Abstract
Rationale:
Intracranial vascular atherosclerotic occlusion is one of the most common causes of ischemic stroke world wide. The involvement of large intracranial vessels, in particular, the middle cerebral artery, is usually associated with unfavorable outcomes in patients. Spontaneous recanalization of atherosclerotic occlusion is relatively rare.
Patient concerns:
The first patient was a 43-year-old male with slurred speech and left-sided weakness for a duration of 24 hours. The second was a 59-year-old male with left-sided weakness over a period of 13 hours. The last was a 49-year-old female patient presented with a 1-month history of right-sided headache.
Diagnoses:
Atherosclerotic middle cerebral artery occlusion.
Interventions:
In all cases, oral aspirin (100 mg; once daily), Plavix (75 mg; once daily), and Lipitor (40 mg; once daily) were used . Oral Plavix was stopped 3 months.
Outcomes:
Spontaneous recanalization occured in the three cases of atherosclerotic middle cerebral artery occlusion.
Lessons:
Spontaneous recanalization may occur in both early and late stages of atherosclerotic middle cerebral artery occlusion. Clinicians should be aware of this particular condition, as it may represent a relatively favorable prognosis.
Keywords: atherosclerotic occlusion, case report, middle cerebral artery, spontaneous recanalization
1. Introduction
Intracranial vascular atherosclerotic stenosis is a major contributor to the incidence of ischemic stroke worldwide.[1] Stenosis of large intracranial vessels, such as the middle cerebral artery, may result in severe neurological deficits in patients, including sensorimotor dysfunction, aphasia, hemianopia, and facial paralysis. According to published findings, outcomes of medical treatment for patients with atherosclerotic middle cerebral artery occlusion are usually unfavorable.[1,2] Annual stroke rate has been estimated to be approximately 8% to 10%.[2] It has been well characterized that pharmacological intervention with warfarin or aspirin may fail to prevent further ischemic events. In patients with acute middle cerebral artery occlusion, mainstay treatments include intravenous thrombolysis and mechanical embolectomy; nevertheless, there has yet been no effective treatment for patients who have missed the short time window for such interventions. Recently, cases with spontaneous recanalization after atherosclerotic middle cerebral artery occlusion have been reported.[3–6] To date, clinical and radiological features and, in particular, the occurrence time of spontaneous recanalization have not been well studied.
Herein, we report 3 cases with spontaneous recanalization of atherosclerotic middle cerebral artery occlusion. Symptom onset and angiographic profiles are presented, along with the possible mechanisms involved.
2. Case report
The study was approved by the Institutional Review Board and Ethics Committee of China-Japan Union Hospital of Jilin University. Informed consent was obtained from all individual participants included into the study.
2.1. Case 1
A 43-year-old male patient presented to our department with slurred speech and weakness in the left limbs for a duration of 24 hours. Physical examination showed dysarthria, shallowing of the left nasolabial fold, and muscle strength of grade 4 in the left extremities; the Babinski sign in the left side was positive. The patient admitted a history of hypertension and smoking. Brain magnetic resonance imaging (MRI) showed new-onset cerebral infarctions in the right frontoparietal lobe, the basal ganglia region, and the right temporo-occipital junction region. After admission, oral aspirin (100 mg; once daily), Plavix (75 mg; once daily), and Lipitor (40 mg; once daily) were administrated. Four days after onset, cerebrovascular digital subtraction angiography (DSA) was performed, which showed occlusion in the initiation area of the M1 segment of the left middle cerebral artery and mild stenosis in the A1 segment of the anterior cerebral artery (Fig. 1A). The pia mater branches from the right anterior cerebral artery were noted to compensate the blood supply in the distribution of the right middle cerebral artery (Fig. 1B and C). When discharged, symptoms significantly improved; slurred speech and weakness in the left limbs completely resolved. The patient was advised to continue the therapeutic regimen prescribed, including Plavix, for 3 months, as well as long-term aspirin and Lipitor. Three months later, follow-up magnetic resonance angiography (MRA) demonstrated spontaneous recanalization of the left middle cerebral artery occlusion, and severe stenosis of the M1 segment of the left middle cerebral artery was observed (Fig. 1D).
Figure 1.
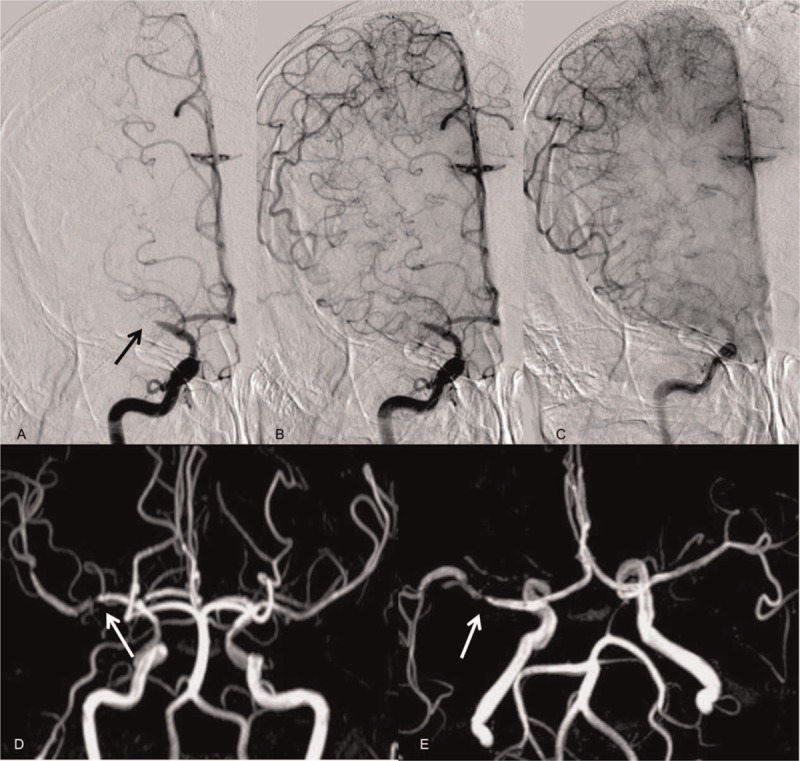
Radiological profiles of case 1. (A) Digital subtraction angiography shows occlusion in the initiation part of the M1 segment of the left middle cerebral artery (black arrow) and mild stenosis in the A1 segment of the anterior cerebral artery. (B, C) Digital subtraction angiography shows pia mater branches from the right anterior cerebral artery compensating for the blood supply in the right middle cerebral artery territory. (D, E) Repeated magnetic resonance angiography after a three month follow-up reveals spontaneous recanalization of the left middle cerebral artery occlusion, and severe stenosis of the M1 segment of the left middle cerebral artery (white arrow) is observed.
2.2. Case 2
A 59-year-old man was admitted with weakness in the left limbs over a period of 13 hours. He had a history of smoking and alcohol consumption. Physical examination showed muscle strength of grade 4 in the left extremities. Brain MRI showed new-onset cerebral infarctions in the right frontal lobe and centrum semiovale. Laboratory examination revealed hyperlipidemia. MRA showed occlusion in the initiation part of the M1 segment of the right middle cerebral artery (Fig. 2A). Perfusion weighted imaging (PWI) showed increased cerebral blood volume and cerebral blood flow in the distribution of the right middle cerebral artery, with prolongation of the mean transit time and peak-reaching time (Fig. 2B–E), indicating compensatory collateral circulation. Oral aspirin (100 mg; once daily), Plavix (75 mg; once daily), and Lipitor (40 mg; once daily) were used. One week later, follow-up computed tomography angiography (CTA) demonstrated spontaneous recanalization of the right middle cerebral artery occlusion, and severe stenosis of the M1 segment was noted (Fig. 2F). When discharged, the symptoms significantly improved; weakness in the left limbs completely resolved. The patient was advised to continue the therapeutic regimen prescribed, including Plavix, for 3 months, as well as long-term aspirin and Lipitor.
Figure 2.
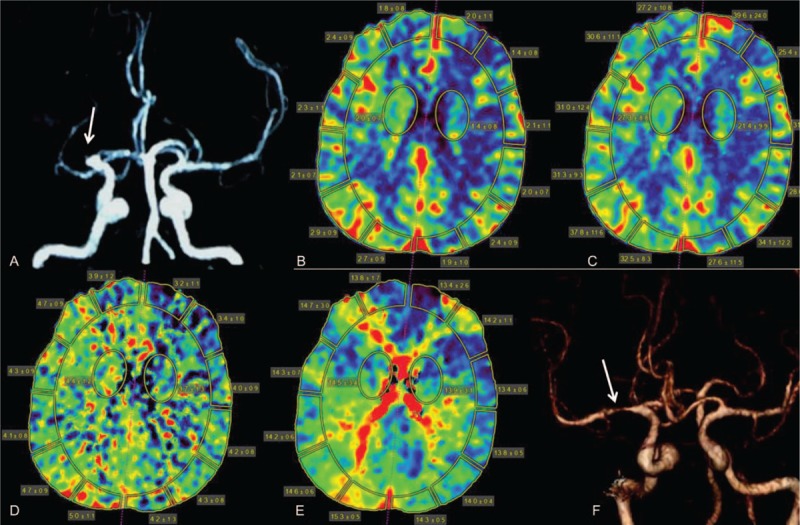
Radiological profiles of case 2. (A) Magnetic resonance angiography shows occlusion in the initiation part of the M1 segment of the right middle cerebral artery (white arrow). (B–E) Perfusion weighted images show increased cerebral blood volume (B) and cerebral blood flow (C) in the distribution of the right middle cerebral artery, whereas the mean transit time (D) and the time to peak (E) are prolonged. (F) Follow-up computed tomography angiography 1 week later demonstrates severe stenosis of the M1 segment of the right middle cerebral artery (white arrow).
2.3. Case 3
A 49-year-old female patient presented with a 1-month history of right-sided headache. She admitted a history of hypertension. Physical examination was normal. DSA showed an aneurysm in the ophthalmic segment of the right internal carotid artery, and severe stenosis of the M1 segment of the left middle cerebral artery. The aneurysm was treated with stent-assisted coiling. Further radiological evaluation of the middle cerebral artery occlusion found a remote branch was perfused and the arterial trunk was occluded (Fig. 3A). The pia mater branches from the left anterior cerebral artery provided compensatory blood supply in the left middle cerebral artery territory (Fig. 3B). Oral aspirin (100 mg; once daily), Plavix (75 mg; once daily), and Lipitor (40 mg; once daily) were used. Oral Plavix was stopped 3 months later. Four years later, repeated DSA showed no significant improvement (Fig. 3C and D). Oral aspirin and Lipitor were continued. After a follow-up period of 7 years, DSA demonstrated spontaneous recanalization of the left middle cerebral artery occlusion; the vascular wall demonstrated no evidence of depositions, and no significant stenosis was observed (Fig. 3E). There were no symptoms on follow-up, and physical examination was all normal. The patient was advised to take long-term aspirin and Lipitor.
Figure 3.
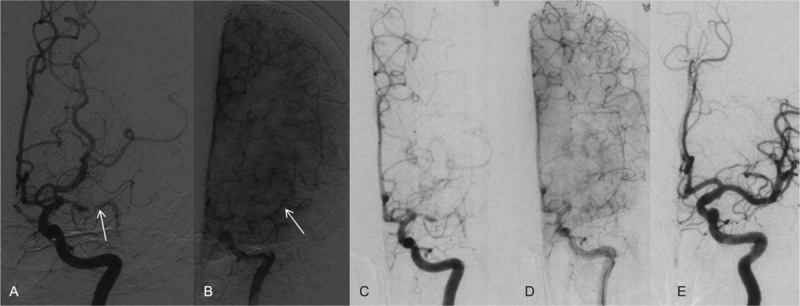
Radiological profiles of case 3. (A, B) Digital subtraction angiography shows severe stenosis in the M1 segment of the left middle cerebral artery with a remote branch perfused, whereas the arterial trunk is occluded (white arrow); pia mater branches from the left anterior cerebral artery compensate the blood supply in the left middle cerebral artery territory. (C and D) Repeat digital subtraction angiography 4 years later shows no significant improvement of the vascular occlusion. (E) After a follow-up period of 7 years, digital subtraction angiography demonstrates spontaneous recanalization of the left middle cerebral artery occlusion; the vascular wall is unobstructed, and there is no significant stenosis.
3. Discussion
Current studies related to spontaneous recanalization following vascular occlusion focus primarily on reperfusion in patients with arterial embolism and arterial dissection.[7] In previous studies, some researchers demonstrated spontaneous recanalization predominantly occurring in patients with ischemic stroke resulting from cardiogenic cerebral embolism or dissection.[3] Spontaneous recanalization in arterial dissection has been well studied, and relevant studies in literature have proposed that antiplatelet agents and anticoagulant drugs may facilitate this phenomenon.[8] A previous meta-analysis found spontaneous recanalization of occluded middle cerebral artery occurred in 21.4% of patients within 24 hours and in 52.7% of patients after a week, and also noted spontaneous recanalization was associated with an improved prognosis.[9] Ultrasonic screening in a middle cerebral artery occlusion cohort noted that the actual recanalization rate might be more optimistic than estimated.[10] Though spontaneous recanalization after atherosclerotic occlusion in internal carotid arteries and middle cerebral arteries has also been reported, in-depth studies and comprehensive descriptions regarding spontaneous recanalization after atherosclerotic middle cerebral artery occlusion are sparse.
The definitive mechanism of spontaneous recanalization following atherosclerotic occlusion is unclear. Predictive factors for the spontaneous recanalization of occluded arteries in patients with acute ischemic stroke have been investigated. Yi et al[11] found that atrial fibrillation is associated with reduced spontaneous recanalization of the occluded large or middle cerebral arteries, whereas stage 3 hypertension may be a contributor to recanalization. Buslovich and Hines[5] reported 3 cases of spontaneous recanalization of chronic internal carotid artery occlusions, 2 of which were treated with endarterectomy and postoperative histopathological examination revealed atherosclerosis. In the present study, all 3 patients suffered with hypertension and smoking histories, which are high-risk factors of atherosclerosis, and compensation of collateral circulation has been established; given the presence of severe focal areas of stenosis of the middle cerebral artery, as well as the absence of proximal embolus origin or cardiac abnormalities, a diagnosis of atherosclerosis was made. In the first case, spontaneous recanalization was observed three months after onset, namely in the acute or sub-acute phase of atherosclerotic middle cerebral artery occlusion. The second patient developed spontaneous recanalization in the acute phase (<1 week), which was confirmed by CTA scanning. Though the occluded arteries were reperfused as spontaneous recanalization occurred in the above two cases, severe stenosis remained in the focal vessels. We speculated that occlusion was induced by the activation of the coagulation system as a result of rupture of unstable atherosclerotic plaques on the basis of vascular stenosis. Additionally, acute occlusion may initiate the autologous fibrinolysis system, dissolving coagulated blood clots, leading to spontaneous recanalization in early stages. The third case had a distinctly chronic course; 4 years after onset, no improvement in arterial occlusion was noted, whereas after a 7-year follow-up, spontaneous recanalization was observed and no stenosis remained. We hypothesized that spontaneous recanalization may be because of the morphology of the thrombus and formation of new vessels, as suggested by a previously published study.[12] Lee et al[13] have reported a case with late spontaneous recanalization of chronic occluded artery; spontaneous recanalization occurred 21 months after middle cerebral artery occlusion, which was similar to our patient. However, the spontaneous recanalization in the current case was much later. Of note, collateral circulation was well established in all 3 cases. We speculated that collateral circulation compensated for the blood supply of the middle cerebral artery territory, and thus facilitated fibrinolysis, thrombus morphology, and neovascularization. In published studies, some researchers have reported that external carotid artery-intracranial artery bypass surgery can promote the spontaneous recanalization of chronic internal carotid artery occlusion, thereby improving distal blood compensation following surgery.[4] Jackson et al reported spontaneous recanalization of a middle cerebral artery occlusion with subsequent carotid endarterectomy. We suggest that clinicians should be aware of the spontaneous recanalization, and appropriate therapeutic strategies should be more accommodating to this observation.[14]
Moreover, these patients were all treated with oral antiplatelet agents and statins, which can inhibit the aggregation and stabilization of platelets, reverse the formation of atherosclerotic plaques, suppress focal inflammatory responses, and stabilize endothelial cells of blood vessels.[15] Whether the administration of these drugs had definitively positive effects on spontaneous recanalization still remains to be elucidated with a larger sample-size cohort.
To date, the most optimal therapeutic strategy for chronic middle cerebral artery stenosis or occlusion remains controversial. Treatment options include bypass surgery and interventional surgery.[16,17] Our cases provide new insight into the natural course and prognosis of atherosclerotic middle cerebral artery occlusion.
In conclusion, spontaneous recanalization may occur in both early and late stages of atherosclerotic middle cerebral artery occlusion. Clinicians should be aware of this particular condition, as it may represent a relatively favorable prognosis in such patients.
Footnotes
Abbreviations: CTA = computed tomography angiography, DSA = digital subtraction angiography, MRA = magnetic resonance angiography, MRI = magnetic resonance imaging, PWI = perfusion weighted imaging.
The authors report no conflicts of interest.
References
- [1].Chen X, Baum L, Ng HK, et al. Atherosclerotic middle cerebral artery stenosis and its risk factors: clinical and genetic risk factors. Atherosclerosis 2014;235:e114–5. [Google Scholar]
- [2].Chang YH, Hwang SK, Kwon OK. Primary angioplasty for symptomatic atherosclerotic middle cerebral artery stenosis. J Cerebrovasc Endovasc Neurosurg 2014;16:166–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Paciaroni M, Caso V, Venti M, et al. Outcome in patients with stroke associated with internal carotid artery occlusion. Cerebrovasc Dis 2005;20:108–13. [DOI] [PubMed] [Google Scholar]
- [4].Kniemeyer HW, Voshege M, Soliman A, et al. Late spontaneous recanalization of a symptomatically occluded internal carotid artery two years after extra-intracranial bypass. Case report and review of the literature. J Cardiovasc Surg (Torino) 2012;53:241–6. [PubMed] [Google Scholar]
- [5].Buslovich S, Hines GL. Spontaneous recanalization of chronic internal carotid artery occlusions: report of 3 cases. Vasc Endovascular Surg 2011;45:93–7. [DOI] [PubMed] [Google Scholar]
- [6].Baracchini C, Tonello S, Meneghetti G, et al. Neurosonographic monitoring of 105 spontaneous cervical artery dissections: a prospective study. Neurology 2010;75:1864–70. [DOI] [PubMed] [Google Scholar]
- [7].Ast G, Woimant F, Georges B, et al. Spontaneous dissection of the internal carotid artery in 68 patients. Eur J Med 1993;2:466–72. [PubMed] [Google Scholar]
- [8].Shchanitsyn IN, Maksyushina TD, Titova YI, et al. Spontaneous recanalization of chronic occlusion of the internal carotid artery. Angiol Sosud Khir 2015;21:124–35. [PubMed] [Google Scholar]
- [9].Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 2007;38:967–73. [DOI] [PubMed] [Google Scholar]
- [10].Zanette EM, Roberti C, Mancini G, et al. Spontaneous middle cerebral artery reperfusion in ischemic stroke. A follow-up study with transcranial Doppler. Stroke 1995;26:430–3. [DOI] [PubMed] [Google Scholar]
- [11].Yi X, Ge Q, Li W, et al. Predictive factors for the spontaneous recanalization of large and middle cerebral arteries after acute occlusion. J Stroke Cerebrovasc Dis 2016;25:1896. [DOI] [PubMed] [Google Scholar]
- [12].Colon GP, Deveikis JP, Dickinson LD. Revascularization of occluded internal carotid arteries by hypertrophied vasa vasorum: report of four cases. Neurosurgery 1999;45:634–7. [DOI] [PubMed] [Google Scholar]
- [13].Lee CY, Ryu CW, Koh JS, et al. Late Spontaneous Recanalization of Chronic Middle Cerebral Artery Occlusion. Neurointervention 2012;7:113–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jackson AJ, Patel A, Renwick B, et al. Spontaneous recanalization of a middle cerebral artery occlusion with subsequent carotid endarterectomy. J Vasc Surg 2009;50:1493–5. [DOI] [PubMed] [Google Scholar]
- [15].Tsai CK, Lee JT, Wu YC, et al. Spontaneous early recanalization after acute innominate artery thromboembolic occlusion secondary to abrupt aspirin and statin discontinuation: a case report. West Indian Med J 2014;63:532–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bambakidis NC, Chowdhry SA. Cerebral revascularization for ischemic disease in the 21st century. J Neurointerv Surg 2010;2:229–36. [DOI] [PubMed] [Google Scholar]
- [17].Ma N, Mo DP, Gao F, et al. Endovascular recanalization for chronic symptomatic middle cerebral artery total occlusion. J Neurointerv Surg 2013;5:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]


