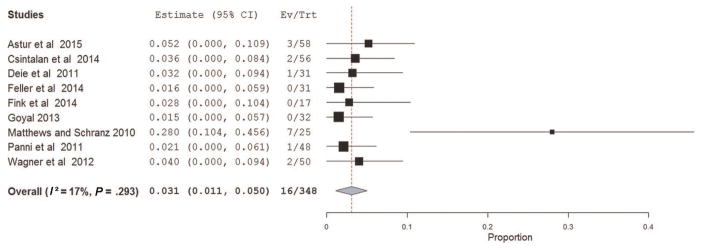
The mean PEDro score was 3.0 (range, 1–6), and for the modified Downs and Black14 checklist, the mean number of items rated was 8.1 (range, 3–10). The PEDro scores were low relative to the maximum possible total score of 10 because of the nonrandomized nature of all but 2 of the included studies.1,34 From the Downs and Black14 checklist, many studies did not report probability values, and no studies performed a power calculation. The specific criteria used to select patients for isolated MPFL reconstruction for each study are presented in Table 3. The data extracted from all studies included in the review, as well as all calculated means, are presented in Table 4. The total mean population size of all 14 studies was 36 participants, with a mean age and follow-up of 24.4 years and 36.8 months, respectively. The mean postoperative Tegner score was 5.7, calculated from 4 studies. Preinjury and preoperative Tegner scores were each reported in 2 studies. The pooled proportion of athletes who returned to sports after surgery was 84.1% (95% CI, 71.1%–97.1%) (Figure 3). The pooled estimated mean from 7 studies that reported means ± SDs for the postoperative Kujala score was 85.8 (95% CI, 81.6–90.0; I2 = 92%) (Figure 4). The pooled total risk of recurrent instability after surgery was 1.2% (95% CI, 0.3%–2.1%; I2 = 0%) (Figure 5). Also, 5 studies reported the frequency at which patients exhibited a positive apprehension sign during follow-up; the pooled risk from these studies was 3.6% (95% CI, 0%–7.2%) (Figure 6). Finally, 9 studies reported reoperation data in which the pooled reoperation risk was 3.1% (95% CI, 1.1%–5.0%) (Figure 7).
TABLE 3.
Patient Criteria for Isolated MPFL Reconstruction in Each Studya
| Study | Patient Criteria |
|---|---|
| Astur et al1 | Skeletally mature; traumatic MPFL tear diagnosed by MRI after history of patellar dislocation; failure after 6 months of nonoperative treatment; no chondral injuries ICRS grade ≥III, trochlear dysplasia, malalignment, or patella alta |
| Csintalan et al11 | No malalignment |
| Deie et al12 | >2 dislocations; no osteoarthritis Kellgren-Lawrence grade >III at patellofemoral joint or grade >II at tibiofemoral joint |
| Ellera Gomes15 | Dislocation and/or subluxation and “exhausted nonoperative treatment strategies”; no genu valgum, obesity, or severe patellofemoral crepitus |
| Feller et al17 | Recurrent subluxation; ISI<1.4; TT-TG distance<21 mm; no J-tracking |
| Fink et al18 | Skeletally mature; >2 dislocations; TT-TG distance<20 mm; no chondral injuries ICRS grade >IIIB |
| Goyal22 | Recurrent patellar instability due to predisposing bony causes; first-time dislocation regardless of predisposing bony causes with persistent instability after 1 month of nonoperative treatment |
| Kang et al27 | ≥2 dislocations or instability persisting >3 months after initial dislocation and nonoperative treatment; Q angle<20° (female) or 17° (male); trochlear angle<145°; TT-TG distance<20 mm; ISI<1.2; no patellar dysplasia Wiberg grade ≥IV; no articular cartilage erosion Outerbridge grade >2 |
| Matthews and Schranz34 | ≥2 dislocations; no degenerative patellofemoral osteoarthritis of grades III or IV; TT-TG distance<15 mm; no severe trochlear dysplasia of Dejour types B or C |
| Mulliez et al40 | Recurrent patellar dislocation or “constant feeling of patellar instability”; failure after 6 months of nonoperative treatment;<45 years old; Caton-Deschamps index<1.2; TT-TG distance<20 mm |
| Panagopoulos et al45 | Posttraumatic patellar instability |
| Panni et al46 | ≥3 dislocations confirmed by radiography or clinical diagnosis and reduction (including manual reduction by nonclinicians); failure after 6 months of nonoperative treatment; Q angle<20° (female) or 17° (male); ISI<1.2; no genu valgum ≥7° on weight bearing long-leg radiographs; trochlear angle<145°; no patellar dysplasia Wiberg grade ≥IV; no meniscal tears requiring repair; no severe trochlear dysplasia of Dejour types B, C, or D; no J-tracking; TT-TG distance<20 mm |
| Wagner et al71 | Chronic patellofemoral instability |
| Witonski et al73 | History of dislocation “as a starting point of recurrent lateral patellar instability”; no abnormal pelvic geometry or Q angle; no femoral anteversion; no trochlear dysplasia; no patella alta or baja; no external tibial torsion or hindfoot position |
Previous surgery and multiligamentous injuries/laxity were exclusion criteria for this review, and thus, these criteria are not included in the table. ICRS, International Cartilage Repair Society; ISI, Insall-Salvati index; MPFL, medial patellofemoral ligament; MRI, magnetic resonance imaging; Q angle, quadriceps angle; TT-TG, tibial tuberosity–trochlear groove.
TABLE 4.
Data Extracted From Included Studies and Calculated Meansa
| Study | Year | Graft Type |
n | Mean Age, y |
Mean Follow-up, mo |
Mean Tegner Score
|
Mean Postoperative Kujala Score |
Prevalence Rate, %
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | RTP | Redislocation | Recurrent Instability/ Subluxation |
Total Recurrent Instability |
Positive Apprehension Sign |
Reoperation | |||||||
| Astur et al1 | 2015 | GR | 58 | 29.8 | 60 | N/A | N/A | 79.6 | N/A | 0 | 0 | 0 | N/A | 5.2 |
| Csintalan et al11 | 2014 | ST | 49 | 24 | 51.6 | 6.1b | 5.6 | N/A | N/A | 0 | 10.7 | 11.1 | 12.5 | 3.6 |
| Deie et al12 | 2011 | B-ST | 29 | 22.2 | 38.4 | N/A | N/A | 94.5 | 100 | 0 | 3.2 | 3.2 | 3.2 | 3.2 |
| Ellera Gomes15 | 1992 | AM or ST | 12 | 19.3 | 53 | N/A | N/A | N/A | 100c | 0 | 0 | 0 | N/A | N/A |
| Feller et al17 | 2014 | GR or ST | 31 | 23.9 | 37.2 | N/A | N/A | N/A | 80.8 | 0 | 0 | 0 | 0 | 0 |
| Fink et al18 | 2014 | QT | 17 | 21.5 | 12 | 4.8d | 5.0 | 89.2 | N/A | 0 | N/A | 0 | 11.8 | 0 |
| Goyal22 | 2013 | QT | 32 | 25 | 38 | N/A | N/A | 91.3 | N/A | 0 | 0 | 0 | N/A | 0 |
| Kang et al27 | 2014 | ST | 45 | 26.6 | 33.7 | N/A | N/A | 90.9 | N/A | 0 | 0 | 0 | 0 | N/A |
| Matthews and Schranz34 | 2010 | GR or ST | 21 | 24 | 31 | 3.0d | 4.4 | 87.0 | N/A | 0 | N/A | 0 | N/A | 28.0 |
| Mulliez et al40 | 2015 | GR or ST | 86 | 22.8e | 34.5e | N/A | N/A | 74.7 | N/A | 0 | N/A | 0 | N/A | N/A |
| Panagopoulos et al45 | 2008 | ST | 25 | 26.9 | 13 | 4.2b | 7.7 | 89.0 | N/A | 0 | N/A | 0 | N/A | N/A |
| Panni et al46 | 2011 | ST | 45 | 28 | 33 | N/A | N/A | 86.8 | 64 | 0 | N/A | 0 | N/A | 2.2 |
| Wagner et al71 | 2013 | GR | 50 | 19 | N/A | N/A | N/A | 87.0 | 80 | 2 | N/A | 2.0 | N/A | 4.0 |
| Witonski et al73 | 2013 | PT | 10 | 27.2 | 43 | N/A | N/A | 84.4 | N/A | 0 | N/A | 0 | N/A | N/A |
| Means for all included studies (n = 14) | 36 | 24.4 | 36.8 | 5.7 | ||||||||||
Means were calculated from all available data. AM, adductor magnus; B-ST, bone-semitendinosus; GR, gracilis; N/A, not available; post, postoperative; pre, preoperative; PT, patellar tendon; QT, quadriceps tendon; RTP, return to play; ST, semitendinosus.
Preinjury Tegner score.
Data obtained via personal correspondence with authors.
Preoperative Tegner score.
Population demographic statistics were reported for the total population, which included a group that underwent tibial tubercle transposition as well as medial patellofemoral ligament reconstruction.
Figure 3.
Individual study proportions and pooled estimated rates of return to play for 5 studies.
Figure 4.
Individual study means and pooled estimated Kujala scores for 7 studies that reported mean ± SD Kujala scores.
Figure 5.
Individual study proportions and pooled estimated rates of recurrent instability for all studies.
Figure 6.
Individual study proportions and pooled estimated rates of a positive apprehension sign for 5 studies.
Figure 7.
Individual study proportions and pooled estimated rates of reoperation for 9 studies.
DISCUSSION
A patellar dislocation is a common injury sustained by young, active patients, with nearly 70% of dislocations occurring during sports activities.20,43,44,50,55,56,63 The risk of redislocations after treatment and rehabilitation has been reported from 0% to 71% in young athletes.43 Recently, surgical reconstruction of the MPFL has gained popularity in the treatment of patellar dislocations, particularly in the setting of recurrent dislocations and/or chronic instability. 62 While previous literature has addressed the outcomes after MPFL reconstruction, methodologies of various studies have differed greatly, as many studies have included within their populations patients who underwent additional surgical procedures.69 This systematic review is intended to determine patient-reported outcomes, return-to-play rates, and the incidence of recurrent instability after isolated MPFL reconstruction in the treatment of recurrent patellar dislocations. Overall, 84.1% of athletes returned to their preinjury level of sports participation after surgery (Figure 3), and the pooled risk of recurrent instability after surgery was 1.2% (Figure 5).
The included studies evaluated a wide variety of patient populations, as shown by the criteria in Table 3. Common criteria include the failure of nonoperative treatment, an absence of malalignment, and a lack of severe cartilage damage and/or trochlear dysplasia. Specific anatomic features such as quadriceps angle (Q angle), tibial tuberosity–trochlear groove (TT-TG) distance, trochlear angle, and the Insall-Salvati index were also utilized in multiple studies. Wagner et al71 utilized lenient criteria for the selection for surgery to study the relationships between some of the aforementioned features and outcomes after MPFL reconstruction. The investigators reported that patients with grade III trochlear dysplasia had significantly worse subjective outcomes as measured by the Kujala score. However, Steiner et al64 reported excellent results in their cohort of patients, 88% of whom had trochlear dysplasia. The authors noted no correlation between outcomes and the degree of trochlear dysplasia present but did not report how many of their patients had high-grade dysplasia. Taken together, these data suggest that while low-grade dysplasia does not adversely affect the results of isolated MPFL reconstruction, further research is required to clarify the effect of high-grade dysplasia (grade III according to the H. Dejour classification or type D according to the D. Dejour classification) on outcomes. Wagner et al71 also reported that a TT-TG distance >20 mm was associated with a trend toward worse scores. These findings support the use of these features in the process of selecting a procedure for the treatment of recurrent patellar instability, but future investigations may be necessary to establish a set of criteria that can be adapted on a wide scale.
On average, the reviewed investigations evaluated a small number of patients with a mean population size of 36 patients, and the mean age of patients in all studies was 24.4 years. The mean follow-up time for all studies was 36.8 months. As the incidence of postoperative episodes of instability increases linearly with time from surgery,1,23 our results should be interpreted with the understanding that certain studies may have underestimated recurrent instability as a consequence of short follow-up periods. 18,34,40,45,46,71 The Tegner activity scale was designed to assess work and sports activity levels and has been validated in cohorts with patellar instability.10,59,66 Only 4 of the 14 included studies utilized the Tegner scale.11,18,34,45 Two studies11,45 had patients fill out the scale retrospectively relative to their preinjury condition and demonstrated higher preinjury scores (6.1 and 4.2) than the other 2 studies,18,34 which collected data prospectively on preoperative conditions (4.8 and 3.0). The mean postoperative Tegner score was 5.7, which is similar to the scores of 5.4 and 5.8 found in recent reviews that examined patients’ ability to return to sports.19,33 Csintalan et al11 were the only authors to report a decreased mean postoperative Tegner score (5.6) relative to the mean preinjury score (6.1).
Data on the Tegner scale are supported by the pooled return-to-play rate of 84.1% (Figure 3). This rate was calculated using data from 5 studies that reported the percentage of patients who returned to sports at their preinjury level after surgery.12,15,17,46,71 Rates of 90% and 77.3% have been previously reported in reviews, although neither of these rates has been specific to isolated MPFL reconstruction.19,33 Panni et al46 reported that 64% returned to sports at the same level. They went on to specify that the remaining 36% reduced their sports level either because of reasons related to surgery (20%) or for reasons unrelated to surgery (16%).46 Although we chose to use the 64% rate in the meta-analysis, if the 7 patients in the Panni et al46 population who reduced their sports level for reasons unrelated to surgery were excluded, the new return-to-play rate for this study would be 76.3%, and the pooled rate becomes 86.6% (95% CI, 76.0%–97.1%; I2 = 79%). There is limited evidence in the literature describing the effect of dynamic factors such as strength, balance, power, and neuromuscular performance on clinical outcomes such as returning to sports after patellar dislocations.26,30,48,49 Studies to this point have focused on the examination of isokinetic knee extension strength, with most finding deficits in both the short term and long term. Even when these deficits are not present, many patients continue to have difficulty with functional activities such as squatting, jumping, cutting, jogging, and running.2 The role of neuromuscular performance should be further investigated as its association with patellar dislocations is currently unclear, and it may have implications for the prevention of knee injuries, as has been shown by previous investigators.24 Additionally, there are no studies that the authors are aware of that investigate hip abduction and hip external rotation strength in patients with patellar dislocations. Previous investigators have shown hip strength deficits in athletes with other patellofemoral dysfunctions such as patellofemoral pain syndrome,3,41,61,70,72 and greater hip abduction strength may protect against lower extremity injuries.29 Assessing the association between hip strength and patellar dislocations may be warranted in determining the readiness to return to sports in young athletes.
The Kujala anterior knee pain scale, a knee-specific scale focused on the patellofemoral joint, was the most frequently reported patient-reported outcome measure among the included studies. The scale assesses items such as limping, mobility aid dependency, walking, stair climbing, squatting, running, jumping, prolonged sitting with the knee flexed, pain, swelling, instability, thigh atrophy, and flexion deficiency. The scale is scored from 0 to 100, with low scores representing greater disability.28 The pooled mean postoperative Kujala score was 85.8. Four studies12,34,45,73 did not report SDs, and therefore, these studies were not included in the pooled estimate. Mean scores from 12 individual study populations were in the “good” category (85–94 points), as proposed by Sillanpaa et al.57 Only 2 included studies1,40 reported scores in the “fair” category of 65 to 84. Overall, these data indicate that isolated MPFL reconstruction yields good subjective outcomes, but continued research is needed to effectively review the results from other subjective outcome measures in this patient population.
Redislocations and postoperative instability are potential complications after patellar stabilization. In the included studies, the pooled estimate of all postoperative recurrent instability was 1.2% (Figure 5). This rate is significantly lower than any of those previously reported in reviews including nonisolated MPFL reconstruction procedures such as tibial tubercle osteotomy and lateral retinacular release. In a recent systematic review, investigators reported redislocation and recurrent instability rates of 24.0% and 32.7%, respectively, in patients who were treated operatively with procedures including MPFL reconstruction, MPFL repair, lateral retinacular release, and others for primary dislocations. 16 Additionally, Matic et al33 conducted a systematic review of return to activity after MPFL repair or reconstruction and reported a 6.6% rate of recurrent instability after reconstruction. An additional review reported a 1% redislocation rate; however, this included studies performing concomitant procedures along with MPFL reconstruction and did not account for other postoperative instances of instability.69 Lateral retinacular release is often performed concomitantly; however, lateral release procedures may increase postoperative instability, particularly the risk of medial patellar subluxations. 9,13,36 Previous investigators have reported rates of medial patellar subluxations from 57% to 94% after lateral retinacular release.54,60 Inappropriate surgical indications for lateral release may underlie these poor outcomes.60 The rate of recurrent instability calculated in the present study does not limit instability to redislocations alone but also includes subluxation and other instability data reported in half of the included studies. In addition, postoperative apprehension (3.6%) (Figure 6) and reoperation (3.1%) (Figure 7) rates were low, with the latter indicating a lack of the need for revision procedures during follow-up. An important technical consideration is the location of femoral tunnel placement. Schottle et al51 described an anatomic and radiographic landmark for this location. While nonanatomically placed femoral tunnels do not necessarily correlate with poor outcomes, investigators have described negative outcomes after both proximally and/or anteriorly positioned grafts.7,35,52 Proper anatomic tunnel placement may reduce strain on the graft and further minimize the potential for postoperative complications. A patellar fracture is another described complication of MPFL reconstruction. A total of 2 patellar fractures occurred in the aggregated cohort of 510 knees (0.4%). This incidence is similar to previously reported incidences of fractures in reviews with similar population sizes (0.6% and 0.4%).19,53 Both fractures in this cohort occurred when transpatellar tunnels were utilized for graft fixation. Previous investigators have reported that direct suture or anchor-based graft fixation or avoiding bone tunnels past the midline of the patella may reduce the risk of this rare, but serious, outcome.47,53 The low rates of morbidity and complications indicate that isolated MPFL reconstruction is effective at re-establishing and maintaining patellofemoral stability after recurrent dislocations. Isolated MPFL reconstruction has also been effective in the acute setting as reported by Bitar et al,5 but further research is needed to confirm this procedure’s efficacy in this setting.
While we followed systematic guidelines to complete this review, we do recognize that our efforts have limitations. One included study12 defined a positive apprehension sign as patellar instability. As the single case of a positive apprehension sign reported in this study required reoperation during follow-up, we chose to be consistent with the investigators’ definition and to consider the case as an instance of recurrent instability. Another potential limitation is that some of the reviewed outcome measures were not reported in all of the included studies. Efforts were made to collect missing information when applicable to address this issue. The authors made attempts to contact corresponding authors for the included studies via email to fill the dataset presented in Table 4. The variation among inclusion criteria used by individual studies also represents a challenge in data aggregation and meta-analysis procedures. As no 2 studies reported identical criteria, it was not possible to group studies for analysis on the basis of age or other factors such as trochlear dysplasia or TT-TG distance. Instead, these results exhibit the overall efficacy of isolated MPFL reconstruction in a variety of patient populations, which might suggest increased generalizability of the current report.
CONCLUSION
This systematic review and meta-analysis demonstrates that both subjective and clinical outcomes are excellent after isolated MPFL reconstruction, as evidenced by the pooled Kujala score, rate of return to play, and rate of postoperative recurrent instability. A wide range of criteria has been used to select patients for this procedure, with common features including prior failure of nonoperative treatment and specific anatomic features such as a normal Q angle, lack of severe trochlear dysplasia, TT-TG distance <20 mm, and normal patellar height. Given the efficacy of isolated MPFL reconstruction, future investigations should aim to establish more uniform criteria for selecting patients to undergo this procedure. Studies should also incorporate long-term clinical outcomes that include performance-based measures as well as patient-reported measures to further characterize the neuromuscular pathophysiology of patellar instability and potential negative outcomes such as patellofemoral degeneration.
Acknowledgments
The authors acknowledge George E. Kuntz IV for his help in assessing the methodological quality of the included studies.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding support was received from the National Institutes of Health/NIAMS (grant 1R21AR065068-01A1).
References
- 1.Astur DC, Gouveia GB, Borges JH, et al. Medial patellofemoral ligament reconstruction: a longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J. 2015;9:198–203. doi: 10.2174/1874325001509010198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 3.de Baldon RM, Nakagawa TH, Muniz TB, Amorim CF, Maciel CD, Serrao FV. Eccentric hip muscle function in females with and without patellofemoral pain syndrome. J Athl Train. 2009;5(44):490–496. doi: 10.4085/1062-6050-44.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beasley LS, Vidal AF. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16(1):29–36. doi: 10.1097/00008480-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Bitar AC, Demange MK, D’Elia CO, Camanho GL. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114–122. doi: 10.1177/0363546511423742. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Pearsall AW, Garrett WE, Jr, Feagin JA., Jr Patellofemoral instability: evaluation and management. J Am Acad Orthop Surg. 1997;5(1):47–57. doi: 10.5435/00124635-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27(8):1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Camanho GL, de Viegas AC, Bitar AC, Demange MK, Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–625. doi: 10.1016/j.arthro.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Christoforakis J, Bull AM, Strachan RK, Shymkiw R, Senavongse W, Amis AA. Effects of lateral retinacular release on the lateral stability of the patella. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):273–277. doi: 10.1007/s00167-005-0699-5. [DOI] [PubMed] [Google Scholar]
- 10.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139–146. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 12.Deie M, Ochi M, Adachi N, Shibuya H, Nakamae A. Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med. 2011;39(1):140–145. doi: 10.1177/0363546510377436. [DOI] [PubMed] [Google Scholar]
- 13.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 14.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellera Gomes JL. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy. 1992;8(3):335–340. doi: 10.1016/0749-8063(92)90064-i. [DOI] [PubMed] [Google Scholar]
- 16.Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(6):1207–1215. doi: 10.1016/j.arthro.2014.11.040. [DOI] [PubMed] [Google Scholar]
- 17.Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470–2476. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 18.Fink C, Veselko M, Herbort M, Hoser C. MPFL reconstruction using a quadriceps tendon graft, part 2: operative technique and short term clinical results. Knee. 2014;21(6):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384–1394. doi: 10.1016/j.arthro.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 21.Gomes JE. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24(4):430–435. doi: 10.1016/j.arthro.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Goyal D. Medial patellofemoral ligament reconstruction: the superficial quad technique. Am J Sports Med. 2013;41(5):1022–1029. doi: 10.1177/0363546513477828. [DOI] [PubMed] [Google Scholar]
- 23.Harilainen A, Sandelin J. Prospective long-term results of operative treatment in primary dislocation of the patella. Knee Surg Sports Traumatol Arthrosc. 1993;1(2):100–103. doi: 10.1007/BF01565461. [DOI] [PubMed] [Google Scholar]
- 24.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 25.Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34(3):385–396. doi: 10.1016/s0030-5898(03)00033-6. [DOI] [PubMed] [Google Scholar]
- 26.Jerosch J, Prymka M. Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears, taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg. 1996;115(3–4):162–166. doi: 10.1007/BF00434546. [DOI] [PubMed] [Google Scholar]
- 27.Kang HJ, Cao JH, Pan S, Wang XJ, Yu da H, Zheng ZM. The horizontal Y-shaped graft with respective graft tension angles in anatomical two-bundle medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2445–2451. doi: 10.1007/s00167-014-3005-6. [DOI] [PubMed] [Google Scholar]
- 28.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 29.Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 30.Maenpaa H, Latvala K, Lehto MU. Isokinetic thigh muscle performance after long-term recovery from patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):109–112. doi: 10.1007/s001670050196. [DOI] [PubMed] [Google Scholar]
- 31.Maenpaa H, Lehto MU. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. doi: 10.1097/00003086-199706000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Mariani PP, Liguori L, Cerullo G, Iannella G, Floris L. Arthroscopic patellar reinsertion of the MPFL in acute patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):628–633. doi: 10.1007/s00167-010-1315-x. [DOI] [PubMed] [Google Scholar]
- 33.Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30(8):1018–1025. doi: 10.1016/j.arthro.2014.02.044. [DOI] [PubMed] [Google Scholar]
- 34.Matthews JJ, Schranz P. Reconstruction of the medial patellofemoral ligament using a longitudinal patellar tunnel technique. Int Orthop. 2010;34(8):1321–1325. doi: 10.1007/s00264-009-0918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarthy M, Ridley TJ, Bollier M, Wolf B, Albright J, Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. [PMC free article] [PubMed] [Google Scholar]
- 36.McCarthy MA, Bollier MJ. Medial patella subluxation: diagnosis and treatment. Iowa Orthop J. 2015;35:26–33. [PMC free article] [PubMed] [Google Scholar]
- 37.Merrick J, Morad M, Halperin I, Kandel I. Physical fitness and adolescence. Int J Adolesc Med Health. 2005;17(1):89–91. doi: 10.1515/ijamh.2005.17.1.89. [DOI] [PubMed] [Google Scholar]
- 38.Miller JR, Adamson GJ, Pink MM, Fraipont MJ, Durand P., Jr Arthroscopically assisted medial reefing without routine lateral release for patellar instability. Am J Sports Med. 2007;35(4):622–629. doi: 10.1177/0363546506296041. [DOI] [PubMed] [Google Scholar]
- 39.Mitchell J, Magnussen RA, Collins CL, et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43(7):1676–1682. doi: 10.1177/0363546515577786. [DOI] [PubMed] [Google Scholar]
- 40.Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J. Clinical outcome in MPFL reconstruction with and without tuberositas transposition [published online June 2, 2015] Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-015-3654-0. [DOI] [PubMed] [Google Scholar]
- 41.Nakagawa TH, Muniz TB, de Baldon RM, Dias Maciel C, de Menezes Reiff RB, Serrao FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22(12):1051–1060. doi: 10.1177/0269215508095357. [DOI] [PubMed] [Google Scholar]
- 42.Nam EK, Karzel RP. Mini-open medial reefing and arthroscopic lateral release for the treatment of recurrent patellar dislocation: a medium-term follow-up. Am J Sports Med. 2005;33(2):220–230. doi: 10.1177/0363546504267803. [DOI] [PubMed] [Google Scholar]
- 43.Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37(9):1814–1820. doi: 10.1177/0363546509333480. [DOI] [PubMed] [Google Scholar]
- 44.Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. doi: 10.2106/JBJS.G.00072. [DOI] [PubMed] [Google Scholar]
- 45.Panagopoulos A, van Niekerk L, Triantafillopoulos IK. MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med. 2008;29(5):359–365. doi: 10.1055/s-2007-965360. [DOI] [PubMed] [Google Scholar]
- 46.Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647–2655. doi: 10.1177/0363546511420079. [DOI] [PubMed] [Google Scholar]
- 47.Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 48.Rauschning W, Nordesjo LO, Nordgren B. Isokinetic knee extension strength and pain before and after correction of recurrent patellar dislocation. Arch Orthop Trauma Surg. 1983;102(2):102–106. doi: 10.1007/BF02498724. [DOI] [PubMed] [Google Scholar]
- 49.Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735–1742. doi: 10.1177/0363546509333482. [DOI] [PubMed] [Google Scholar]
- 50.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 51.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 52.Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 53.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shannon BD, Keene JS. Results of arthroscopic medial retinacular release for treatment of medial subluxation of the patella. Am J Sports Med. 2007;35(7):1180–1187. doi: 10.1177/0363546507299445. [DOI] [PubMed] [Google Scholar]
- 55.Shea K, Nilsson K. Patellar dislocation in skeletally immature athletes. Oper Tech Sports Med. 2006;14(3):188–196. [Google Scholar]
- 56.Sillanpaa P, Mattila VM, Iivonen T, Visuri T, Pihlajamaki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. doi: 10.1249/MSS.0b013e318160740f. [DOI] [PubMed] [Google Scholar]
- 57.Sillanpaa PJ, Maenpaa HM, Mattila VM, Visuri T, Pihlajamaki H. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med. 2008;36(12):2301–2309. doi: 10.1177/0363546508322894. [DOI] [PubMed] [Google Scholar]
- 58.Sillanpaa PJ, Mattila VM, Visuri T, Maenpaa H, Pihlajamaki H. Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):230–235. doi: 10.1007/s00167-010-1285-z. [DOI] [PubMed] [Google Scholar]
- 59.Smith TO, Davies L, O’Driscoll ML, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15(4):255–262. doi: 10.1016/j.knee.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 60.Song GY, Hong L, Zhang H, Zhang J, Li Y, Feng H. Iatrogenic medial patellar instability following lateral retinacular release of the knee joint [published online January 25, 2015] Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-015-3522-y. [DOI] [PubMed] [Google Scholar]
- 61.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- 62.Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93–101. doi: 10.1097/BLO.0b013e31802eb40a. [DOI] [PubMed] [Google Scholar]
- 63.Stein B, Ahmad C. The management of patellar instability in the skeletally immature patient. Oper Tech Orthop. 2007;17(4):250–256. [Google Scholar]
- 64.Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 65.Stupay KL, Swart E, Shubin Stein BE. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review. Arthroscopy. 2015;31(7):1372–1380. doi: 10.1016/j.arthro.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 66.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 67.Thomee P, Thomee R, Karlsson J. Patellofemoral pain syndrome: pain, coping strategies and degree of well-being. Scand J Med Sci Sports. 2002;12(5):276–281. doi: 10.1034/j.1600-0838.2002.10226.x. [DOI] [PubMed] [Google Scholar]
- 68.Tjoumakaris FP, Forsythe B, Bradley JP. Patellofemoral instability in athletes: treatment via modified Fulkerson osteotomy and lateral release. Am J Sports Med. 2010;38(5):992–999. doi: 10.1177/0363546509357682. [DOI] [PubMed] [Google Scholar]
- 69.Tompkins MA, Arendt EA. Patellar instability factors in isolated medial patellofemoral ligament reconstructions: what does the literature tell us? A systematic review. Am J Sports Med. 2015;43(9):2318–2327. doi: 10.1177/0363546515571544. [DOI] [PubMed] [Google Scholar]
- 70.Tyler TF, Nicholas SJ, Mullaney MJ, McHugh MP. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34(4):630–636. doi: 10.1177/0363546505281808. [DOI] [PubMed] [Google Scholar]
- 71.Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):318–324. doi: 10.1007/s00167-012-2015-5. [DOI] [PubMed] [Google Scholar]
- 72.Willson JD, Davis IS. Lower extremity strength and mechanics during jumping in women with patellofemoral pain. J Sport Rehabil. 2009;18(1):76–90. doi: 10.1123/jsr.18.1.76. [DOI] [PubMed] [Google Scholar]
- 73.Witonski D, Keska R, Synder M, Sibinski M. An isolated medial patellofemoral ligament reconstruction with patellar tendon autograft. Biomed Res Int. 2013;2013:637678. doi: 10.1155/2013/637678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Woo R, Busch MT. Management of patellar instability in children. Oper Tech Sports Med. 1998;6(4):247–258. [Google Scholar]
- 75.Yao LW, Zhang C, Liu Y, et al. Comparison operative and conservative management for primary patellar dislocation: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol. 2015;25(4):783–788. doi: 10.1007/s00590-014-1523-z. [DOI] [PubMed] [Google Scholar]