Abstract
National HIV preventive programs in Mexico focus on high-risk groups that do not consider women, apart from prenatal screening. Nonetheless, the epidemic in women is growing, and there is a need to better understand sociodemographic factors in women living with HIV (WLH). We performed a case–control study in Mexico City, including HIV+ and HIV− women with a recent pregnancy to compare their sociodemographic characteristics and describe the circumstances of diagnosis in HIV+ women, as well as prenatal screening frequency in both groups. Fifty cases and 102 controls were interviewed. HIV+ women were more frequently the only economic support of the family (20% vs 0%, P < .0001). Thirty-eight percent of cases had their first pregnancy at ≤18 years, versus 16% of controls (odds ratio 2.47, 95% confidence interval 1.07–5.72, P = .03); 16% of cases had lived in the street; 6% reported transactional sex, versus none of the controls (P < .0001). In the multivariate analysis, there was strong evidence of an association between HIV infection and age at the time of the interview, history of sexually transmitted diseases, substance abuse, history of violence, and civil status. Only 6% of controls were tested for HIV during prenatal follow-up. WLH in this study faced important social vulnerability. Targeting women living in these social contexts might increase early diagnosis and could tailor HIV prevention strategies. Prenatal coverage needs to be improved and should represent a national priority.
Keywords: HIV epidemic in women, HIV in Mexico, prenatal HIV screening, vulnerability in women
1. Introduction
Mexico, as other Latin American countries, has a concentrated HIV epidemic, mostly driven by men who have sex with men (MSM), who represent 70% of all people living with HIV in the country. While the overall prevalence is about 0.3%, HIV prevalence among MSM ranges from 9.9 to almost 20%.[1] Women account for 20% of new cases of HIV infection in Mexico.[2] Although this proportion has remained rather stable in the last 5 years,[3] the frequency of heterosexual transmission has risen, and the male-to-female ratio has decreased from 1:31 at the beginning of the epidemic to 1:4 in recent years.[3,4] The factors associated to HIV infection in women have changed since the beginning of the epidemic[5] and continue to do so. Therefore, there is a growing need to understand the HIV epidemic in women, which has been increasing in all Latin America.[6–8]
So far, due to its concentrated nature, most of the national HIV programs and policies have focused on high-risk groups, such as MSM, transgender women, sex workers, and injection drug users. National HIV prevention programs do not target women outside these groups. Women are considered to be at low risk for HIV infection. The only national preventive policy focused on women in Mexico is HIV screening for prevention of mother-to-child transmission (PMTCT). However, despite being mandatory and even though reports have showed the test is well accepted when offered,[9,10] the coverage for HIV test in pregnancy is still insufficient in the country: 56% according to the Pan American Health Organization (PAHO).[11]
A better understanding of the characteristics of women living with HIV (WLH) would help to better identify potential targets that need to be tackled by national HIV preventive policies addressing specifically women. Although some studies describe Mexican women with HIV as highly vulnerable,[8,12,13] so far no studies have compared them to women without HIV. The aim of this study was to compare the sociodemographic characteristics of HIV-positive and HIV-negative women with a recent pregnancy, and evaluate the circumstances of HIV diagnosis for positive women. We also looked at the prenatal screening frequency in both HIV-positive and -negative women.
2. Methods
2.1. Study design
This was a case–control study conducted in Mexico City, both in the Clínica Especializada Condesa (CEC) and the General Hospital Manuel Gea Gonzalez (GHMGG).
2.2. Setting
The CEC is an ambulatory HIV referral center providing service at no cost to people without employment-linked health insurance. The clinic has a population of 13,000 patients on HIV care; 10% of them are women. The GHMGG is one of the main referral hospitals of the Southern area of Mexico City for HIV-positive patients who require in-hospital care. It has a gynecological–obstetric service that receives on average 232 pregnant women per month for delivery. Many of the women attending the hospital arrive during labor and have not received any prenatal care. As a general practice, all pregnant women with unknown HIV status attending the hospital for delivery are offered an HIV rapid test. Also, most of the pregnant WLH who get their regular prenatal care at CEC are referred to this hospital for delivery.
2.3. Study procedures and study participants
Between November 2013 and March 2014, a quantitative questionnaire was applied through face-to-face structured interviews to Mexican-born women with a recent history of pregnancy, defined as pregnancies between 2010 and 2013. Cases were HIV-positive women older than 18 years, identified either through the CEC, during their gynecological consultations before or after delivery or directly at the GHMGG at any stage of pregnancy. Some of the HIV-positive women were recently diagnosed in the GHMGG during labor. We excluded WLH who acquired the infection through vertical transmission. For logistical reasons, controls were hospital-based; they were defined as HIV-negative women older than 18 years, all identified at the GHMGG after labor, either before hospital discharge or in the first month after delivery.
Women fulfilling the inclusion criteria were invited to participate. Written informed consent was obtained from all of them. The questionnaire was divided in 5 main sections. For all of the interviewees it included: cultural and sociodemographic characteristics (including violence and sexual abuse), medical history (including sexual risk behavior), description of their last pregnancy, economic aspects, and knowledge about HIV.
Violence was considered as present if the women reported having experienced any physical or psychological violence at any time. As for sexual abuse, women were asked if they had ever suffered from any kind of sexual abuse, at any age and regardless of the aggressor.
An additional section was only applied to WLH and included questions about circumstances of HIV diagnosis and access to medical care. This questionnaire was adapted from a validated questionnaire used in a previous study for Mexican HIV-positive women.[13] To avoid observer bias, all questions were formatted as multiple-choice questions, with objective answers that did not depend on the interviewer's perception.
2.4. Statistical analysis
Descriptive frequencies are reported as percentages, and as measures of central tendency and variation, by HIV status. The median and interquartile range (IQR) are used, since the data were skewed to the right and not normally distributed. Statistical analysis was done with STATA 14.0 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). Mann–Whitney U test was used for hypothesis testing in quantitative variables as a nonparametric test in cases of nonnormal distribution. The χ2 test was used for categorical variables. A univariate analysis was done to compare cases and controls. To control for confounding, a logistic regression model was built with HIV infection as the binary outcome and included those variables found to have an association with HIV infection in the univariate analysis; considered as P < .05. For the multivariate model, some of the variables were grouped since subgroups were very small. One variable grouped as “any kind of violence” was defined as having experienced sexual abuse or physical or psychological violence. Another variable grouped as “any kind of substance use” was defined as the consumption at any time of solvents or marihuana or MDMA (methylenedioxymethamphetamine). We also regrouped 1 variable as “any sexually transmitted diseases (STD)” when cervicitis, genital ulcers, or genital warts were reported.
2.5. Ethics committee
The institutional review board of the GHMGG reviewed and approved the study (reference number 36-90-2013), and the study was authorized by the CEC coordination. Only participants who gave written informed consent were included. The interviewer read the informed consent with each woman to ensure they understood the confidentiality and anonymity of their statements and their liberty to withdraw from the study at any time. Also, every woman was offered the option of being referred to legal counseling and psychological support, in case sensitive issues (such as reported violence) appeared during the interview.
3. Results
Seventy-four cases and 111 controls were invited to the study; 37 refused to participate, mostly due to a lack of time. Fifty cases and 102 controls were interviewed. Characteristics of both groups are reported in Table 1.
Table 1.
Characteristics of cases and controls.
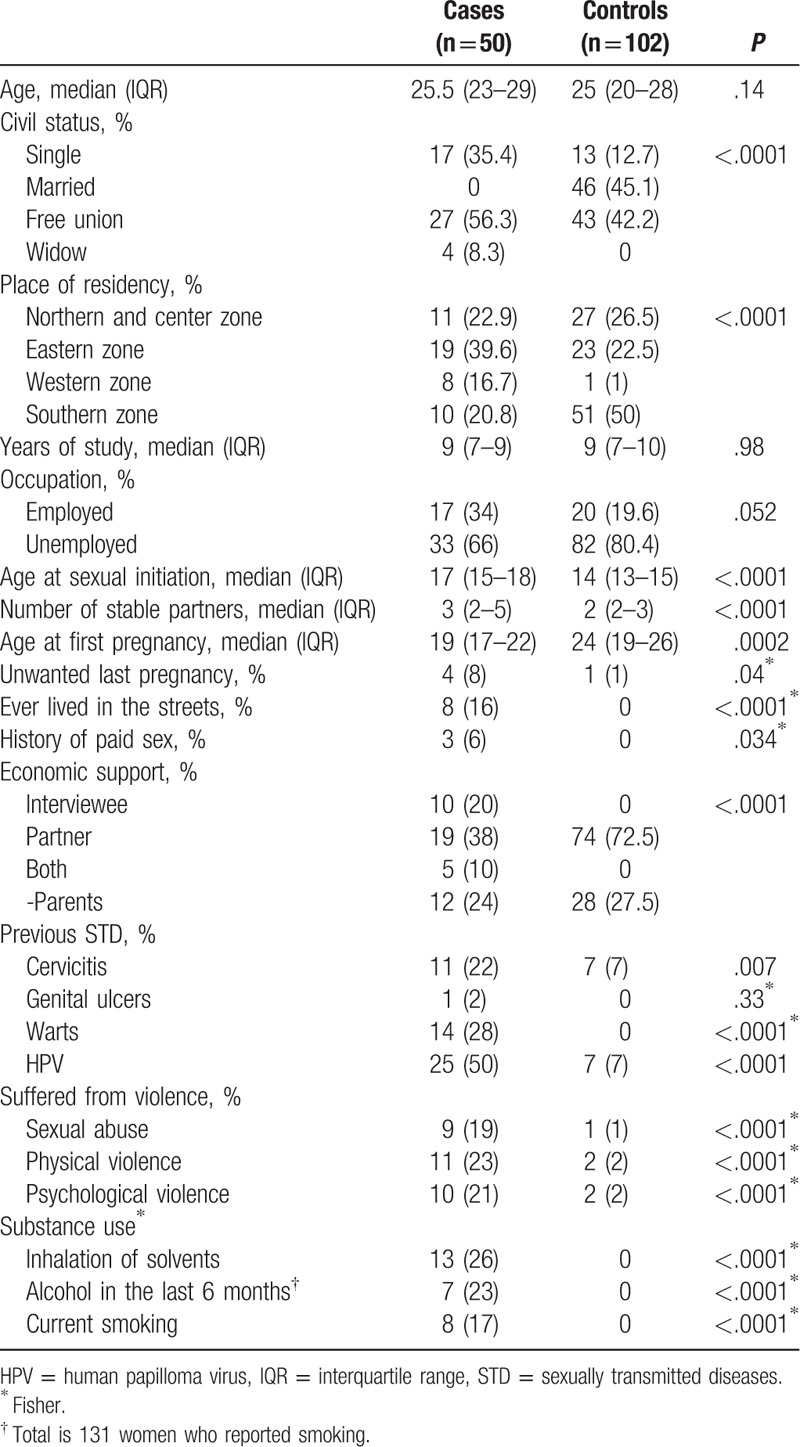
3.1. Socioeconomic context
There were no differences between groups in age and level of education. There was a higher proportion of widows or separated women in the cases compared to the controls (43.7% vs 12.7%, P < .0001). Cases were slightly less unemployed than controls (66% compared to 80.4%, P = .052) and more frequently the only economic support of the family (20% compared to 0%, P < .0001). Cases relied less on their partner or parents for economic support, compared to controls (62% compared to 100%, P < .0001). Sixteen percent of cases reported having lived in the street, and 6% reported transactional sex, compared to none of the controls (P < .0001). More cases lived in the eastern area of the city (40% vs 22.5% of controls, P < .0001). The controls lived closer to the hospital, in the southern area of the city (50% vs 21% of cases). This difference seems to be mainly related to the fact that controls were assigned to this hospital due to their address location, and cases were mostly referred from primary care places due to their HIV+ condition.
3.2. Reproductive context
Cases reported a slightly higher number of sexual partners than controls (2 IQR 2–3, vs 3 IQR 2–5, P < .0001). There were no differences in the number of pregnancies, abortions or number of offspring between groups. Although the median age at sexual initiation was lower in controls compared to cases (14 years IQR 13–15, vs 17 years IQR 15–18, P < .0001), cases had their first pregnancy at a younger age than controls (19 years IQR 17–22, vs 24 years IQR 19–26, P < .0002); 38% of cases had their first pregnancy at 18 years or less, compared to 16% of controls (odds ratio [OR] 2.47, 95% confidence interval [CI] 1.07–5.72, P = .03). Last pregnancy was unwanted in 8% of cases compared to none of the controls (P = .023). Overall 46% of cases had had an STD (defined as cervicitis, warts, or genital ulcers) compared to 7% of controls (P < .0001). More cases reported a previous human papilloma virus (HPV) diagnosis compared to controls (50% vs 7%, P < .0001)
3.3. Substance abuse
None of the participants reported intravenous (IV) drug use or ever consuming cocaine or heroin. Only a few reported marihuana (1 case and 1 control) and MDMA use (1 control). Cases reported more inhalation of solvents (26% vs 0% in controls, P < .0001). Overall, almost a third of cases had consumed solvents, marihuana, or MDMA at least once (28%) compared to 2% of the controls (P < .0001). In the univariate analysis, cases had 19 times the odds of having used any of those substances, compared to controls (OR 19.44 95% CI 3.65–103–66, P < .0001). Also 20% of cases were current smokers, compared to none of the controls (P < .0001), and 23% of cases had drank alcohol in the last 6 months compared to none of the controls (P < .0001).
3.4. Violence and HIV
Cases reported higher levels of any kind of violence: 18%, 22%, and 21% of cases had been victims of sexual abuse, physical, or psychological violence, respectively, compared to 1%, 2%, and 2% of the controls (P < .0001). In general, in the univariate analysis, cases had 16 times the odds of being subjected to some kind of violence (sexual, physical, or psychological) compared to the controls (OR = 16.05 95% CI 4.35–59.28, P < .0001).
3.5. Circumstances of diagnosis in HIV-infected women
All HIV diagnosis were made between 2003 and 2013, half of them after 2012. The most frequent reasons to be diagnosed were after their partner was diagnosed (36%), through screening (32%), (including prenatal), because of symptoms (22%) and 10% after their child was diagnosed.
3.6. HIV screening during pregnancy
Although 96% of all women received medical attention during their last pregnancy, screening during pregnancy was low. Only 6% of the controls were tested for HIV during prenatal follow-up. Among the cases, 23 women (46%) already knew they were HIV-positive before their last pregnancy. Of the 27 women who did not know their status, 5 did not get a test during their last pregnancy, and were diagnosed after because they were symptomatic (3) or because an offspring was diagnosed (2). Nine women were diagnosed during pregnancy, but for other reasons than prenatal screening (symptoms or a partner infected). Only 13 women were tested because they were pregnant, 8 of them were tested during labor.
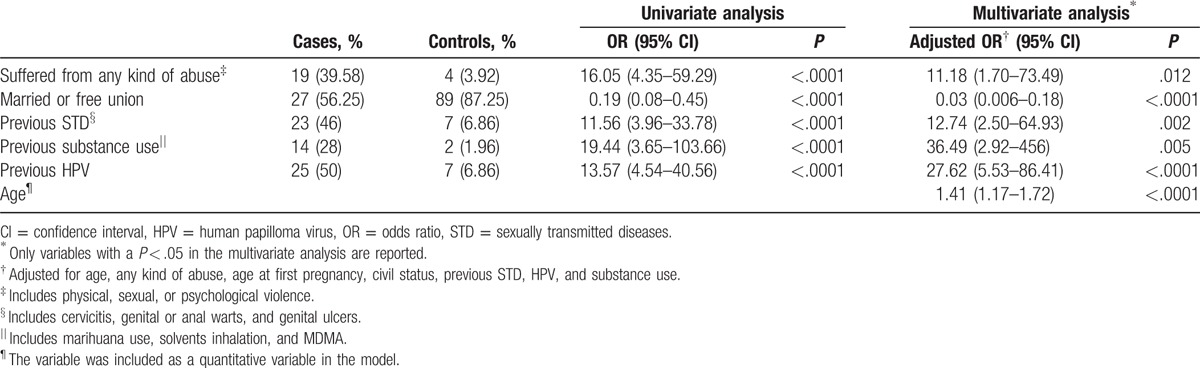
3.7. Multivariate analysis
The logistic regression model is reported in Table 2. The adjusted odds ratio reported was controlled for age at the moment of the interview (as a quantitative variable), age at first pregnancy, civil status, any kind of violence (a variable including physical, sexual, or psychological violence), any kind of substance abuse (a variable including use of solvents, marihuana, or MDMA), a history of STD (including genital ulcers, cervicitis, or warts), and history of HPV. After adjusting for all these variables, there was still strong evidence of an association between HIV infection and age at the time of the interview, history of STD or HPV, history of substance abuse, history of violence, and civil status. After we included the city area of residency, the model was not significantly modified.
Table 2.
Multivariate logistic regression.
4. Discussion
The first Mexican woman reported with AIDS in 1985 was infected through tainted blood.[5] During the first decade, HIV epidemic in women was mainly due to blood transfusion with a gradual transition to heterosexual transmission. Nowadays, WLH in Mexico are usually married or in free union, have few sexual partners and their main risk factor for HIV acquisition is their stable partner.[14] They frequently face gender inequity and its consequences: intramarital violence, economic dependency, lack of condom negotiation, lower levels of education, and lower wages when compared to men.[6,15] These characteristics pose women's HIV epidemic in a different social setting than many of the “most-at-risk populations” (MARP's).[6,15] Although they have a much lower prevalence of HIV (less than 0.1%), women with the aforementioned characteristics represent the majority of WLH in Mexico.[8]
This is the first study to compare sociodemographic characteristics between HIV-positive and HIV-negative women in childbearing age in Mexico City. It highlights some social determinants that support a highly vulnerable profile of HIV-positive women that are not included in the MARP's.
In this study, women infected with HIV report more frequently a history of substance use, STDs, and violence than HIV-negative women. So far, previous reports done in Mexico including only HIV-positive women had described them with a high prevalence of sexual abuse, physical violence, and STDs. That prevalence, when using national surveys and census as a comparator, seemed higher than the prevalence reported in the general population of women.[13] There are no published studies comparing HIV-positive with HIV-negative women in Mexico. One study compared gender differences between HIV-positive men and women in Mexico City and found that in general, women had less years of schooling than men, lower average monthly salaries, and they were more likely to have been infected by a stable partner than men. Their data support more social vulnerability and economic marginalization in women, compared to HIV-positive men in whom riskier sexual behaviors predominate. This highlights the need to address preventive policies to fight the epidemic differently for each gender.[6] One study published in Brazil in 2009 analyzed and compared HIV-negative and HIV-positive women interviewed in 2003 to 2004, using a similar questionnaire, with comparable results: their findings also highlight higher levels of violence, substance abuse and STD, as well as transactional sex, in HIV-positive women.[16] In that study, HIV-positive women were also more frequently living without a partner as was found in the present study.
We report substance abuse as associated to HIV infection. Although none of the interviewees reported IV drug use, they used solvents, which are cheap and accessible substances that could represent a proxy of low socioeconomic levels. Moreover, almost 25% of cases had been drinking in the last 6 months and 20% were current smokers. Alcohol use and smoking have been reported in women as a way of coping with stressors and negative emotions, not only related to HIV but to economic distress and violence.[17,18] In a qualitative study using focus groups, HIV-infected women reported drinking as a way of self-managing emotions, life issues or bad experiences, and controlling their mood.[17]
WLH are frequently single and they usually have to work and earn money in order to support the family. In general, substance abuse has also been associated to poor ART adherence.[19] We report a higher prevalence of substance abuse in a group of women that do not belong to recognized “high-risk behavior groups” such as sex workers or IV drug users. These results show that substance abuse has become frequent among HIV-positive women that are not typically considered as “MARP's”. Since this is a cross-sectional study, we were not able to specify the timing of substance use in relation to the HIV diagnosis; however, this issue should be addressed as part of HIV preventive programs and retention in care programs. Moreover, it should not only be addressed in terms of HIV risk but also in terms of the consequences of alcohol exposure in utero, which is an important cause of preventable poor birth outcomes.[18] In this study, many women were drinking during their pregnancy; this urges for better detection of prenatal alcohol consumption and the inclusion of stronger programs for prevention of substance consumption during pregnancy as part of the prenatal follow-up of HIV-infected women.
Mexico is a country with a high prevalence of violence in the general population. National surveys have reported up to 40% to 60% of physical violence against women.[20,21] The prevalence of violence reported here is lower than the one reported in these surveys; however, there were higher rates of violence in cases than controls. Many studies have analyzed violence and its association with HIV.[12,22] On the one hand, violence leads to an increased risk of acquiring HIV in prospective studies[22] and has also been reported as an obstacle for seeking medical care. On the other hand, HIV diagnosis disclosures can increase domestic violence, which can impact in women's staying in care and adhere to HIV treatment.[12,23] In this study, we did not ask if the violence experienced was before, during, or after the pregnancy. We cannot define the temporality of violence with respect to HIV infection. However, violence should be a matter to tackle both for HIV prevention and retention in care issues and more efforts should be made to screen and identify pregnant women suffering from any type of violence during their pregnancy, due to the consequences for both the offspring and the mother. On the other hand, studies show that screening for violence in maternal health services increases detection of women suffering intimate partner violence.[24] More studies should be done to establish the prevalence of violence in HIV-infected women during their pregnancy, but these results prompt for better screening tools during prenatal care.
HIV-positive women reported more frequently STD than HIV-negative women, which is compatible with previous literature. The prevalence of STD in this study is probably underestimated since diagnostic tests for infections such as gonorrhea or chlamydia are not widely available in Mexico. Besides the fact that HPV infection and other STD are clearly described as risk factors associated with acquiring HIV, many studies have also described STD clinics as an opportunity to improve prevention and early diagnosis, since these clinics are the main contacts with medical services in young women.[13,25] It has been reported that women tend to have more medical contacts than men, through family planning and screening for cervical and breast cancer. This should be an opportunity to extend HIV test offer and improve HIV detection in women.
Although cases and controls were similar in age and education levels, there were differences according to their place of residence. Controls tended to live closer to the hospital, in the south of the city, which is due to the selection method: they were hospital-based controls that are assigned to that hospital by place of residence. Cases tended to live either closer to the HIV clinic of reference (CEC) or to the eastern zone of the city. The eastern part of the city has specific markers of less social and urban development and higher rates of delinquency, and a higher prevalence of HIV in the city. The place of residence was also associated to different levels of substance abuse: 40% of women reporting previous STDs lived in the east zone, as well as almost a third of women using substances. Even when the place of residence was included in the multivariate model, there was still an association between substance abuse and STDs with HIV infection.
Finally, many recent studies in Mexico report low levels of HIV test offering during pregnancy, despite prenatal HIV screening being a national official recommendation. This study reports again very low levels of HIV testing in the controls, which could be considered as a representation of the whole population without employment-linked health insurance. Only 6% of them were tested during their last pregnancy, despite studies done in Mexico that show that women are willing to accept the test when receiving appropriate counseling.[9,10,26] Notwithstanding many campaigns conducted to promote HIV testing in the country, and the fact that it is an official recommendation,[27] this is still a field of missed opportunities with an urgent need of reinforcement nationwide. In this sample, there were still 2 children in whom vertical transmission was not prevented. This fact, in an era of universal access to antiretroviral therapy, is unacceptable.
This study has some limitations. As mentioned before, since it is a case–control study, the causality and temporality of the associations found cannot be ascertained. However, it is more likely that the vulnerability factors reported here are part of a scenario frequently faced by WLH, and thus they could be considered as risk factors. The study included childbearing age women coming to a general hospital in Mexico City, which makes the findings applicable to this population of women. There could be some different findings in women from rural settings. Finally, women were not randomly selected, and it is also possible that the women who did not accept to participate had a different profile from the women interviewed, which could lead to a selection bias.
5. Conclusion
Mexican women of childbearing age living with HIV face important social vulnerability, which possibly represents a risk factor for HIV acquisition. We specifically found that violence and non-IV substance abuse were associated to HIV. Adequately addressing women living in these social contexts might increase early diagnosis and may also open new perspectives for tailored HIV prevention strategies. Furthermore, some of these social determinants could also be related to poor linkage and retention in care. Exploring the impact that different social factors have in the continuum of care of Mexican WLH might also contribute to improve retention and adherence to ART. Moreover, the results suggest better screening tools are needed to identify and address issues such as substance use and violence during the pregnancy.
Routine HIV testing during pregnancy is one of the most important goals both for World Health Organization and PAHO to fight the HIV epidemic. Mexico's performance regarding PMTCT needs improvement and should represent a major priority for health programs and policy makers.
Acknowledgments
To all the women who participated in the study's interviews.
Footnotes
Abbreviations: CEC = Clínica Especializada Condesa, GHMGG = General Hospital Manuel Gea Gonzalez, HPV = human papilloma virus, MARP = most-at-risk population, MDMA = methylenedioxymethamphetamine, MSM = men who have sex with men, PAHO = Pan American Health Organization, PMTCT = prevention of mother-to-child transmission, STD = sexually transmitted disease, WLH = women living with HIV.
Author's contributions: DAZ designed and implemented the study and contributed to the data analysis and writing of the manuscript. APM, PVF, and AMO contributed to the design, analysis of data, and writing of the manuscript. PRZ contributed to the analysis of data and writing of the manuscript. URA and TDJ contributed to the implementation and writing of the manuscript.
There was no funding for this study. AMO and PVF have received honoraria from Abbvie, DAZ, APM, URA, and TCL declares no conflicts of interest; PRZ has received honoraria from Stendhal, AstraZeneca, Pfizer, and MSD.
References
- [1].Bautista-Arredondo S, Colchero MA, Romero M, et al. Is the HIV epidemic stable among MSM in Mexico? HIV prevalence and risk behavior results from a nationally representative survey among men who have sex with men. PLoS One 2013;8:e72616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].CENSIDA. Women and HIV and AIDS in Mexico. CENSIDA: National Centre for Prevention and Control of HIV/AIDS; 2016. [Google Scholar]
- [3].Ministry of Health, Secretaria de Salud C. Ministry of Health. National Report of the advances on HIV/AIDS response.2014. 2014. [Google Scholar]
- [4].Allen Leigh B, Gender, power and HIV/AIDS in women's life. In: Public Health National Institute, 25 years of HIV in Mexico: achievments and challenges 2009. [Google Scholar]
- [5].Volkow P, Mohar A, Terrazas JJ, et al. Changing risk factors for HIV infection. Arch Med Res 2002;33:61–6. [DOI] [PubMed] [Google Scholar]
- [6].Bautista-Arredondo S, Servan-Mori E, Beynon F, et al. A tale of two epidemics: gender differences in socio-demographic characteristics and sexual behaviors among HIV positive individuals in Mexico City. Int J Equity Health 2015;14:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Johnson M, Samarina A, Xi H, et al. Barriers to access to care reported by women living with HIV across 27 countries. AIDS Care 2015;27:1220–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].INMUJERES, Public Health National Institute, Mexican women, adolescents and girls: a compassionate look to HIV/AIDS. Epidemiology, prevention, medical care and better practices in Mexico. [Google Scholar]
- [9].Romero-Gutierrez G, Delgado-Macias AA, Mora-Escobar Y, et al. Mexican women's reasons for accepting or declining HIV antibody testing in pregnancy. Midwifery 2007;23:23–7. [DOI] [PubMed] [Google Scholar]
- [10].Vera Gamboa L, Gongora Biachi RA, Pavia Ruz N, et al. Acceptability of a test for antibodies against HIV in a group of pregnant women in Yucatan, Mexico. Ginecol Obstet Mex 2005;73:355–9. [PubMed] [Google Scholar]
- [11].PAHO: PanAmerican Health Organization, Pan American Health Organization. Elimination of Mother-to-Child Transmission of HIV and Syphilis in the Americas. Update 2015. 2015. [Google Scholar]
- [12].Kendall T, van Dijk M, Wilson KS, et al. A lifetime of violence: results from an exploratory survey of Mexican women with HIV. J Assoc Nurses AIDS Care 2012;23:377–87. [DOI] [PubMed] [Google Scholar]
- [13].Martin-Onraet A, Volkow-Fernandez P, Alvarez-Wyssmann V, et al. Late diagnosis due to missed opportunities and inadequate screening strategies in HIV Infected Mexican women. AIDS Behav 2017;21:505–14. [DOI] [PubMed] [Google Scholar]
- [14].Martin-Onraët A, Alvarez-Wyssman V, Volkow-Fernandez P, et al. HIV infected women in Mexico: vulnerability, missed opportunities and late diagnosis. 20th International AIDS Conference; Melbourne, Australia, 2014. [Google Scholar]
- [15].Hirsch JS, Meneses S, Thompson B, et al. The inevitability of infidelity: sexual reputation, social geographies, and marital HIV risk in rural Mexico. Am J Public Health 2007;97:986–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Santos NJ, Barbosa RM, Pinho AA, et al. Contexts of HIV vulnerability among Brazilian women. Cad Saude Publica 2009;25(suppl 2):S321–33. [DOI] [PubMed] [Google Scholar]
- [17].Cook RL, Cook CL, Karki M, et al. Perceived benefits and negative consequences of alcohol consumption in women living with HIV: a qualitative study. BMC Public Health 2016;16:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Watt MH, Eaton LA, Choi KW, et al. “It's better for me to drink, at least the stress is going away”: perspectives on alcohol use during pregnancy among South African women attending drinking establishments. Soc Sci Med 2014;116:119–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].De Boni RB, Shepherd BE, Grinsztejn B, et al. Substance use and adherence among people living with HIV/AIDS receiving cART in Latin America. AIDS Behav 2016;20:2692–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].INEGI. Population and Habitat Census 2012. INEGI: National Institute of Statistics and Geography; 2012. [Google Scholar]
- [21].Ministry of Health, Public Health National Institute, Ministry of Health. National Survey on Violence in Women. 2003. [Google Scholar]
- [22].Jewkes RK, Dunkle K, Nduna M, et al. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet 2010;376:41–8. [DOI] [PubMed] [Google Scholar]
- [23].Gonzalez A. Poverty and gender inequalities reduce the quality of life of women living with HIV/AIDS in Chiapas, Mexico. AIDS Conference Abstract no TUPE0696; 2008. [Google Scholar]
- [24].O’Doherty L, Hegarty K, Ramsay J, et al. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev 2015. CD007007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Duffus WA, Davis HT, Byrd MD, et al. HIV testing in women: missed opportunities. J Womens Health 2012;21:170–8. [DOI] [PubMed] [Google Scholar]
- [26].Viani RM, Araneta MR, Ruiz-Calderon J, et al. Perinatal HIV counseling and rapid testing in Tijuana, Baja California, Mexico: seroprevalence and correlates of HIV infection. J Acquir Immune Defic Syndr 2006;41:87–92. [DOI] [PubMed] [Google Scholar]
- [27].Ministry of Health. Mexican official Norm for prevention and control of HIV infection, NOM-010-SSA2-2010. [Google Scholar]


