Badran et al. demonstrate an essential contribution of biallelic RELA expression in protecting stromal and epithelial cells from TNF-mediated cell death in patients with chronic mucocutaneous ulceration.
Abstract
The treatment of chronic mucocutaneous ulceration is challenging, and only some patients respond selectively to inhibitors of tumor necrosis factor-α (TNF). TNF activates opposing pathways leading to caspase-8–mediated apoptosis as well as nuclear factor κB (NF-κB)–dependent cell survival. We investigated the etiology of autosomal-dominant, mucocutaneous ulceration in a family whose proband was dependent on anti-TNF therapy for sustained remission. A heterozygous mutation in RELA, encoding the NF-κB subunit RelA, segregated with the disease phenotype and resulted in RelA haploinsufficiency. The patients’ fibroblasts exhibited increased apoptosis in response to TNF, impaired NF-κB activation, and defective expression of NF-κB–dependent antiapoptotic genes. Rela+/− mice have similarly impaired NF-κB activation, develop cutaneous ulceration from TNF exposure, and exhibit severe dextran sodium sulfate–induced colitis, ameliorated by TNF inhibition. These findings demonstrate an essential contribution of biallelic RELA expression in protecting stromal cells from TNF-mediated cell death, thus delineating the mechanisms driving the effectiveness of TNF inhibition in this disease.
Introduction
Chronic mucocutaneous ulceration is considered a hallmark of inflammation. Most patients with chronic mucocutaneous ulcers lack a genetic diagnosis, and the factors driving the development of mucosal lesions remain incompletely understood (Ciccarelli et al., 2014). Therapeutic interventions are typically empirical and do not uniformly achieve disease remission. A subset of patients selectively responds TNF inhibitors, implicating TNF in the pathogenesis of mucocutaneous lesions (Vitale et al., 2013; Olesen et al., 2016). TNF activates distinct pathways, leading to apoptosis as well as to survival. The proapoptotic effect of TNF is mediated primarily through caspase-8 activation. Its prosurvival effect is mediated predominantly by NF-κB, which is essential for protection against TNF toxicity (Zhou et al., 2003; Brenner et al., 2015). NF-κB exists as a hetero- or homodimer of its subunits RelA, RelB, c-Rel, NF-κB1, and NF-κB2. RelA/NF-κB1 heterodimers constitute the predominant form of NF-κB (Hayden and Ghosh, 2012). NF-κB is sequestered in the cytoplasm by the inhibitors of κB (IκB), which are degraded by inflammatory stimuli, thereby permitting nuclear translocation of NF-κB and the transcription of genes important for cell survival, inflammation, and host immunity (Hayden and Ghosh, 2012).
NF-κB has opposing roles in the pathogenesis of mucocutaneous ulceration (Atreya et al., 2008). NF-κB activation in mucosal macrophages results in increased secretion of proinflammatory cytokines, such as IL-6 (Neurath et al., 1996; Wang et al., 2003). In contrast, epithelial cell–specific, conditional ablation of NEMO or IKK-β, both of which are essential for NF-κB activation, results in increased intestinal inflammation (Nenci et al., 2007; Zaph et al., 2007). Although NF-κB is critical for cell survival, the contribution of defective RelA-mediated cellular homeostasis to human disease is unknown.
We report human RelA haploinsufficiency as the cause of an autosomal-dominant, mucocutaneous disease with impaired NF-κB activation. We identify TNF as a major driver of epithelial and stromal cell apoptosis in RelA haploinsufficiency. Our results provide the first evidence for an essential contribution of biallelic RELA expression to human mucosal integrity and elucidate mechanisms driving the favorable response to TNF inhibition in patients with recurrent mucocutaneous ulcers.
Results and discussion
Identification of a heterozygous mutation in RELA resulting in RelA haploinsufficiency
The proband (P1) presented at 3 yr of age with intermittent episodes of abdominal pain, vomiting, fever, leukocytosis, and elevated inflammatory markers, without evidence of infection or autoantibodies (Table S1). Biopsy revealed severe, acute ileitis, which was absent during periods of spontaneous disease remission. The patient had a history of oral ulcers but no other symptoms. Testing for inflammatory bowel disease markers with an IBD sgi diagnostic test (Prometheus Laboratories) was negative. Her serum TNF levels were <15 pg/ml (normal <22 pg/ml). Her disease did not respond to mesalamine, azathioprine, colchicine, or the IL-1 receptor antagonist anakinra. Daily prednisone was required for symptomatic relief. At the age of 5 yr, she was treated with the TNF inhibitors infliximab (Janssen Immunology) and methotrexate, resulting in remission without prednisone. In the 2 yr after starting treatment, her disease flared only when she gained weight resulting in an infliximab dose <5 mg/kg. She had no history of recurrent infections and had a normal immunologic evaluation (Table S1). Her mother and siblings had mucocutaneous lesions (Fig. 1 A). Her mother’s disease was refractory to colchicine and azathioprine but responded to prednisone; she declined treatment with infliximab. The proband’s parents declined in-depth testing and treatment of the proband’s siblings. The proband’s father and grandparents have no mucocutaneous lesions or recurrent gastrointestinal symptoms.
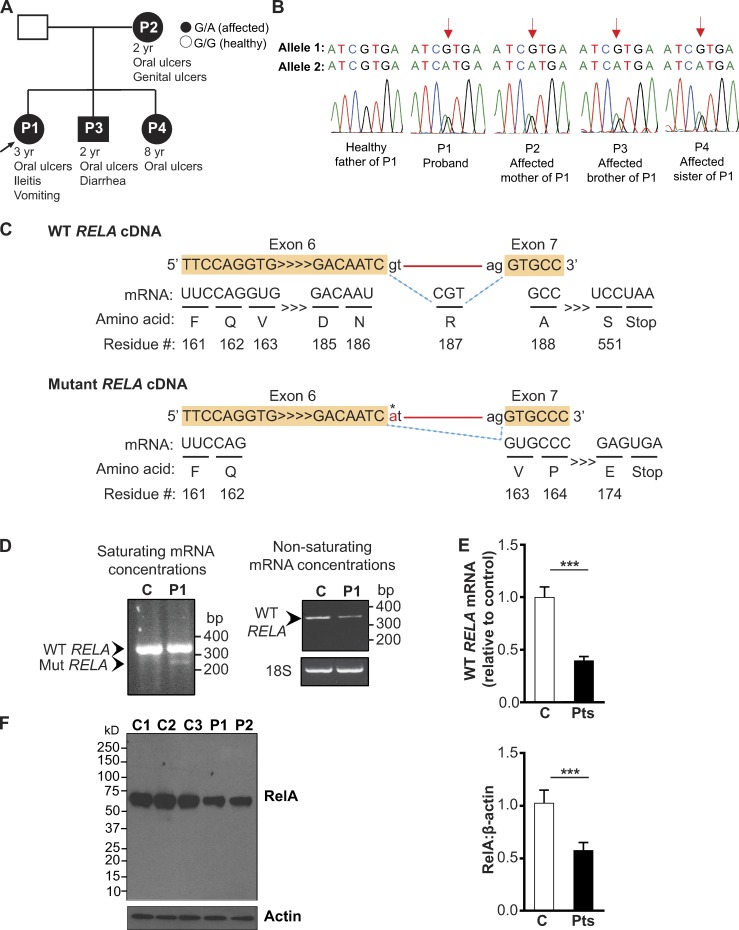
Figure 1.
Identification of a mutation in RELA that results in RelA haploinsufficiency. (A) Pedigree with RELA genotypes. (B) Sanger sequencing of the RELA mutation (arrow). (C) Schematic of WT and mutant RELA cDNA splicing (dotted blue lines) with the patients’ mutation (asterisk), interval nucleotides and aa (arrowheads), introns (red line). Alternative splicing of a cryptic splice site within exon 6 to the canonical acceptor splice site before exon 7 deletes 73 nucleotides at the 3′ of exon 6 and introduces a premature stop codon at residue 174. (D, left) RT-PCR, performed with saturating mRNA concentrations, identifies the alternatively spliced transcript (Mut RELA) in patient 1 (P1), but not in the control (Right) WT RELA transcript detected with RT-PCR under nonsaturating mRNA concentrations. Similar results were obtained in P2. Data are from one representative experiment of three independently performed. (E) WT RELA mRNA in P1 and P2 and three controls determined by qPCR using a primer complementary to the nucleotides in exon 6, specific to the WT RELA transcript. Gene expression was normalized to GAPDH. (F) Immunoblot of fibroblast lysates from controls (C1–C3) and patients (P1 and P2) using an N-terminal specific antibody against RelA, with densitometric quantification of RelA relative to β-actin. Data from E and F are pooled from three independent experiments. Columns and bars represent experiment means ± SEM. ***, P < 0.001, Student’s t test.
The family history suggested an autosomal-dominant disease. Whole-exome sequencing (WES) of the unaffected father and patients P1–P4 revealed seven rare heterozygous variants shared by the patients and absent in the healthy father (Table S2). Of these, only RELA is known to be important for counteracting TNF toxicity (Beg et al., 1995; Alcamo et al., 2001), a hallmark of the proband’s disease. Neither the Exome Aggregation Consortium nor 1000 Genomes databases contain loss-of-function variants for RELA, a gene that is known to be under strong, purifying selection (Lek et al., 2016). The RELA mutation alters the canonical donor splice site downstream of exon 6 (NM_021975: c.559+1G>A; Fig. 1, B and C). Sanger sequencing of the patients’ cDNA identified a minor, alternatively spliced RELA mRNA product containing a premature stop codon and a 50% reduction in WT RELA mRNA expression (Fig. 1, D and E). Immunoblotting using an antibody specific to the N terminus of RelA showed a 50% decrease in WT RelA protein expression in the patients compared with controls without detectable truncated products (Fig. 1 F). These data indicate that the mutation results in RelA haploinsufficiency.
Impaired NF-κB activation and impaired stromal cell survival in RelA haploinsufficiency
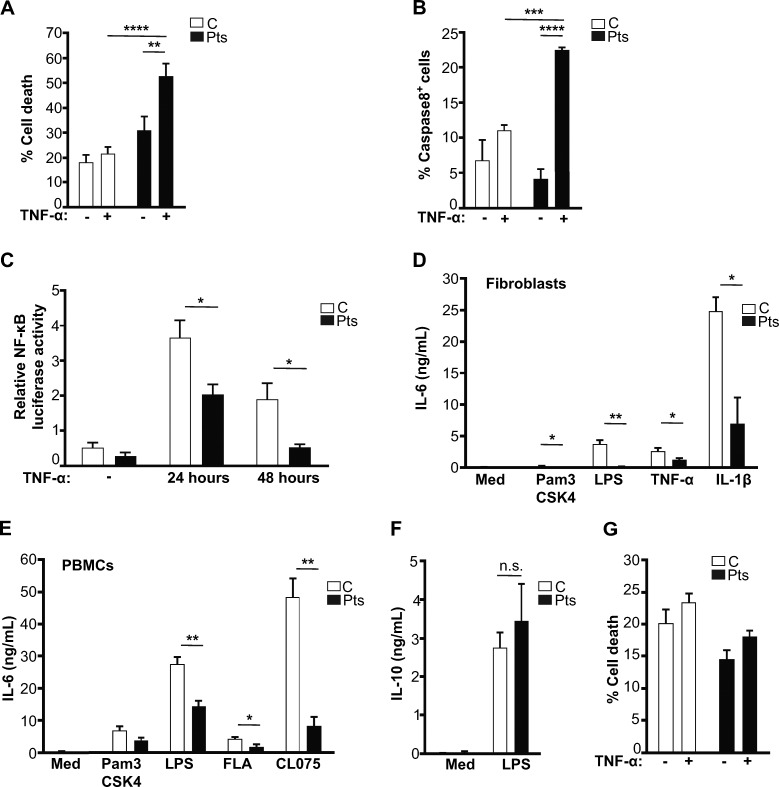
TNF activates divergent pathways leading to caspase-mediated apoptosis as well as NF-κB–activated survival, a balance that determines the extent of TNF-induced cell death. Compared with controls, the patients’ fibroblasts exhibited significantly more TNF-induced cell death and caspase-8 cleavage, with significantly less NF-κB activation and secretion of the NF-κB–regulated cytokine IL-6 (Fig. 2, A–D). PBMCs from the patients, but not from the healthy father, also had significantly impaired IL-6 secretion after TNF stimulation (Fig. 2 E and not depicted). In contrast, LPS-mediated IL-10 secretion, which is independent of RelA (Cao et al., 2006), from the patients’ PBMCs was normal (Fig. 2 F), thus indicating the specificity of the patients’ defect to the NF-κB pathway. These findings contrast with the increased NF-κB activation and IL-6 secretion characteristics of NF-κB–driven autoinflammatory disorders (Damgaard et al., 2016; Zhou et al., 2016a,b). The patients’ lymphocytes did not undergo increased apoptosis after TNF exposure (Fig. 2 G), consistent with their normal lymphocyte counts. RelA haploinsufficiency, therefore, results in increased stromal cell apoptosis in response to TNF but permits sufficient NF-κB activation for the maintenance of intact lymphocyte numbers and host immunity.
Figure 2.
RelA haploinsufficiency is associated with impaired NF-κB signaling and increased sensitivity to TNF. (A) Cell death, determined by annexin-V and/or fixable viability-dye staining, after fibroblasts from three controls (C) and patients 1 and 2 (Pts) were treated with TNF for 24 h. (B) Percentage of cleaved caspase8+ cells among the annexin-V+ population after fibroblasts from three controls and patients 1 and 2 were treated with TNF for 24 h. (C) Relative NF-κB luciferase activity in fibroblasts from three controls and patients 1 and 2 after treatment with TNF. (D) IL-6 secretion from fibroblasts and (E) PBMCs from three controls and patients 1 and 2 in response to stimulation with Pam3CSK4 (TLR1/2 agonist), LPS (TLR4 agonist), flagellin (FLA, TLR5 agonist), CL075 (TLR7/8 agonist), TNF, or IL-1β. (F) IL-10 secretion after LPS stimulation of PBMCs from patients 1 and 2 and five controls. (G) Cell death in TNF-treated PBMCs from three controls and Patients 1 and 2. All data are pooled from 3 independent experiments. Columns and bars represent means ± SEM, n.s., not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001; Student’s t test.
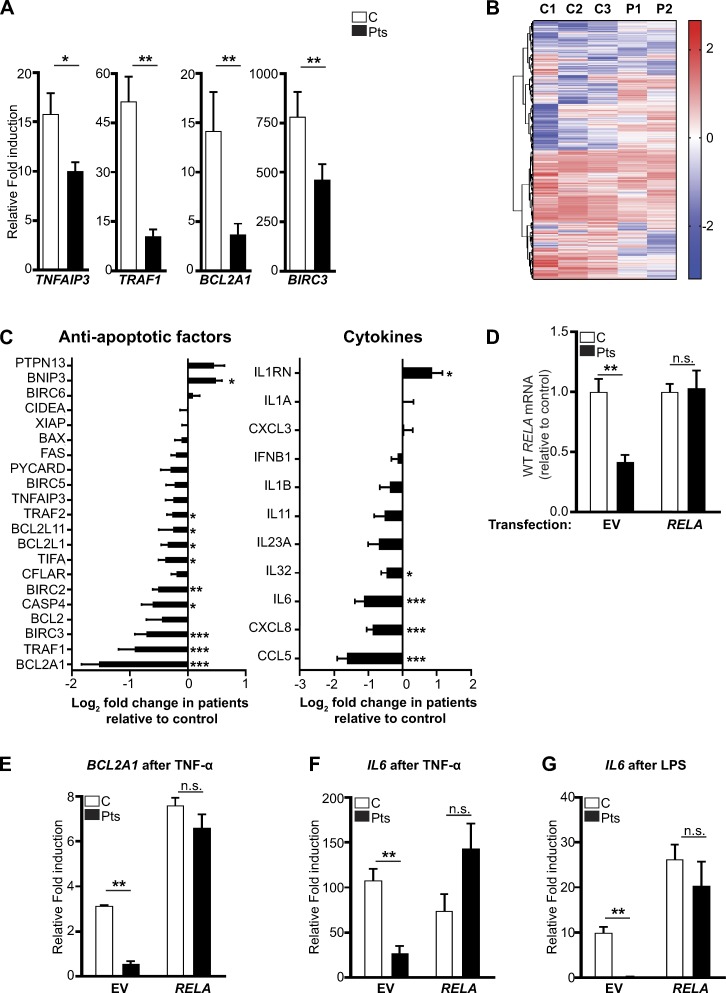
To investigate the molecular mechanisms driving the patients’ defective stromal survival, we analyzed gene expression in patient and control fibroblasts, with and without TNF stimulation. TNF-treated patient fibroblasts had decreased expression of TNF-induced protein 3 (TNFAIP3), TNF receptor–associated factor 1 (TRAF1), Bcl-2–related protein A1 (BCL2A1), and baculoviral IAP repeat-containing protein 3 (BIRC3; Fig. 3 A). Transcriptome analysis of TNF-treated fibroblasts identified 120 genes with a >1.5-fold up- or down-regulation in the patients, relative to three controls (Fig. 3 B). Most transcripts encoding NF-κB–dependent antiapoptotic proteins and cytokines were decreased in patient cells (Fig. 3 C). To validate the association between RelA haploinsufficiency and the impaired up-regulation of key NF-κB–regulated genes, we transiently nucleofected WT RELA into the patient fibroblasts. The expression of WT RelA in the patient fibroblasts restored the expression of BCL2A1 and IL-6 in response to NF-κB–activating stimuli (Fig. 3, D–G). Collectively, these data indicate that RelA haploinsufficiency results in impaired up-regulation of NF-κB antiapoptotic genes, thus providing a mechanistic rationale for the cell death induced in patient fibroblasts by in vitro TNF exposure.
Figure 3.
Decreased NF-κB regulated gene transcription in patient fibroblasts. (A) qPCR gene expression using TNF-treated fibroblasts from three controls (C) and two patients (Pts). (B) Heat map with unsupervised clustering showing the top 5% of genes with the most difference in TNF-treated fibroblasts from three controls and two patients, as determined by RNA-seq in one experiment. (C) Log2-fold change in the expression of indicated genes using RNA-seq data from two patients relative to three controls. (D) qPCR analysis of WT RELA expression in GFP+ fibroblasts from two controls and two patients after nucleofection with a vector encoding GFP or GFP-RELA. (E–G) RT-qPCR analysis of the expression of BCLA21 and IL6 in GFP+ fibroblasts from two controls and two patients after nucleofection with a vector encoding GFP or GFP-RELA and stimulated as indicated. Gene expression data in A and D–G were normalized to β-glucuronidase, expressed as the fold increase relative to unstimulated cells and were pooled from at least two independent experiments. Columns and bars represent means ± SEM. *, P < 0.05; **, P < 0.01; ***, P < 0.001; n.s., not significant.
The essential role of RelA in the maintenance of an intact epithelial–stromal cell barrier
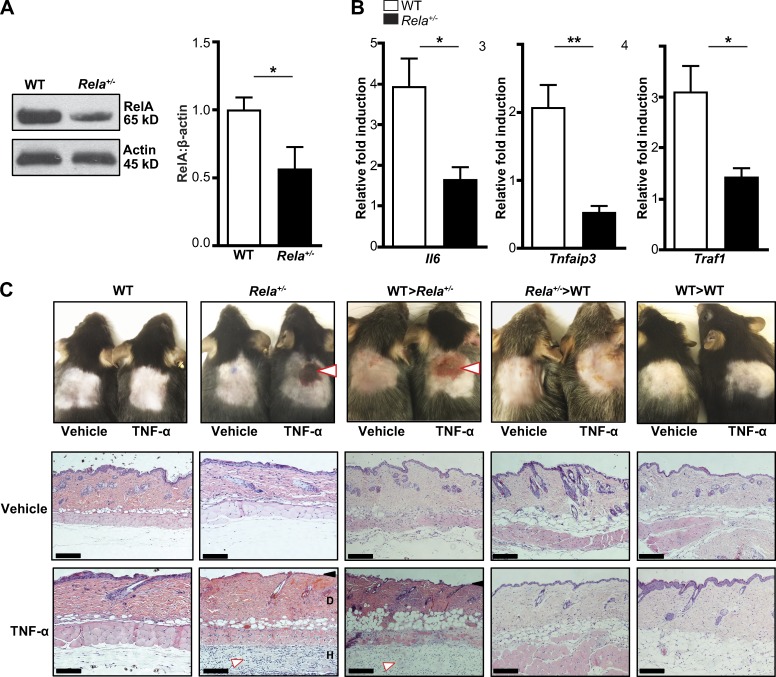
We next used Rela+/− mice to demonstrate the in vivo contribution of RelA haploinsufficiency to TNF-driven mucocutaneous ulceration. Rela+/− mice, which develop normally, have a ∼50% reduction in RelA expression compared with littermate controls (Fig. 4 A). TNF stimulation of Rela+/− splenocytes resulted in significantly impaired up-regulation of Il6, Tnfaip3, and Traf1; all which depend on NF-κB activation (Fig. 4 B). A low-dose, s.c. TNF injection had no effect on WT mice but resulted in cutaneous ulceration in Rela+/− mice, which was notable for epidermal skin loss and a predominance of neutrophils and macrophages in the dermis and hypodermis (Fig. 4 C and Table S3), consistent with the known role of TNF in the recruitment of neutrophils and macrophages to inflammatory lesions (Tsitsikov et al., 2001). To distinguish between the contribution of stromal and hematopoietic cells to the development of mucocutaneous ulceration in RelA haploinsufficiency, we created chimeras by transplanting WT bone marrow into irradiated Rela+/− recipients (WT→Rela+/−) and Rela+/− bone marrow into WT recipients (Rela+/−→WT). A s.c. TNF injection caused cutaneous ulceration in WT→Rela+/−, but not Rela+/−→WT chimeras (Fig. 4 C). Therefore, the mucosal ulceration seen in RelA haploinsufficiency results from a epithelial and stromal cell–intrinsic defect in cell survival.
Figure 4.
RelA haploinsufficient mice develop cutaneous ulceration after TNF exposure. (A) Immunoblotting for RelA in WT and Rela+/− mice (n = 8 mice per genotype, pooled from three independent experiments). (B) qPCR analysis of NF-κB–regulated genes in WT and Rela+/− splenocytes after 24 h of TNF treatment. Gene expression was normalized to β-glucuronidase and expressed as the relative fold increase compared with unstimulated cells. Data are pooled from three independent experiments (n = 6 per genotype). (C, top) Photographs of shaved skin 24 h after s.c. injection of saline (vehicle) or TNF in the indicated genotypes. White arrows note ulceration. (Bottom) Hematoxylin and eosin stain of TNF-treated skin from WT and Rela+/− mice. The black arrow indicates loss of the epidermis. The white arrow indicates the inflammatory infiltrate. D, dermis; H, hypodermis. Bars, 500 µm. Data are from one representative experiment of three independently performed experiments. Means ± SEM are shown. *, P < 0.05; **, P < 0.01; Student’s t test.
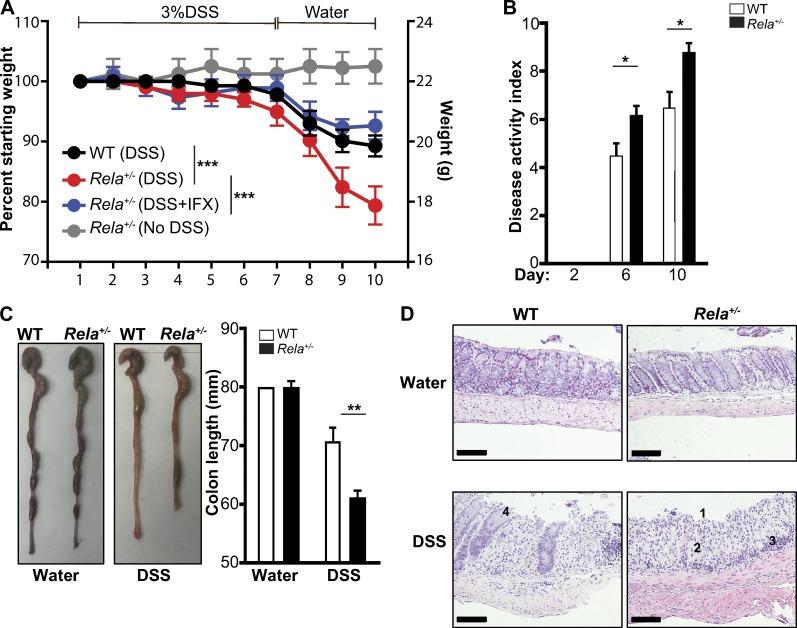
Because the proband’s ileitis responded to TNF inhibition, we assessed the contribution of TNF to gastrointestinal inflammation in Rela+/− mice. Dextran sulfate sodium (DSS)–induced colitis is a widely used model of inflammatory bowel disease, characterized by TNF release in response to mucosal injury and activation by the gastrointestinal microbiota (Alex et al., 2009; Lopetuso et al., 2013). Compared with littermate controls, Rela+/− mice developed a twofold greater weight loss and significantly worse disease activity index (DAI) requiring euthanasia (Fig. 5, A and B). Rela+/− mice had significantly shorter colons than WT littermates on d 10 (Fig. 5 C), reflecting severe colitis (Diaz-Granados et al., 2000). DSS-treated Rela+/− mice colons had severe ulceration, widespread loss of crypt architecture, and a moderate inflammatory infiltrate; control mice showed mild crypt dropout, sparse inflammation, and less-contiguous ulceration (Fig. 5 D). No differences were seen between vehicle-treated Rela+/− and WT mice. Treatment of Rela+/− mice with the TNF inhibitor infliximab led to significantly improved weight gain (Fig. 5 A), paralleling the proband’s clinical response to infliximab. Collectively, these data indicate that RelA haploinsufficiency leads to a biologically significant impairment in stromal and epithelial cell recovery in response to mucosal injury. The patients’ ulcerations occurred specifically in oral, gastrointestinal, and vaginal mucosae rich in microbiota, which may have served as inflammatory stimuli inducing TNF release, which, in turn, induces fevers and elevated inflammatory markers, mucosal injury, and finally, impaired epithelial recovery.
Figure 5.
RelA haploinsufficient mice develop significantly more severe DSS-induced colitis, which is ameliorated by TNF inhibition. (A) Weight loss in DSS-exposed WT, Rela+/−, and Rela+/− mice treated with infliximab. n = 5 mice per condition pooled from two independent experiments. ***, P < 0.001; two-way ANOVA. (B) DAI in DSS-treated WT and Rela+/− mice scores weight loss, stool consistency, and bleeding. n = 5 mice per condition pooled from two independent experiments. *, P < 0.05; Student’s t test. (C) Colon length of DSS-treated WT and Rela+/− mice at day 10. **, P < 0.01; Student’s t test. (D) Hematoxylin and eosin stain of colonic sections from DSS-treated WT and Rela+/− mice on day 10. Numbers show the following: 1, severe ulceration; 2, loss of crypt architecture; 3, inflammatory infiltrate; and 4, mild crypt dropout with sparse inflammation. Bars, 500 µm. Data in C and D are from one representative experiment of two independently performed. Bars represent means ± SEM.
Our study identifies a central role for impaired NF-κB activity in the pathogenesis of mucocutaneous disease. We show that RelA haploinsufficiency results in impaired NF-κB activation downstream of TLR and TNF stimulation, followed by impaired up-regulation of antiapoptotic genes and increased stromal cell apoptosis. Rela+/− mice and WT→Rela+/− bone marrow chimeras demonstrated cutaneous ulceration in response to TNF. Rela+/− mice developed severe DSS-induced colitis ameliorated by infliximab, thus recapitulating a key feature of the human disease.
RelA haploinsufficiency provides a counterpoint to autoinflammatory diseases characterized by increased inflammatory cytokine signaling. Defects in the genes encoding the NF-κB regulatory proteins A20 and Otulin result in NF-κB overactivation and multisystemic autoinflammation characterized by oral ulcers, arthritis, uveitis, and/or vasculitis (Damgaard et al., 2016; Zhou et al., 2016a,b). Mutations in TNFRSF1A, impairing TNF receptor 1 down-regulation, result in a periodic fever syndrome characterized by painful rashes, abdominal pain, arthritis, myalgias, rashes, and orbital edema (McDermott et al., 1999; Ciccarelli et al., 2014). In contrast, RelA haploinsufficiency is associated with isolated mucocutaneous ulceration. Our study highlights mucocutaneous ulceration as a manifestation of not only autoinflammation but also defective stromal and epithelial cell survival and impaired RelA function.
Classically, human defects in NF-κB activation, such as mutations in IKBKG, NFKBIA, and IKBKA, are associated with primary immunodeficiency because of the role of NF-κB in lymphocyte activation (Boisson et al., 2012, 2015; Pannicke et al., 2013; Zhang et al., 2017), as well as ectodermal dysplasia, lymphedema, or osteopetrosis because of its role in the development of ectodermal structures, lymphatic vessels, and osteoclasts, respectively. Mucocutaneous ulceration is not a universal finding of impaired NF-κB activation, because it was not found in the 21 reported patients with mutations in NFKB1 (Rieux-Laucat and Casanova, 2014; Fliegauf et al., 2015; Boztug et al., 2016; Zhang et al., 2017). The two generations of RelA patients have no evidence of primary immunodeficiency, which mirrors the intact lymphocyte function seen in Rela+/− mice (Erdman et al., 2001), thus providing the first evidence that stromal and epithelial cells, unlike lymphocytes, have a biallelic requirement for Rela for the maintenance of normal cell function.
Collectively, these data support a new paradigm that NF-κB functions as a rheostat governing mucosal integrity through distinct mechanisms: decreased NF-κB signaling results in decreased expression of antiapoptotic proteins important for mucosal cell recovery, whereas overactive NF-κB–mediated signaling generates a proinflammatory state. Currently, there are no biomarkers for predicting the clinical response to TNF inhibition. Assessment of NF-κB activation downstream of TLR stimulation is readily available in clinical laboratories. Future studies are needed to determine whether decreased NF-κB activation can function as a biomarker for susceptibility to TNF toxicity in patients with chronic mucocutaneous ulcers.
Materials and methods
Study oversight
The study was approved by the Boston Children’s Hospital institutional review board. Written, informed consent was obtained from the patients’ parents. Animal studies were approved by the Institutional Animal Care and Use Committee at Boston Children’s Hospital.
WES
Ten micrograms of genomic DNA were isolated from peripheral blood samples using the Gentra Puregene blood kit (QIAGEN), as per kit protocol. WES of patients 1, 2, 3, and 4 and the unaffected father was performed with an Illumina HiSeq-2000. The paired-end Illumina libraries were captured in solution according to the Agilent Technologies SureSelect protocol with 101-bp read length. The sequence data were mapped to the human reference genome (hg-19, NCBI37) using the Burrows–Wheeler Alignment method at default settings. The percentage of mapped reads was ∼99%, and mean coverage of the target regions was ∼197 times. Variants were identified with the Genome Analysis Toolkit, SAMtools, and Picard Tools (http://broadinstitute.github.io/picard/). Variants with a read coverage <2 times or Phred-scaled, single-nucleotide polymorphism quality <20 were discarded.
Sanger sequencing
Sanger sequencing was used to validate the donor splice-site variant in intron 6 of the RELA gene identified by WES in the affected family members. This was done by designing two sets of specific primers in intron 5, exon 5, and intron 6 of the RELA gene (F1: 5′-GTACTCTCCCACTTTACCACTG-3′, F2: 5′-GACTACGACCTGAATGCTGTG-3′, R1: 5′-TCCTAGAGTCATTATCGCAGT-3′, R2: 5′-AGTAGACAAATACGCAAGATG-3′).
Cell culture
Skin biopsies to generate fibroblast cell lines were collected from patients. Fibroblasts were maintained in DMEM, supplemented with 10% FBS, 50,000 U penicillin, 50,000 µg streptomycin, 10 µM HEPES, and 2 mM glutamine. PBMCs were isolated using Ficoll gradient centrifugation (GE Healthcare) and were then cultured in RPMI-1640 medium1 supplemented with 10% FBS, 50,000 U penicillin, 50,000 µg streptomycin, 10 µM HEPES, and 2 mM glutamine.
Cell stimulations and ELISA
Cells were stimulated with the described amount of the following cytokines and agonists: TNFs (R&D Systems), IL-1β (Gemini Bio-Products), Pam3CSK4 (InvivoGen), LPS (InvivoGen), flagellin (InvivoGen), and CL075 (InvivoGen). PBMCs were purified by Ficoll gradient centrifugation and were seeded at a density of 4 × 105 cell/well on a 96-well plate. Cells were then stimulated for 24 h with Pam3CSK4 (100 ng/ml), LPS (100 ng/ml), flagellin (1 µg/ml), and CL075 (2.5 µg/ml) in a total of 200 µm. Fibroblasts were seeded at a density of 104 cell/well on a 96-well plate and were then stimulated for 24 h with Pam3CSK4 (1 μg/ml), TNF-α (20 ng/ml), LPS (1 µg/ml), and IL-1β (10 ng/ml). Supernatants were collected and stored at −80°C for future analysis or were immediately analyzed for IL-6 secretion using the human IL-6 ELISA Ready-SET-Go! kit (88-7064-77; eBioscience) and IL-10 secretion using the human IL-10 ELISA MAX Deluxe kit (430604; BioLegend).
Luciferase assay
Fibroblasts from two patients and three controls were seeded at a density of 104 cell/well on a 96-well plate. Cells were transduced with the Cignal Lenti NF-κB firefly luciferase reporter (expressing the firefly luciferase gene under the control of a minimal CMV promoter and tandem repeats of the NF-κB transcriptional response element [QIAGEN]) and Renilla luciferase lentivirus at a multiplicity of inflection of 10 and 5, respectively. Cells were spun at 800 g for 1 h and were incubated at 37°C for 24 h. Medium containing the lentivirus was then removed, and fresh medium was added; 72 h after transduction, cells were treated with TNF (0.1 ng/ml) for 24 h, and luciferase activity was assessed using the Dual-Luciferase Reporter assay system (Promega), per kit protocol.
Immunoblot analysis
Cultured skin fibroblasts were homogenized in radioimmunoprecipitation assay buffer (Thermo Fisher Scientific). Proteins were separated by electrophoresis on 4–15% precast polyacrylamide gels (Bio-Rad Laboratories) and were transferred to 0.45 μm nitrocellulose membrane (Bio-Rad Laboratories). Membranes were blocked in a 1X solution of Tris-buffered saline/Tween 20 (TBST) with 5% (wt/vol) nonfat dry milk for 1 h at room temperature and then incubated overnight at 4°C with purified rabbit mAb against RelA (C22b4; Cell Signaling Technology) and diluted 1:1,000 in 1X TBST with 5% milk. As a loading control, membranes were reprobed with a purified mouse mAb against β-actin (ab3280; Abcam) and diluted 1:3,000 in 1X TBST with 5% milk. Antigen–antibody complexes were visualized with anti-rabbit or anti-mouse antibodies, respectively (GE Healthcare). Quantification of the signal intensities of RelA and β-actin bands was done using the ImageJ analyzer software (version 1.48).
RNA sequencing and transcriptome analysis
Human dermal fibroblasts from P1 and P2, as well as from three healthy controls, were treated with TNF for 24 h. RNA was prepared using RNeasy Mini kit (QIAGEN) with DNase treatment (QIAGEN). Samples were sent to the Dana Farber Cancer Institute’s Molecular Biology core facility for library preparation and sequencing. Technical duplicates with a minimum RNA integrity number score of seven were processed. cDNA was synthesized using Takara Bio Inc. SmartSeq version 4 reagents from 1 ng of RNA and fragmented to a mean size of 150 bp with a Covaris M220 ultrasonicator. Illumina standard mRNA libraries were prepared from cDNA using Rubicon Genomics ThruPLEX DNA-seq reagents, according to manufacturer’s protocol. The finished double-stranded DNA libraries were quantified and sequenced on a single Illumina NextSeq 500 run with single-end 75-bp reads. Sequenced reads were aligned to the University of California, Santa Cruz, hg9 reference genome assembly, gene counts were quantified using STAR (version 2.5.1b), and differential expression testing was performed with DESeq2 (version 1.10.1) as part of the VIPER analysis pipeline (https://bitbucket.org/cfce/viper/). Normalized read counts per kilobase were calculated using cufflinks (version 2.2.1). The normalized read counts per kilobase values were log2-transformed, and samples were normalized with respect to the median intensity for control samples. Data described in this article have been submitted to the National Center for Biotechnology Information’s Gene Expression Omnibus under accession no. GSE98624.
Gene expression analysis
After treating fibroblasts from two patients and three controls with TNF receptor (20 ng/ml), mRNA was extracted using RNeasy Mini kit (QIAGEN) and was reverse-transcribed with the iScript cDNA synthesis kit (Bio-Rad Laboratories). The expression of the mediators TNFAIP3 (Hs00234713_m1), TRAF1 (Hs01090170_m1), BCL2A1 (Hs00187845_m1), BIRC3 (Hs00985031_g1), and Il6 (Hs00174131_m1) were measured using quantitative PCR (qPCR) in a TaqMan Gene Expression assay (Applied Biosystems). The expression of these genes was analyzed using the 2-ΔΔCT method in comparison to the housekeeping gene GUSB (Hs00939627_m1). RT-PCR (QIAGEN OneStep RT-PCR kit) was used to assess RELA expression in mRNA isolated from unstimulated fibroblasts from controls and patients. A forward primer in exon 5 (5′-GAACCTGGGAATCCAGTGTGTG-3′) and a reverse primer spanning exons 7 and 8 (5′-TGAAATACACCTCAATGTCCTCTTTC-3′) were used to identify alternatively spliced products; 18S was used as an internal control and was amplified using the forward primer (5′-CGGCTACCACATCCAAGGAA-3′) and the reverse primer (5′-GCTGGAATTACCGCGGCT-3′). To assess the expression of the WT allele of RELA, Power SYBR Green Master Mix (Thermo Fisher Scientific) was used as a forward primer designed in the 3′ end of exon 6 (5′-TCTCATCCCATCTTTGACAATC-3′) and a reverse primer spanning exons 7 and 8 (5′-TGAAATACACCTCAATGTCCTCTTTC-3′). The expression was normalized to the housekeeping gene GAPDH using the forward (5′-GATCATCAGCAATGCCTCCTG-3′) and reverse primers (5′-TGCTTCACCACCTTCTTGAT-3′).
FACS for cell viability and cleaved caspase 8 activity
Fibroblasts were seeded at 105 and were treated with TNF (20 ng/ml) for 24 h. Cells were harvested and stained with annexin-V (640920; BioLegend) and propidium iodide (421301; BioLegend) for cell viability studies. To assess cleaved caspase-8 activation, after stimulation with TNF for 24 h, cells were incubated for 1 h with fluorescein isothiocyanate–conjugated IETD-FMK (88700542; eBioscience), a specific inhibitor of active caspase-8. The reagent used is cell permeable, nontoxic, and irreversibly binds to the active enzyme. The cells were also stained with annexin-V and propidium iodide. The data were analyzed with FlowJo (version 10.1; Tree Star).
Reconstitution experiments
Fibroblasts from patients 1 and 2 and from two healthy controls were nucleofected with the vectors, per kit protocol (Amaxa human dermal fibroblast nucleofector kit; Lonza). Cells were either transfected with a vector encoding GFP (EX-NEG-M61; GeneCopoeia) or a vector encoding RELA and GFP under an internal ribosomal entry site (EX-Z4808-M61; GeneCopoeia); 48 h after transfection, cells were treated with TNF (20 ng/ml), LPS (1 µg/ml), or complete medium, and 24 h later, cells were sorted for GFP positivity. RNA was isolated, cDNA was synthesized, and qPCR was performed as described in gene expression analysis.
Generation of Rela+/− mice
Mice homozygous for Relafl, possessing loxP sites flanking exon 1 of the Rela gene, were obtained from The Jackson Laboratory (B6.129S1-Relatm1Ukl/J). These mice were bred against WT mice to generate Relaf/+ mice. When these Relaf/+ mice were bred against mice possessing the cre recombinase gene under the transcriptional control of the cytomegalovirus minimal promoter (B6.C-Tg[CMV-cre]1Cgn/J; The Jackson Laboratory), the resulting progeny was born in normal mendelian ratios, and the mice were either Rela+/+ or Rela+/−. PBMCs obtained through retro-orbital vein bleeding were screened for GFP positivity to determine the mouse genotype. Mice that have undergone successful deletion of exon 1 were GFP+ve, whereas mice that are WT were GFP-ve. Because the loss of two copies of Rela results in embryonic lethality (Beg et al., 1995), any mouse that is GFP+ve is necessarily heterozygous. The genotype of the mice was further validated by immunoblotting for RelA in splenocytes of the mice using the purified rabbit mAb against RelA (C22b4; Cell Signaling Technology). Rela+/− mice had a normal life span and did not exhibit any visible abnormalities.
Generation of chimeras
Bone marrow was isolated from Rela+/− and WT mice. RBCs were lysed, and 10 million bone marrow cells were injected i.v. into the corresponding mice. Recipient mice were irradiated with 1,100 cGy for 6 h before injection with donor cells. To assess the engraftment of the chimeras, PBMCs were isolated 6 wk after transplant from the chimeric mice and were assessed for their GFP positivity. PBMCs from WT into Rela+/− mice were on average 98% GFP-ve, whereas PBMCs from Rela+/− into WT mice were on average 97% GFP+ve.
Subcutaneous injection of TNF-α
6–8-wk-old mice were shaved in the back area and injected with 1.5 µg of mouse TNF-α (PeproTech) in 75 µl of 0.9% normal saline or with 75 µl of 0.9% normal saline alone; 24 h after injection, skin from the injection area was harvested and fixed in 4% paraformaldehyde then embedded in paraffin. Tissue blocks were cut into 4-µm sections that were stained with hematoxylin and eosin. Images were acquired with a Leica DM LB2 microscope at a magnification of X400 and a Leica DFC 280 camera.
Assessment of NF-κB regulated genes in mice
Mice spleens were harvested immediately after mice were euthanized. Splenocytes were isolated by grinding moistened spleen sections between the ends of frosted microscope slides. The resultant cell suspensions were filtered through a 70-µm cell strainer (Thermo Fisher Scientific) and then counted, plated in equal numbers for all mice, and stimulated with 20 ng/ml mouse TNF for 24 h. mRNA was extracted using RNeasy Mini kit and was reverse-transcribed with the iScript cDNA synthesis kit (Bio-Rad Laboratories). The expression of the mediators Il6 (Mm00446190_m1), Tnfaip3 (Mm00437121_m1), and Traf1 (Mm00493827_m1) was measured using qPCR in a TaqMan Gene Expression Assay. The expression of these genes was analyzed using the 2-ΔΔCT method in comparison to the housekeeping gene GUSB (Mm01197698_m1).
DSS colitis
6–8-wk-old mice were introduced to 3% (wt/vol) DSS (molecular weight, 36,000-50,000; MP Biomedicals) in drinking water fed ad libitum for 7 d consecutively. Mice were assessed daily for their weight loss or clinical changes. On day 7 after induction with DSS, mice were switched to normal drinking water and were monitored for the same parameters for 3 d conescutively. A group of Rela+/− mice were administered 10 mg/kg infliximab on d 1, 3, 7, and 9 during the course of the experiment. Animals were then sacrificed by CO2 overdose and were rapidly dissected. Colons were quickly removed and cleared of feces. Colon length was measured. Small segments of the colon were taken for histopathology and were fixed in 4% paraformaldehyde for 24 h and were then embedded in paraffin and sectioned at 4-µm thickness with a paraffin microtome. The DAI was calculated daily using the following parameters as previously described (Alex et al., 2009): (a) weight loss (0 point, none; 1 point, 1–5% weight loss; 2 points, 5–10% weight loss; 3 points, 10–15% weight loss; and 4 points, >15% weight loss); (b) stool consistency (0 points, normal; 2 points, loose stools; and 4 points, watery diarrhea); and (c) bleeding per rectum (0 points, no bleeding; 2 points, slight bleeding; and 4 points, gross bleeding). Bleeding was assessed using the hemoccult routine screening test for fecal occult blood (Beckman Coulter). The DAI was calculated as the total of these scores: the sum of weight loss, stool consistency, and bleeding per rectum, resulting in the total DAI score ranging from 0 (unaffected) to 12 (severe colitis).
Statistical analysis
All data are presented as means ± SEM. Statistical comparison between two groups was evaluated using the two-tailed, unpaired Student’s t test. When comparing more than two groups one-way ANOVA was used. Statistical analysis was performed using GraphPad Prism software (version 6.0; GraphPad Software). For all experiments, P < 0.05 was considered statistically significant.
Online supplemental material
Table S1 provides the hemogram, inflammatory markers, autoantibodies, and immunologic evaluation for the proband at 5 yr old. Table S2 provides the heterozygous mutations shared among the patients identified by WES. Table S3 characterizes the cellular infiltrate in the skin of WT and Rela+/− mice after s.c. injection of TNF.
Supplementary Material
Acknowledgments
We are grateful to the patients and their family. We thank Dr. Irit Tirosh for providing clinical care and Drs. Luigi D. Notarangelo and George C. Tsokos for their insightful discussion.
This work was supported by the Perkins Fund (to R.S. Geha), National Institutes of Health grant 1K08AI116979-01 (to J. Chou), and a Jeffrey Modell Foundation Translational Research Program grant award (to J. Chou).
The authors declare no competing financial interests.
Author contributions: Y.R Badran, J.M. Leyva Castillo, W. Bainter, J.D Goldsmith, and J. Chou performed experiments and data analysis. F. Dedeoglu and A. Bousvaros collected clinical data. T.K. Ohsumi and J. Chou analyzed genomic data. Y.R. Badran, R.S. Geha and J. Chou designed the study and wrote the manuscript, which was approved by all authors.
Footnotes
Abbreviations used:
- DAI
- disease activity index
- DSS
- dextran sulfate sodium
- qPCR
- quantitative PCR
- TBST
- Tris-buffered saline/Tween 20
- WES
- whole-exome sequencing
References
- Alcamo E., Mizgerd J.P., Horwitz B.H., Bronson R., Beg A.A., Scott M., Doerschuk C.M., Hynes R.O., and Baltimore D.. 2001. Targeted mutation of TNF receptor I rescues the RelA-deficient mouse and reveals a critical role for NF-κB in leukocyte recruitment. J. Immunol. 167:1592–1600. 10.4049/jimmunol.167.3.1592 [DOI] [PubMed] [Google Scholar]
- Alex P., Zachos N.C., Nguyen T., Gonzales L., Chen T.-E., Conklin L.S., Centola M., and Li X.. 2009. Distinct cytokine patterns identified from multiplex profiles of murine DSS and TNBS-induced colitis. Inflamm. Bowel Dis. 15:341–352. 10.1002/ibd.20753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atreya I., Atreya R., and Neurath M.F.. 2008. NF-kappaB in inflammatory bowel disease. J. Intern. Med. 263:591–596. 10.1111/j.1365-2796.2008.01953.x [DOI] [PubMed] [Google Scholar]
- Beg A.A., Sha W.C., Bronson R.T., Ghosh S., and Baltimore D.. 1995. Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-kappa B. Nature. 376:167–170. 10.1038/376167a0 [DOI] [PubMed] [Google Scholar]
- Boisson B., Laplantine E., Prando C., Giliani S., Israelsson E., Xu Z., Abhyankar A., Israël L., Trevejo-Nunez G., Bogunovic D., et al. . 2012. Immunodeficiency, autoinflammation and amylopectinosis in humans with inherited HOIL-1 and LUBAC deficiency. Nat. Immunol. 13:1178–1186. 10.1038/ni.2457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisson B., Laplantine E., Dobbs K., Cobat A., Tarantino N., Hazen M., Lidov H.G., Hopkins G., Du L., Belkadi A., et al. . 2015. Human HOIP and LUBAC deficiency underlies autoinflammation, immunodeficiency, amylopectinosis, and lymphangiectasia. J. Exp. Med. 212:939–951. 10.1084/jem.20141130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boztug H., Hirschmugl T., Holter W., Lakatos K., Kager L., Trapin D., Pickl W., Förster-Waldl E., and Boztug K.. 2016. NF-κB1 haploinsufficiency causing Immunodeficiency and EBV-driven lymphoproliferation. J. Clin. Immunol. 36:533–540. 10.1007/s10875-016-0306-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner D., Blaser H., and Mak T.W.. 2015. Regulation of tumour necrosis factor signalling: live or let die. Nat. Rev. Immunol. 15:362–374. 10.1038/nri3834 [DOI] [PubMed] [Google Scholar]
- Cao S., Zhang X., Edwards J.P., and Mosser D.M.. 2006. NF-κB1 (p50) homodimers differentially regulate pro- and anti-inflammatory cytokines in macrophages. J. Biol. Chem. 281:26041–26050. 10.1074/jbc.M602222200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarelli F., De Martinis M., and Ginaldi L.. 2014. An update on autoinflammatory diseases. Curr. Med. Chem. 21:261–269. 10.2174/09298673113206660303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damgaard R.B., Walker J.A., Marco-Casanova P., Morgan N.V., Titheradge H.L., Elliott P.R., McHale D., Maher E.R., McKenzie A.N.J., and Komander D.. 2016. The deubiquitinase OTULIN is an essential negative regulator of inflammation and autoimmunity. Cell. 166:1215–1230.e20. 10.1016/j.cell.2016.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Granados N., Howe K., Lu J., and McKay D.M.. 2000. Dextran sulfate sodium-induced colonic histopathology, but not altered epithelial ion transport, is reduced by inhibition of phosphodiesterase activity. Am. J. Pathol. 156:2169–2177. 10.1016/S0002-9440(10)65087-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdman S.E., Fox J.G., Dangler C.A., Feldman D., and Horwitz B.H.. 2001. Cutting edge: typhlocolitis in NF-κB-deficient mice. J. Immunol. 166:1443–1447. 10.4049/jimmunol.166.3.1443 [DOI] [PubMed] [Google Scholar]
- Fliegauf M., Bryant V.L., Frede N., Slade C., Woon S.-T., Lehnert K., Winzer S., Bulashevska A., Scerri T., Leung E., et al. . 2015. Haploinsufficiency of the NF-κB1 subunit p50 in common variable immunodeficiency. Am. J. Hum. Genet. 97:389–403. 10.1016/j.ajhg.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden M.S., and Ghosh S.. 2012. NF-κB, the first quarter-century: remarkable progress and outstanding questions. Genes Dev. 26:203–234. 10.1101/gad.183434.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lek M., Karczewski K.J., Minikel E.V., Samocha K.E., Banks E., Fennell T., O’Donnell-Luria A.H., Ware J.S., Hill A.J., Cummings B.B., et al. Exome Aggregation Consortium . 2016. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 536:285–291. 10.1038/nature19057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopetuso L.R., Petito V., Cufino V., Arena V., Stigliano E., Gerardi V., Gaetani E., Poscia A., Amato A., Cammarota G., et al. . 2013. Locally injected Infliximab ameliorates murine DSS colitis: differences in serum and intestinal levels of drug between healthy and colitic mice. Dig. Liver Dis. 45:1017–1021. 10.1016/j.dld.2013.06.007 [DOI] [PubMed] [Google Scholar]
- McDermott M.F., Aksentijevich I., Galon J., McDermott E.M., Ogunkolade B.W., Centola M., Mansfield E., Gadina M., Karenko L., Pettersson T., et al. . 1999. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell. 97:133–144. 10.1016/S0092-8674(00)80721-7 [DOI] [PubMed] [Google Scholar]
- Nenci A., Becker C., Wullaert A., Gareus R., van Loo G., Danese S., Huth M., Nikolaev A., Neufert C., Madison B., et al. . 2007. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature. 446:557–561. 10.1038/nature05698 [DOI] [PubMed] [Google Scholar]
- Neurath M.F., Pettersson S., Meyer zum Büschenfelde K.H., and Strober W.. 1996. Local administration of antisense phosphorothioate oligonucleotides to the p65 subunit of NF-κB abrogates established experimental colitis in mice. Nat. Med. 2:998–1004. 10.1038/nm0996-998 [DOI] [PubMed] [Google Scholar]
- Olesen C.M., Coskun M., Peyrin-Biroulet L., and Nielsen O.H.. 2016. Mechanisms behind efficacy of tumor necrosis factor inhibitors in inflammatory bowel diseases. Pharmacol. Ther. 159:110–119. 10.1016/j.pharmthera.2016.01.001 [DOI] [PubMed] [Google Scholar]
- Pannicke U., Baumann B., Fuchs S., Henneke P., Rensing-Ehl A., Rizzi M., Janda A., Hese K., Schlesier M., Holzmann K., et al. . 2013. Deficiency of innate and acquired immunity caused by an IKBKB mutation. N. Engl. J. Med. 369:2504–2514. 10.1056/NEJMoa1309199 [DOI] [PubMed] [Google Scholar]
- Rieux-Laucat F., and Casanova J.-L.. 2014. Autoimmunity by haploinsufficiency. Science. 345:1560–1561. 10.1126/science.1260791 [DOI] [PubMed] [Google Scholar]
- Tsitsikov E.N., Laouini D., Dunn I.F., Sannikova T.Y., Davidson L., Alt F.W., and Geha R.S.. 2001. TRAF1 is a negative regulator of TNF signaling. enhanced TNF signaling in TRAF1-deficient mice. Immunity. 15:647–657. 10.1016/S1074-7613(01)00207-2 [DOI] [PubMed] [Google Scholar]
- Vitale A., Rigante D., Lucherini O.M., Caso F., Muscari I., Magnotti F., Brizi M.G., Guerrini S., Patti M., Punzi L., et al. . 2013. Biological treatments: new weapons in the management of monogenic autoinflammatory disorders. Mediators Inflamm. 2013:939847 10.1155/2013/939847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Walia B., Evans J., Gewirtz A.T., Merlin D., and Sitaraman S.V.. 2003. IL-6 induces NF-κB activation in the intestinal epithelia. J. Immunol. 171:3194–3201. 10.4049/jimmunol.171.6.3194 [DOI] [PubMed] [Google Scholar]
- Zaph C., Troy A.E., Taylor B.C., Berman-Booty L.D., Guild K.J., Du Y., Yost E.A., Gruber A.D., May M.J., Greten F.R., et al. . 2007. Epithelial-cell-intrinsic IKK-β expression regulates intestinal immune homeostasis. Nature. 446:552–556. 10.1038/nature05590 [DOI] [PubMed] [Google Scholar]
- Zhang Q., Lenardo M.J., and Baltimore D.. 2017. 30 Years of NF-κB: a blossoming of relevance to human pathobiology. Cell. 168:37–57. 10.1016/j.cell.2016.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou A., Scoggin S., Gaynor R.B., and Williams N.S.. 2003. Identification of NF-κB–regulated genes induced by TNFα utilizing expression profiling and RNA interference. Oncogene. 22:2054–2064. 10.1038/sj.onc.1206262 [DOI] [PubMed] [Google Scholar]
- Zhou Q., Wang H., Schwartz D.M., Stoffels M., Park Y.H., Zhang Y., Yang D., Demirkaya E., Takeuchi M., Tsai W.L., et al. . 2016a Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat. Genet. 48:67–73. 10.1038/ng.3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q., Yu X., Demirkaya E., Deuitch N., Stone D., Tsai W.L., Kuehn H.S., Wang H., Yang D., Park Y.H., et al. . 2016b Biallelic hypomorphic mutations in a linear deubiquitinase define otulipenia, an early-onset autoinflammatory disease. Proc. Natl. Acad. Sci. USA. 113:10127–10132. 10.1073/pnas.1612594113 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.