Abstract
Background:
This meta-analysis aimed to perform a meta-analysis to compare the efficiency and safety between femoral nerve block (FNB) and fascia iliaca block (FIB) for postoperative pain control in patients undergoing total knee and hip arthroplasties.
Methods:
A systematic search was performed in Medline (1966-2017.05), PubMed (1966-2017.05), Embase (1980-2017.05), ScienceDirect (1985-2017.05) and the Cochrane Library. Inclusion criteria (1) Participants: Only published articles enrolling adult participants that with a diagnosis of end-stage of osteoarthritis and prepared for unilateral TKA or THA; (2) Interventions: The intervention group received FIB for postoperative pain management; (3) Comparisons: The control group was received FNB for postoperative pain control; (4) Outcomes: Visual analogue scale (VAS) scores in different periods, opioids consumption, length of stay and postoperative complications; (5) Study design: clinical randomized control trials (RCTs) were regarded as eligible in our study. Cochrane Hand book for Systematic Reviews of Interventions was used for assessment of the included studies and risk of bias was shown. Fixed/random effect model was used according to the heterogeneity tested by I2 statistic. Sensitivity analysis was conducted and publication bias was assessed. Meta-analysis was performed using Stata 11.0 software.
Results:
Five RCTs including 308 patients met the inclusion criteria. The present meta-analysis indicated that there were no significant differences between groups in terms of visual analog scale (VAS) score at 12 hours (SMD = −0.080, 95% CI: −0.306 to 0.145, P = .485), 24 hours (SMD = 0.098, 95% CI: −0.127 to 0.323, P = .393), and 48 hours (SMD = −0.001, 95% CI: −0.227 to 0.225, P = .993). No significant differences were found regarding opioid consumption at 12 hours (SMD = 0.026, 95% CI: −0.224 to 0.275, P = .840), 24 hours (SMD = 0.037, 95% CI: −0.212 to 0.286, P = .771), and 48 hours (SMD = −0.016, 95% CI: −0.265 to 0.233, P = .900). In addition, no significant increase of complications was identified between groups.
Conclusion:
There is no significant differences of VAS scores at 12-48 hour and opioids consumption at 12-48 hour between two groups following total joint arthroplasty. No increased risk of nausea, vomiting and pruritus was observed in both groups. More high-quality large RCTs with long follow-up period are necessary for proper comparisons of the efficacy and safety of FNB with FIB. The present meta-analysis exists some limitations that should be noted: (1) Only five articles were included in present meta-analysis, although all of them are recently published RCTs, the sample size are relatively small; (2) Functional outcome is an important parameter, due to the insufficiency of relevant data, we cannot perform a meta-analysis. (3) Dose and types of local anesthetics are varied, which may influence the results; (4) The duration of follow up is relatively short which leads to underestimating complications. (5) Publication bias in present meta-analysis may influence the results.
Keywords: fascia iliaca block, femoral nerve block, meta-analysis, pain control, total hip arthroplasty, total knee arthroplasty
1. Introduction
Total joint arthroplasty (TJA) are common surgical procedures for treatment of the degenerative disorders and traumatic diseases. It has been estimated that more than 700 thousand total knee arthroplasties (TKAs) and 400 thousand total hip arthroplasties (THAs) are performed annually in the United States.[1–3] However, a majority of patients often experience moderate to severe postoperative pain after TJA.[4] Postoperative pain control has a significant impact on earlier ambulation, initiation of physiotherapy, and better functional recovery.[5] In addition, effective pain control would lower the length of hospital stay and the risk of thrombotic events which improves patients’ satisfaction. Multiple analgesic strategies have been proposed including intravenous opioid, epidural analgesia, and peripheral nerve block.[6–8] Each of them has its limitations. Systemic use of opioids is associated with various adverse effects such as nausea, vomiting, pruritus, and respiratory depression which would influence rehabilitation. Patients who received epidurals had more frequent hypotension, urinary retention, and pruritus. Hypotension and urinary retention occurred more frequently in patients who received epidural analgesia. Multimodal analgesia with peripheral nerve block has been recommended and considered as gold standard for pain management in lower extremity joint arthroplasty.
Previous studies has shown that femoral nerve block (FNB) could significantly reduce pain scores and opioids consumption.[9,10] However, it was criticized for a potential injury to femoral nerve and femoral vessels. Recently, fascia iliaca block (FIB) has been proposed to avoid the complications by anesthetizing the femoral nerve remotely from major neurovascular structures, and achieve adequate analgesia.[11]
Whether FIB would be equivalent to FNB for analgesia in TJA remains unclear due to a lack of published studies and small sample sizes. Therefore, we performed the present meta-analysis from randomized controlled trials to compare the efficiency and safety between FNB and FIB for postoperative pain control. Only published articles enrolling adult participants that with a diagnosis of end-stage of osteoarthritis and prepared for unilateral TKA or THA. The intervention group received FIB for postoperative pain management. The control group was received FNB for postoperative pain control. Primary outcomes were VAS scores and opioids consumption in different periods. Secondary outcomes were length of hospital stay and postoperative complications.
2. Methods
This meta-analysis was reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
2.1. Search strategy
Potentially relevant studies were identified from electronic databases including Medline (1966–2017.05), PubMed (1966–2017.05), Embase (1980–2017.05), ScienceDirect (1985–2017.05), and the Cochrane Library. The following key words were used on combination with Boolean operators AND or OR: “total knee replacement OR arthroplasty,” “total hip replacement OR arthroplasty,” “femoral nerve block,” “fascia iliaca block,” and “pain control.” No restrictions were imposed on language. The bibliographies of retrieved trials and other relevant publications were cross-referenced to identify additional articles. The search process was performed as presented in Fig. 1.
Figure 1.
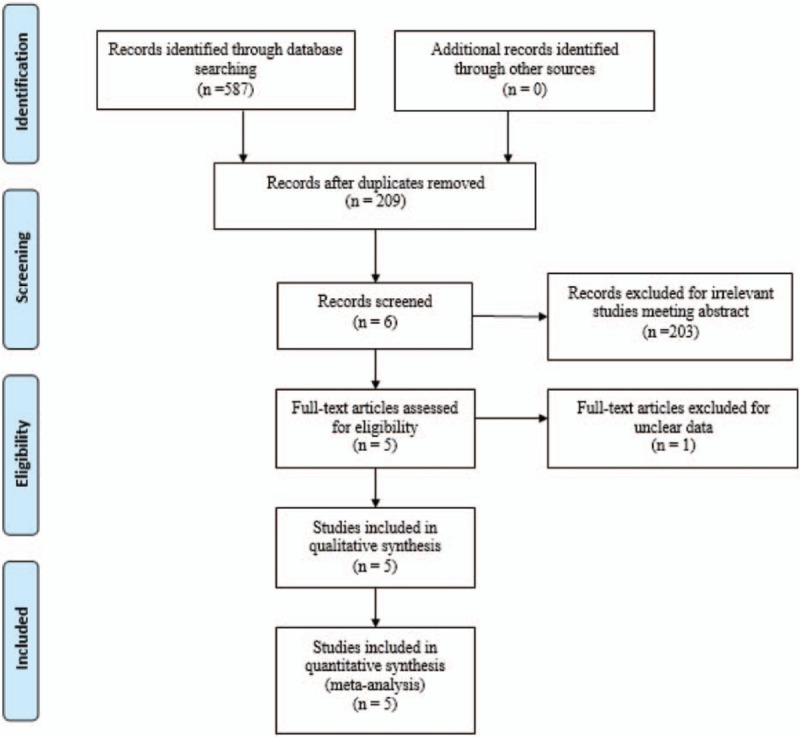
Search results and the selection procedure.
2.2. Inclusion and exclusion criteria
-
(1)
Participants: Only published articles enrolling adult participants that with a diagnosis of end-stage of osteoarthritis and prepared for unilateral TKA or THA.
-
(2)
Interventions: The intervention group received FIB for postoperative pain management.
-
(3)
Comparisons: The control group was received FNB for postoperative pain control.
-
(4)
Outcomes: Visual analog scale (VAS) scores in different periods, opioids consumption, length of stay, and postoperative complications.
-
(5)
Study design: clinical randomized control trials (RCTs) were regarded as eligible in our study.
Articles would be excluded from current meta-analysis for incomplete data, case reports, conference abstract, or review studies.
2.3. Selection criteria
Two reviewers independently scanned the abstracts of the potential articles identified by the above searches. Subsequently, the full text of the studies that met the inclusion criteria was screened, and a final decision was made. A senior author had the final decision in any case of disagreement regarding which studies to include.
2.4. Date extraction
Two of the authors independently extracted data from the included studies. Corresponding authors were consulted for details of data were incomplete. The following data were extracted and recorded in a spreadsheet: first author names, publication year, language, samples size, baseline characteristics, intervention procedures, anesthesia method, and outcome parameters. Other relevant data were also extracted from individual studies. Primary outcomes were VAS scores and opioids consumption in different periods. Secondary outcomes were length of hospital stay and postoperative complications.
2.5. Quality assessment
Quality assessment of each randomized trial was performed by 2 reviewers based on the Cochrane Handbook for Systematic Reviews of Interventions. We created a “risk of bias” table that included the following elements: random sequence generation, allocation concealment, blinding, incomplete outcome data, free of selective reporting, and other bias. Each item was recorded by “Yes,” “No,” or “Unclear.” The quality of the evidence for the main outcomes in present meta-analysis was evaluated using the Recommendations Assessment, Development and Evaluation (GRADE) system including the following items: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The recommendation level of evidence is classified into the following categories: high, which means that further research is unlikely to change confidence in the effect estimate; moderate, which means that further research is likely to significantly change confidence in the effect estimate but may change the estimate; low, which means that further research is likely to significantly change confidence in the effect estimate and to change the estimate; and very low, which means that any effect estimate is uncertain. Publication bias is a tendency on average to produce results that appear significant, because negative or near neutral results are almost never published. Publication bias may exist in all meta-analyses. Selective reporting is a strong bias that prevents correct conclusions arising from hypothesis tests, this bias is a specific form of selection bias whereby only interesting or relevant examples are cited. Therefore, the meta-analysis results should be considered appropriate. Subgroup analysis was performed for the main outcomes depending on if premedication was used.
2.6. Data analysis and statistical methods
Pooling of data was carried out using Stata 11.0 software (The Cochrane Collaboration, Oxford, United Kingdom). Statistical heterogeneity was evaluated based on the value of P and I2 using standard Chi-square test. When I2 > 50%, P < .1 was considered to be significant heterogeneity, random-effect model was used for meta-analysis. Otherwise, fixed-effect model was performed. Sensibility analysis is conducted to assess the origins of heterogeneity. The results of dichotomous outcomes (postoperative complications) were expressed as risk difference (RD) with 95% confidence intervals (CIs). For continuous various outcomes (VAS scores, opioids consumption, and length of stay), mean difference (MD) or standard mean difference (SMD) with a 95% confidence intervals (CIs) was applied for assessment. Forest plots were exported to show the pooled data and present the results of included studies.
3. Results
3.1. Search result
A total of 587 studies were identified through the initial search. Three hundred seventy-eight studies were excluded for duplication. By scanning the abstracts, 203 reports did not meet inclusion criteria and 1 paper was excluded for unclear data. No gray literature was included. Finally, 5 RCTs[12–16] published between 2010 and 2016 were included in the present meta-analysis and all studies were published in English. These studies included 152 patients in the experimental groups and 156 patients in the control groups. No gray reference was included.
3.2. Study characteristics
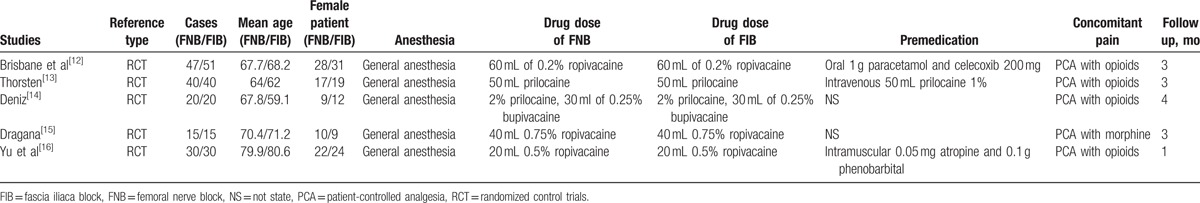
The sample size of the included studies ranged from 30 to 98. All of them compare the analgesic efficiency between FNB and FIB in total knee and hip arthroplasties. Experimental groups received FNB, while control groups received FIB. There is a variation in dosage and types of local anesthetics among articles. All patients received general anesthesia for surgery. Four articles[11–14] reported that TJAs were performed by same teams. Three studies[11,13,15] received premedication for pain relief. All participates received patient-controlled analgesia (PCA) with opioids as an adjunct concomitant pain management. None of the included articles performed a sample size calculation. All of them suggest the outcomes for at least 95% of the patients. The follow-up period ranged from 1 to 4 months (Table 1).
Table 1.
Trial characteristics.
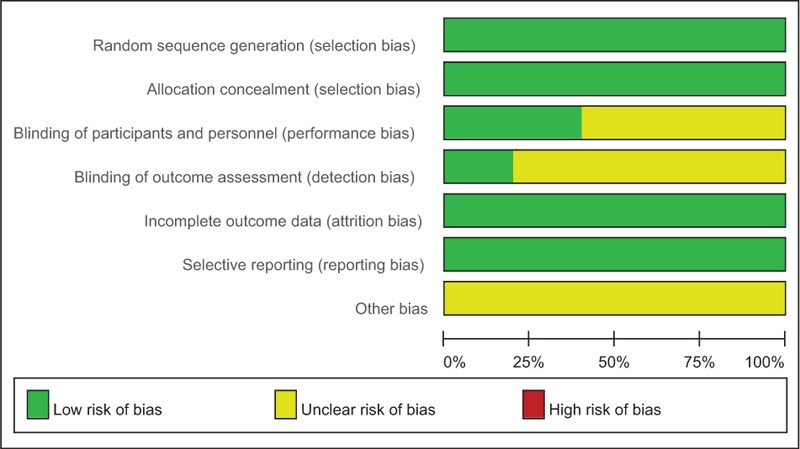
3.3. Risk of bias within studies
The Cochrane Handbook for Systematic Review of Interventions was consulted to assess risk of bias among RCTs. All RCTs provided clear inclusion and exclusion criteria and described their randomization methodology by using computer software. Five studies reported allocation concealment was achieved by sealed opaque envelopes. Double blinding was reported in 2 RCTs,[11,12] only 1[13] of the included articles attempted to blind the assessors. All RCTs provided complete outcome data. The methodological quality assessment is summarized in Table 2. Each risk of bias item is presented as the percentage across all included studies, which indicates the proportion of different levels of risk of bias for each item (Table 3).
Table 2.
Methodological quality of the randomized controlled trials.
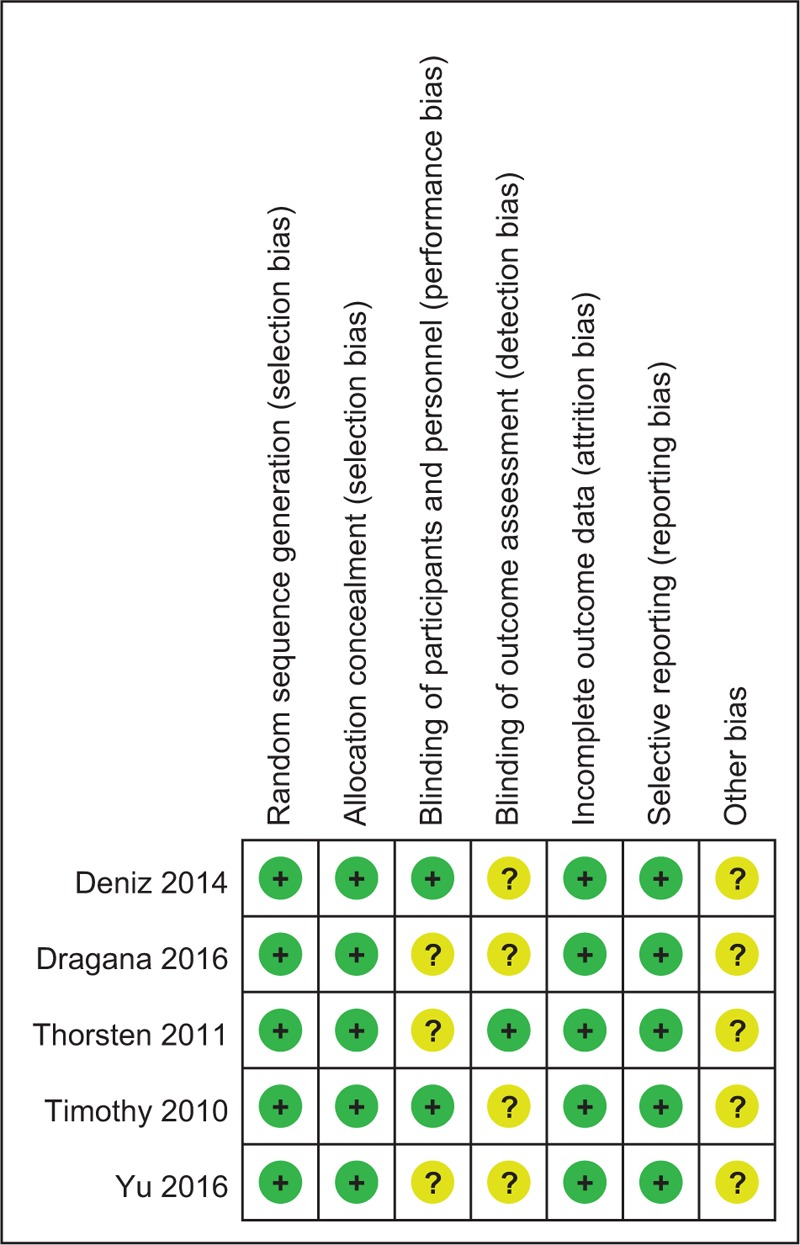
Table 3.
Risk of bias of included RCTs.
3.4. Outcomes for meta-analysis
The most interesting finding of the meta-analysis was that FNB showed similar analgesic effect compared FIB within the first 48 hours. No significant difference regarding opioids consumption and postoperative complications were identified.
3.4.1. VAS scores at 12 hours
Five articles[11–15] reported the outcomes of VAS scores at 12 hours after TJA. A random-effects model was used because significant heterogeneity was found among the studies (χ2 = 10.97, df = 4, I2 = 63.5%, P = .027). The pooled results demonstrated that no significant difference in VAS scores at 12 hours was found between 2 groups (SMD = −0.080, 95% CI: −0.306 to 0.145, P = .485; Fig. 2).
Figure 2.
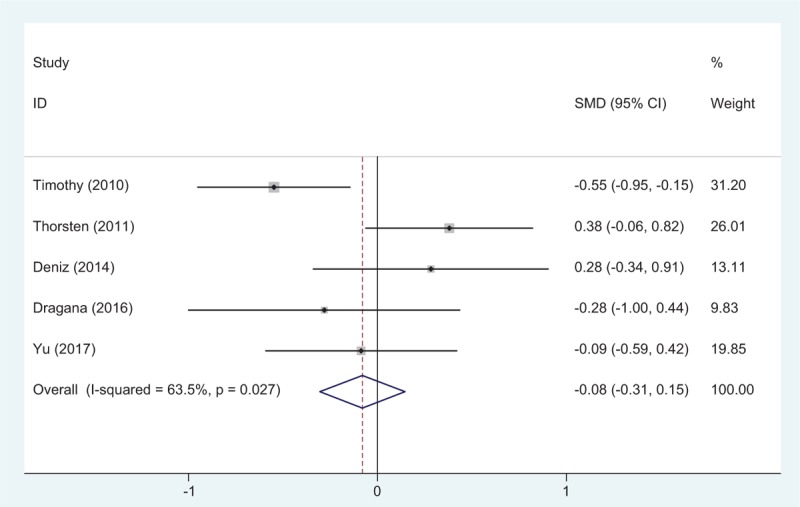
Forest plot diagram showing VAS scores at 12 hours following TJA.
3.4.2. VAS scores at 24 hours
Five studies[11–15] reported the outcomes of VAS scores at 24 hours after TJA. A fixed-effects model was used because no significant heterogeneity was found among the studies (χ2 = 5.82, df = 4, I2 = 31.3%, P = .213). The pooled results demonstrated that there was no significant difference in VAS scores at 24 hours between groups (SMD = 0.098, 95% CI: −0.127 to 0.323, P = .393; Fig. 3).
Figure 3.
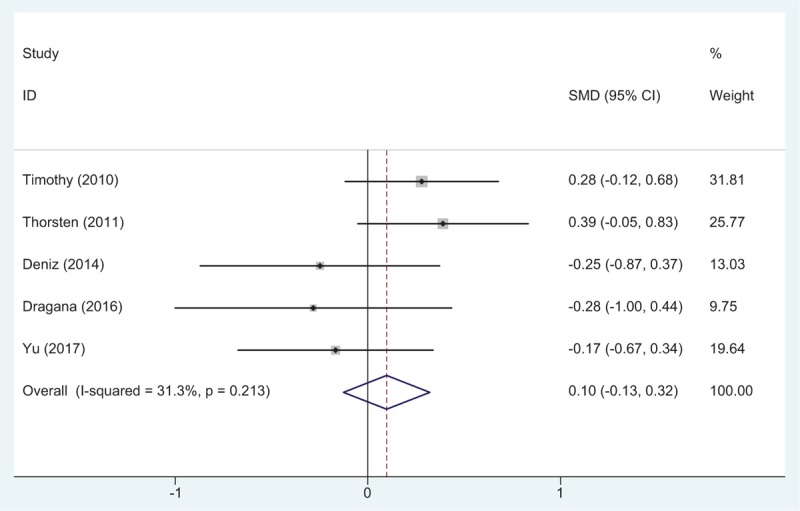
Forest plot diagram showing VAS scores at 24 hours following TJA.
3.4.3. VAS scores at 48 hours
Five studies[11–15] reported the outcomes of VAS scores at 48 hours after TJA. A random-effects model was used because significant heterogeneity existed among these studies (χ2 = 11.38, df = 4, I2 = 64.9%, P = .023). The pooled results demonstrated that no significant difference in VAS scores at 48 hours was identified between groups (SMD = −0.001, 95% CI: −0.227 to 0.225, P = .993; Fig. 4).
Figure 4.
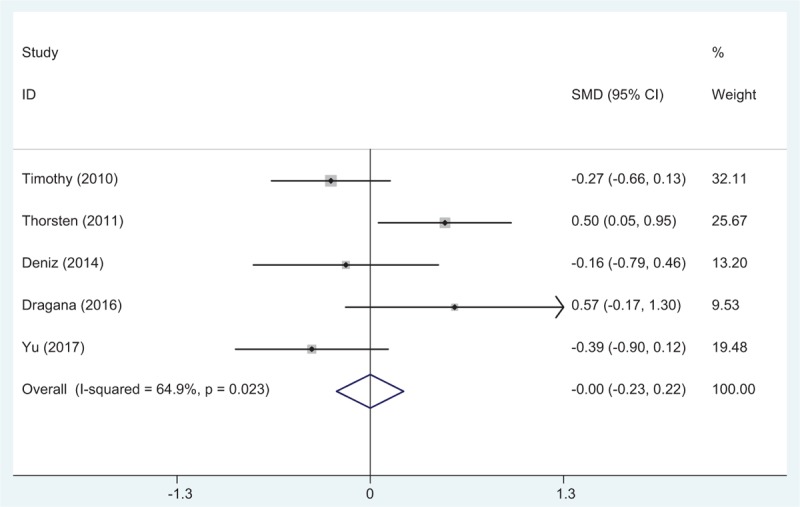
Forest plot diagram showing VAS scores at 48 hours following TJA.
3.4.4. Opioids consumption at 12 hours
Opioids consumption at 12 hours after TJA was reported in 4 articles.[11–14] A fixed-effects model was applied because no significant heterogeneity was found among these studies (χ2 = 0.35, df = 3, I2 = 0%, P = .951). No significant difference was detected in opioids consumption at 12 hours between the 2 groups (SMD = 0.026, 95% CI: −0.224 to 0.275, P = .840; Fig. 5).
Figure 5.
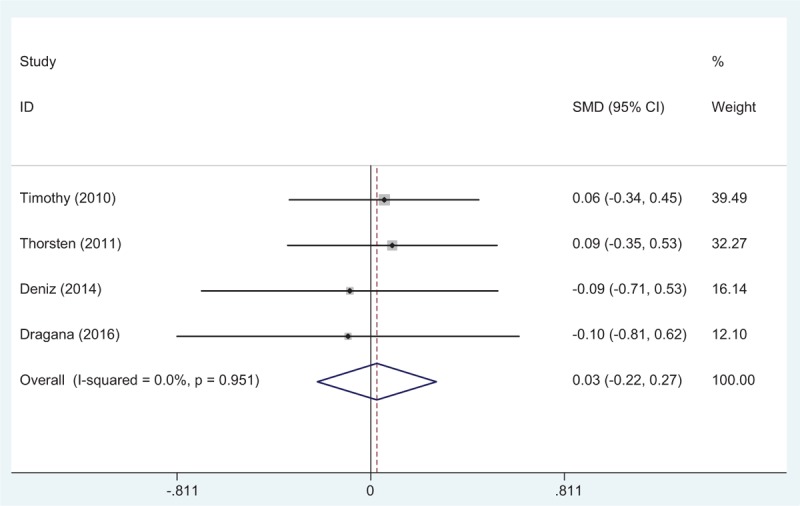
Forest plot diagram showing opioid consumption at 12 hours following TJA.
3.4.5. Opioids consumption at 24 hours
Opioids consumption at 24 hours after TJA was provided in 4 studies.[11–14] A fixed-effects model was used because no significant heterogeneity was found among these studies (χ2 = 0.56, df = 3, I2 = 0%, P = .906). The pooled results demonstrated that there was no significant difference in opioids consumption at 24 hours between groups (SMD = 0.037, 95% CI: −0.212 to 0.286, P = .771; Fig. 6).
Figure 6.
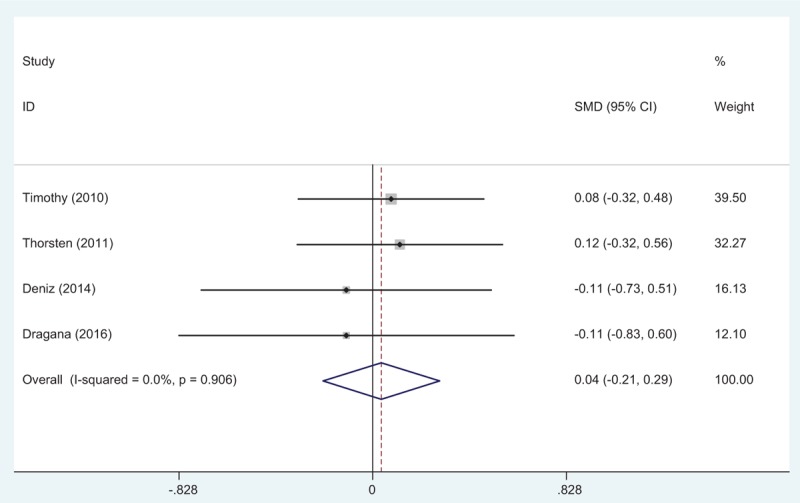
Forest plot diagram showing opioid consumption at 24 hours following TJA.
3.4.6. Opioids consumption at 48 hours
Four articles[11–14] reported the outcomes of opioids consumption at 48 hours after TJA. A fixed-effects model was used because no significant heterogeneity was found among the pooled data (χ2 = 0.61, df = 3, I2 = 0%, P = .893). No significance difference in opioids consumption at 48 hours was observed between the 2 groups. (SMD = −0.016, 95% CI: −0.265 to 0.233, P = .900; Fig. 7).
Figure 7.
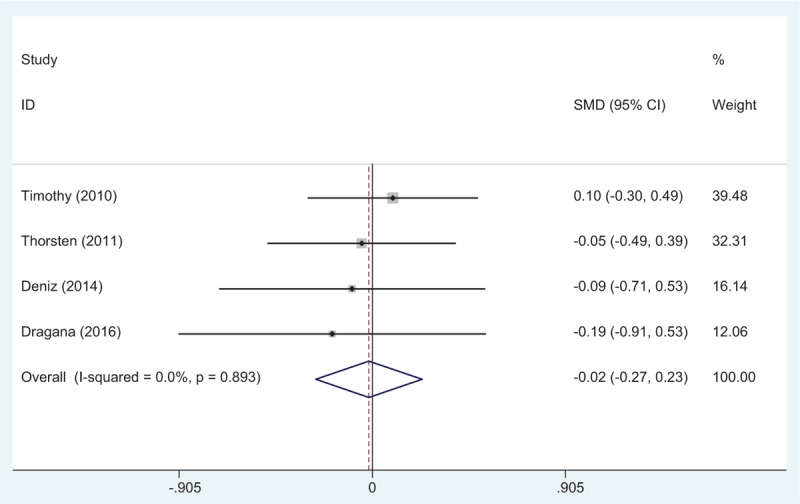
Forest plot diagram showing opioid consumption at 48 hours following TJA.
3.4.7. Length of hospital stay
Five studies[11–15] reported the length of hospital stay for the groups. A random-effects model was used because significant heterogeneity was identified in the pooled results (χ2 = 18.83, df = 4, I2 = 78.8%, P = .001). No significant difference in the length of hospital stay was observed between the 2 groups (SMD = −0.044, 95% CI: −0.271 to 0.183, P = .705; Fig. 8).
Figure 8.
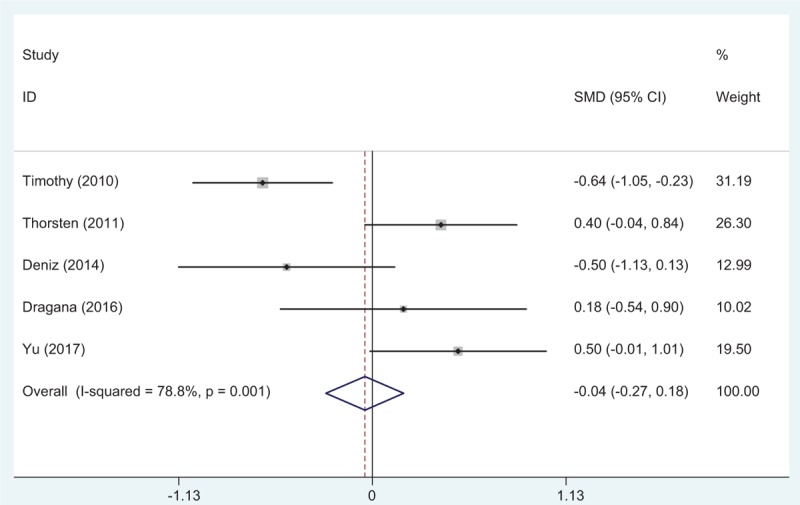
Forest plot diagram showing length of hospital stay following TJA.
3.4.8. Nausea and vomiting
Five studies[11–15] reported the postoperative complications of nausea and vomiting. A fixed-effects model was used because no significant heterogeneity was found among these studies (χ2 = 4.01, df = 4, I2 = 0.3%, P = .405). No significant difference in the incidence of nausea and vomiting was found between the 2 groups (RD = −0.001, 95% CI: −0.102 to 0.100, P = .986; Fig. 9).
Figure 9.
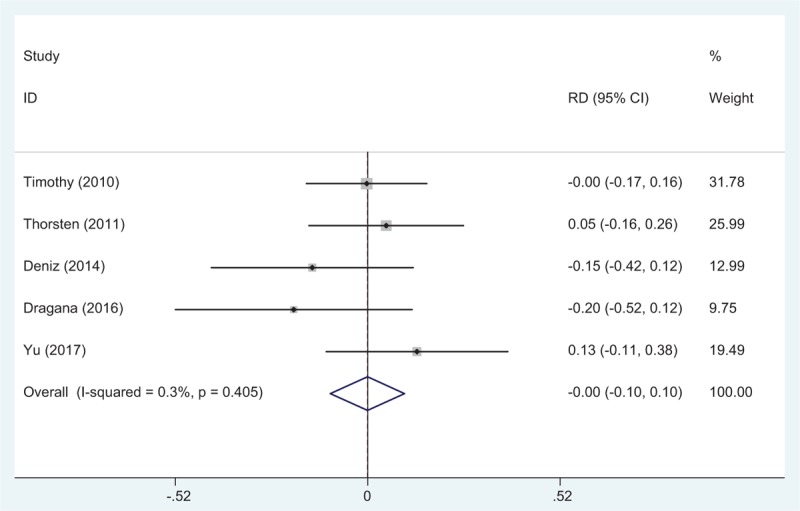
Forest plot diagram showing the incidence of nausea and vomiting following TJA.
3.4.9. Pruritus
Four articles[11–15] reported the incidence of pruritus following TJA. A fixed-effects model was used due to the low significant heterogeneity among these studies (χ2 = 1.10, df = 3, I2 = 0%, P = .777). No significant difference was found in terms of the incidence of pruritus between the groups (RD = 0.026, 95% CI: −0.041 to 0.094, P = .448; Fig. 10).
Figure 10.
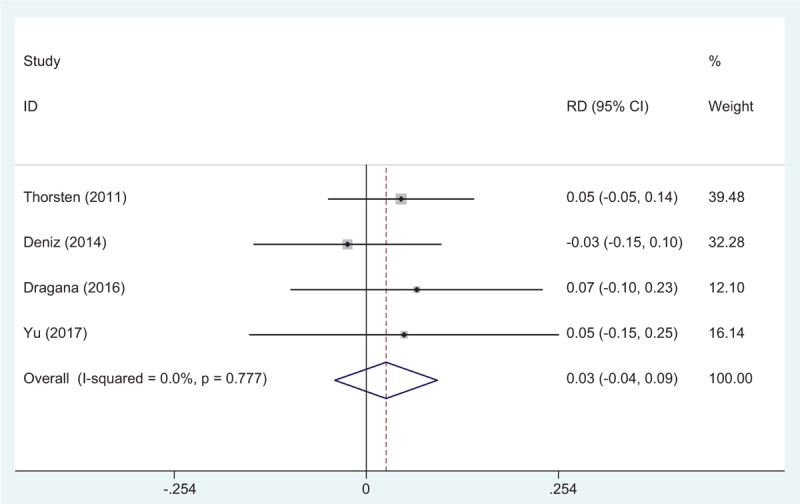
Forest plot diagram showing the incidence of pruritus following TJA.
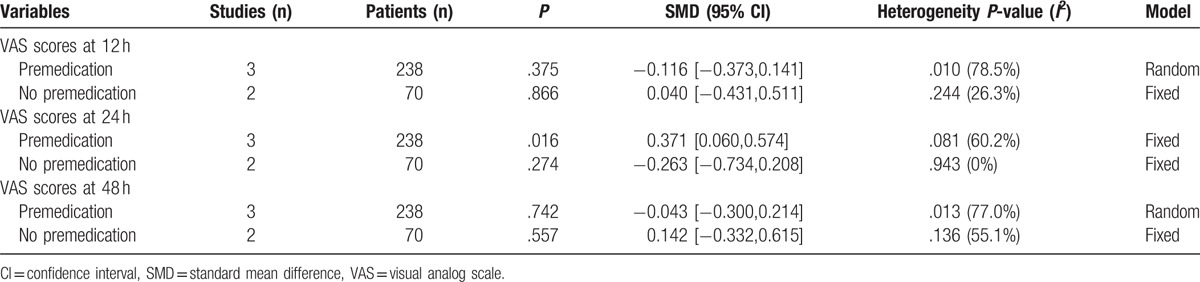
3.4.10. Publication bias and subgroup analysis
Publication bias was tested for the outcome of VAS scores at 24 hours after TJA (Fig. 11). Funnel plots were symmetrical and low risk of publication bias was showed. However, we cannot eliminate publication bias as the reliability of this evaluation strategy was weak especially when a small number of articles were enrolled. Subgroup analysis is presented in Table 4.
Figure 11.
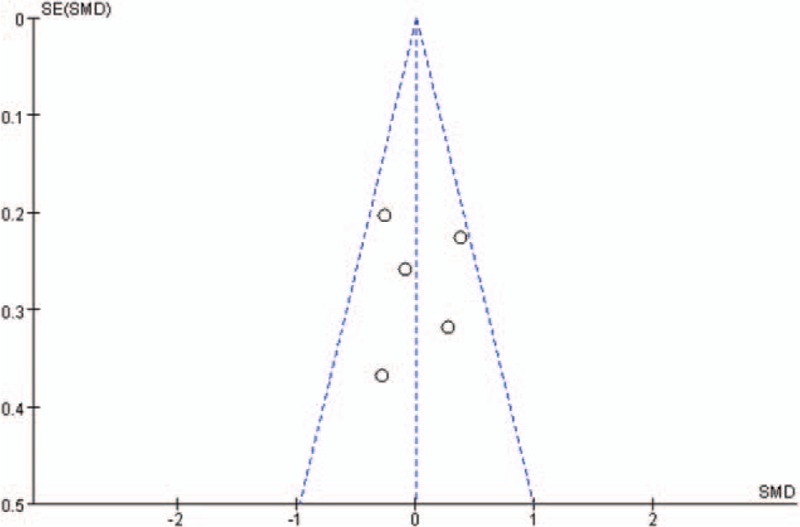
Funnel plot of VAS score at 24 hours.
Table 4.
Outcome of subgroup analysis for main results.
3.4.11. Evidence level
All main outcomes in this meta-analysis were evaluated using the GRADE system (Table 5).
Table 5.
The GRADE evidence quality for main outcome.
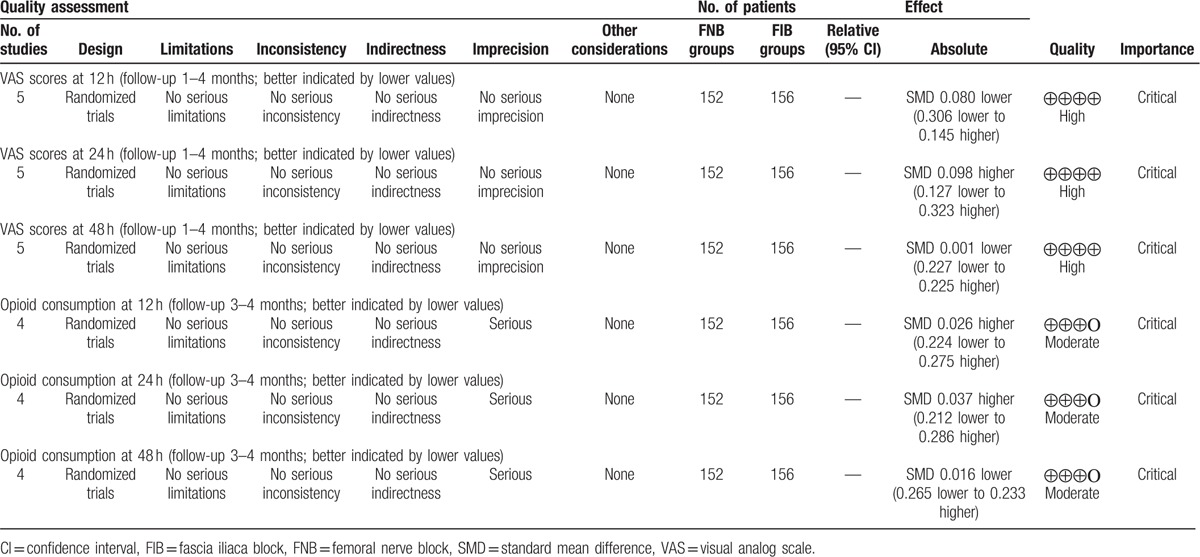
The overall evidence quality for each outcome was high to moderate.
4. Discussion
The overall evidence of the present meta-analysis was high to moderate (Table 5) which means that further research is likely to significantly change confidence in the effect estimate and may change the estimate. To the best of our knowledge, this study is the first meta-analysis from RCTs to compare the efficiency and safety between FNB and FIB for pain management after TJA. The most interesting finding of the meta-analysis was that FNB showed similar analgesic effect compared FIB. No significant difference regarding opioids consumption and postoperative complications were identified.
With the aging population, TJA was frequently performed in patient who suffers knee and hip osteoarthritis and there has been a general uptrend by the year. However, pain control following TJA can be very problematic. Optimal analgesia may achieve early functional recovery and shorten hospital stays resulting in decreased risks of thrombotic events. Postoperative pain control is an interesting topic in orthopedic surgery and still remains controversial.
Regional anesthesia and analgesia is more and more popular and showed superior in reducing neurotoxic effects, medical costs compared general anesthesia.[17,18] Furthermore, it can be performed unilaterally and cardiovascular parameters are more stable. Multimodal techniques featuring peripheral nerve blocks have demonstrated superior efficacy for pain relief in TJA. Although nerve block is not completely sufficient in pain relief for TJA, it can significantly relieve pain with less morphine consumption. Published articles have shown its many advantages in reducing postoperative pain. Hadzic et al[3] demonstrated that FNB resulted in modestly lower pain scores and reduced opioid requirements without increasing the incidence of adverse events after TKA. Moreover, FNB has previously found to be superior compared PCA administrated opioids. However, some articles has criticized that there was a potential risk of femoral nerve injury which led to a weakness in the quadriceps muscles and subsequently resulting in an increased risk of postoperative falls.[19,20]
Recently, FIB has also showed effectiveness in pain management by anesthetizing the femoral nerve remotely from important neurovascular structures in lower extremity surgery and could avoid neurologic damage complications. It was considered as an alternative choice for pain management especially in children. Zhang et al[21] performed a meta-analysis from RCTs and suggest that the application of FIB could significantly reduce VAS scores and morphine consumption within the first 24 hours compared placebo following TJA. In addition, there were fewer adverse effects in FIB groups. In the present meta-analysis, both FNB and FIB were effectiveness in pain control and there was no significant difference in VAS scores within the first 48 hours following TJA. However, based on the current data available, we cannot compare the neurologic damage complications between groups and large sample of RCTs were required for further investigation.
It was reported that there was approximately 30% to 60% of patients who suffered moderate to severe pain in the first 2 days following TJA.[22,23] Additional opioids were used as an adjunct to concomitant pain control. The personal control aspect of PCA and the rapid onset were preferred by patients. Numerous articles have reported that the application of PCA device was associated with a high level of patients’ satisfaction.[24,25] In our study, opioid consumption was considered as an objective means to measure pain. Morphine-related adverse effects including nausea, vomiting, respiratory depression, and pruritus were well known and drew our attention. Besides the side effects, drug dependence is also an important issue related to opioid administration that should be considered. It was crucial to minimize the opioid consumption for patients and improve their recovery and satisfaction. The use of local anesthetic nerve block has been recommended by the UK National Institute of Health and Care Excellence as part of an opioid sparing strategy.[26] Currently, FNB versus FIB in reducing opioids consumption remains controversial. Newman et al[27] reported that patients with femoral neck fracture receiving a FNB required less morphine after the block than those receiving fascia iliaca compartment block. While, Reavley et al[28] showed equivalent opioids consumption in adult neck of femur fractures between treatment groups. The present meta-analysis indicated that both FNB and FIB could significantly minimize opioids consumption and no significant difference was identified.
Analgesia efficacy is not the only concern when comparing 2 kinds of strategies. Nausea and vomiting are known adverse effects that are frequently associated with PCA opioids. Decreased morphine consumption can subsequently avoid such complications effectively. The overall incidence of nausea and vomiting was 46/152 in FNB groups compared 47/156 in FIB groups. No significant difference was found regarding postoperative complications. Due to the small number of included articles, large sample sizes of high quality RCTs are further needed.
Although, further evidence of the clinical benefits and cost effectiveness of FNB versus with FNB is required, the current data support that both of them could reduce pain and opioid consumptions. For clinicians, owing to the quality of evidence, the current data support the either FIB or FNB was performed for the management of postoperative pain. For policymakers, the current data do not permit firm estimates of the size of the effect owing to the low number of studies in the analysis. For patients, both FIB and FNB could significantly reduce pain, morphine consumption, and adverse effects. Furthers studies should be focused on surgeries that are known to be associated with significant postoperative pain, particularly surgeries where improved pain control may deliver significant clinical benefits through reduced morbidity, or cost-effectiveness benefits through faster rehabilitation and discharge.
The present meta-analysis exists some limitations that should be noted. Only 5 articles were included in present meta-analysis, although all of them are recently published RCTs, the sample size are relatively small; functional outcome is an important parameter, due to the insufficiency of relevant data, we cannot perform a meta-analysis. Dose and types of local anesthetics are varied, which may influence the results; the duration of follow up is relatively short which leads to underestimating complications. Publication bias in present meta-analysis may influence the results.
Despite the limitations above, this is the first meta-analysis from RCTs to compare the efficiency and safety between FNB and FIB for postoperative pain control in patients undergoing total knee and hip arthroplasties. Due to the quality of the evidence currently available, high quality RCTs are required.
5. Conclusion
FNB provides equal postoperative pain control compared with FIB following total joint arthroplasty. Both of them can reduce the consumption of opioids without severe adverse effects. More high-quality large RCTs with long follow-up period are necessary for proper comparisons of the efficacy and safety of FNB with FIB.
Footnotes
Abbreviations: FIB = fascia iliaca block, FNB = femoral nerve block, RCTs = randomized controlled trials, THA = total hip arthroplasty, TKA = total knee arthroplasty.
Authors’ contributions: YS conceived the design of the study. XH and LW performed and collected the data and contributed to the design of the study. XW finished the manuscript. All authors read and approved the final manuscript.
The authors have no conflicts of interest to disclose.
Xin Wang and Yuan Sun equally contributed to this study.
References
- [1].Li JF, Li H, Zhao H, et al. Combined use of intravenous and topical versus intravenous tranexamic acid in primary total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. J Orthop Surg Res 2017;12:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Petis SM, Howard JL, Lanting BA, et al. In-hospital cost analysis of total hip arthroplasty: does surgical approach matter? J Arthroplasty 2016;31:53–8. [DOI] [PubMed] [Google Scholar]
- [3].Hadzic A, Houle TT, Capdevila X, et al. Femoral nerve block for analgesia in patients having knee arthroplasty. Anesthesiology 2010;113:1014–5. [DOI] [PubMed] [Google Scholar]
- [4].Singelyn FJ, Ferrant T, Malisse MF, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med 2005;30:452–7. [DOI] [PubMed] [Google Scholar]
- [5].Duellman TJ, Gaffigan C, Milbrandt JC, et al. Multi-modal, pre-emptive analgesia decreases the length of hospital stay following total joint arthroplasty. Orthopedics 2009;32:167. [PubMed] [Google Scholar]
- [6].Bendtsen TF, Moriggl B, Chan V, et al. The optimal analgesic block for total knee arthroplasty. Reg Anesth Pain Med 2016;41:711–9. [DOI] [PubMed] [Google Scholar]
- [7].Looke TD, Kluth CT. Effect of preoperative intravenous methocarbamol and intravenous acetaminophen on opioid use after primary total hip and knee replacement. Orthopedics 2013;36(2 suppl):25–32. [DOI] [PubMed] [Google Scholar]
- [8].Liu SS, Bae JJ, Bieltz M, et al. A prospective survey of patient-controlled epidural analgesia with bupivacaine and clonidine after total hip replacement: a pre- and postchange comparison with bupivacaine and hydromorphone in 1,000 patients. Anesth Analg 2011;113:1213–7. [DOI] [PubMed] [Google Scholar]
- [9].Deng LQ, Hou LN, Song FX, et al. Effect of pre-emptive analgesia by continuous femoral nerve block on early postoperative cognitive function following total knee arthroplasty in elderly patients. Exp Ther Med 2017;13:1592–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Stebler K, Martin R, Kirkham KR, et al. Electrophysiological study of femoral nerve function after a continuous femoral nerve block for anterior cruciate ligament reconstruction. Am J Sports Med 2017;45:578–83. [DOI] [PubMed] [Google Scholar]
- [11].Bali C, Ozmete O, Eker HE, et al. Postoperative analgesic efficacy of fascia iliaca block versus periarticular injection for total knee arthroplasty. J Clin Anesth 2016;35:404–10. [DOI] [PubMed] [Google Scholar]
- [12].McMeniman TJ, McMeniman PJ, et al. Brisbane Orthopaedic & Sports Medicine Centre Writing Committee. Femoral nerve block vs fascia iliaca block for total knee arthroplasty postoperative pain control: a prospective, randomized controlled trial. J Arthroplasty 2010;25:1246–9. [DOI] [PubMed] [Google Scholar]
- [13].Möller T. A Randomized and Observer Blinded Comparison of Continuous Femoral Block and Fascia Iliaca Compartment Block in Hip Replacement Surgery. Journal of Anesthesia & Clinical Research 2013;4: [Google Scholar]
- [14].Deniz S, Kurt E. Comparison of the postoperative analgesic efficacy of an ultrasound-guided fascia iliaca compartment block versus 3 in 1 block in hip prosthesis surgery. Agri 2014;26:151–7. [DOI] [PubMed] [Google Scholar]
- [15].Lončar-Stojiljković D, Stojiljković MP, Golijanin R, et al. Comparative postoperative analgesia with femoral nerve block ‘3-in-1’ and with fascia iliaca compartment nerve block after hip alloarthroplasty. Vojnosanit Pregl 2016;50:12–6. [Google Scholar]
- [16].Yu B, He M, Cai GY, et al. Ultrasound-guided continuous femoral nerve block vs continuous fascia iliaca compartment block for hip replacement in the elderly: a randomized controlled clinical trial (CONSORT). Medicine 2016;95:e5056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Macrinici GI, Murphy C, Christman L, et al. Prospective, double-blind, randomized study to evaluate single-injection adductor canal nerve block versus femoral nerve block: postoperative functional outcomes after total knee arthroplasty. Reg Anesth Pain Med 2017;42:10–6. [DOI] [PubMed] [Google Scholar]
- [18].Zhang Y, Lu M, Chang C. Local anesthetic infusion pump for pain management following total knee arthroplasty: a meta-analysis. BMC Musculoskelet Disord 2017;18:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Foisy K. Thou shalt not fall! Decreasing falls in the postoperative orthopedic patient with a femoral nerve block. Medsurg Nurs 2013;22:246–9. [PubMed] [Google Scholar]
- [20].Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Reg Anesth Pain Med 2013;38:321–5. [DOI] [PubMed] [Google Scholar]
- [21].Zhang P, Li J, Song Y, et al. The efficiency and safety of fascia iliaca block for pain control after total joint arthroplasty: a meta-analysis. Medicine 2017;96:e6592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Rajeev A, Tumia N, Karn K, et al. Postoperative pain relief and functional outcome following total knee arthroplasty—a prospective comparative audit of three analgesic regimes. Acta Orthop Belg 2016;82:265–70. [PubMed] [Google Scholar]
- [23].Sporer SM, Rogers T. Postoperative pain management after primary total knee arthroplasty: the value of liposomal bupivacaine. J Arthroplasty 2016;31:2603–7. [DOI] [PubMed] [Google Scholar]
- [24].Hall MJ, Dixon SM, Bracey M, et al. A randomized controlled trial of postoperative analgesia following total knee replacement: transdermal fentanyl patches versus patient controlled analgesia (PCA). Eur J Orthop Surg Traumatol 2015;25:1073–9. [DOI] [PubMed] [Google Scholar]
- [25].Singelyn FJ, Gouverneur JM. Postoperative analgesia after total hip arthroplasty: i.v. PCA with morphine, patient-controlled epidural analgesia, or continuous “3-in-1” block?: a prospective evaluation by our acute pain service in more than 1,300 patients. J Clin Anesth 1999;11:550–4. [DOI] [PubMed] [Google Scholar]
- [26].Chesters A, Atkinson P. Fascia iliaca block for pain relief from proximal femoral fracture in the emergency department: a review of the literature. Emerg Med J 2014;31:e84–7. [DOI] [PubMed] [Google Scholar]
- [27].Newman B, McCarthy L, Thomas PW, et al. A comparison of pre-operative nerve stimulator-guided femoral nerve block and fascia iliaca compartment block in patients with a femoral neck fracture. Anaesthesia 2013;68:899–903. [DOI] [PubMed] [Google Scholar]
- [28].Reavley P, Montgomery AA, Smith JE, et al. Randomised trial of the fascia iliaca block versus the ‘3-in-1’ block for femoral neck fractures in the emergency department. Emerg Med J 2015;32:685–9. [DOI] [PubMed] [Google Scholar]


