Abstract
Diagnosis is one of the most important tasks performed by primary care physicians. The World Health Organization (WHO) recently prioritized patient safety areas in primary care, and included diagnostic errors as a high-priority problem. In addition, a recent report from the Institute of Medicine in the USA, ‘Improving Diagnosis in Health Care’, concluded that most people will likely experience a diagnostic error in their lifetime. In this narrative review, we discuss the global significance, burden and contributory factors related to diagnostic errors in primary care. We synthesize available literature to discuss the types of presenting symptoms and conditions most commonly affected. We then summarize interventions based on available data and suggest next steps to reduce the global burden of diagnostic errors. Research suggests that we are unlikely to find a ‘magic bullet’ and confirms the need for a multifaceted approach to understand and address the many systems and cognitive issues involved in diagnostic error. Because errors involve many common conditions and are prevalent across all countries, the WHO’s leadership at a global level will be instrumental to address the problem. Based on our review, we recommend that the WHO consider bringing together primary care leaders, practicing frontline clinicians, safety experts, policymakers, the health IT community, medical education and accreditation organizations, researchers from multiple disciplines, patient advocates, and funding bodies among others, to address the many common challenges and opportunities to reduce diagnostic error. This could lead to prioritization of practice changes needed to improve primary care as well as setting research priorities for intervention development to reduce diagnostic error.
Keywords: Diagnostic errors, Patient safety, Primary care, Health policy, Information technology
Introduction
Diagnosis is one of the most important tasks performed by primary care physicians (PCPs). The World Health Organization (WHO) recently prioritised safety areas in primary care and recognised the importance of errors in diagnosis.1 Recognising the paucity of literature,2–4 WHO set up a Safer Primary Care Expert Working Group to compile key lessons and topics for further research. This initiative led to the development of the 2016 Technical Series on Safer Primary Care, a series of 9 monographs to promote good practices and to implement systems changes to improve safety. This narrative review informed the development of the monograph focused on diagnostic errors, expected to be released by WHO in late 2016.
For multiple reasons, diagnosis in primary care (ie, first-contact, accessible, continued, comprehensive and coordinated care)5 represents a high-risk area for errors. PCPs typically face high patient volumes and make decisions amid uncertainty.6 Undifferentiated presenting features are the norm for diseases common in primary care, which tend to be benign and self-limiting, as well as uncommon diseases, which tend to be serious and life threatening. Diagnosis typically unfolds over time and across several episodes of care.7 8 PCPs need to carefully balance the risk of missing serious illness with the wise use of often scarce and costly referral and testing resources. Thus, diagnostic errors leading to patient harm from wrong or delayed testing or treatment have emerged as a global safety priority.9
Defining diagnostic errors
A diagnostic error occurs when a patient's diagnosis is missed altogether, inappropriately delayed and/or wrong, as judged by the eventual appreciation of definitive information10 but these categories of missed, delayed and wrong overlap extensively. For example, the following scenarios could involve an error in colorectal cancer diagnosis. The diagnoses can be considered ‘missed’ (cancer missed at three different primary care visits despite alarming symptoms), ‘wrong’ (patient told they have haemorrhoids at these visits but actually have cancer) or ‘delayed’ (patient had an abnormal laboratory test result, such as iron deficiency anaemia, suggestive of cancer but no one reviewed the results or notified the patient). But it is often hard to distinguish between the three; for example, in both missed and wrong scenarios, diagnosis was also delayed. Thus, these concepts have to be applied in concert to gain situational understanding. The evolution of diagnoses over time often makes it challenging to pinpoint a diagnostic error and operationalise diagnostic error definitions and measurements. The diagnostic process can also extend across multiple providers and in different locations. Moreover, there are no clear guidelines for ‘timely’ diagnosis for majority of conditions.11
Recent work has framed the diagnostic process along five process dimensions all of which must be considered in understanding diagnostic error.12 These dimensions include (1) the patient-provider encounter (history, exam, ordering tests/referrals based on appropriate assessment); (2) performance and interpretation of diagnostic tests; (3) follow-up and tracking of diagnostic information (such as abnormal tests) over time; (4) subspecialty and referral-related communication and coordination issues; and (5) patient behaviours, adherence and engagement. All five process dimensions are vulnerable to breakdowns in primary care, and sometimes more than one dimension is involved in an error.13–16
A recent Institute of Medicine (IOM) report ‘Improving Diagnosis in Health Care’ defines a diagnostic error as a “failure to establish an accurate and timely explanation of the patient's health problem or communicate that explanation to the patient.”14 Other formal definitions of diagnostic error have also been previously proposed.10 17 18 However, in this paper, we contextualise errors as missed opportunities that could be used to promote learning and improvement versus assigning blame or responsibility to a single clinician.18 The concept of missed opportunities also implies that something different could be done to prevent the error.
Three criteria should be considered when defining preventable diagnostic errors.12 19–22 First, an error should only be designated when case analysis reveals evidence of a missed opportunity to make a correct or timely diagnosis, that is, something different could have been done to make the correct diagnosis earlier.18 Such missed opportunities may result from individual cognitive or system-related factors, or more commonly interplay of both, or infrequently from more blatant factors such as lapses in accountability. Second, the missed opportunity is framed within the context of an ‘evolving’ diagnostic process such that error determination depends on the temporal or sequential context of events. This would imply that there is evidence of omission (failure to do the right thing) or commission (doing something wrong) at the particular point in time at which the ‘error’ occurred. Third, the opportunity could be missed by the provider, care team, system and/or patient.
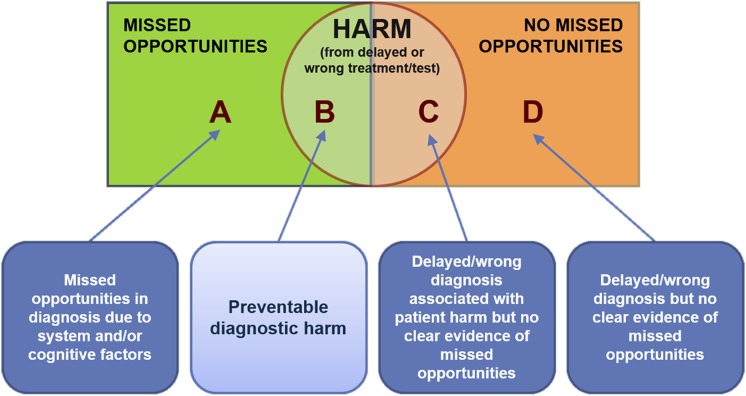
A preventable error or delay in diagnosis may occur due to factors outside a single clinician's immediate control.3 Studies of diagnostic errors often involve some degree of hindsight bias—a type of bias in judgement about a diagnosis coloured by retrospective knowledge where earlier warning symptoms and signs are later found to be either overlooked or not considered seriously yet were less obvious when at the time of the actual encounter.23 Not all delayed/wrong diagnoses are accompanied by evidence of missed opportunities (areas C and D in conceptual model, figure 1) and not all missed opportunities are harmful (area A). Although the goal is to focus on preventable diagnostic harm (area B), this will require learning from all types of diagnostic error.
Figure 1.
Relationships between diagnostic errors, missed opportunities and patient harm (adapted from Singh H).18
Epidemiology of diagnostic errors
A recent study estimated that about 5% of US adult patients experience diagnostic errors (defined as missed opportunities to make a correct or timely diagnosis or area A in Figure 1) in outpatient settings every year.24 Over half of these included the possibility of harm (area B). This was likely an underestimate, and it is unclear whether this rate would be similar in primary care in other countries, where data are generally lacking. Current US estimates are based on studies from integrated health systems using electronic health records that facilitate access to diagnostic data. A cross-sectional study of 12 primary care clinics in Malaysia reported a prevalence of errors of 3.6% (95% CI 2.2 to 5.0).25 While not representative of prevalence, in large studies of outpatient malpractice claims, diagnostic errors emerge as the most common category.26 27 Additional literature demonstrates evidence of diagnostic errors in primary care.28 29 The frequency of diagnostic error in paediatrics is unknown. However, a survey of US paediatricians found that more than half reported making a diagnostic error at least once or twice a month, and that they made harmful errors at least once or twice a year.30 Based on the available data, the IOM report ‘Improving Diagnosis in Health Care’ concluded that most people will likely have a diagnostic error in their lifetime.14
Diagnostic errors often reflect healthcare system complexities and vulnerabilities. In low-and-middle-income countries (LMICs; gross national income per capita below US$12 736),31 32 diagnosis poses even greater challenges as the process is further complicated by limited access to care and diagnostic testing resources, a paucity of qualified primary care providers and sometimes of specialists, and pre-electronic record-keeping systems. These factors likely suggest a higher rate of diagnostic errors in such settings compared with high-resource settings, though evidence for this is scarce (table 1).33 34 While access to primary care or specialists and limited availability of health professionals and diagnostic tests might lead to underdiagnosis in LMICs, high-resource settings might also be more prone to overdiagnosis because sophisticated imaging and laboratory testing, and subspecialty consultation, are all more accessible and there is greater concern about malpractice liability if a diagnosis is missed.
Table 1.
Factors that predispose to diagnostic errors in primary care settings
| Factors | Ideal circumstances | Problems contributing to error |
|---|---|---|
| Access to high-quality primary care | Universal access without significant geographic, financial barriers | Limited access due to lack of money, remoteness, illiteracy, travel constraints or limited number of healthcare facilities |
| Availability of healthcare professionals | Sufficient range and number of healthcare professionals who contribute to the primary care team | Lack of sufficient healthcare professionals perhaps due to lack of training, outward migration or poor employment situation |
| Access to specialists | Specialists immediately available in person (or remotely through telemedicine) for expert assessment | Specialty expertise may not exist, or may be limited in number or quality |
| Diagnostic tests | Full range of appropriate diagnostic modalities (eg, imaging, laboratory tests) available when needed/appropriate | Diagnostic tests limited in scope, availability or quality as well as failure to interpret tests correctly |
| Communication | Patients and providers communicate efficiently; consultation and test results exchanged reliably and in timely fashion | Little or no sharing of medical information |
| Care coordination | Coordinated care facilitates available; accurate and efficient evaluation | Consultations are delayed; test results are lost, lack of health records to document care |
| Follow-up | Diagnosis enhanced by being able to follow symptom evolution; diagnostic errors are detected and errors ameliorated | Limited follow-up and discontinuities degrade the ability for diagnostic impressions to evolve |
| Affordability of care | All needed care is affordable and/or covered by insurance | Care unaffordable, or compromises other basic needs such as food or housing |
| Training of healthcare professionals | Physicians, nurses and all professional staff are well trained. Certification and licensure requirements ensure competency | Training is sub-optimal. Certification and licensure requirements are deficient |
| Availability of health informatics resources | Mature health informatics resources exist to support clinical care and decision-making | Health informatics resources including internet access not available especially in remote areas. Unaffordable subscription or download fees for medical information |
| Culture | Culture of safety exists; climate where clinicians not afraid to share and learn from mistakes. Patient-empowerment promoted, patients are partners in care | Traditional cultures often punitive, which discourages sharing and inhibits learning. Patients more passive care recipients |
Typically, there are multiple ‘root causes’ in each error case. These include both cognitive errors such as failing to synthesise the available evidence correctly or failure to use the physical exam or test data appropriately. System flaws such as problems with communication or coordinating care, problems with the availability of medical record data and insufficient access to specialists are also contributory factors.10 12 35–38 A survey of 600 US PCPs identified typical concerns, such as settling too rapidly on a diagnosis, failing to consider an appropriately broad differential diagnosis or failing to order appropriate tests or consultations.39
High-risk situations
Studies on the relative frequency of conditions involved are largely from high-income countries. Reviews of diagnostic errors encountered in ambulatory care settings suggest that diagnostic errors may derive from routine as well as infrequent/rare conditions. Some of the conditions described in a systematic review included malignancies, myocardial infarction, meningitis, dementia, iron deficiency anaemia, asthma, tremor in the elderly and HIV.6 The observational study of 190 cases of diagnostic errors12 described earlier found that the most commonly encountered conditions involved pneumonia (6.7%), decompensated congestive heart failure (5.7%), acute renal failure (5.3%), cancer (5.3%) and urinary tract infection or pyelonephritis (4.8%).
Common diagnostic errors reported in a survey of PCPs included cancer, pulmonary embolism and coronary artery disease.39 Another survey of US internal medicine physicians reported both outpatient and inpatient errors related to pulmonary embolism (4.5%), drug reactions (4.5%), lung, colorectal and breast cancers (3.9%, 3.3% and 3.1%, respectively), acute coronary syndrome (3.1%) and stroke (2.6%).17 In a US study of 181 malpractice claims, cancer was the most common diagnosis involved.37 An analysis of 1000 negligent claims against the UK general practitioners identified diagnostic errors most commonly involving infections, trauma and cancer.40 Malpractice claims, however, tend to involve diagnoses that are more serious or most harmful if not diagnosed correctly in a timely fashion and do not necessarily represent error frequency. Nevertheless, infections, cardiovascular disease and cancer consistently emerge as the most significant categories of harmful diagnostic errors in the outpatient setting (table 2). Because children are frequently seen in primary care and are vulnerable to errors, we include them as a population at risk.
Table 2.
At-risk categories of harmful diagnostic errors
| High-risk area | Disease | Additional considerations |
|---|---|---|
| Infections | Viral infections | Often misdiagnosed as bacterial and result in unnecessary antibiotics |
| Pneumonia, dehydration from diarrhoea and malaria | Diagnoses of children often suboptimal, particularly with less well-trained healthcare workers41 | |
| Malaria | Key presenting features (eg, fever) not specific42 | |
| Tuberculosis | Lack of careful use of basic diagnostics result in almost 10% being misdiagnosed.43 Failure to diagnose has important public health implications. Also occur from misinterpretation of test results and failure to use basic diagnostic tools (microbiology or imaging)44 |
|
| Cardiovascular disease | Myocardial infarction, stroke | Ranks high in malpractice claims37 and autopsy studies45 Subtle premonitory symptoms at first-contact settings often missed Delays in diagnosis prevalent in predisposing conditions, including type 2 diabetes (median delay >2 years; 7% remained undiagnosed at 7.5 years) and hypertension46–48 |
| Cancer | Several cancer types49–54 | Alarm symptoms often poorly predictive,55 low signal-to-noise ratio. Cancer can be in differential of many common symptoms including headache, weight loss, bleeding, pain Almost a third of colorectal and lung cancer diagnoses have missed opportunities despite ‘red flags’ (abnormal faecal occult blood, microcytic anaemia and abnormal imaging)19 20 Referral of patients with suspected cancer for confirmatory testing challenging due to poor access or cost Challenges of overdiagnosis emerge when incidental findings relentlessly pursued |
| Paediatrics | Claims study56 suggests meningitis, gastroenteritis, pneumonia, appendicitis, sepsis and malignancy | Misdiagnoses may contribute to the nearly 7 million children who die each year, largely from preventable causes57 |
| Meningococcal disease58 | Half of children misdiagnosed at the first physician contact largely because presenting symptoms were non-specific | |
| Viral illnesses diagnosed as bacterial, medication side effects, appendicitis and psychiatric disorders30 | More than half of surveyed paediatricians reported making a diagnostic error at least once or twice a month, and harmful errors at least once or twice a year | |
| Hypertension, problems with referrals and follow-up of abnormal laboratory values59 | Primary care paediatricians who were surveyed expressed high interest in trying to improve common sub-critical errors vs errors in less common acute situations |
Interventions to reduce diagnostic errors
Physicians are often unaware of outcomes of their care, including their own diagnostic errors. Furthermore, both autopsy studies and vignette reviews show that physicians' diagnostic accuracy and the confidence they have in that accuracy are not always aligned.60 61 The marked decline of autopsies in recent years and absence of effective feedback mechanisms are factors that can lead to overconfidence and lack of appropriate calibration.33 62 Beyond raising awareness and developing effective strategies to deal with diagnostic uncertainty, a host of interventions targeting both cognitive-related and systems-related elements have been proposed, although few have been empirically tested.63 Systems-based interventions target all five dimensions mentioned earlier, whereas cognitive interventions seek to expand clinicians' knowledge and experience (eg, using simulation), improve clinical reasoning and decision-making skills or provide cognitive ‘help’ (decision support and second opinions).
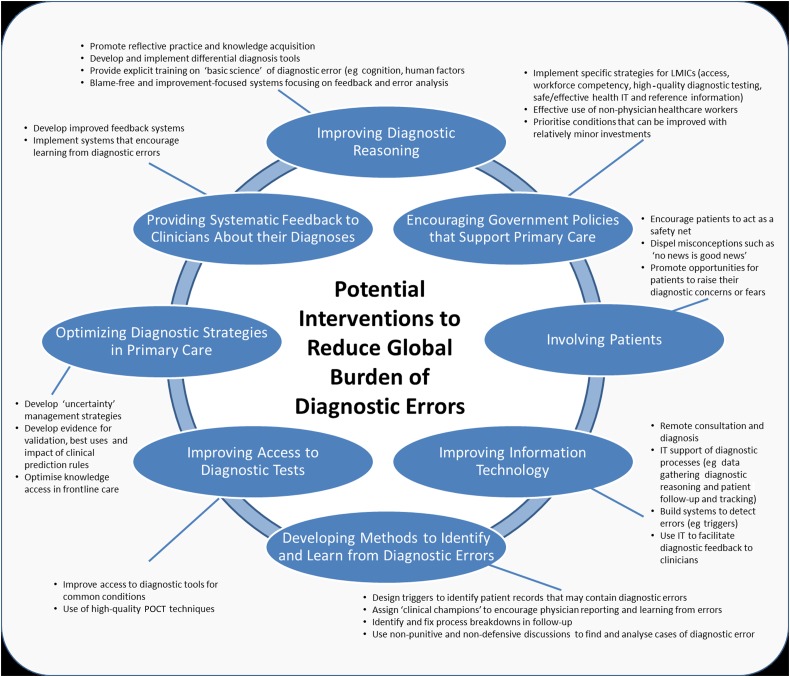
While some interventions we consider here should logically improve diagnosis,2 current evidence of their effectiveness is limited.64 65 There is likely a need for multifaceted or multiple interventions.66 Recognising the lack of robust evidence of error reduction, we identify areas where interventions could be designed and tested (figure 2). We propose eight themes for interventions, all of which are grounded in ‘the Safer Dx framework’ to measure and reduce diagnostic error.13 The framework follows Donabedian's Structure-Process-Outcome model where the structural component is the ‘sociotechnical work system’ composed of various dimensions including people, technologies (particularly health information technologies), organisational policies and practices and external rules and regulations. Because errors arise from interactions among the various dimensions of the sociotechnical healthcare system, multiple components need to be simultaneously addressed by interventions. The ‘process’ aspects of the Safer Dx framework are defined by the five process dimensions described earlier in the Introduction. The ‘outcome’ is safe and efficient diagnosis (correct and timely, as opposed to missed, delayed, wrong) as well as long-term outcomes (eg, value, patient outcomes) related to healthcare delivery.
Figure 2.
Potential interventions to reduce global burden of diagnostic errors. IT, information technology; POCT, point-of-care testing.
Improving diagnostic reasoning
Studies of PCPs who recounted diagnostic errors highlight failures in all stages of the diagnostic process.6 17 67–69 Several experimental studies have highlighted reasoning biases, in relation to both hypothesis generation and information interpretation in PCPs. Certain aspects of diagnostic reasoning67 might be more important, more common or more amenable to interventions. Interventions that could potentially improve clinical reasoning include advice to practice reflectively,70–72 use of tools such as mnemonics and checklists,73 and web-based decision support products that assist with differential diagnosis.74–76 ‘Debiasing’ has been proposed as an approach to eliminate subconscious biases that contribute to error.77 78 While many find the idea of focusing on cognitive biases and heuristics to improve clinical reasoning appealing, physicians find it difficult to characterise specific biases with any reliability and identify twice as many biases when outcome implies incorrect versus correct diagnosis.79 80 Knowledge is still key to diagnostic accuracy and efforts to promote it essential.81
Improving reliability of diagnosis requires reforming training and medical education for PCPs and including concepts related to the ‘basic science’ of diagnostic error.82 PCPs would also benefit from working in blame-free and improvement-focused systems that focus on feedback and error analysis as tools to improve performance. They need an environment that transforms errors into learning opportunities.
Encouraging government policies that support primary care
Robust government policies focusing on strengthening primary care systems and making it safe and effective while seem logical83 84 are often not well implemented. Specific strategies, some of which are more challenging for LMICs,85 include enhancing access to care and appropriate expertise, ensuring the competency of PCPs and primary care teams,86 making available high-quality diagnostic testing services (radiology/laboratory), providing a suitable work environment with safe and effective health information technology (IT) and improving access to reference information resources.87
In areas where access to primary care is limited, non-physician healthcare workers provide primary care, and in some cases have made considerable impact on health indicators,88 often using simple clinical algorithms such as the WHO's Integrated Management of Child Illness.89 However, adequate access to trained PCPs and specialists needs to be ensured for more challenging cases or when specialised diagnostic procedures are required. Short-term policies should prioritise conditions that can be improved with relatively minor investments, such as cancer or infection diagnoses or improved follow-up of patients seen for emergency care.
Improving information technology
Assuming internet access is available, an attractive option for improving access to appropriate expertise is the use of new technology that enables remote consultation and diagnosis. Remote reading of radiology imaging was a pioneering area,50 and the applications of remote diagnosis have expanded to include cardiology, ophthalmology, pathology, dermatology and even mental health. These resources enhance access to subspecialty expertise, often in real-time and can be particularly valuable for remote or dispersed clinical settings. Moreover, health IT can support diagnostic reasoning90 and promote detection of errors and follow-up and tracking.91 92 Deploying health IT-based interventions requires a coordinated plan to provide safe and effective hardware and software that support processes, users and workflow, as well as organisational support.93 Health IT approaches, tools and algorithms could be used in several steps of the diagnostic process in order to reduce diagnostic errors.87 These steps could include traditional steps of data gathering and broadening differential diagnosis but also novel ways to improve patient follow-up,94 detecting diagnostic errors via novel use of ‘triggers’22 95 96 and enabling diagnostic feedback to clinicians.97
Involving patients
Engaging and empowering patients is another low-cost investment with large potential to leverage improvement.98 Patients can act as a safety net by educating them what symptoms to look for, on the expected time course of their illness and how to re-access care if their condition does not improve or new symptoms emerge. In addition, patients can be proactive in ensuring diagnostic test results are reviewed. They can prompt providers to think comprehensively of a differential diagnosis (such as asking ‘what else do you think this could be?’), access medical knowledge on their own through reliable web sources and help prevent diagnostic errors by participating in follow-up and feedback.99–101 Ensuring longitudinal patient follow-up beyond the consultation is particularly important in primary care, given the non-specific presentation and evolution of many serious diseases over time.102 Patient empowerment includes dispelling misconceptions such as ‘no news is good news’ from the doctor (which could contribute to failures in follow-up of abnormal test results) and encouraging them to raise their diagnostic concerns or fears without feeling intimidated by the physician. However, this can be challenging in passive or paternalistic cultures, requiring a cultural reacclimation of both patients and providers. Allowing patients access to their medical records has substantial potential to improve diagnostic reliability.
Improving access to diagnostic tests
In addition to improving access to appropriate diagnostic tools for common infectious conditions such as pneumonia and diarrhoea,103 more focus is needed on non-communicable diseases (NCDs), which require laboratory or imaging tests for accurate diagnosis and monitoring.104 A recent WHO report points to a global cancer epidemic by 2025, which should be a high-priority area for future interventions given high rates of delayed cancer diagnosis and the difficulties with making diagnoses based on clinical features alone.19 20 105 Pathology and imaging services to support diagnostic testing are often limited in LMICs. Although plain radiography is available in many first-contact settings, access to more sophisticated imaging, including ultrasound, can be limited.
In many LMICs where centralised/referral laboratories are unavailable, point-of-care testing (POCT) may offer improved access to diagnostic and monitoring laboratory tests. A recent survey of PCPs in five countries highlighted the variation in POCT adoption and prioritised them for further development and implementation, but we need to demonstrate their effectiveness, including cost-effectiveness.106 In addition to developing, evaluating and implementing cost-effective POCT techniques for common conditions, healthcare personnel need to be trained on how to use them, and the testing, interpretation and reporting processes need appropriate oversight.
Developing methods to identify and learn from diagnostic errors
Current measures of quality of care in primary care are not focused on diagnostic error.107–109 To routinely assess the quality of diagnostic care, we need methods to better identify and define diagnostic errors. Promising approaches include designing triggers to identify patient records that may contain diagnostic errors,110 assigning ‘clinical champions’ to encourage physician reporting and learning from errors,111 and identifying and fixing process breakdowns in the follow-up of abnormal findings.3 96
Finding and analysing individual cases of diagnostic error through non-punitive and non-defensive discussions provide a unique opportunity to understand the problem and explore solutions.112 To minimise hindsight bias that arises when events are reviewed retrospectively, it is helpful to play forward rather than backward to see if a different set of appropriate actions/judgement emerge. The goal is to understand why the actions (or inactions) made sense at the time, and what could be improved in the future.113 Actions that worked well should also be highlighted.
Optimising diagnostic strategies in primary care
Research is needed to define how best to manage uncertainty, delineating the diagnostic value and time course of emergence of individual and combinations of clinical features. More evidence is also needed for the validation, best uses and impact of clinical prediction rules in primary care—many of which remain untested in this setting.114 Research on optimising knowledge access in frontline care is needed. Many knowledge-related diagnostic questions during practice go unanswered as busy physicians move on to the next patient.113 For many reasons, diagnostic decision support programmes are underused, with physicians mainly citing lack of time and concerns about their efficiency and utility.115
Providing systematic feedback to clinicians about their diagnoses
In addition to learning from their own (and others') errors, physicians need to continuously refine and recalibrate their diagnostic skills. Improving feedback to PCPs is consistent with good engineering principles, but is generally minimal or absent in primary care.62 One fertile area for investigation is the potential impact of feedback on competency in diagnostic reasoning62 and what roles patients could play here. Research is also needed to identify the most practical and effective methods of providing feedback to PCPs, and how to implement systems that encourage practitioners and systems to learn from diagnostic errors (and diagnostic successes). One model is the Confidential Enquiry approach used in several countries,116 117 which can explore reasons for underlying catastrophic diagnostic errors and help identify priority actions. This approach uses expert panels and local clinicians to perform detailed case reviews of a series of patients who suffered poor outcomes (usual fatalities) in a non-judgemental multiperspective process.
Next steps for policy, practice and science
While there are plenty of intervention opportunities discussed above, most work in this area is retrospective and conducted in high-income settings and might not represent multiple types of primary care settings globally. Much more robust data are needed from LMICs. Rigorous research is needed to establish the incidence and epidemiology of diagnostic error, to understand the role of contributory factors and to evaluate potential cognitive and/or system-related interventions.118 Evidence suggests that there is no single ‘magic bullet’ intervention for diagnostic error, and solutions need to be rigorously evaluated for benefits and unintended consequences.66 Moreover, we need research to define and evaluate the quality of diagnostic performance. Funding is required for all of this research.
The IOM recently also made several concrete recommendations to reduce diagnostic error, focusing on individual clinicians and also on patients, diagnostic services such as laboratory, pathology and radiology, and healthcare delivery systems.14 Many of these recommendations are applicable globally, such as better teamwork among all parties involved in diagnosis, adequate time and reimbursement for ‘cognitive’ work of PCPs, health IT that supports diagnosis, engaging patients, learning from errors and research funding climate conducive to accelerating our understanding of both problems and solutions. However, most will take sustained action and what is needed now are steps to outline a multifaceted approach that takes into account the local context where solutions are to be implemented.119 Based on the review, we suggest that the WHO consider bringing together primary care leaders, practicing frontline clinicians, safety experts, policymakers, health IT community, medical education and accreditation organisations, researchers from multiple disciplines, patient advocates and funding bodies among others, to address the many common challenges and opportunities to reduce diagnostic error.
Conclusions
Diagnostic errors are relatively frequent and harmful in primary care. While much remains to be learned, it is evident that errors involve diagnosis of common conditions. Diagnostic errors in primary care affect all countries, strategies to address them involve many stakeholders, and there is no other global agency addressing the problem. Thus, WHO's leadership and actions on a global level will be instrumental for prioritisation of practice changes needed to improve primary care as well as setting research priorities for intervention development to reduce diagnostic error.
Footnotes
Twitter: Follow Hardeep Singh at @HardeepSinghMD
Funding: Dr. Singh's research is supported by the VA Health Services Research and Development Service (CRE 12–033; Presidential Early Career Award for Scientists and Engineers USA 14–274), the VA National Center for Patient Safety, the Agency for Health Care Research and Quality (R01HS022087 and R21 HS 023602) and in part by the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cresswell KM, Panesar SS, Salvilla SA, et al. Global research priorities to better understand the burden of iatrogenic harm in primary care: an international Delphi exercise. PLoS Med 2013;10:e1001554 10.1371/journal.pmed.1001554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evidence scan: Improving safety in primary care. The Health Foundation, 2011. (cited 16 May 2016). http://www.health.org.uk/sites/default/files/ImprovingSafetyInPrimaryCare.pdf [Google Scholar]
- 3.Graber ML, Trowbridge RL, Myers JS, et al. The next organizational challenge: finding and addressing diagnostic error. Jt Comm J Qual Patient Saf 2014;40:102–10. [DOI] [PubMed] [Google Scholar]
- 4.Verstappen W, Gaal S, Bowie P, et al. A research agenda on patient safety in primary care. Recommendations by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract 2015;21(Suppl):72–7. 10.3109/13814788.2015.1043726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Primary health care: Main terminology. World Health Organization, 2016. (cited 14 June 2016). [Google Scholar]
- 6.Kostopoulou O, Delaney BC, Munro CW. Diagnostic difficulty and error in primary care—a systematic review. Fam Pract 2008;25:400–13. 10.1093/fampra/cmn071 [DOI] [PubMed] [Google Scholar]
- 7.Singh H, Sittig DF. Setting the record straight on measuring diagnostic errors. Reply to: ‘Bad assumptions on primary care diagnostic errors’ by Dr Richard Young. BMJ Qual Saf 2015;24:345–8. 10.1136/bmjqs-2015-004140 [DOI] [PubMed] [Google Scholar]
- 8.Goyder CR, Jones CHD, Heneghan CJ, et al. Missed opportunities for diagnosis: lessons learned from diagnostic errors in primary care. Br J Gen Pract 2015;65:e838–44. 10.3399/bjgp15X687889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panesar SS, de Silva D, Carson-Stevens A, et al. How safe is primary care? A systematic review. BMJ Qual Saf 2016;25:544–53. 10.1136/bmjqs-2015-004178 [DOI] [PubMed] [Google Scholar]
- 10.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med 2005;165:1493–9. 10.1001/archinte.165.13.1493 [DOI] [PubMed] [Google Scholar]
- 11.Zwaan L, Singh H. The challenges in defining and measuring diagnostic error. Diagnosis (Berl) 2015;2:97–103. 10.1515/dx-2014-0069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh H, Giardina TD, Meyer AN, et al. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med 2013;173:418–25. 10.1001/jamainternmed.2013.2777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf 2015;24:103–10. 10.1136/bmjqs-2014-003675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute of Medicine. Improving diagnosis in health care. Washington, DC: National Academies of Sciences, Engineering, and Medicine, 2015. (http://iom.nationalacademies.org/Reports/2015/Improving-Diagnosis-in-Healthcare.aspx). [Google Scholar]
- 15.Casalino LP, Dunham D, Chin MH, et al. Frequency of failure to inform patients of clinically significant outpatient test results. Arch Intern Med 2009;169:1123–9. 10.1001/archinternmed.2009.130 [DOI] [PubMed] [Google Scholar]
- 16.Singh H, Esquivel A, Sittig DF, et al. Follow-up actions on electronic referral communication in a multispecialty outpatient setting. J Gen Intern Med 2011;26:64–9. 10.1007/s11606-010-1501-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med 2009;169:1881–7. 10.1001/archinternmed.2009.333 [DOI] [PubMed] [Google Scholar]
- 18.Singh H. Editorial: Helping health care organizations to define diagnostic errors as missed opportunities in diagnosis. Jt Comm J Qual Patient Saf 2014;40:99–101. [DOI] [PubMed] [Google Scholar]
- 19.Singh H, Daci K, Petersen LA, et al. Missed opportunities to initiate endoscopic evaluation for colorectal cancer diagnosis. Am J Gastroenterol 2009;104:2543–54. 10.1038/ajg.2009.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh H, Hirani K, Kadiyala H, et al. Characteristics and predictors of missed opportunities in lung cancer diagnosis: an electronic health record-based study. J Clin Oncol 2010;28:3307–15. 10.1200/JCO.2009.25.6636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh H, Giardina TD, Petersen LA, et al. Exploring situational awareness in diagnostic errors in primary care. BMJ Qual Saf 2012;21:30–8. 10.1136/bmjqs-2011-000310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh H, Giardina TD, Forjuoh SN, et al. Electronic health record-based surveillance of diagnostic errors in primary care. BMJ Qual Saf 2012;21:93–100. 10.1136/bmjqs-2011-000304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fischhoff B. Hindsight does not equal foresight: the effect of outcome knowledge on judgment under uncertainty. J Exp Psychol Hum Percept Perform 1975;1:288–99. 10.1037/0096-1523.1.3.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh H, Meyer AN, Thomas EJ. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf 2014;23:727–31. 10.1136/bmjqs-2013-002627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khoo EM, Lee WK, Sararaks S, et al. Medical errors in primary care clinics—a cross sectional study. BMC Fam Pract 2012;13:127 10.1186/1471-2296-13-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips RL Jr, Bartholomew LA, Dovey SM, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care 2004;13:121–6. 10.1136/qshc.2003.008029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schiff GD, Puopolo AL, Huben-Kearney A, et al. Primary care closed claims experience of Massachusetts malpractice insurers. JAMA Intern Med 2013;173:2063–8. 10.1001/jamainternmed.2013.11070 [DOI] [PubMed] [Google Scholar]
- 28.Sandars J, Esmail A. The frequency and nature of medical error in primary care: understanding the diversity across studies. Fam Pract 2003;20:231–6. 10.1093/fampra/cmg301 [DOI] [PubMed] [Google Scholar]
- 29.Bhasale AL, Miller GC, Reid SE, et al. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust 1998;169:73–6. [DOI] [PubMed] [Google Scholar]
- 30.Singh H, Thomas EJ, Wilson L, et al. Errors of diagnosis in pediatric practice: a multisite survey. Pediatrics 2010;126:70–9. 10.1542/peds.2009-3218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Health statistics and information systems: definition of region groupings. World Health Organization, 2016. (cited 14 June 2016). http://www.who.int/healthinfo/global_burden_disease/definition_regions/en/ [Google Scholar]
- 32.Data: Country and Lending Groups. The World Bank, 2016. (cited 16 May 2016); http://data.worldbank.org/about/country-and-lending-groups [Google Scholar]
- 33.Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med 2008;121(Suppl 1):S2–23. 10.1016/j.amjmed.2008.01.001 [DOI] [PubMed] [Google Scholar]
- 34.Graber ML. The incidence of diagnostic error in medicine. BMJ Qual Saf 2013;22(Suppl 2):ii21–7. 10.1136/bmjqs-2012-001615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnostic errors: Lessons from a multi-institutional collaborative project. Advances in Patient Safety: from Research to Implementation (Volume 2: Concepts and Methodology). Rockville, MD: Agency for Healthcare Research and Quality, AHRQ Publication Nos. 050021 (1-4), 2005:255-78. [Google Scholar]
- 36.Sarkar U, Bonacum D, Strull W, et al. Challenges of making a diagnosis in the outpatient setting: a multi-site survey of primary care physicians. BMJ Qual Saf 2012;21:641–8. 10.1136/bmjqs-2011-000541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med 2006;145:488–96. 10.7326/0003-4819-145-7-200610030-00006 [DOI] [PubMed] [Google Scholar]
- 38.Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med 2005;142:352–8. 10.7326/0003-4819-142-5-200503010-00010 [DOI] [PubMed] [Google Scholar]
- 39.Ely JW, Kaldjian LC, D'Alessandro DM. Diagnostic errors in primary care: lessons learned. J Am Board Fam Pract 2012;25:87–97. 10.3122/jabfm.2012.01.110174 [DOI] [PubMed] [Google Scholar]
- 40.Silk N. What Went Wrong in 1,000 Negligence Claims. Health Care Risk Report. Medical Protection Society 2000.
- 41.Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012;379:2151–61. 10.1016/S0140-6736(12)60560-1 [DOI] [PubMed] [Google Scholar]
- 42.Leslie T, Mikhail A, Mayan I, et al. Rapid diagnostic tests to improve treatment of malaria and other febrile illnesses: patient randomised effectiveness trial in primary care clinics in Afghanistan. BMJ 2014;348:g3730 10.1136/bmj.g3730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ollé Goig JE. Diagnostic errors related with tuberculosis in hospitalized patients. Arch Bronconeumol 2000;36:515–18. 10.1016/S0300-2896(15)30113-7 [DOI] [PubMed] [Google Scholar]
- 44.Szczuka I, Pawlicka L, Kuś J, et al. Analysis of diagnostic errors and recommendations of diagnostic procedures in bacteriologically negative pulmonary tuberculosis. Pneumonol Alergol Pol 1998;66:17–23. [PubMed] [Google Scholar]
- 45.Winters B, Custer J, Galvagno SM Jr, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf 2012;21:894–902. 10.1136/bmjqs-2012-000803 [DOI] [PubMed] [Google Scholar]
- 46.Samuels TA, Cohen D, Brancati FL, et al. Delayed diagnosis of incident type 2 diabetes mellitus in the ARIC study. Am J Manag Care 2006;12:717–24. [PubMed] [Google Scholar]
- 47.Edelman D. Outpatient diagnostic errors: unrecognized hyperglycemia. Eff Clin Pract 2002;5:11–16. [PubMed] [Google Scholar]
- 48.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68. 10.1001/jama.2013.184182 [DOI] [PubMed] [Google Scholar]
- 49.Singh H, Khan R, Giardina TD, et al. Postreferral colonoscopy delays in diagnosis of colorectal cancer: a mixed-methods analysis. Qual Manag Health Care 2012;21:252–61. 10.1097/QMH.0b013e31826d1f28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Noro R, Hubaux JP, Meuli R, et al. Real-time telediagnosis of radiological images through an asynchronous transfer mode network: the ARTeMeD project. J Digit Imaging 1997;10(3 Suppl 1):116–21. 10.1007/BF03168673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Toddler dies of leukaemia after medics miss condition 35 times. The Telegraph. http://www.telegraph.co.uk/news/health/12133228/Toddler-dies-of-leukaemia-after-medics-miss-condition-35-times.html. Date accessed: 15 February 2016.
- 52.Onysko J, Maxwell C, Eliasziw M, et al. Large increases in hypertension diagnosis and treatment in Canada after a healthcare professional education program. Hypertension 2006;48:853–60. 10.1161/01.HYP.0000242335.32890.c6 [DOI] [PubMed] [Google Scholar]
- 53.Lyratzopoulos G, Vedsted P, Singh H. Understanding missed opportunities for more timely diagnosis of cancer in symptomatic patients after presentation. Br J Cancer 2015;112(Suppl 1):S84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Singh H, Sethi S, Raber M, et al. Errors in cancer diagnosis: current understanding and future directions. J Clin Oncol 2007;25:5009–18. 10.1200/JCO.2007.13.2142 [DOI] [PubMed] [Google Scholar]
- 55.Hamilton W, Lancashire R, Sharp D, et al. The risk of colorectal cancer with symptoms at different ages and between the sexes: a case-control study. BMC Med 2009;7:17 10.1186/1741-7015-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wallace E, Lowry J, Smith SM, et al. The epidemiology of malpractice claims in primary care: a systematic review. BMJ Open 2013;3:e002929 10.1136/bmjopen-2013-002929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.UNICEF. Levels and trends in child mortality, estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York: United Nations Children's Fund, 2014. [Google Scholar]
- 58.Thompson MJ, Ninis N, Perera R, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet 2006;367:397–403. 10.1016/S0140-6736(06)67932-4 [DOI] [PubMed] [Google Scholar]
- 59.Rinke ML, Singh H, Ruberman S, et al. Primary care pediatricians' interest in diagnostic error reduction. Diagnosis 3.2 (2016):65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meyer AN, Payne VL, Meeks DW, et al. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med 2013;173:1952–8. 10.1001/jamainternmed.2013.10081 [DOI] [PubMed] [Google Scholar]
- 61.Podbregar M, Voga G, Krivec B, et al. Should we confirm our clinical diagnostic certainty by autopsies? Intensive Care Med 2001;27:1750–5. 10.1007/s00134-001-1129-x [DOI] [PubMed] [Google Scholar]
- 62.Schiff GD. Minimizing diagnostic error: the importance of follow-up and feedback. Am J Med 2008;121(Suppl 1):S38–42. 10.1016/j.amjmed.2008.02.004 [DOI] [PubMed] [Google Scholar]
- 63.McDonald KM, Matesic B, Contopoulos-Ioannidis DG, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med 2013;158(Pt 2):381–9. 10.7326/0003-4819-158-5-201303051-00004 [DOI] [PubMed] [Google Scholar]
- 64.Graber ML, Kissam S, Payne VL, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf 2012;21:535–57. 10.1136/bmjqs-2011-000149 [DOI] [PubMed] [Google Scholar]
- 65.Singh H, Graber ML, Kissam SM, et al. System-related interventions to reduce diagnostic errors: a narrative review. BMJ Qual Saf 2012;21:160–70. 10.1136/bmjqs-2011-000150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singh H. Diagnostic errors: moving beyond ‘no respect’ and getting ready for prime time. BMJ Qual Saf 2013;22:789–92. 10.1136/bmjqs-2013-002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Balla J, Heneghan C, Goyder C, et al. Identifying early warning signs for diagnostic errors in primary care: a qualitative study. BMJ Open 2012;2:e001539 10.1136/bmjopen-2012-001539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kostopoulou O, Devereaux-Walsh C, Delaney BC. Missing celiac disease in family medicine: the importance of hypothesis generation. Med Decis Making 2009;29:282–90. 10.1177/0272989X08327493 [DOI] [PubMed] [Google Scholar]
- 69.Kostopoulou O, Russo JE, Keenan G, et al. Information distortion in physicians’ diagnostic judgments. Med Decis Making 2012;32:831–9. 10.1177/0272989X12447241 [DOI] [PubMed] [Google Scholar]
- 70.Balla JI, Heneghan C, Glasziou P, et al. A model for reflection for good clinical practice. J Eval Clin Pract 2009;15:964–9. 10.1111/j.1365-2753.2009.01243.x [DOI] [PubMed] [Google Scholar]
- 71.Mamede S, Schmidt HG, Rikers R. Diagnostic errors and reflective practice in medicine. J Eval Clin Pract 2007;13:138–45. 10.1111/j.1365-2753.2006.00638.x [DOI] [PubMed] [Google Scholar]
- 72.Lambe KA, O'Reilly G, Kelly BD, et al. Dual-process cognitive interventions to enhance diagnostic reasoning: a systematic review. BMJ Qual Saf 2016; Published Online First 12 February 2016 10.1136/bmjqs-2015-004417 [DOI] [PubMed] [Google Scholar]
- 73.Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med 2011;86:307–13. 10.1097/ACM.0b013e31820824cd [DOI] [PubMed] [Google Scholar]
- 74.Ramnarayan P, Cronje N, Brown R, et al. Validation of a diagnostic reminder system in emergency medicine: a multi-centre study. Emerg Med J 2007;24:619–24. 10.1136/emj.2006.044107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kostopoulou O, Rosen A, Round T, et al. Early diagnostic suggestions improve accuracy of GPs: a randomised controlled trial using computer-simulated patients. Br J Gen Pract 2014;65:e49–54. 10.3399/bjgp15X683161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Riches N, Panagioti M, Alam R, et al. The effectiveness of electronic differential diagnoses (DDX) generators: a systematic review and meta-analysis. PLoS ONE 2016;11:e0148991 10.1371/journal.pone.0148991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf 2013;22(Suppl 2):ii58–64. 10.1136/bmjqs-2012-001712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Larrick R. Debiasing. In: Koehler D, Harvey N. The Blackwell Handbook of Judgment and Decision Making. Oxford: Blackwell Publishing, 2004:316–37. [Google Scholar]
- 79.Zwaan L, Monteiro S, Sherbino J, et al. Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Qual Saf 2016; Published Online First 29 January 2016 10.1136/bmjqs-2015-005014 [DOI] [PubMed] [Google Scholar]
- 80.Dhaliwal G. Premature closure? Not so fast . BMJ Qual Saf 2016; Published Online First 15 March 2016 10.1136/bmjqs-2016-005267 [DOI] [PubMed] [Google Scholar]
- 81.Monteiro SD, Sherbino JD, Ilgen JS, et al. Disrupting diagnostic reasoning: do interruptions, instructions, and experience affect the diagnostic accuracy and response time of residents and emergency physicians? Acad Med 2015;90:511–17. 10.1097/ACM.0000000000000614 [DOI] [PubMed] [Google Scholar]
- 82.Singh H, Petersen LA, Thomas EJ. Understanding diagnostic errors in medicine: a lesson from aviation. Qual Saf Health Care 2006;15:159–64. 10.1136/qshc.2005.016444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83:457–502. 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wolfe I, Thompson M, Gill P, et al. Health services for children in Western Europe. Lancet 2013;381:1224–34. 10.1016/S0140-6736(12)62085-6 [DOI] [PubMed] [Google Scholar]
- 85.Anant P, Bergkvist S, Chandani T, et al. Landscaping of primary healthcare in India. ACCESS Health International, 2016. (cited 14 June 2016). http://accessh.org/wp-content/uploads/2016/05/Primary-Care-Landscape_ACCESS-Health-International.pdf [Google Scholar]
- 86.Singh H, Graber M. Reducing diagnostic error through medical home-based primary care reform. JAMA 2010;304:463–4. 10.1001/jama.2010.1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.El-Kareh R, Hasan O, Schiff GD. Use of health information technology to reduce diagnostic errors. BMJ Qual Saf 2013;22(Suppl 2):ii40–51. 10.1136/bmjqs-2013-001884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Makaula P, Bloch P, Banda HT, et al. Primary health care in rural Malawi—a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res 2012;12:328 10.1186/1472-6963-12-328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Druetz T, Siekmans K, Goossens S, et al. The community case management of pneumonia in Africa: a review of the evidence. Health Policy Plan 2015;30:253–66. 10.1093/heapol/czt104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nurek M, Kostopoulou O, Delaney BC, et al. Reducing diagnostic errors in primary care. A systematic meta-review of computerized diagnostic decision support systems by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract 2015;21(Suppl):8–13. 10.3109/13814788.2015.1043123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Singh H, Naik AD, Rao R, et al. Reducing diagnostic errors through effective communication: harnessing the power of information technology. J Gen Intern Med 2008;23:489–94. 10.1007/s11606-007-0393-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Singh H, Sittig DF. Were my diagnosis and treatment correct? No news is not necessarily good news. J Gen Intern Med 2014;29:1087–9. 10.1007/s11606-014-2890-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care 2010;19(Suppl 3):i68–74. 10.1136/qshc.2010.042085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Murphy DR, Wu L, Thomas EJ, et al. Electronic trigger-based intervention to reduce delays in diagnostic evaluation for cancer: a cluster randomized controlled trial. J Clin Oncol 2015;33:3560–7. 10.1200/JCO.2015.61.1301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Murphy DR, Thomas EJ, Meyer AN, et al. Development and validation of electronic health record-based triggers to detect delays in follow-up of abnormal lung imaging findings. Radiology 2015;277:81–7. 10.1148/radiol.2015142530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Murphy DR, Laxmisan A, Reis BA, et al. Electronic health record-based triggers to detect potential delays in cancer diagnosis. BMJ Qual Saf 2014;23:8–16. 10.1136/bmjqs-2013-001874 [DOI] [PubMed] [Google Scholar]
- 97.Schiff GD, Bates DW. Can electronic clinical documentation help prevent diagnostic errors? N Engl J Med 2010;362: 1066–9. 10.1056/NEJMp0911734 [DOI] [PubMed] [Google Scholar]
- 98.Southwick FS, Cranley NM, Hallisy JA. A patient-initiated voluntary online survey of adverse medical events: the perspective of 696 injured patients and families. BMJ Qual Saf 2015;24:620-9. 10.1136/bmjqs-2015-003980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McDonald KM, Bryce CL, Graber ML. The patient is in: patient involvement strategies for diagnostic error mitigation. BMJ Qual Saf 2013;22(Suppl 2):ii33–9. 10.1136/bmjqs-2012-001623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Graber ML. Reducing diagnostic error in medicine – there's a job for everyone. NPSF Focus Patient Saf 2009;12:6–7. [Google Scholar]
- 101.Patient Toolkit. Society to Improve Diagnosis in Medicine. 2015. (cited 16 A.D. May 2016). [Google Scholar]
- 102.Almond S, Mant D, Thompson M. Diagnostic safety-netting. Br J Gen Pract 2009;59:872–4. 10.3399/bjgp09X472971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bhutta ZA, Das JK, Walker N, et al. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet 2013;381:1417–29. 10.1016/S0140-6736(13)60648-0 [DOI] [PubMed] [Google Scholar]
- 104.World Health Organization. Implementation tools: package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. Geneva: World Health Organization, 2014. [Google Scholar]
- 105.Lyratzopoulos G, Wardle J, Rubin G. Rethinking diagnostic delay in cancer: how difficult is the diagnosis? BMJ 2014;349:g7400 10.1136/bmj.g7400 [DOI] [PubMed] [Google Scholar]
- 106.Howick J, Cals JWL, Jones C, et al. Current and future use of point-of-care tests in primary care: an international survey in Australia, Belgium, The Netherlands, the UK and the USA. BMJ Open 2014;4:e005611 10.1136/bmjopen-2014-005611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lorincz CY, Drazen E, Sokol PE, et al. Research in Ambulatory Patient Safety 2000–2010: A 10-Year Review. American Medical Association, 2011. [Google Scholar]
- 108.Wynia MK, Classen DC. Improving ambulatory patient safety: learning from the last decade, moving ahead in the next. JAMA 2011;306:2504–5. 10.1001/jama.2011.1820 [DOI] [PubMed] [Google Scholar]
- 109.Improving diagnosis in health care. National Academies of Sciences Engineering and Medicine 2015. (cited 14 June 2016). http://iom.nationalacademies.org/Reports/2015/Improving-Diagnosis-in-Healthcare.aspx [Google Scholar]
- 110.Singh H, Thomas EJ, Khan MM, et al. Identifying diagnostic errors in primary care using an electronic screening algorithm. Arch Intern Med 2007;167:302–8. 10.1001/archinte.167.3.302 [DOI] [PubMed] [Google Scholar]
- 111.Okafor N, Payne VL, Chathampally Y, et al. Using voluntary reports from physicians to learn from diagnostic errors in emergency medicine. Emerg Med J 2016;33: 245–52. 10.1136/emermed-2014-204604 [DOI] [PubMed] [Google Scholar]
- 112.Al-Mutairi A, Meyer AN, Thomas EJ, et al. Accuracy of the Safer Dx instrument to identify diagnostic errors in primary care. J Gen Intern Med 2016;31:602–8. 10.1007/s11606-016-3601-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ely JW, Osheroff JA, Ebell MH, et al. Obstacles to answering doctors’ questions about patient care with evidence: qualitative study. BMJ 2002;324:710 10.1136/bmj.324.7339.710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Plüddemann A, Wallace E, Bankhead C, et al. Clinical prediction rules in practice: review of clinical guidelines and survey of GPs. Br J Gen Pract 2014;64:e233–42. 10.3399/bjgp14X677860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sittig DF, Krall MA, Dykstra RH, et al. A survey of factors affecting clinician acceptance of clinical decision support. BMC Med Inform Decis Mak 2006;6:6 10.1186/1472-6947-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Harnden A, Mayon-White R, Mant D, et al. Child deaths: confidential enquiry into the role and quality of UK primary care. Br J Gen Pract 2009;59:819–24. 10.3399/bjgp09X472520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cantwell R, Clutton-Brock T, Cooper G, et al. Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011;118(Suppl 1):1–203. 10.1111/j.1471-0528.2010.02847.x [DOI] [PubMed] [Google Scholar]
- 118.Zwaan L, Schiff GD, Singh H. Advancing the research agenda for diagnostic error reduction. BMJ Qual Saf 2013;22(Suppl 2):ii52–7. 10.1136/bmjqs-2012-001624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sittig DF, Kahol K, Singh H. Sociotechnical evaluation of the safety and effectiveness of point-of-care mobile computing devices: a case study conducted in India. Stud Health Technol Inform 2013;192:515–19. [PubMed] [Google Scholar]