Abstract
Objective
The aim of this study was to determine key components in neuromuscular training that optimise ACL injury reduction in female athletes using meta-regression analyses.
Design
Systematic review and meta-regression.
Data sources
The literature search was performed in PubMed and EBSCO.
Eligibility criteria
Inclusion criteria for the current analysis were: (1) documented the number of ACL injuries, (2) employed a neuromuscular training intervention that aimed to reduce ACL injuries, (3) had a comparison group, (4) used a prospective control study design and (5) recruited female athletes as participants. Two independent reviewers extracted studies which met the inclusion criteria. Methodological quality of included study and strength of recommendation were evaluated. Number of ACL injuries and participants in control and intervention groups, age of participants, dosage of neuromuscular training, exercise variations within neuromuscular training and status of verbal feedback were extracted.
Results
The meta-regression analyses identified age of participants, dosage of neuromuscular training, exercise variations within neuromuscular training and utilisation of verbal feedback as significant predictors of ACL injury reduction (p=0.01 in fixed-effects model, p=0.03 in random-effects model). Inclusion of 1 of the 4 components in neuromuscular training could reduce ACL injury risk by 17.2–17.7% in female athletes. No significant heterogeneity and publication bias effects were detected. Strength of recommendation was rated as A (recommendation based on consistent and good-quality patient-oriented study evidence).
Conclusions
Age of participants, dosage of neuromuscular training, exercise variations within neuromuscular training and utilisation of verbal feedback are predictors that influence the optimisation of prophylactic effects of neuromuscular training and the resultant ACL injury reduction in female athletes.
Introduction
ACL injury is a major concern in the field of sports medicine. Individuals who have sustained ACL disruption experience various functional impairments, including inability to decelerate, cut, pivot and perform other dynamic movements necessary for sport. Also, comorbidity such as meniscus tear,1–3 avulsion fractures4 and medial collateral tear1,5 is often present with ACL injury. Owing to these functional impairments and clinical significance, patients with an ACL-deficient knee often choose to have reconstruction surgery, and the number of reported ACL reconstruction surgery cases is as high as 350 000 annually in the USA alone.6 Although ACL reconstruction surgery has a high success rate, younger and more physically active individuals have a relatively high rate of reinjury,7 which ranges from 24%8 to 29%9 along with strength deficits,10 reduced postural control11,12 and altered kinematics.13,14 Furthermore, a systematic review that synthesised a total of 31 studies indicated that 48% of knee osteoarthritis prevalence rates more than 10 years following ACL reconstruction surgery.15 The negative impact of knee osteoarthritis development on quality of life has also been reported.16
Owing to the unfavourable health consequences following ACL injury, preventive interventions have been proposed.17 One of the proposed methods to reduce ACL injury is to implement neuromuscular training (NMT) programme. In order to examine the efficacy of NMT programme, a number of different NMT programmes have been implemented.18–31 Systematic review and meta-analysis studies have examined the effectiveness of those NMT programmes by comparing the number of ACL injuries between the intervention and control groups and reported consistent evidence: NMT is an effective intervention to reduce ACL injuries in female athletes.32–34
The reported NMT programmes are diverse, and the question remains as to which specific components of NMT contribute to the fullest prophylactic effects of NMT and are essential for ACL injury reduction.33,35 To identify essential elements needed to maximise prophylactic effects of the preventive NMT, a series of subgroup analyses were performed based on different age groups, dosage categorisations, exercise genres and intervention compliance/adherence.32,36–38 Results of those analyses indicate that the prophylactic effectiveness of NMT is influenced by the age of participants, dosage of NMT, type and number of exercises and level of compliance/adherence.32,36–38 In addition to those studies, recent literature disseminates importance of verbal feedback on biomechanical alteration in dynamic movements.39–41 In order to evaluate these key components accurately, the current study employed a meta-regression analysis. The meta-regression can analyse a global effect of these key components on ACL injury rate using a logistic regression model and accurately quantify ACL injury risk. This analytical approach enables to evaluate which component of NMT is critical to enhance prophylactic effectiveness of NMT along with risk reduction of ACL injury, which is a limitation of meta-analysis.33 Therefore, analysis of combinatory and synergistic effects that can measure contribution of specific key NMT components on ACL injury risk has not been documented in past studies. Performance of a meta-regression analysis with these key components may enhance the precision of NMT intervention design to optimise ACL injury risk reduction. Furthermore, results of the current study may give practical knowledge to clinicians who aim to take preventive initiatives for ACL injury reduction in physically active population. Thus, the primary purpose of the present study was to investigate synergistic effects of combining key components in NMT that optimise ACL injury reduction in female athletes through meta-regression analysis. It was hypothesised that key components included in this analysis—age of participants, dosage of NMT, exercise variations within NMT and utilisation of verbal feedback—are predictors of ACL injury reduction in female athletes. The secondary purpose was to further examine age effects of NMT on ACL injury reduction in female athletes.
Methods
Literature search and criteria
A literature search was performed using PubMed and EBSCO host (CINAHL, MEDLINE and SPORTDiscus), which is displayed in table 1. The search was performed on 3 September 2015. The keyword search was performed by application of a combination of the following words: ‘knee,’ ‘anterior cruciate ligament,’ ‘ACL,’ ‘prospective,’ ‘neuromuscular,’ ‘training,’ ‘female,’ and ‘prevention.’ Language was limited to English, and all participants were human. The following inclusion criteria were applied: (1) the number of ACL injury incidence was reported, (2) an NMT intervention aimed to reduce ACL incidence was applied, (3) a comparison group was used, (4) a prospective controlled trial study design was employed and (5) females were included as participants. Primary author performed the literature search. Abstracts, posters and unpublished data were excluded. When eligibility of certain studies was questionable, primary author and secondary author discussed and determined the status based on the five inclusion criteria. During the literature search, a cross-referencing was also performed when studies that met inclusion criteria cited other studies.
Table 1. Literature search strategies and results using PubMed and EBSCO.
| Step | Strategy | PubMed | EBSCO |
|---|---|---|---|
| #17 | Search (#11) AND (#16) | 432 | 93 |
| #16 | Search (#12) OR (#13) OR (#14) OR (#15) | 25 690 | 46 368 |
| #15 | Search ‘preventing’ [TIAB] | 5480 | 1383 |
| #14 | Search ‘preventive’ [TIAB] | 2475 | 2409 |
| #13 | Search ‘prevent’ [TIAB] | 8912 | 2456 |
| #12 | Search ‘prevention’ [TIAB] | 14 218 | 16 928 |
| #11 | Search(#5) AND (#10) | 4563 | 3923 |
| #10 | Search (#6) OR (#7) OR (#8) OR (#9) | 75 157 | 78 807 |
| #9 | Search ‘female’ [TIAB] | 14 101 | 27 891 |
| #8 | Search ‘training’ [TIAB] | 12 777 | 29 002 |
| #7 | Search ‘neuromuscular’ [TIAB] | 1572 | 2875 |
| #6 | Search ‘prospective’ [TIAB] | 50 704 | 22 190 |
| #5 | Search (#1) OR (#2) OR (#3) OR (#4) | 13 278 | 61 295 |
| #4 | Search ‘ACL’ [TIAB] | 503 | 1256 |
| #3 | Search ‘anterior cruciate ligament’ [TIAB] | 620 | 4430 |
| #2 | Search ‘knee’ [TIAB] | 5679 | 18 631 |
| #1 | Search ‘injury’ [TIAB] | 7890 | 39 534 |
Language was limited in English. Species were limited in humans. Sex was limited in female. The search period was set from 1 January 1995 to 1 September 2015.
MEDLINE was used for a journal category selection for the PubMEd. CINAHL, MEDLINE and SPORTDiscus were included in the EBSCO search.
TIAB, title and abstract.
Risk of bias
To examine risk of bias, the Physiotherapy Evidence Database (PEDro) scale was used to analyse methodological quality of the included studies. The PEDro scale consists of 11 binary (yes/no) questions and is a widely accepted measurement tool for rating the methodological quality of randomised clinical intervention studies. The PEDro scale of each reviewed study was evaluated and reported in table 2. Primary and secondary authors independently examined the PEDro scale. Discrepancies between the authors were settled by arbitration and consensus.
Table 2. PEDro scores of the reviewed studies.
| Reviewed studies | Total scores | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hewett et al31* | 3 | – | X | X | X | |||||||
| Soderman et al18* | 4 | – | X | X | X | X | ||||||
| Heidt et al19 | 5 | – | X | X | X | X | X | |||||
| Myklebust et al20* | 5 | – | X | X | X | X | X | |||||
| Mandelbaum et al21* | 3 | – | X | X | X | |||||||
| Olsen et al22 | 7 | – | X | X | X | X | X | X | X | |||
| Petersen et al30* | 2 | – | X | X | ||||||||
| Pfeiffer et al23* | 2 | – | X | X | ||||||||
| Steffen et al24 | 7 | – | X | X | X | X | X | X | X | |||
| Gilchrist et al25 | 4 | – | X | X | X | X | ||||||
| Pasanen et al26 | 8 | – | X | X | X | X | X | X | X | X | ||
| Kiani et al27* | 4 | – | X | X | X | X | ||||||
| LaBella et al28 | 6 | – | X | X | X | X | X | X | ||||
| Walden et al29 | 7 | – | X | X | X | X | X | X | X |
X: ‘yes’ score. Blank: ‘no’ score. PEDro scale is optimised for the evaluation of randomised control trials; thus, the PEDro assessment score for the non-randomised control should be interpreted with caution. Studies with * are not randomised trial or low-quality randomised trial. 1 Eligibility criteria specified, 2 random allocation of participants, 3 allocation concealed, 4 similar groups at baseline, 5 blinding of participants, 6 blinding of intervention providers, 7 blinding of outcome assessors, 8 outcomes obtained from 85% of participants, 9 use of intent-to-treat analysis if protocol violated, 10 between-group statistical comparison and 11 point measures and measures of variability.
Level of evidence and strength of recommendation assessment method
To evaluate the quality of the current analysis, the Strength of Recommendation Taxonomy (SORT) was implemented.42 The SORT was designed to generate strength of recommendation based on the quality of the reviewed studies. The reviewed studies were classified either level 1 (good-quality patient-oriented evidence based on high-quality individual randomised control trial) or level 2 (limited-quality patient-oriented evidence based on lower quality clinical trial and cohort study) by primary and secondary authors. The patient-oriented evidence refers to information pertinent to patients such as morbidity and mortality42 and ACL injury was used in this project. After each reviewed study was evaluated, the following scales were determined by primary and secondary authors to express strength of the current analysis of evidence: A (consistent patient-oriented evidence), B (inconsistent evidence or limited-quality patient-oriented evidence) and C (consensus, usual practice, opinion, disease-oriented evidence).
Data extraction
For the primary purpose, the number of ACL injuries and the number of participants in each group (control and intervention groups) were extracted. When included studies included two consecutive years of NMT intervention, the numbers of ACL injuries and participants in control and intervention groups during first year were extracted. Similarly, to analyse effects of age, dosage, exercise and feedback, each variable was reviewed and extracted. Specifically, in order to analyse participants' age effects, a tertile age categorisation, mid teens (aged 14–18 years), late teens (aged 18–20 years) and early adults (older than 20 years), was developed. Dosage was divided by two components: duration and frequency of NMT. Time spent for NMT was labelled as duration. Dichotomous categorisation of short (up to 20 min of NMT) and long (more than 20 min of NMT) NMT duration was made. NMT frequency was classified either single (one NMT session per week) or multiple (at least two NMT sessions per week) categorisations. Similarly, two types of categorisations were generated for investigation of the effects of exercise variations: single (only one type of exercise) or several (more than one type of exercises). Status of verbal feedback was also dichotomised and rated either absence or presence based on availability of written statements in original studies. For the secondary purpose, early teen (younger than 14 years) category was also developed. These data were carefully reviewed and extracted by two independent reviewers. When there were discrepancies between the two reviewers during the data extraction and categorisation process, a third reviewer was invited to resolve the discrepancies.
Data synthesis
To determine combinatory effects of age, dosage, exercise and feedback, each study was evaluated with a numerical point system. Previous studies that examined effects of age, dosage and exercise on ACL injury expressed the risk reduction through OR, which ranges from 0.28 to 1.15.32,36,38 The reported OR was divided by 3 in order to classify each component to 1, 2 and 3 point. Following classifications were made: OR>0.77=1, OR between 0.76 and 0.39=2 and OR<0.38=3. Similar tertile approaches of ORs were previously performed.32,36,37 Higher points were given to each component that demonstrated lower OR, which is indicative of greater ACL injury reduction. On the basis of the OR categorisations, following numerical points were defined in each age, dosage and exercise components:
Age : early adults = 1; late teens = 2; mid - teens = 3
Dosage : duration : short NMT session = 1, long NMT session = 2 frequency : single NMT session per week = 1; multiple NMT sessions per week = 2
Exercise : single exercise type = 1; several exercise types = 3
Several exercise types were labelled 3 because previous investigation identified NMT programmes consisted of several exercise genres generated OR of 0.32.38 As there were no previous subgroup analyses based on status of feedback in NMT, effect of verbal feedback was conservatively estimated and expressed as:
Feedback : absence of verbal feedback = 0, presence of verbal feedback = 1
To identify age effects of NMT on ACL injury reduction, ACL injury was categorised by early teens (under 14 years), mid teens (aged 14–18 years), late teens (aged 18–20 years) and early adults (older than 20 years).
Data analysis
The points for each study were summed and expressed as a numerical study score (values 0–11), which was incorporated in a meta-regression model. A regression line was applied to express effects of the study scores (x-axis) on ACL injury. Since the meta-regression involves a logistic regression model, log OR (LOR) was displayed on the y-axis. To compare a ratio of ACL injuries in participants between intervention and comparison groups, an OR was used. In order to explain the per cent increase/decrease in odds, the LOR was further converted to OR by using following mathematical formulas:
Fixed-effects and random-effects models were analysed. It was assumed that the effect size of each study was different, and a fixed-effects model does not adjust variability among reviewed studies. Thus, the result of the fixed-effects models is proportional to the actual effect size of each study. Conversely, a random-effects model incorporates variability among studies and minimises the effect. Coefficient of determination (R2) value of random-effects model was calculated to determine variability of generated model. The R2 of fixed-effects model was not analysed because fixed-effects model reflects actual effect size of each study so that between-study variance is considered as 0. For the same reason, only random-effects model was used to determine age effects of NMT on ACL injury. I2 statistics were employed to examine total variation across the included studies due to heterogeneity as opposed to random chance. Egger's regression and trim and fill plot were used to examine potential risks of publication bias assessment. The α level of all analyses was set a priori at <0.05. A 95% CI was also incorporated. All analyses were performed using comprehensive meta-analysis software (BioStat, Englewood, New Jersey, USA).
Results
A total of 14 studies18–31 met the inclusion criteria of the current analyses. A total of 23 544 athletes (intervention group n=10 634; control group n=12 910) were included in the analyses. The study design, sports, age, dosage, exercise, feedback, study scores and number of ACL injuries in intervention and control groups of each NMT programme were summarised and were displayed in table 3.
Table 3. Summary of reviewed studies including study design, ages, duration, frequency, type, verbal feedback, total study scores and ACL injury.
| Study (years) | Study design | Age(mean ±SD)* | Duration | Frequency | Type | Verbal feedback | Total study scores | Number of ACL injury |
|---|---|---|---|---|---|---|---|---|
| Hewett et al (1999)31 | Prospective non-randomised cohort | 14–18 years (range) | 60–90 min | 3 days per week in preseason | Stretching, plyometrics, weight training | Yes | 11 | 5 (control) 2 (intervention) |
| Soderman et al (2000)18† | Prospective randomised control | C:20.4 ±5.4 years I: 20.4 ±4.6 years | 10–15 min | Each day for 30 days. 3 days per week rest of the season | Balance with balance boards | No | 5 | 1 (control) 4 (intervention) |
| Heidt et al (2000)19 | Prospective randomised control | 14–18 years (range) | 75 min | 3 days per week in preseason | Cardiovascular, plyometrics, strength, flexibility, agility and sports-specific drills | No | 10 | 8 (control) 1 (intervention) |
| Myklebust et al (2003)20‡ | Prospective non-randomised cross over | 21–22 years | 15 min | 3 days per week for 5–7 weeks. Once a week for rest of the season | Balance with mats and wobble boards | No in first intervention Yes in second intervention | 5 | 29 (control year) 23 (first intervention year) 17 (second intervention year) |
| Mandelbaum et al (2005)21 | Prospective non-randomised cohort | 14–18 years (range) | 20 min | 2–3 times per week in in-season | Basic warm-up, stretching, strengthening, plyometrics and agility | No | 10 | 67 (control) 6 (intervention) |
| Olsen et al (2005)22 | Prospective cluster randomised controlled | 16–17 years | 15–20 min | 15 consecutive sessions. Once a week for rest of the season | Warm-up, technique, balance, strength and power | Yes | 9 | 9 (control) 3 (intervention) |
| Petersen et al (2005)30§ | Prospective matched cohort | C:19.8 I: 19.4 years | 10 min | 3 times per week in preseason. Once per week for rest of the season | Education, balance board exercise, jump training | Yes | 8 | 5 (control) 1 (intervention) |
| Pfeiffer et al (2006)23 | Prospective non-randomised cohort | 14–18 years (range) | 20 min | 2 times per week in in-season | Plyometrics | No | 8 | 3 (control) 3 (intervention) |
| Steffen et al (2008)24 | Prospective block randomised controlled | 15.4 years | 15 min | 15 consecutive sessions. Once a week for rest of the season | Core stability, balance, plyometrics | Yes | 8 | 5 (control) 4 (intervention) |
| Gilchrist et al (2008)25 | Prospective cluster randomised controlled | C:19.9 years I: 19.9 years | 20 min | 3 times per week in in-season | Basic warm-up, stretching, strengthening, plyometrics and agility | Yes | 9 | 18 (control) 7 (intervention) |
| Pasanen et al (2008)26 | Prospective cluster randomised controlled | 24 years | 20–30 min | 2–3 times per week for preseason (intensive training period) and once a week in in-season (maintenance period) | Running techniques, balance and body control, plyometrics, strengthening | Yes | 10 | 4 (control) 6 (intervention) |
| Kiani et al (2010)27¶ | Prospective cluster non-randomised cohort | C: 15.0 I: 14.7 years | 20–25 min | 2 days per week for 2 months. Once a week for rest of the season | Core strengthening, balance | No | 9 | 5 (control) 0 (intervention) |
| LaBella et al (2011)28 | Prospective cluster randomised controlled | C: 16.2 I: 16.2 years | 20 min | 3 times per week in preseason and in-season | Strengthening, plyometrics, balance, agility | Yes | 11 | 6 (control) 2 (intervention) |
| Walden et al29 | Prospective cluster randomised controlled | C: 14.1 I: 14.0 years | 15 min | 2 times per week | Core stability, balance, jump-landing with knee alignment feedback | No | 9 | 14 (control) 7 (intervention) |
Unless otherwise indicated. ‘C’ stands for control group and ‘I’ stands for intervention group.
Although the study was a randomised controlled design, the follow-up rate was low (51.2%).
For the analysis purpose, only the 1st year intervention data was used.
Although there was no specific statement, the neuromuscular training indicated plyometric components.
Although there were jump-landing manoeuvers, repeated stretch-shortening cycles were not employed in the training. Therefore, the level of evidence was rated as II.
Meta-regression: fixed-effects model
The slope of the regression line that represents the 14 reviewed studies18–31 demonstrated that the four variables in the study scores are statistically significant predictors of ACL injury LOR (p=0.01, β1= −0.29, 95% CI −0.33 to −0.05) (figure 1). The mathematical model generated ACL OR of 0.828, which can be translated as 17.2% of ACL risk can be reduced if one of the four components was included.
Figure 1.
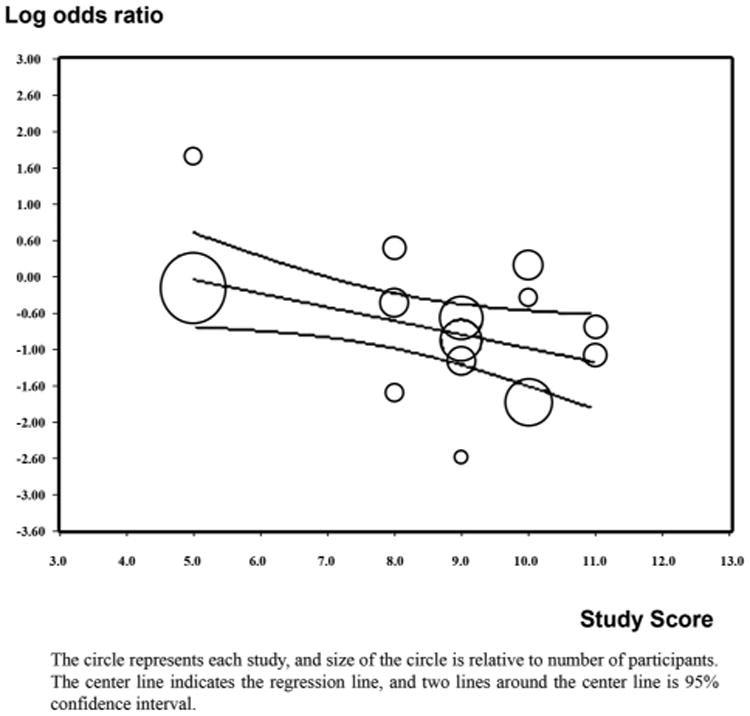
Meta-regression with fixed-effects model.
Meta-regression: random-effects model
The slope of the regression line that represented the 14 reviewed studies18–31 showed that the four variables included in the study scores are significant predictors of ACL injury LOR (p=0.03, β1=−0.20, 95% CI −0.37 to −0.03) (figure 2). The mathematical model indicated ACL OR of 0.823, which can be interpreted as 17.7% of ACL injury risk can be reduced if one of the four components was included.
Figure 2.
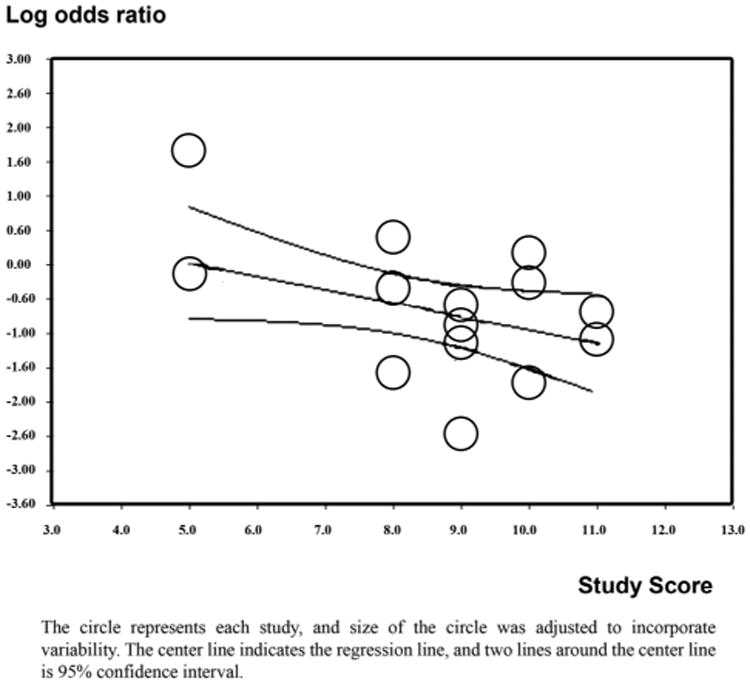
Meta-regression with random-effects model.
Coefficient of determination
The R2 value was analysed based on ratio of the between-study variance and total between-study variance. The obtained R2 value was 0.73, which can be translated that 73% of variability of the random-effects model was explained by the four components.
Age effect of NMT on ACL injury reduction
There was a statistically greater ACL injury reduction in midteens (14–18 years old: n=17 304, p=0.01, OR=0.293, 95% CI 0.19 to 0.44) compared to early teens (under 14 years old: n=2135, p=0.45, OR=0.288, 95% CI 0.01 to 7.09), late teens (18–20 years old: n=1711, p=0.07, OR=0.476, 95% CI 0.21 to 1.07), and early adults (older than 20 years old: n=2394, p=0.97, OR=1.011, 95% CI 0.62 to 1.64) (figure 3).
Figure 3.
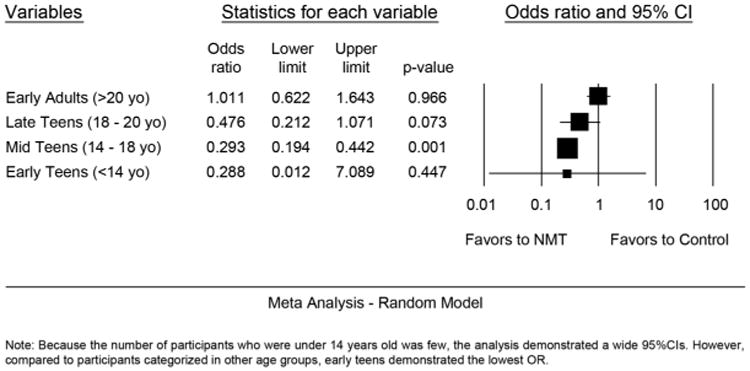
Subgroup analysis between four different age categorisations and ACL injuries. NMT stands for neuromuscular training.
Heterogeneity
The I2 statistics of the reviewed 14 studies18–31 did not reach statistical significance (p=0.09, I2 value: 36.4). Thus, significant heterogeneity effects were not found.
Bias assessment
Egger's regression for the publication bias for the 14 studies18–31 showed an interception at −0.17 (p=0.41, one-tailed test, 95% CI −1.93 to 1.59), indicating no publication bias, and the trim and fill plot also displayed no publication bias (figure 4).
Figure 4.
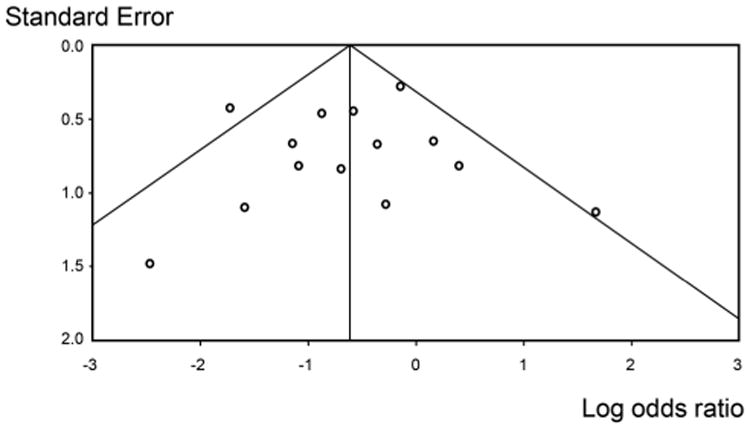
Trim and fill plot for testing publication bias.
Evidence synthesis
In the current analysis, seven of the included clinical trials19,22,24–26,28,29 were rated as level 1 (high-quality individual randomised control trial), while seven clinical trials18,20,21,23,27,30,31 were rated as level 2 (lower quality clinical trial and cohort study). Although the number of level 1 and 2 clinical trials was equal, the current meta-analysis supports consistency of evidence since 11 of the 14 reviewed studies demonstrated fewer ACL injuries in NMT intervention groups compared to control groups. On the basis of the consistency of the results from the included clinical trials, the strength of recommendation grade is A (recommendation based on consistent and good-quality patient-oriented study evidence).
Discussion
Combinatory effects of age, dosage, exercise and feedback on ACL injury reduction
The current project focused on determination of synergistic effects of combining key components in NMT that optimise ACL injury reduction in female athletes. Past studies demonstrated prophylactic effectiveness of NMT as an intervention to reduce ACL injury risk.32–35 Also, a series of subgroup analyses identified key components associated with NMT.32,36–38 However, combinatory effects of the key NMT components found in the previous subgroup analyses have not been answered. With using a meta-regression analysis, combinatory and synergistic effects of the key NMT components on ACL injury risk were quantified. On the basis of the significant association, the age of participants, NMT dosage, exercise variations within NMT, and utilisation of verbal feedback are considered key predictors of ACL injury reduction with an OR of 0.823–0.828 (figures 1 and 2). It can be interpreted that the risk of ACL injury can be reduced by 17.2–17.7% given that any of the four key components were incorporated in NMT. The obtained combination of the four components explains prophylactic effectiveness of NMT variations up to 73%. The ideal components of NMT that potentially influence outcome of NMT on ACL injury were unclear.33 However, the current study provides the more specific guidelines for the components of NMT prevention procedures.
It is observable that the regression model was most heavily influenced by one study,18 located at the upper left side of figures 1 and 2. On the basis of our definitions, this study was rated as one of the lowest scores (table 1) and reported more ACL injuries in the intervention group versus the control group.18 In this study, female soccer players were instructed to perform balance board exercises 10–15 min three times per week during the in-season. The dosage appears sufficient, but ages of the participants were slightly older (mean ages: 20.4 years old), and only one type of exercise type was incorporated. Combination of all the aspects may have influenced the negative outcome of this particular study.18
Study scores of the five studies19,21,25,28,31 were rated >9, and one common aspect in the five studies is the dosage of NMT. NMT protocols of all five studies were longer than 20 min of duration and at least two times per week in frequency. Previous subgroup analysis investigation reported an inverse dose–response association between NMT volume and ACL injury reduction.36 Therefore, the dosage is definitely a crucial point to consider for the development and implementation of NMT. In addition, it is interesting to note that the three studies with the highest study scores aimed to prevent ACL injury and also enhance athletic performance skills.19,21,25 One study24 measured variables associated with athletic performance.43 Using female soccer players, this study compared lower extremity strength and athletic performance tests including vertical jump tests, sprint running and soccer skill tests between intervention and control groups, but no significant difference was found between the two groups. Therefore, association between prophylactic effectiveness of NMT and athletic performance enhancement is inconclusive.
Effect of age
Two studies implemented the same NMT programme into the mid teens (14–18 years old) and late teens (19–20 years old) populations.21,25 One of the two studies that included midteens showed significant ACL injury reduction in two consecutive years21 (p=0.0001 year 1, p=0.0047 year 2). However, the study that implemented the same NMT programme for the late teens did not demonstrate significant ACL injury reduction.25 (p=0.07). The risk reduction of the intervention group in relation to control group in the study in mid teens was 81.9% compared to 73.4% in the study with late teens.44 In order to investigate the effect of age further, early teen (participants who are younger than 14 years old) category was created, and a subgroup analysis was performed. As the number of participants who were under 14 years old was few, the analysis demonstrated a wide 95% CIs and did not show statistical significance (p=0.45). However, compared to participants categorised in other age groups, early teens demonstrated the lowest OR (OR: 0.288, 95% CI 0.01 to 7.09) (figure 3). This finding is important from a standpoint of when the female athletes should begin preventive NMT. Since the peak age of ACL injury in female population is during the mid teens,45 it may be beneficial to begin the practice of preventive NMT in early teens. If appropriate NMT programmes are initiated prior to the time when female athletes are susceptible to ACL injury, risk of ACL injuries may be substantially prevented. Therefore, implementation of NMT in early ages is the first step for ACL injury reduction in female athletes.
Effect of dosage
An inverse dose–response relationship (the longer and more frequent NMT was practiced, the fewer ACL injuries were observed) was previously reported.36 Additionally, a previous subgroup analysis also reported a meaningful clinical implication: nearly 70% of ACL injuries can be reduced if the NMT is performed for 30 min duration and two times per week of frequency during the in-season.36 In this manuscript, the effect of dosage was analysed based on duration and frequency, and the current results confirmed that NMT prophylactic effectiveness on ACL injury is dose dependent. Owing to the inverse dose–response association,36 securing sufficient time for performing preventive NMT is a critical issue. Two reviewed studies noted low compliance to the given NMT was a limitation,20,24 and two other studies analysed effect of compliance on ACL injury37 and athletic injuries.46 To understand the compliance of NMT further, one study investigated coaches' perception of the NMT and identified a lack of knowledge, time restriction and lack of understanding and support as a barrier to implementing a NMT.47 Therefore, having educated healthcare practitioners who can bridge these gaps may be a key to successfully reduce ACL injury in young female athletes.
Effect of exercise variation
A previous investigation found a greater prophylactic effect on ACL injuries in NMT programmes that had multiple types of exercises compared to studies that instituted only a single type of exercise.38 Thus, exercise modality variations within NMT appeared to be critical. For instance, one study did not find significant ACL injury reduction in performing balance exercises alone.18 Similarly, another study that incorporated one type of exercises (plyometric exercises), but not other types of exercises, also failed to demonstrate ACL injury reduction.23 In short, a single type of exercise such as performing balance or plyometric exercises in isolation is not an effective exercise modality selection to reduce ACL injury. However, incorporating both exercises is more likely to demonstrate high prophylactic effectiveness. An investigation by Petersen et al used a programme with a combination of balance and plyometrics and did record fewer numbers of ACL injuries in the intervention group (78.8% of risk reduction relative to control group).44 Furthermore, NMT programmes that incorporated strengthening and proximal control exercises demonstrated significant decreases in ACL injury reduction when compared to NMT programmes that did not include these components.38 One of the novel findings in this review process was to observe a trend to include proximal control exercises in recent NMT programmes.24,27–29 The NMT programmes which included proximal control training demonstrated greater ACL injury reduction.38 Those exercises included plank24,29 and side plank24,29 as well as sit-ups/abdominal curl,27,31 push-up and upper body weight training.31 Numerous laboratory controlled studies that investigated the influence of proximal segments on lower extremity muscles reported an association between trunk and hip strength and knee joint kinematics.48–50 Therefore, the inclusion of trunk stabilisation and posterior chain strengthening exercise among plyometric and strength training components appear to be key to optimise the beneficial effects of NMT to reduce ACL injury.
Effect of verbal feedback
One reviewed study20 implemented 15 min of balance exercises once per week in female handball players. This study reported ACL injury reduction in the first intervention season compared to observation control season, but the reduction was not significant.20 (p=0.62, OR=0.87, 95% CI 0.50 to 1.52) Owing to the limited effect, a few modifications were introduced in the second intervention season: implementation of more sport (handball)-specific movements, challenging balance exercises, and emphasis on quality of movements with verbal feedback. To enhance the awareness of knee joint alignment, verbal cues such as ‘knee over toe’ was incorporated. With these modifications, fewer numbers of ACL injuries were recorded in the second intervention season.20 (p=0.15, OR=0.64, 95% CI0.35 to 1.18) Although it is difficult to identify which aspect contributed to further ACL injury reduction from the first to the second intervention seasons, including possible carry-over effects, use of verbal feedback could have provided beneficial effects on ACL injury reduction. After this study was published, a few ACL injury prevention studies incorporated verbal feedback into their programmes and subsequently demonstrated greater prophylactic effectiveness of NMT.22,25,28 Another reviewed study used verbal cues including ‘land softly’ and ‘don't let knees cave inward,’ and this study reported significant ACL injury reduction. (p=0.04, injury rate ratio =0.07 in intervention group vs injury rate ratio =0.26 in control group).28 Recent studies have also reported more prophylactically favourable biomechanical alterations when feedback mechanism was added to NMT39–41
Limitations
The present study was initially designed to include compliance/adherence of NMT as another key component. However, many reviewed studies did not record the compliance/adherence information in the original studies, or, the measurement methods varied considerably among reviewed studies. Therefore, this current meta-regression model was unable to include compliance/adherence as a key of components. Moreover, the focused populations (young female athletes) were homogenous, and significant heterogeneity effects were not detected, but several different types of sports were included in the reviewed studies, which were soccer,18,19,21,23–25,27–29,31 handball,20,22,30 basket-ball,23,28,31 volleyball23,31 and floorball.26 Compared to soccer, the number of studies focused on handball, basketball, volleyball and floorball were very limited.51 In fact, only six studies examined the effect of a preventive NMT on ACL reduction for handball20,22,30 and basketball.23,28,31 Unlike soccer, these other sports involve more upper body movements so that neuromuscular demands may be different than soccer. Hence, future investigations may need to focus on basketball, floorball, volleyball and handball athletes.
Conclusion
Current analyses found four variables to be significant predictors of ACL injury reduction in female athletes, and 73% of prophylactic effectiveness variability is explained by the four components. More precisely, 17% of ACL injury risk can be reduced if one of the four key variables met following conditions, which include that participants are younger, and NMT is performed longer than 20 min in duration and frequency greater than two times per week with more exercise variations within NMT along with usage of verbal feedback. Clinicians, experts and specialists in a field of sports medicine should consider the current study results when designing and implementing an ACL prevention NMT programme. Further investigations are necessary to determine the effects of the four key components on ACL injury reduction based on specific sporting activities.
What are the findings?
Inception of one of the four critical components of neuromuscular training, which include younger age, greater neuromuscular dosage, more exercise variations within neuromuscular training and utilisation of verbal feedback, can reduce the risk of ACL injury by 17.2–17.7%.
The four key components can explain prophylactic effectiveness of neuromuscular training variability up to 73%.
How might it impact on clinical practice in the future?
Neuromuscular training is an effective intervention to reduce ACL injury risk in physically active females.
The prophylactic effectiveness of neuromuscular training to reduce ACL injury risk is greater in young athletes.
There is an inverse dose–response association between compliance/dosage of neuromuscular training and ACL injury risk.
The more pronounced prophylactic effectiveness of neuromuscular training was obtained when a variety of exercises, particularly, strengthening and proximal control training, were performed with verbal feedback.
Acknowledgments
The authors appreciate every member and supporting personnel of the Micheli Center for Sports Injury Prevention and division of Sports Medicine at Boston Children's Hospital, especially Felix Wang.
Funding: Funding support from National Institutes of Health/NIAMS Grants R21AR065068-01A1 and U01AR067997.
Footnotes
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/bjsports-2015-095596).
Contributors: DS conceptualised and designed the study, analysed the data and contributed to the writing and revisions of the manuscript. GDM provided valuable input, critically reviewed the manuscript and participated in drafting the manuscript. KDBF critically reviewed the manuscript and participated in drafting the manuscript. MJP performed data interpretation, critically reviewed the manuscript, and participated in drafting the manuscript. LJM delivered directional guidance, provided valuable input, critically reviewed the manuscript and participated in drafting the manuscript. TEH delivered directional guidance, critically reviewed the manuscript and participated in drafting the manuscript. All of the named authors approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93:1510–18. doi: 10.2106/JBJS.J.01320. [DOI] [PubMed] [Google Scholar]
- 2.Binfield PM, Maffulli N, King JB. Patterns of meniscal tears associated with anterior cruciate ligament lesions in athletes. Injury. 1993;24:557–61. doi: 10.1016/0020-1383(93)90038-8. [DOI] [PubMed] [Google Scholar]
- 3.Paletta GA, Jr, Levine DS, O'Brien SJ, et al. Patterns of meniscal injury associated with acute anterior cruciate ligament injury in skiers. Am J Sports Med. 1992;20:542–7. doi: 10.1177/036354659202000510. [DOI] [PubMed] [Google Scholar]
- 4.Cimino F, Volk BS, Setter D. Anterior cruciate ligament injury: diagnosis, management, and prevention. Am Fam Physician. 2010;82:917–22. [PubMed] [Google Scholar]
- 5.Shelbourne KD, Nitz PA. The O'Donoghue triad revisited. Combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19:474–7. doi: 10.1177/036354659101900509. [DOI] [PubMed] [Google Scholar]
- 6.Wojtys EM, Brower AM. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. 2010;45:509–12. doi: 10.4085/1062-6050-45.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Csintalan RP, Inacio MC, Funahashi TT, et al. Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:619–25. doi: 10.1177/0363546513511416. [DOI] [PubMed] [Google Scholar]
- 8.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–78. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641–7. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 10.Greenberg EM, Greenberg ET, Ganley TJ, et al. Strength and functional performance recovery after anterior cruciate ligament reconstruction in preadolescent athletes. Sports Health. 2014;6:309–12. doi: 10.1177/1941738114537594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clagg S, Paterno MV, Hewett TE, et al. Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45:444–52. doi: 10.2519/jospt.2015.5040. [DOI] [PubMed] [Google Scholar]
- 12.Paterno MV, Schmitt LC, Ford KR, et al. Altered postural sway persists after anterior cruciate ligament reconstruction and return to sport. Gait Posture. 2013;38:136–40. doi: 10.1016/j.gaitpost.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmitt LC, Paterno MV, Ford KR, et al. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47:1426–34. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elias AR, Hammill CD, Mizner RL. Changes in quadriceps and hamstring cocontraction following landing instruction in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45:273–80. doi: 10.2519/jospt.2015.5335. [DOI] [PubMed] [Google Scholar]
- 15.Øiestad BE, Engebretsen L, Storheim K, et al. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–43. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 16.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–52. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Myer GD, Ford KR, et al. Dynamic neuromuscular analysis training for preventing anterior cruciate ligament injury in female athletes. Instr Course Lect. 2007;56:397–406. [PubMed] [Google Scholar]
- 18.Soderman K, Werner S, Pietila T, et al. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8:356–63. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 19.Heidt RS, Jr, Sweeterman LM, Carlonas RL, et al. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659–62. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 20.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13:71–8. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–10. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 22.Olsen OE, Myklebust G, Engebretsen L, et al. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330:449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfeiffer RP, Shea KG, Roberts D, et al. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88:1769–74. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 24.Steffen K, Myklebust G, Olsen OE, et al. Preventing injuries in female youth football —a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18:605–14. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 25.Gilchrist J, Mandelbaum BR, Melancon H, et al. Neuromuscular training and the risk of leg injuries in female floorball players: cluster randomised controlled study. BMJ. 2008;337:a295. doi: 10.1136/bmj.a295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pasanen K, Parkkari J, Pasanen M, et al. Effect of a neuromuscular warm-up programme on muscle power, balance, speed and agility: a randomised controlled study. Br J Sports Med. 2009;43:1073–8. doi: 10.1136/bjsm.2009.061747. [DOI] [PubMed] [Google Scholar]
- 27.Kiani A, Hellquist E, Ahlqvist K, et al. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170:43–9. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 28.LaBella CR, Huxford MR, Grissom J, et al. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:1033–40. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 29.Walden M, Atroshi I, Magnusson H, et al. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. doi: 10.1136/bmj.e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614–21. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 31.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 32.Myer GD, Sugimoto D, Thomas S, et al. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41:203–15. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor JB, Waxman JP, Richter SJ, et al. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: a systematic review and meta-analysis. Br J Sports Med. 2015;49:79–87. doi: 10.1136/bjsports-2013-092358. [DOI] [PubMed] [Google Scholar]
- 34.Grimm NL, Jacobs JC, Jr, Kim J, et al. Anterior cruciate ligament and knee injury prevention programs for soccer players: a systematic review and meta-analysis. Am J Sports Med. 2015;43:2049–56. doi: 10.1177/0363546514556737. [DOI] [PubMed] [Google Scholar]
- 35.Gagnier JJ, Morgenstern H, Chess L. Interventions designed to prevent anterior cruciate ligament injuries in adolescents and adults: a systematic review and meta-analysis. Am J Sports Med. 2013;41:1952–62. doi: 10.1177/0363546512458227. [DOI] [PubMed] [Google Scholar]
- 36.Sugimoto D, Myer GD, Barber Foss KD, et al. Dosage effects of neuromuscular training intervention to reduce anterior cruciate ligament injuries in female athletes: meta- and sub-group analyses. Sports Med. 2014;44:551–62. doi: 10.1007/s40279-013-0135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sugimoto D, Myer GD, Bush HM, et al. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47:714–23. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sugimoto D, Myer GD, Barber Foss KD, et al. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2015;49:282–9. doi: 10.1136/bjsports-2014-093461. [DOI] [PubMed] [Google Scholar]
- 39.Myer GD, Stroube BW, DiCesare CA, et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. Am J Sports Med. 2013;41:669–77. doi: 10.1177/0363546512472977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stroube BW, Myer GD, Brent JL, et al. Effects of task-specific augmented feedback on deficit modification during performance of the tuck-jump exercise. J Sport Rehabil. 2013;22:7–18. doi: 10.1123/jsr.22.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parsons JL, Alexander MJ. Modifying spike jump landing biomechanics in female adolescent volleyball athletes using video and verbal feedback. J Strength Cond Res. 2012;26:1076–84. doi: 10.1519/JSC.0b013e31822e5876. [DOI] [PubMed] [Google Scholar]
- 42.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17:59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 43.Steffen K, Bakka HM, Myklebust G, et al. Performance aspects of an injury prevention program: a ten-week intervention in adolescent female football players. Scand J Med Sci Sports. 2008;18:596–604. doi: 10.1111/j.1600-0838.2007.00708.x. [DOI] [PubMed] [Google Scholar]
- 44.Sugimoto D, Myer GD, McKeon JM, et al. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46:979–88. doi: 10.1136/bjsports-2011-090895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.LaBella CR, Hennrikus W, Hewett TE. Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics. 2014;133:e1437–50. doi: 10.1542/peds.2014-0623. [DOI] [PubMed] [Google Scholar]
- 46.Soligard T, Nilstad A, Steffen K, et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010;44:787–93. doi: 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- 47.Joy EA, Taylor JR, Novak MA, et al. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J Strength Cond Res. 2013;27:2263–9. doi: 10.1519/JSC.0b013e31827ef12e. [DOI] [PubMed] [Google Scholar]
- 48.Baldon Rde M, Lobato DF, Carvalho LP, et al. Effect of functional stabilization training on lower limb biomechanics in women. Med Sci Sports Exerc. 2012;44:135–45. doi: 10.1249/MSS.0b013e31822a51bb. [DOI] [PubMed] [Google Scholar]
- 49.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154–63. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 50.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41:625–32. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 51.Sugimoto D, Myer GD, Micheli LJ, et al. ABCs of evidence-based anterior cruciate ligament injury prevention strategies in female athletes. Curr Phys Med Rehab Rep. 2015;3:43–9. doi: 10.1007/s40141-014-0076-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


