Flt3 expression is absent in the large majority of phenotypic hematopoietic stem cells (HSCs). Mead et al. show that FLT3-ITD–driven myeloproliferation causes cell-extrinsic suppression of the normal HSC reservoir through disruption of HSC-supporting BM stromal cells, including overexpression of TNF.
Abstract
Although previous studies suggested that the expression of FMS-like tyrosine kinase 3 (Flt3) initiates downstream of mouse hematopoietic stem cells (HSCs), FLT3 internal tandem duplications (FLT3 ITDs) have recently been suggested to intrinsically suppress HSCs. Herein, single-cell interrogation found Flt3 mRNA expression to be absent in the large majority of phenotypic HSCs, with a strong negative correlation between Flt3 and HSC-associated gene expression. Flt3-ITD knock-in mice showed reduced numbers of phenotypic HSCs, with an even more severe loss of long-term repopulating HSCs, likely reflecting the presence of non-HSCs within the phenotypic HSC compartment. Competitive transplantation experiments established that Flt3-ITD compromises HSCs through an extrinsically mediated mechanism of disrupting HSC-supporting bone marrow stromal cells, with reduced numbers of endothelial and mesenchymal stromal cells showing increased inflammation-associated gene expression. Tumor necrosis factor (TNF), a cell-extrinsic potent negative regulator of HSCs, was overexpressed in bone marrow niche cells from FLT3-ITD mice, and anti-TNF treatment partially rescued the HSC phenotype. These findings, which establish that Flt3-ITD–driven myeloproliferation results in cell-extrinsic suppression of the normal HSC reservoir, are of relevance for several aspects of acute myeloid leukemia biology.
Introduction
Suppression and collapse of normal blood cell replenishment underlies the severe morbidity and high mortality accompanying many hematologic malignancies, including acute myeloid leukemia (AML; Löwenberg et al., 1999). However, the intrinsic and extrinsic cellular and molecular mechanisms responsible for this suppression of normal hematopoiesis remain to be established and are of critical importance toward development of improved and targeted therapies.
Studies of the surface expression and function of FMS-like tyrosine kinase 3 (Flt3) have provided fundamental insights into its role in normal hematopoiesis (Luc et al., 2007; Boyer et al., 2012). Within the hematopoietic progenitor compartment, expression of Flt3 is present in multipotent progenitors (MPPs), including lymphoid-primed MPPs (LMPPs; Adolfsson et al., 2001, 2005; Boyer et al., 2011; Buza-Vidas et al., 2011) and early lymphoid (Luc et al., 2012) and myeloid (Böiers et al., 2010) progenitor populations. Genetic knockout approaches established an important role for Flt3 in the maintenance of these early progenitor cell populations (Sitnicka et al., 2002; Böiers et al., 2010). In contrast, up-regulation of surface expression of Flt3 marks loss of self-renewal of mouse hematopoietic stem cells (HSCs; Adolfsson et al., 2001; Christensen and Weissman, 2001), and importantly, genetic knockout studies of Flt3, or its ligand, have demonstrated no significant impact of loss of Flt3 on the normal HSC compartment (Buza-Vidas et al., 2009). Moreover, lineage-tracing experiments demonstrated that although Flt3 transcriptional expression first occurs in a minor population of cells within the phenotypic HSC compartment, these cells in fact lack self-renewal capability and therefore represent progenitors rather than bona fide HSCs (Boyer et al., 2011, 2012; Buza-Vidas et al., 2011). Those results highlight the well-recognized heterogeneity of the phenotypic HSC compartment, which in addition to genuine HSCs contains non-HSC progenitors, marked in part by expression of Flt3 transcript (Purton and Scadden, 2007; Boyer et al., 2011; Buza-Vidas et al., 2011).
Constitutively activating internal tandem duplications (ITDs) of FLT3 are one of the most common, recurrent somatic mutations found in patients with AML (Meshinchi and Appelbaum, 2009). Although FLT3 ITDs often occur as a secondary mutation (Gale et al., 2008), there are also cases in which they clearly originate in the founding leukemic clone (Ding et al., 2012), and it is clear that FLT3 ITDs act as a potent driver mutation (Smith et al., 2012) and confer a poor outcome because of high relapse risk (Gale et al., 2008). Thus, it is of considerable importance to understand which cells propagate FLT3-ITD–associated myeloid disease and how these cells contribute to clonal dominance over normal hematopoietic cells to result in the hematopoietic suppression typically observed in patients (Löwenberg et al., 1999). Although FLT3-ITD mutations are present in the primitive human CD34+CD38− stem/progenitor cell compartment, including LMPP-like cells (Levis et al., 2005; Goardon et al., 2011; Mead et al., 2013), FLT3 ITDs appear to be absent in the majority of “preleukemic” HSCs in patients with FLT3-ITD AML (Jan et al., 2012). However, in a recent study of Flt3-ITD knock-in mice in which phenotypic HSCs were reduced, Flt3 mRNA was found to be expressed in the phenotypically defined HSC compartment when analyzed at the cell population level (Chu et al., 2012), and based on this and other findings, it was concluded that a HSC-intrinsic mechanism is responsible for the observed HSC suppression in Flt3-ITD mice (Chu et al., 2012). Importantly, this implicates a previously unrecognized HSC-intrinsic role for Flt3 and Flt3-ITD in governing the dynamics of the HSC compartment and potentially radically revises our understanding of the role of Flt3 in normal hematopoiesis and the impact of FLT3-ITDs on HSCs in hematologic malignancies.
Because a definitive description of the heterogeneous expression pattern of Flt3 is important for understanding the physiological role of the receptor and the potential intrinsic impact of Flt3-ITD in HSC homeostasis, we herein explored Flt3 expression at the transcriptional and protein levels in the phenotypically defined HSC compartment at the single-cell level. We then explored whether the observed HSC suppression in Flt3-ITD mice might rather involve an HSC-extrinsic mechanism, including an impact on components of the HSC niche.
Results
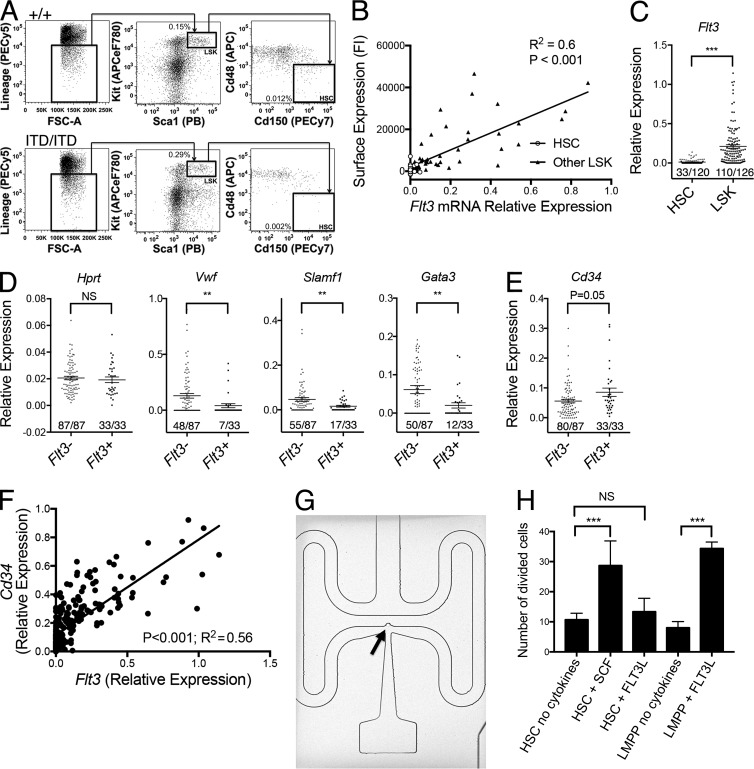
Flt3 mRNA is expressed only in a small and distinct subset of phenotypically defined mouse HSCs
We first sought to investigate heterogeneity of Flt3 expression in phenotypically defined HSCs, by determining the relationship between Flt3 mRNA and cell-surface Flt3 protein expression at the single-cell level. Index FACS of 90 WT (Flt3+/+) Lin−Sca1+Kit+ (LSK) cells (Fig. 1 A), encompassing all HSCs as well as distinct subpopulations of MPPs, showed a significant correlation between surface Flt3 protein and Flt3 mRNA expression in the same single cells (Fig. 1 B; P < 0.001). All 28 LSK cells within the stringent phenotypic HSC compartment (LSKCD150+48−) clearly showed much lower expression of both Flt3 protein and Flt3 mRNA than other LSK cells (Fig. 1 C). Gene expression analysis of 120 single LSKCD150+48− cells and 126 single LSK cells not residing in the LSKCD150+48− HSC compartment showed that as many as 72% of LSKCD150+48− cells did not express any detectable Flt3 at the single-cell level as opposed to only 13% of other (MPP) LSK cells (Fig. 1 C; P < 0.001). Moreover, the minority of phenotypic HSCs expressing Flt3 mRNA did so at a much lower level than did other (MPP) LSK cells (Fig. 1 C; P < 0.001). Single-cell gene expression analysis of HSCs stratified according to presence (n = 33) or absence (n = 87) of Flt3 expression revealed reduced frequencies and/or levels of expression of key stem cell–associated genes (Vwf, Slamf1, and Gata3; Fig. 1 D) in Flt3 mRNA–positive cells. Indeed, only 7 of 55 (13%) Vwf-expressing LSKCD150+48− HSCs, which reside at the apex of the hematopoietic hierarchy (Sanjuan-Pla et al., 2013), showed detectable Flt3 mRNA expression. Further, Flt3 mRNA–negative HSCs showed reduced Cd34 mRNA expression, characteristic of adult mouse HSCs (Osawa et al., 1996; P = 0.05; Fig. 1 E), with strong correlation between Flt3 and Cd34 mRNA expression in LSK cells (P < 0.001, Fig. 1 F). Together, these findings support that within the phenotypic HSC compartment, expression of Flt3 mRNA correlates with loss of HSC-associated gene expression programs. Importantly, gene expression of single LSKCD150+48− cells captured in nanofluidic reaction chambers (Fig. 1 G), with sensitivity for gene expression detection to the single-molecule level (Wu et al., 2014), showed that 12 of 17 (71%) captured LSKCD150+48− cells did not express any Flt3 mRNA, supporting that the absence of Flt3 expression is unlikely to represent a lack of sensitivity of the assay.
Figure 1.
Single-cell analysis of the phenotypic HSC compartment. (A) Representative flow cytometry–based analysis and quantification of LSK cells and phenotypic (LSKCD150+CD48−) HSCs in 8–10-wk-old Flt3+/+ and Flt3ITD/ITD mice. Shown are the mean values for the frequencies (percentage of total BM cells) of the indicated population across all experiments (+/+, n = 31 mice; ITD/ITD, n = 23 mice). (B) Correlation of Flt3 protein cell-surface expression (fluorescence intensity; FI) and Flt3 relative mRNA gene expression level in 28 phenotypic (LSKCD150+48−) HSCs (open circles) and 62 single non-HSC LSK cells (filled triangles) from two 8-wk-old Flt3+/+ mice. P-value represents Pearson correlation coefficient. (C) Flt3 relative mRNA gene expression level in 120 LSKCD150+48− HSCs and 126 single non-HSC LSK cells from 8-wk-old Flt3+/+ mice (n = 5 mice). P-value at the top of the graph represents unpaired t test; the x/y figures beneath each dot plot indicate the number of cells demonstrating amplification for indicated gene (x) and total numbers of cells analyzed (y). (D) Relative mRNA gene expression level of Hprt, Vwf, Slamf1, and Gata3 in 120 LSKCD150+48− HSCs from 8-wk-old Flt3+/+ mice stratified according to presence (n = 33) or absence (n = 87) of Flt3 expression (n = 5 mice). (E) Relative mRNA gene expression level of Cd34 in 120 LSKCD150+48− HSCs from 8-wk-old Flt3+/+ mice stratified according to presence (n = 33) or absence (n = 87) of Flt3 expression (n = 5 mice). (F) Correlation of Flt3 and Cd34 relative mRNA gene expression level in 120 phenotypic HSCs and 126 single non-HSC LSKs from 8-wk-old Flt3+/+ mice (n = 5 mice). (G) Single mouse phenotypic HSC (arrow) captured in a 4.5-nl reaction chamber for single-cell gene expression analysis (representative image from one experiment). (H) Number of cells undergoing cell division after incubation of 180 single LSKCD150+48− HSCs or LSKFlt3high LMPPs under the indicated conditions for 5 d followed by culture in a full cytokine cocktail (see Materials and Methods) for a further 10 d. SCF indicates stem cell factor, and FLT3L indicates FLT3 ligand. Three independent experiments with 60 cells per experiment. P-values represent χ2 analysis comparing frequency of cells undergoing cell division of a total of 180 plated cells in the three experiments. Data are shown as mean (SEM) values. **, P < 0.01; ***, P < 0.001. NS, not significant.
To confirm that LSKCD150+48− cells were not functionally responsive to FLT3 ligand (FLT3L), we cultured single LSKCD150+48− cells in the absence of cytokines or in the presence of FLT3L or stem cell factor (SCF), the ligand for c-kit shown to be highly expressed on HSCs (Ikuta and Weissman, 1992). Importantly, both of these cytokines have been shown to act as potent viability factors for stem and progenitor cells expressing the corresponding receptors (Veiby et al., 1996). After a 5-d preincubation period, we added a strongly proliferative cytokine cocktail to promote the proliferation of cells that had survived the preincubation period, thereby assessing the ability of SCF and FLT3L to act as viability factors for LSKCD150+48−-enriched HSCs. In agreement with previous studies (Yang et al., 2005), SCF markedly promoted the survival of LSKCD150+48−-enriched HSCs (Fig. 1 H). In marked contrast, FLT3L had no ability to enhance survival of LSKCD150+48− cells, although in agreement with previous studies (Adolfsson et al., 2001), it potently enhanced survival of LSKFlt3high LMPPs (Fig. 1 H). Together, these data along with previous studies (Adolfsson et al., 2001; Christensen and Weissman, 2001; Boyer et al., 2011, 2012; Buza-Vidas et al., 2011), provide several lines of evidence supporting that Flt3 is not expressed at functionally relevant levels in bona fide mouse HSCs.
Flt3-ITD–induced myeloproliferation results in a progressive loss of Flt3 mRNA–negative HSCs
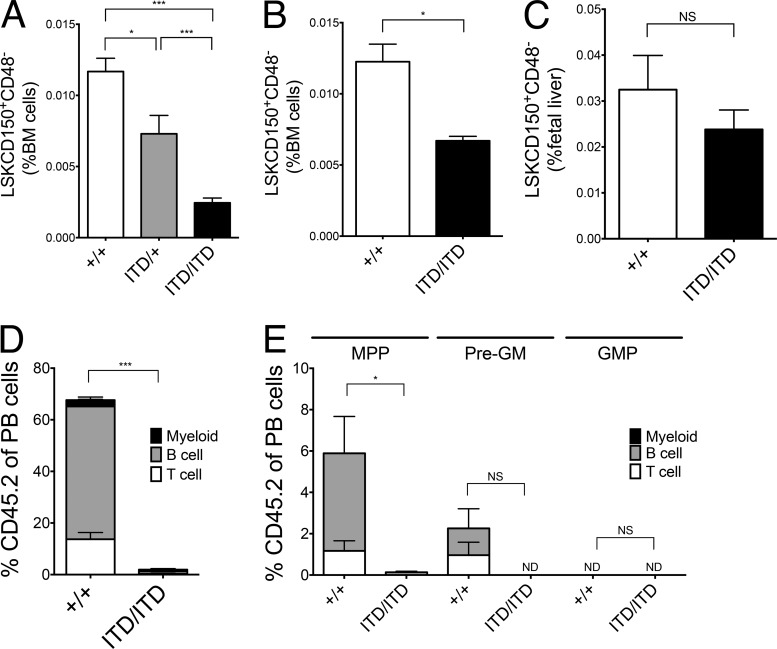
Despite the expansion of LSK cells in Flt3-ITD mice (Lee et al., 2007; Kharazi et al., 2011), there was a gene dosage–dependent reduction of LSKCD150+48− phenotypic HSCs in the BM of Flt3-ITD mice (Fig. 2 A; P < 0.001) that paralleled the increased severity of myeloproliferation in homozygous mice (Kharazi et al., 2011). The loss of phenotypic HSCs in Flt3ITD/ITD mice occurred progressively and in parallel to the development of myeloproliferation (Lee et al., 2007), with a mild HSC phenotype already apparent in 2-wk-old mice (Fig. 2 B); notably, LSKCD150+48− cells were present at normal numbers in Flt3-ITD fetal livers (FLs) before the development of overt myeloid disease (Fig. 2 C; Mead et al., 2013). Transplantation of 500,000 BM cells from 8–10-wk-old Flt3+/+ or Flt3ITD/ITD (CD45.2) mice together with 200,000 WT (CD45.1) BM cells showed a profound loss of functional/repopulating HSCs as defined by multilineage reconstitution (Fig. 2 D). Because 500,000 Flt3ITD/ITD BM cells will include 10–15 phenotypic HSCs for each recipient mouse, the failure to observe significant engraftment in any recipient mouse (n = 15) was surprising. Furthermore, transplantation of large numbers of cells purified from the expanded progenitor populations also failed to sustain long-term Flt3ITD/ITD myeloproliferation (Fig. 2 E). Together, these data support that the BM of Flt3ITD/ITD mice contains very few long-term repopulating HSCs.
Figure 2.
Flt3-ITDs cause gene dosage–dependent and progressive suppression of BM HSCs. (A) Gene dosage–dependent reduction in LSKCD150+48− cells in 8–10-wk-old Flt3+/+, Flt3ITD/+, and Flt3ITD/ITD mice (+/+, n = 31; ITD/+, n = 14; ITD/ITD, n = 23). (B) Reduction in LSKCD150+48− cells in 2-wk-old Flt3ITD/ITD mice (+/+, n = 4; ITD/ITD, n = 6). (C) Numbers of phenotypic (LSKCD150+CD48−) HSCs in E15 FL from Flt3+/+ and Flt3ITD/ITD mice (+/+, n = 8; ITD/ITD, n = 9). (D) Percentage CD45.2 chimerism in peripheral blood of recipient mice 16 wk after transplantation of 500,000 unfractionated CD45.2 BM cells and 200,000 CD45.1 WT competitor cells (eight to nine recipients per genotype in three experiments). (E) Percentage CD45.2 chimerism in BM of recipient (CD45.1) mice 16 wk after transplantation of 5,000 CD45.2 MPPs (LSKCD150−CD48+), pre-GM (Lin−Kit+Sca1−CD41−CD16/32−CD150−CD105−), and GMPs (Lin−Kit+Sca1−CD41−CD16/32+) together with 200,000 CD45.1 WT BM competitor cells (eight to nine recipients per genotype in two experiments). Data are shown as mean (SEM) values. *, P < 0.05; ***, P < 0.001 by t test. NS, not significant.
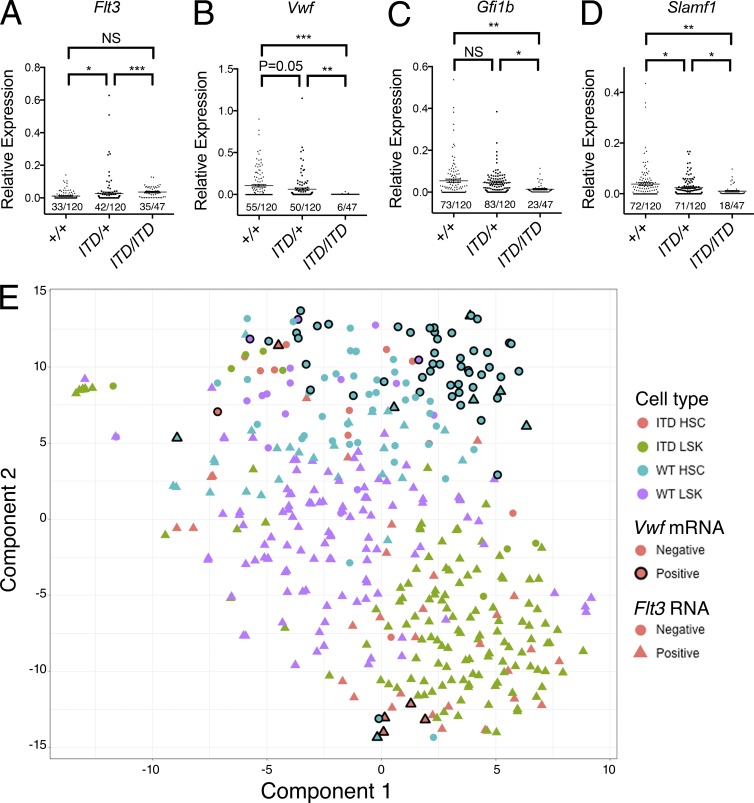
To explore the discrepancy between phenotypic (LSKCD150+48−) and long-term repopulating HSCs in Flt3ITD/ITD mice, we performed single-cell gene expression analysis on the cells residing in the phenotypic HSC compartment in Flt3-ITD mice. This analysis showed increased frequency of Flt3 expression in single LSKCD150+48− cells in Flt3-ITD mice, with 28, 35, and 74% of cells showing Flt3 expression in Flt3+/+, Flt3ITD/+, and Flt3ITD/ITD mice, respectively (P < 0.001, Fig. 3 A), in keeping with a relative preservation (less than twofold reduction) of Flt3-ITD–expressing LSKCD150+48− cells in Flt3ITD/ITD mice, as opposed to a 13-fold reduction of Flt3 mRNA-negative LSKCD150+48− cells. The disrupted composition of the HSC compartment in Flt3ITD/ITD mice was accompanied by reduced frequencies and levels of expression of the HSC-affiliated genes Vwf, Gfi1b, and Slamf1 in Flt3ITD/+ and Flt3ITD/ITD HSCs (Fig. 3, B–D), consistent with a 17-fold reduction of Vwf mRNA–positive HSCs in Flt3ITD/ITD mice, despite 87% of these cells not expressing any Flt3. Furthermore, t-distributed stochastic neighbor embedding (t-SNE) analysis clearly demonstrated that most cells residing in the phenotypic HSC compartment in Flt3ITD/ITD mice clustered more closely with LSK progenitor cells than with HSCs (Fig. 3 E). To confirm the distinct clustering of HSCs from Flt3ITD/ITD mice, we performed hierarchical clustering analysis. After excluding a small number of cells falling into a minor cluster, this analysis identified two major clusters of cells. The first HSC cluster contained 98 of 119 (82%) phenotypic WT HSCs but only 12 of 47 (26%) phenotypic Flt3ITD/ITD HSCs (P < 0.001). The LSK cluster contained 216 of 250 (86%) Flt3+/+ and Flt3ITD/ITD LSKs. Crucially, 35 of 47 (74%) phenotypic Flt3ITD/ITD HSCs were contained within this LSK cluster versus only 21 of 119 (18%) Flt3+/+ HSCs (P < 0.001).
Figure 3.
The cellular composition of the phenotypic HSC compartment is severely disrupted in Flt3-ITD mice. (A–D) Relative mRNA gene expression level for Flt3 (A), Vwf (B), Gfi1b (C), and Slamf1 (D) in LSKCD150+48− single cells from 8-wk-old Flt3+/+ (n = 120), Flt3ITD/+ (n = 120), and Flt3ITD/ITD (n = 47) mice (n = 3–5 mice for each genotype). The x/y figures beneath each dot plot indicate the number of cells demonstrating amplification for indicated gene (x) and total numbers of cells analyzed (y). (E) t-SNE analysis demonstrating distinct clustering of HSCs and total LSK cells from Flt3+/+ and Flt3ITD/ITD mice. Color of each point indicates cell type: red, Flt3ITD/ITD HSC (n = 47); green, Flt3ITD/ITD LSK (n = 133); blue, Flt3+/+ HSC (n = 120); and purple, Flt3+/+ LSK (n = 126). Presence (triangles) or absence (circles) of Flt3 mRNA and presence (black border) or absence (no border) of Vwf mRNA is also indicated. The large majority of phenotypic HSCs from Flt3ITD/ITD mice cluster together with LSK progenitor cells and are clearly separated from Vwf mRNA–positive Flt3+/+ HSCs. Data are shown as mean (SEM) values. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by t test. NS, not significant.
Together, these data demonstrate a selective and profound depletion of Vwf-positive and Flt3 mRNA–negative LSKCD150+48− cells (likely to represent bona fide functional HSCs) and relative preservation of Flt3-expressing LSKCD150+48− cells with reduced expression of HSC-affiliated genes (likely to represent contaminating progenitor cells). These data are in keeping with the LSKCD150+48− compartment in Flt3ITD/ITD mice being primarily composed of “contaminating” Flt3-expressing progenitor cells rather than HSCs, helping to explain the failure to observe any long-term engraftment after transplantation of Flt3ITD/ITD BM despite only a moderate reduction in the LSKCD150+48− compartment.
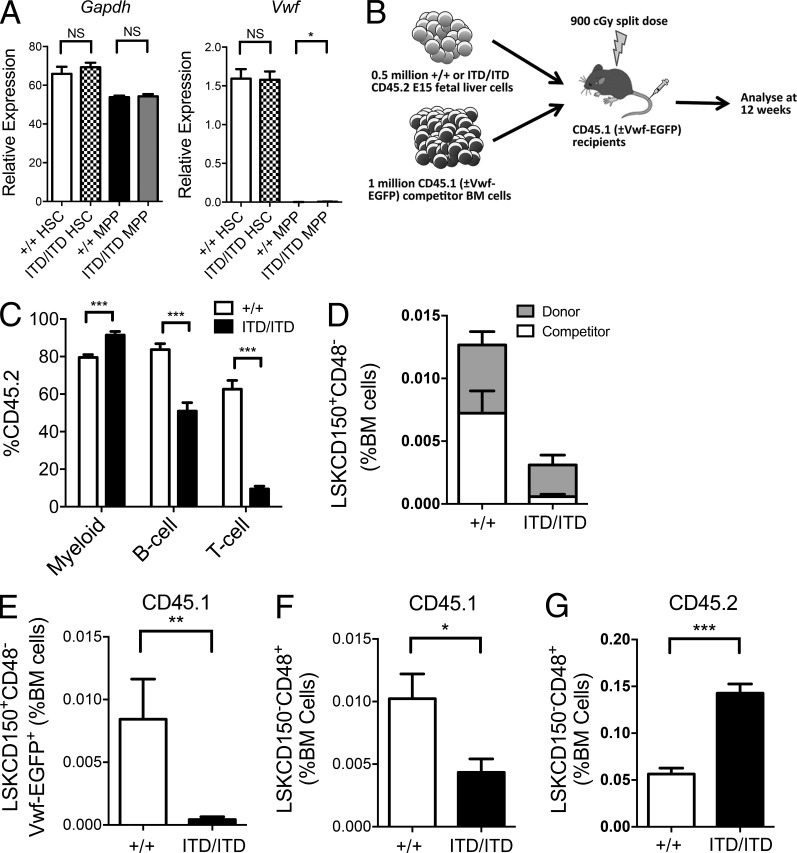
The loss of HSCs in Flt3ITD/ITD mice involves cell-extrinsic mechanisms
The lack of Flt3 mRNA expression in the majority of phenotypic HSCs is inconsistent with the proposed cell-intrinsic role for aberrant Flt3 signaling as an explanation for the marked suppression of the HSC compartment in Flt3ITD/ITD mice (Chu et al., 2012). The dramatic reduction of non–Flt3-expressing LSKCD150+48− HSCs in Flt3-ITD mice appeared more compatible with the observed HSC suppression being mediated through an HSC-extrinsic mechanism. To explore this, we performed competitive transplantation experiments using Flt3-ITD FL cells (CD45.2), because they contain normal numbers of LSKCD150+48− cells (Fig. 2 C) expressing normal levels of Vwf (Fig. 4 A), in keeping with an intact HSC compartment. Importantly, WT BM competitor (CD45.1) cells were cotransplanted to determine the extrinsic impact of Flt3-ITD on WT HSCs (Fig. 4 B). Unlike Flt3ITD/ITD BM cells, Flt3ITD/ITD FL cells showed robust engraftment and recapitulated Flt3-ITD–induced myeloproliferation (Fig. 4 C). Flt3ITD/ITD donor cells dominated hematopoiesis, with increased myeloid engraftment in comparison with WT FL transplanted mice (P < 0.001; Fig. 4 C), but reduced lymphoid engraftment (P < 0.001; Fig. 4 C) in keeping with the myeloid bias of Flt3ITD/ITD MPPs (Mead et al., 2013). Most notably, not only Flt3ITD/ITD donor but also WT competitor LSKCD150+48− HSC-enriched cells were markedly reduced in recipient mice (Fig. 4 D), conclusively demonstrating that Flt3-ITD–expressing cells exert an extensive extrinsic suppression of the WT LSKCD150+48− HSC compartment. In fact, the observed reduction of LSKCD150+48− cells was more extensive in the WT (CD45.1) competitor BM than in the Flt3ITD/ITD donor cells, including vWF-EGFP–positive competitor HSCs (20-fold reduction; P < 0.01; Fig. 4 E), compatible with the observed HSC suppression being entirely HSC-extrinsically mediated. Also, competitor WT LSKCD150−48+ MPPs were reduced in Flt3ITD/ITD-engrafted mice, although less than HSCs (Fig. 4 F); in striking contrast, Flt3ITD/ITD-expressing MPPs (expressing high levels of Flt3) were markedly expanded (Fig. 4 G), suggesting that a cell-extrinsic negative impact of Flt3ITD/ITD selectively affects normal HSCs, and that Flt3ITD/ITD cell-intrinsically drives an expansion of LSKCD150−48+ MPPs.
Figure 4.
Flt3-ITDs cause cell-extrinsic suppression of BM HSCs. (A) Relative mRNA gene expression (normalized to Hprt) of Gapdh and Vwf in E15 fetal liver phenotypic HSCs (LSKCD150+CD48−) and MPPs (LSKCD150−CD48+) from Flt3+/+ and Flt3ITD/ITD mice (n = 9 replicates from three mice per genotype). (B) Experimental design for competitive transplantation experiments. (C) Analysis of engraftment 12 wk after transplantation of 5 × 105 CD45.2 E15 FL cells (Flt3+/+ or Flt3ITD/ITD) into CD45.1 recipients with 106 WT CD45.1 BM competitor cells (four donor FL of each genotype transplanted into two to three recipients in two experiments). Results are expressed as percentage of cells expressing CD45.2 of each lineage, myeloid (Mac1+), B cell (B220+CD19+), and T cell (CD4+ and/or CD8+), in the peripheral blood 12 wk after transplantation. (D) Percentage (of total BM cells) of donor (CD45.2) and competitor (CD45.1) HSCs (LSKCD150+CD48−) in BM of recipient mice 12 wk after transplantation (four donor FL of each genotype transplanted into two to three recipients in two experiments). (E) Percentage competitor Vwf-EGFP+ HSCs (LSKCD150+CD48−Vwf-EGFP+CD45.1) in BM of recipient mice 12 wk after transplantation, expressed as percentage of total BM cells. (F and G) Percentage (of total BM cells) of competitor (CD45.1; F) or donor (CD45.2; G) MPPs (LSKCD150−CD48+) in BM of recipient mice 12 wk after transplantation (four donor FL of each genotype each transplanted into two to three recipients in two experiments). Data are shown as mean (SEM) values. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by t test. NS, not significant.
Flt3-ITD–induced myeloproliferation disrupts BM stromal cells
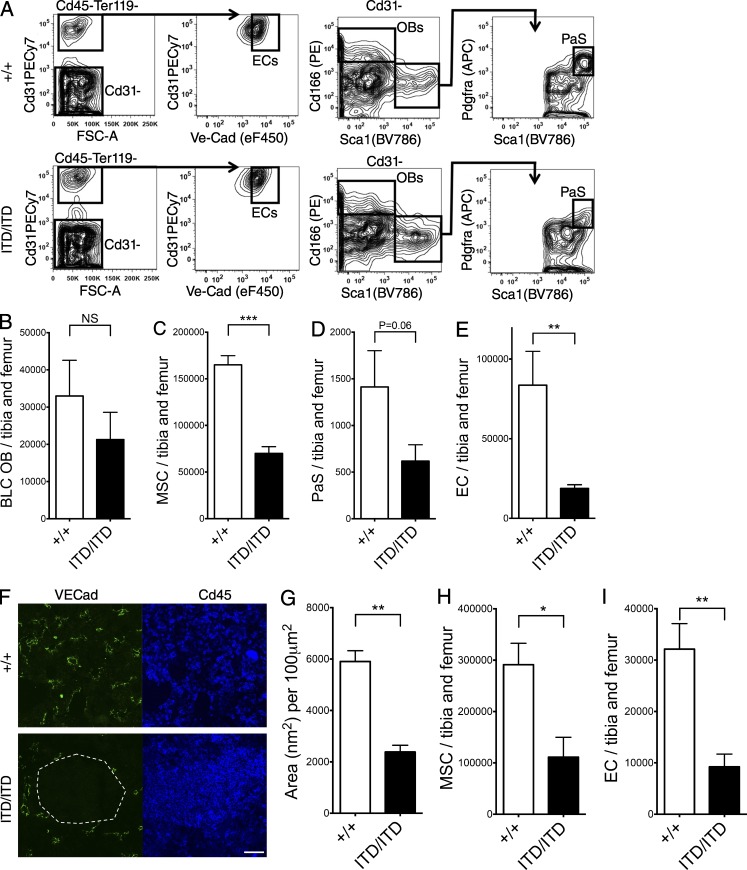
In view of the marked cell-extrinsic suppression of HSCs observed in Flt3ITD/ITD mice, we next analyzed key cellular components of the BM HSC niche to explore whether the nonhematopoietic BM microenvironment might be disrupted in Flt3ITD/ITD mice. FACS analysis of bone lining cells (BLCs; Fig. 5 A; Nakamura et al., 2010) revealed that numbers of BLC osteoblasts (CD45−Ter119−CD31−CD166+Sca1−; Fig. 5 B) were relatively normal. In contrast, total BM mesenchymal stromal cells (MSCs; CD45−Ter119−CD31−Pdgfra+; ×0.4; P < 0.001; Fig. 5 C), BLC Pdgfra+Sca1+ (Houlihan et al., 2012) MSCs (PaS; ×0.4; P = 0.06; Fig. 5 D), and total BM endothelial cells (ECs; CD45−Ter119−CD31+VE-cadherin+; ×0.21; P < 0.01; Fig. 5 E) were all reduced in number in the BM of Flt3ITD/ITD mice. Immunohistochemistry confirmed loss of ECs in the BM of Flt3ITD/ITD mice (P < 0.01; Fig. 5, F and G). To confirm that the observed changes in the niche were also present in transplanted WT recipient mice, CD45.1 mice were analyzed 12 wk after transplantation of 5 × 105 CD45.2 E15 FL cells (Flt3+/+ or Flt3ITD/ITD) with 106 WT CD45.1 BM competitor cells. This analysis confirmed a similar reduction of MSCs (×0.38, P < 0.05; Fig. 5 H) and ECs (×0.29, P < 0.01; Fig. 5 I).
Figure 5.
Flt3-ITD–induced myeloproliferation disrupts the vascular HSC niche. (A) Representative gating strategy to identify osteoblasts (OBs; CD45−Ter119−CD31−CD166+Sca1−), PaS MSCs (CD45−Ter119−CD31−CD166−Sca1+Pdgfra+), and ECs (CD45−Ter119−CD31+VE-Cadherin+) in BLCs from Flt3+/+ and Flt3ITD/ITD mice. (B–E) FACS quantification of OBs in the BLC of 8–10-wk-old Flt3+/+ and Flt3ITD/ITD mice (11 and 13 mice per genotype, respectively; B), MSCs (C) and PaS MSCs (D) in the BLC, and ECs in the BLC and BM (E) of 8–10-wk-old Flt3+/+ and Flt3ITD/ITD mice (six and seven mice per genotype, respectively). (F) Representative images of Flt3+/+ and Flt3ITD/ITD BM in which ECs are identified by VE-cadherin and hematopoietic cells by CD45 staining. An area devoid of vasculature and entirely replaced by CD45+ Flt3ITD/ITD hematopoietic cells is highlighted by the white dashed line. Bar, 50 µm. (G) Sum of blood vessel areas in Flt3+/+ and Flt3ITD/ITD mouse BM (n = 15 areas from three mice of each genotype). (H and I) Numbers of MSCs (H) and ECs (I) in recipient mice 12 wk after transplantation of 5 × 105 CD45.2 E15 FL cells (Flt3+/+ or Flt3ITD/ITD) into CD45.1 WT recipients with 106 WT CD45.1 BM competitor cells (two donor FL of each genotype transplanted into two to three recipients in two experiments). Data are shown as mean (SEM) values. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by t test. NS, not significant.
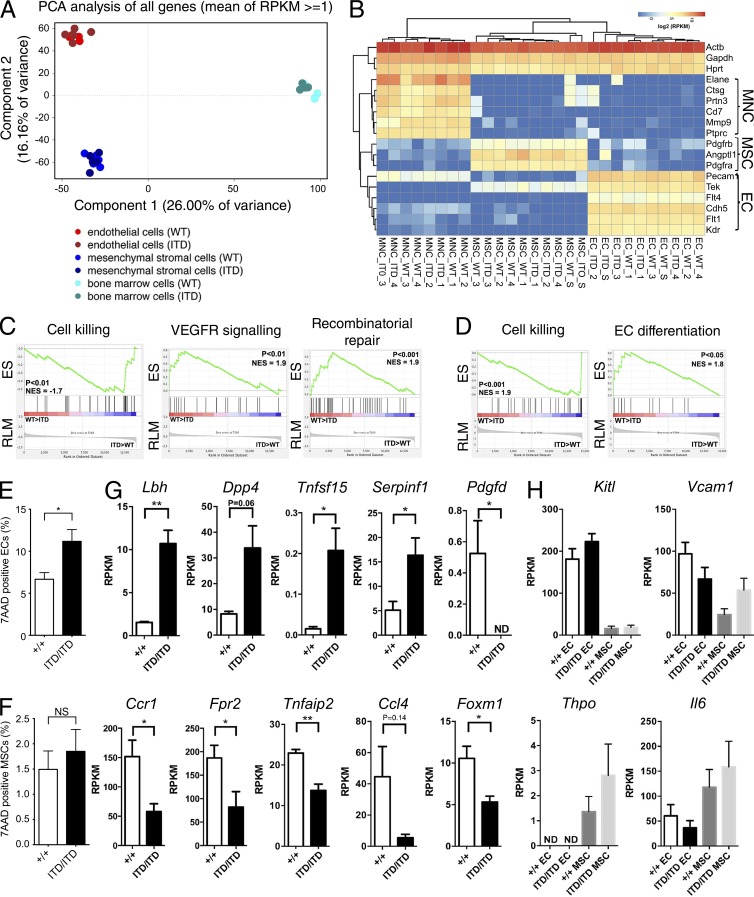
We next performed RNA sequencing of purified ECs, MSCs, and total BM mononuclear cells (MNCs) from BLCs of Flt3+/+ and Flt3ITD/ITD mice (Nakamura et al., 2010). Principle component analysis confirmed that each of the three cell populations tightly clustered in Flt3+/+ and Flt3ITD/ITD mice (Fig. 6 A) and that lineage-specific genes were selectively expressed (Fig. 6 B). However, differential gene expression between Flt3+/+ and Flt3ITD/ITD ECs, MSCs, and MNCs was detected for 392, 308, and 428 genes, respectively. In keeping with the reduced numbers of ECs and MSCs in Flt3ITD/ITD mice, gene set enrichment analysis (GSEA) showed increased expression of genes associated with cell killing in Flt3ITD/ITD ECs; reduced expression of vascular endothelial growth factor receptor signaling pathway genes, a key regulator of angiogenesis (Breier, 2000); and impaired DNA repair (Fig. 6 C). Furthermore, GSEA demonstrated similarly enhanced expression of pathways involved in cell killing in Flt3ITD/ITD MSCs and impaired regulation of EC differentiation (Fig. 6 D). In further support of increased cell death in ECs, frequency of 7AAD-positive cells was increased in ECs and MSCs from Flt3ITD/ITD mice (Fig. 6, E and F), although the increase did not reach statistical significance for MSCs. In keeping with these findings, analysis of specific genes involved in regulation of angiogenesis in MNCs (Fig. 6 G) revealed up-regulation of several angiogenesis-inhibiting genes in Flt3ITD/ITD mice (Lbh, Dpp4, Tnfsf15, and Serpinf1) and down-regulation of angiogenesis-promoting factors (Pdgfd, Ccl4, Ccr1, Fpr2, Tnfaip2, and Foxm1). In contrast, expression of key steady-state extrinsic regulators of HSCs (Kitl, Vcam1, Thpo, and Il6) was not significantly affected in ECs and MSCs (Fig. 6 H).
Figure 6.
Molecular features of niche elements in Flt3-ITD mice. BM MNCs, ECs (CD45−Ter119−CD31+), and MSCs (CD45−Ter119−CD31−CD166−Sca1+) from Flt3+/+ and Flt3ITD/ITD 8–10-wk-old mice (four to five mice per genotype) were subjected to global RNA sequencing. (A) Principal component analysis of MNCs, ECs, and MSCs from Flt3+/+ and Flt3ITD/ITD mice. Each dot represents the indicated cell population from one mouse. (B) Expression of hematopoietic, endothelial, and MSC-associated genes in purified populations of MNCs, ECs, and MSCs from Flt3+/+ and Flt3ITD/ITD 8–10-wk-old mice (four to five mice per genotype). (C) GSEA comparing ECs from Flt3+/+ and Flt3ITD/ITD mice for genes involved in regulation of cell killing and regulation of vascular endothelial growth factor receptor signaling pathway and DNA repair (five mice per genotype). (D) GSEA genes comparing MSCs from Flt3+/+ and Flt3ITD/ITD mice for genes involved in regulation of cell killing and regulation of endothelial cell differentiation (five mice per genotype). (E and F) Frequency of 7AAD-positive ECs (E) and MSCs (F) in the BLC of 8–10-wk-old Flt3+/+ and Flt3ITD/ITD mice (six and seven mice per genotype, respectively). (G) Aberrant expression of angiogenesis-associated genes in MNCs from Flt3ITD/ITD mice (four mice per genotype). (H) Expression of genes implicated in extrinsic regulation of HSCs in EC and MSC from Flt3+/+ and Flt3ITD/ITD mice (five mice per genotype). Data are shown as mean (SEM) values. *, P < 0.05; **, P < 0.01 by t test. ND, not detected; NS, not significant.
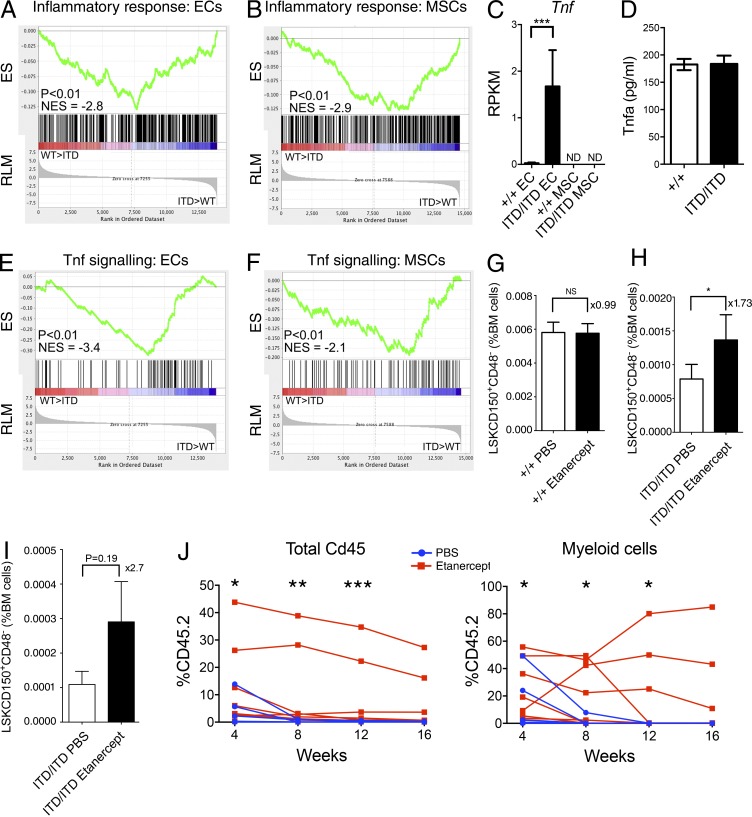
We next performed MetaCore analysis of the differentially expressed genes in MNCs, ECs, and MSCs. Strikingly, inflammation pathways were disrupted in all three cell types (Table S1). Furthermore, GSEA showed up-regulation of gene expression associated with inflammatory response in both ECs (Fig. 7 A) and MSCs (Fig. 7 B). Of particular note, expression of the proinflammatory cytokine Tnf-α (Tnf) was up-regulated in ECs (Fig. 7 C). Notably, serum levels of TNF were not increased in Flt3ITD/ITD mice (Fig. 7 D), suggesting that the up-regulation of Tnf in BM endothelial cells might result in a local effect. In keeping with increased TNF signaling in the BM microenvironment, GSEA showed up-regulation of gene expression associated with TNF signaling in both ECs (Fig. 7 E) and MSCs (Fig. 7 F). Inflammation is known to be an important suppressor of HSC function (King and Goodell, 2011; Schuettpelz and Link, 2013), including TNF, which is notably one of the few known cell-extrinsic suppressors of HSCs (Pronk et al., 2011). We reasoned that the increased TNF expression in the BM of Flt3ITD/ITD mice might account for some of the suppression of HSCs observed. We therefore treated Flt3+/+ and Flt3ITD/ITD mice with the clinically approved TNF inhibitor etanercept for 3 wk. Whereas the numbers of phenotypic HSCs were not affected in Flt3+/+ mice (Fig. 7 G), they were significantly increased in Flt3ITD/ITD mice (Fig. 7 H). CD45.1 competitor HSCs analyzed 12 wk after transplantation of 5 × 105 CD45.2 E15 Flt3ITD/ITD FL cells with 106 WT CD45.1 BM competitor cells showed a similar increase after etanercept treatment, although the difference was not statistically significant (Fig. 7 I). Transplantation of BM cells from PBS or etanercept-treated Flt3ITD/ITD mice showed the expected lack of long-term engraftment in all PBS-treated mice (n = 9; Fig. 7 J). However, three of nine mice treated with etanercept showed sustained engraftment to 16 wk with no evidence of a loss of engraftment that would be anticipated if there was a cell-intrinsic deleterious effect of Flt3-ITD on HSCs (Fig. 7 J). This finding is in marked contrast to the lack of sustained engraftment in 24 recipient mice transplanted with 500,000 BM cells from non–etanercept-treated Flt3ITD/ITD mice (P < 0.01). Collectively, these data demonstrate that Flt3ITD/ITD-driven myeloproliferation creates a proinflammatory BM microenvironment, including overexpression of Tnf in BM niche cells, that causes cell-extrinsic suppression of non–Flt3-expressing HSCs.
Figure 7.
Aberrant inflammation and TNF signaling cause HSC suppression in Flt3-ITD mice. (A and B) GSEA comparing ECs (A) and MSCs (B) in Flt3+/+ and Flt3ITD/ITD mice for inflammatory response–associated gene expression (five mice per genotype in two experiments). (C) Increased expression of Tnf in ECs from Flt3ITD/ITD mice (five mice per genotype). Adjusted p-value from edgeR analysis is shown. (D) Serum TNF-α levels in Flt3+/+ and Flt3ITD/ITD 8–10-wk-old mice (two to three mice per genotype). (E and F) GSEA comparing ECs (E) and MSCs (F) in Flt3+/+ and Flt3ITD/ITD mice for TNF signaling–associated gene expression (five mice per genotype). (G and H) Impact of 3 wk of etanercept treatment on numbers (percentage of total BM cells) of phenotypic (LSKCD150+CD48−) HSCs in Flt3+/+ (G) and Flt3ITD/ITD (H) mice (n = 6–7 mice per group in two independent experiments). (I) Impact of etanercept treatment (compared with PBS treatment) on numbers of phenotypic competitor HSCs (CD45.1+LSKCD150+CD48−) in recipient mice 12 wk after transplantation of 5 × 105 CD45.2 E15 FL cells (Flt3ITD/ITD) into CD45.1 WT recipients with 106 WT CD45.1 BM competitor cells. Data are shown as mean (SEM) values (n = 6 mice per treatment group, two independent experiments). (J) Serial analysis of percentage CD45.2 chimerism in peripheral blood of recipient mice after transplantation of 500,000 unfractionated CD45.2 BM cells from Flt3ITD/ITD mice after 3 wk of treatment with PBS or etanercept (n = 9 mice per treatment group in two experiments). WT CD45.1 competitor cells (n = 200,000) were cotransplanted. Data are shown for total PBMCs (left) and Mac1+Gr1− myeloid cells (right). P-values were generated using Mann–Whitney test to compare percentage of CD45.2 across all replicates for each time point. *, P < 0.05; **, P < 0.01; ***, P < 0.001. ND, not detected; NS, not significant.
Discussion
In the present study, we demonstrated a progressive and gene dosage–dependent severe suppression of phenotypically and functionally defined HSCs in Flt3-ITD knock-in mice, in keeping with previous work (Chu et al., 2012). Several previous studies, including Flt3-Cre fate mapping, concluded that Flt3 protein as well as mRNA expression in normal mouse hematopoiesis initiates in MPPs rather than bona fide HSCs (Adolfsson et al., 2001; Christensen and Weissman, 2001; Buza-Vidas et al., 2009, 2011; Boyer et al., 2011). This would suggest that the mechanism through which Flt3-ITDs affect the HSC reservoir is unlikely to be intrinsic to HSCs. However, a recent study implied a previously unrecognized intrinsic impact of Flt3 in HSC homeostasis by concluding that the FLT3-ITD–induced HSC suppression is not extrinsically, but rather HSC-intrinsically, mediated in Flt3-ITD knock-in mice (Chu et al., 2012). The distinction between a cell-intrinsic or -extrinsic effect of Flt3-ITD on the HSC compartment is of considerable importance for understanding the role of Flt3 in normal hematopoiesis and the impact of Flt3-ITDs on HSCs in hematologic malignancies. We therefore investigated the possibility of HSC-intrinsic and -extrinsic impacts of Flt3-ITD through a combination of single-cell interrogation of Flt3 expression in the phenotypically defined HSC compartment, functional assays, and examination of key components of the HSC niche.
If an HSC-intrinsic impact of Flt3-ITDs on HSCs were to explain the severe reduction in HSC numbers in Flt3-ITD mice, then the expectation would be that the Flt3 receptor is expressed in the large majority of HSCs, because the mutation cannot exert an intrinsic impact on HSCs when it is not expressed. Herein, using a highly sensitive nanofluidic approach to interrogate Flt3 expression at the single-cell level, we found that only a small fraction of LSKCD150+48− cells expressed Flt3 mRNA, and at very low levels. Furthermore, this infrequent Flt3 expression was inversely correlated with expression of several HSC-associated genes, including Vwf, a highly specific marker of platelet-biased HSCs (Sanjuan-Pla et al., 2013). Furthermore, single-cell gene expression analysis of Flt3-ITD mice suggested that the phenotypic HSC compartment is composed primarily of progenitor cells, with a selective depletion of Flt3 mRNA–negative bona fide HSCs, which represent only a small minority of cells within the LSKCD150+48− population in Flt3-ITD mice. Indeed, it has been widely recognized that LSKCD150+48− cells (and any other phenotypically defined HSC population) also contain a substantial fraction of non-HSCs, and that the proportion of such contaminating non-HSCs within the phenotypically defined HSC compartment might be increased in genetically modified mice (Purton and Scadden, 2007), in particular if the fraction of bona fide HSCs is selectively depleted, such as described here in Flt3-ITD mice. This selective loss of Flt3 mRNA–negative and Vwf-positive LSKCD150+48− cells in Flt3-ITD mice suggests that the LSKCD150+48− compartment in Flt3-ITD mice contains a much lower proportion of bona fide HSCs than in WT mice. This was further supported by the dramatic loss of long-term reconstituting activity of BM cells from Flt3-ITD mice as established through competitive transplantation experiments. These findings highlight the clear advantage of single-cell analysis to reveal cellular heterogeneity in phenotypically defined cell types that is not apparent at the cell population level (Wills and Mead, 2015), a finding that has potentially important implications for the analysis of other disease models.
It is not possible to exclude the possibility that some Flt3 mRNA might be expressed below the limit of detection of the assays; however, our single-cell gene expression analysis did not provide any support for a HSC-intrinsic suppression of bona fide HSCs in Flt3-ITD mice, and we therefore explored the possibility of a cell-extrinsic mechanism. Although a competitive reconstitution assay (Purton and Scadden, 2007) is the only manner in which one can conclusively establish whether an observed reduction in HSC numbers is intrinsically or extrinsically mediated, reliable interpretation of the results depends entirely on a comparable number of genuine HSCs being transplanted from the genetically modified and control WT mice. The extent of contaminating non-HSCs might be altered extensively in genetically modified mice, in particular if such non-HSCs are expanded compared with the WT setting or if the true HSCs are selectively depleted, as specifically demonstrated to be the case in Flt3-ITD mice through single-cell gene expression analysis. Thus, when HSC numbers as well as the HSC functional readout are already severely affected by a mutation such as Flt3-ITD, transplantation of equal numbers of functional HSCs is difficult if not impossible to achieve. Failure to take this heterogeneity into account can lead to false assumptions in the experimental design and incorrect interpretation of data. Consequently, transplantation of equal numbers of phenotypic HSCs will in reality result in transplantation of markedly lower numbers of functional HSCs from Flt3-ITD versus WT mice (Chu et al., 2012). In light of this, such a competitive assay must therefore be performed before a significant HSC phenotype has been acquired, through establishing BM chimeric mice either before the mutation is induced (requiring, unlike here and in the studies of Chu et al. [2012], a mouse model with an inducible mutation) or before the HSC phenotype has been acquired. In our case, this was possible by establishing BM chimeras with E15 FL cells, at which time the number of LSKCD150+48− cells was unperturbed, likely because this is before the development of overt myeloproliferative disease in Flt3-ITD mice (Mead et al., 2013). Furthermore, FL HSCs are extremely robust at engraftment (Bowie et al., 2007), and it is a frequently observed phenomenon in the literature that FL HSCs can sustain high-level engraftment in mouse models associated with a postnatal HSC defect (Jones et al., 2015). Through this approach, we were able to provide definitive evidence of a marked cell-extrinsic effect of Flt3-ITDs on the HSC compartment, as WT competitor LSKCD150+48− cells were dramatically reduced in the presence of competing Flt3-ITD–expressing cells, in fact more extensively than LSKCD150+48− cells in the Flt3-ITD donor cells in the same mice, a finding in further support of LSKCD150+48− cells in Flt3-ITD mice being relatively depleted of genuine HSCs and most compatible with the observed HSC suppression in Flt3-ITD mice being mediated fully cell-extrinsically. Importantly, if in fact HSCs were already somewhat reduced in the FL of Flt3-ITD mice, we would if anything have underestimated the level of cell-extrinsic suppression of HSCs in the competitive transplantation experiments performed. Distinguishing between a cell-extrinsic and -intrinsic impact of Flt3-ITD on HSCs is crucial, as it has extensive implications for the understanding of Flt3 as a key regulator of normal hematopoiesis and the impact and therapeutic targeting of FLT3-ITD mutations in hematologic malignancies. Our findings are in line with results from other models of hematologic malignancies (Schepers et al., 2013) and human disease (Colmone et al., 2008), supporting an extrinsic impact of some hematopoietic tumors on HSCs.
We also explored the possible mechanistic basis of the HSC-extrinsic suppression of HSCs in Flt3-ITD mice through analysis of key cellular components and molecular determinants of the HSC niche. We found a two- to fivefold reduction in the numbers of MSCs and ECs in the BM of Flt3-ITD mice, both niche cell populations suggested to be critical for the regulation of HSCs (Morrison and Scadden, 2014). Moreover, ECs and MSCs in Flt3-ITD mice demonstrated aberrant gene expression, consistent with increased apoptosis and impaired EC homeostasis. Analysis of total BM MNCs also revealed dysregulation of genes implicated in angiogenesis. In addition, mediators of inflammation known to be associated with suppression of HSCs, such as TNF-α (King and Goodell, 2011; Pronk et al., 2011), were overexpressed by ECs in Flt3-ITD mice. Furthermore, several inflammatory mediators are known to increase TNF expression in endothelial cells (Ranta et al., 1999; Imaizumi et al., 2000). Inflammation and TNF signaling have also been directly implicated in the disruption of BM microenvironment and hematopoiesis in patients with a range of myeloid malignancies (Chen et al., 2016; Koschmieder et al., 2016), including elevated TNF levels in patients with AML (Sanchez-Correa et al., 2013), correlating with high leukocyte count and resistant disease (Tsimberidou et al., 2008). We therefore treated Flt3-ITD mice with a clinically approved anti-TNF therapy (etanercept), which resulted in a partial rescue of the HSC phenotype in Flt3-ITD mice, as confirmed in functional, competitive HSC repopulation assays. Because etanercept treatment only partially rescued the HSC defect in Flt3-ITD mice, it is likely that other mechanisms of HSC repression, including other inflammatory mediators, might also play a role. Collectively, we observed both quantitative (reduction in numbers of ECs and MSCs) and qualitative (inflammation and TNF signaling) disruption of the BM microenvironment in Flt3-ITD mice, which likely underlie the observed extrinsic suppression of HSCs, in agreement with other studies implying that hematologic malignancies dysregulate HSC niches (Schepers et al., 2015).
Although genetically engineered mouse lines are imperfect model systems for human malignancies, our findings do raise several potentially highly relevant issues for the understanding of human AML biology. Because only HSCs are capable of long-term propagation of the Flt3-ITD clone (Chu et al., 2012), this is to our knowledge the first demonstration of a tumor model that is dependent on propagation by a stem cell compartment which carries the relevant DNA mutation but nevertheless does not express the mutant protein. Consequently, acquisition of the mutation by a HSC will have no intrinsic impact on the cell, exerting neither positive nor negative selection pressure. Although at a cell population level FLT3-ITD mutations are not easily detectable in preleukemic HSCs (Jan et al., 2012), it remains fully possible that rare HSCs might still carry the mutation, which upon subsequent differentiation and FLT3-ITD protein expression would confer a clonal advantage in a progenitor population, as here demonstrated for Flt3-expressing MPPs. Indeed, there is ample support for such FLT3-expressing progenitor populations being transformed to become leukemic stem cell populations in patients with AML (Goardon et al., 2011). The clinical use of small-molecule inhibitors of FLT3 signaling has in general been disappointing in AML (Kayser and Levis, 2014), with frequent acquisition of resistance causing mutations in patients demonstrating an initial response (Smith et al., 2012). This suggests that inhibitor-insensitive FLT3-ITD mutated cells, potentially because they do not express the mutant protein, remain in responding patients, acting as a reservoir for the acquisition of additional mutations (Smith et al., 2012). Given the lack of expression of the mutant protein, such mutant HSCs would not have a competitive advantage at the HSC level, but would nevertheless be very relevant for the initiation of AML and propagation of relapse, because they would not be targeted by FLT3 inhibitors. Studies of leukemic stem cell populations would be insufficiently sensitive to detect such extremely rare cells, and further studies on larger patient cohorts to explore this possibility with single-cell resolution are therefore warranted.
Materials and methods
Animals
All mice were bred and maintained in accordance with UK Home Office regulations, and experiments were conducted after approval by the University of Oxford Animal Welfare and Ethical Review Body (project license 30/3103). Flt3-ITD knock-in mice on C57BL/6 background have been previously described (Lee et al., 2007; Kharazi et al., 2011). Homozygous (Flt3ITD/ITD) and heterozygous (Flt3ITD/+) Flt3-ITD mice were studied as specified. Vwf-EGFP mice have been previously described (Sanjuan-Pla et al., 2013) and were on a C57BL/6 background. Mice were analyzed with littermate controls of the appropriate genotype when available and as specified.
FACS
Specific details of mouse antibodies and viability dyes used for flow cytometry analysis are shown in Table S2. All antibodies were used at predetermined (titrated) optimized concentrations. Cell acquisition and analysis were performed on a four-laser LSRII (BD) using FlowJo software (Tree Star). Myeloid progenitor populations were identified as previously described (Kharazi et al., 2011). Cell sorting was done on a BD FACSAria II cell sorter. Cells used in cell sorting experiments were not enriched and were stained after initial Fc-block incubation. Gates were set using a combination of fluorescence-minus-one controls and also populations that are known to be negative for the antigen.
Competitive transplantation assay
Congenic CD45.1 and CD45.2 WT C57BL/6 mice were used as controls and recipients in transplantation experiments. Adult (8–10-wk-old mice) BM transplantation was performed using 500,000 donor CD45.2 BM cells, or purified cell populations as indicated, from Flt3+/+ or Flt3ITD/ITD mice along with 200,000 CD45.1 WT competitor cells. FL transplantations used 500,000 donor Flt3+/+ or Flt3ITD/ITD CD45.2 FL cells with 1,000,000 CD45.1 WT BM competitor cells. Cells were injected into tail veins of lethally irradiated (900 cGy) recipient CD45.1 mice. Flow cytometric analysis of CD45.1 and CD45.2 reconstitution and donor-derived lineage and progenitor reconstitution were assessed 12 wk after transplantation as indicated and previously reported (Kharazi et al., 2011).
For etanercept treatment, 8-wk-old WT C57BL/6J and Flt3ITD/ITD mice were injected intraperitoneally with PBS or etanercept (Pfizer) at a dose of 10 mg/kg body weight three times a week for 3 wk before BM cells were collected for transplantation. For etanercept treatment of transplanted mice, 500,000 unfractionated WT or Flt3-ITD E15 FL cells (CD45.2 allotype) were intravenously injected along with 1,000,000 WT unfractionated CD45.1 BM cells into lethally irradiated CD45.1 recipients (900 cGy, split dose). Transplanted mice were injected intraperitoneally with PBS or etanercept (Pfizer) at a dose of 10 mg/kg body weight three times a week from 6 wk posttransplantation until the final analysis. Peripheral blood reconstitution was monitored at 4, 8, and 12 wk after transplantation. 12 wk after transplantation, phenotypic analysis of BM HSCs was performed.
In vitro HSC survival assay
Single LSKCD150+48− HSC-enriched cells or LSKFlt3high LMPPs were preincubated in 10 µl Stemspan SFEM (STEMCELL Technologies) supplemented with 100 ng/ml mouse SCF, 100 ng/ml human FLT3L, or no cytokines as indicated for 5 d. Next, an additional 10 µl medium containing a highly proliferative cytokine cocktail was added into each well. Final concentrations of cytokines for all cells were 50 ng/ml mSCF, 50 ng/ml FLT3L, 5 ng/ml human thrombopoietin, 5 ng/ml murine IL-3, 10 ng/ml murine GM-CSF, and 10 ng/ml human G-CSF. After an additional 10 d of incubation at 37°C, 98% humidity, and 5% CO2, wells were analyzed under an inverted light microscope for cells that had undergone at least one cell division.
Preparation of single-cell suspension of stromal cells
For preparation of BLCs, femurs and tibias were harvested, cleaned of excess muscle tissue, and placed into PBS/5% FCS. Bones were crushed in a mortar, and BM was removed for separate processing of central BM. The bones were fragmented with scissors and transferred to a 15-ml tube (Falcon). Bones were spun down, and excess PBS/FCS was removed. Cells were isolated by incubation at 37°C with type I collagenase (3 mg/ml; Worthington Biochemical Corporation) for 45 min with rotation in DMEM with 10% FCS. The cell suspension was collected by passing through a 70-µm cell strainer. Collagenase was then added for a further 45 min. Cells were collected and washed in PBS/5% FCS/2 mM EDTA to reduce clumping.
For analysis of central BM stromal cells, BM cells were incubated at 37°C with type IV collagenase (2 mg/ml; Worthington Biochemical Corporation) for 20 min with rotation in DMEM with 10% FCS, and RBCs were lysed with ammonium chloride solution (STEMCELL Technologies) at room temperature for 10 min. Subsequently, CD45+ cells were depleted with anti-CD45 MicroBeads (Miltenyi Biotec). Cells were collected and resuspended in PBS/5% FCS/2 mM EDTA for FACS analysis.
Multiplex quantitative real-time PCR analysis of single cells and cell populations
For cDNA synthesis and preamplification of target genes, CellsDirect One-Step qRT-PCR kit (Invitrogen) was used. Cells were sorted directly into PCR plates or 0.2-ml PCR tubes containing 2.5 µl gene-specific 0.2× TaqMan gene expression assays (Applied Biosystems), 5 µl CellsDirect 2× Reaction mix (Invitrogen), 1.2 µl CellsDirect RT/Taq mix, 1.2 µl TE buffer, and 0.1 µl SUPERase•In RNase Inhibitor (Ambion) to a total volume of 10 µl. For single cells, the reaction volume was reduced to 5 µl. Conditions for reverse transcription and target gene amplification were 15 min at 50°C; 2 min at 95°C; and 22 cycles of 95°C for 15 s and 60°C for 4 min. Preamplified products were diluted 1:5 in TE buffer and analyzed on Dynamic Array (Fluidigm) using the following PCR cycling conditions: 95°C for 10 min and 40 cycles of 95°C for 15 s and 60°C for 60 s. Data were analyzed using the ΔCt method; results were normalized to Hprt expression for cell populations and Gapdh expression for single-cell analysis and expressed as relative expression level. Single cells not expressing B2m, Hprt, or Gapdh were excluded from the analysis. For t-SNE analysis, single-cell expression data were aggregated, and genes with zero variance were excluded from the analysis. The Ct value range was truncated to a maximum value of 40, in excess of the maximum recorded Ct. The t-SNE (van der Maaten and Hinton, 2008; van der Maaten, 2014) transformation was performed in Matlab (v. R2015a, 8.5.0.297613) using all 96 murine genes included in the gene expression analysis, and transformed data were plotted in R. Cells were hierarchically clustered on the basis of their expression profiles. The resulting dendrogram was used to identify two major clusters of cells. The deviation of the frequency of each population from a uniform partitioning between the two clusters was assessed by means of binomial tests. Details of TaqMan assays used are shown in Table S3.
Nanofluidic cell capture and single-cell gene expression analysis
Cell capture and target preamplification were performed using the C1 system (Fluidigm) according to the manufacturer’s instructions, using forward, 5′-GTGGCCAAAGGCATGGAATT-3′, and reverse, 5′-TGGGTGACCAACACATTCCT-3′ primers (Fluidigm DELTAgene assays). Real-time PCR was performed on preamplified material from single cells using the BioMark 96.96 Dynamic Array platform (Fluidigm).
RNA sequencing
Samples for RNA sequencing were prepared using the SMARTer Ultra Low RNA kit for Illumina Sequencing (Takara Bio Inc.) according to the manufacturer’s instructions as previously described (Böiers et al., 2013; Woll et al., 2014). In brief, cDNA libraries were prepared from 100 (EC and MSC) or 200 (MNC) cells, with four to five biological replicates from each genotype. Cells were sorted directly into lysis buffer supplemented with RNase Inhibitor (Takara Bio Inc.). cDNA libraries were prepared according to manufacturer instructions with 15 cycles of amplification. Amplified cDNA libraries validated with a distinct peak spanning 400–9,000 bp in size as measured by High Sensitivity DNA kit (Agilent Technologies) on Agilent 2100 Bioanalyzer were further processed for RNA sequencing. Libraries were prepared for Illumina sequencing using the Nextera XT DNA Sample Preparation kit (Illumina) using the manufacturer’s recommended protocol. The size of the amplified fragments was confirmed by Agilent DNA1000 kit (Agilent Technologies). Four to five samples with different indexes were pooled per lane and sequenced on a HiSeq2000 (Illumina) generating single-end, 51-bp reads. After quality control analysis, reads were aligned using Bowtie (Langmead et al., 2009) against the murine transcriptome (mouse NCBI build38 [mm10] UCSC transcripts). Non–uniquely mapped reads were discarded. Expression levels of all genes were quantified using RSEM with default parameters (Li and Dewey, 2011). The estimated read count for each gene generated by RSEM was used for statistical calculation of global differential gene expression between specified populations using DESeq2 (Anders and Huber, 2010) and edgeR (Robinson et al., 2010) packages. Genes were considered differentially expressed between populations at an adjusted p-value <0.1 from either DESeq2 or edgeR and log2 fold change of reads per kilobase of transcript per million mapped reads (RPKM) values ≥1. The RPKM values estimated by RSEM were used when investigating the expression of specific genes. Hierarchical clustering and principal components analysis were performed in R. The pheatmap function was used to generate the heatmap and the prcomp function was used for PCA analysis on the log-transformed RPKM values. GSEA analysis (Subramanian et al., 2005) was performed using GSEA software (http://www.broadinstitute.org/gsea). Pathways enrichment analysis was performed using MetaCore software (Thomson Reuters). Data files have been uploaded to GEO database (accession no. GSE63206).
Immunohistochemistry
Femoral bones were cryoembedded in OCT compound and sectioned at 8-µm thickness. Sections were fixed with methanol for 15 min and blocked with a protein blocker (Dako). Specimens were then incubated with goat anti–VE-cadherin antibody (R&D Systems) followed by donkey anti–goat IgG antibody conjugated to Alexa Fluor 488 (Molecular Probes) and nuclear staining. Images were acquired with a confocal laser-scanning microscope (FV1000; Olympus). Blood vessel perimeters were measured using ImageJ (NIH).
ELISA
Mouse serum samples were collected from peripheral blood clotted for 2 h at room temperature by centrifuging for 20 min at 2,000 g. Samples were assessed by murine TNF ELISA kits (Abcam) according to the manufacturer’s instructions. Optical density measurements were determined using a microplate reader (SpectraMax M2e; Molecular Devices) set to 450 nm with wavelength correction set to 570 nm.
Statistical analysis
Unless otherwise indicated, the statistical significance of differences between samples was determined using a Student’s t test for normally distributed data and Mann–Whitney test for non–normally distributed data.
Online supplemental material
Table S1 shows metacore analysis of ECs and MSCs. Table S2 lists the antibodies used. Table S3 lists the TaqMan assays used.
Supplementary Material
Acknowledgments
A.J. Mead received funding from a Bloodwise Senior Bennett Fellowship and Medical Research Council (MRC) Senior Clinical Fellowship (MR/L006340/1). These studies were supported by grants to S.E.W. Jacobsen from the UK MRC (G0801073 and MC_UU_12009/5) and the Swedish Research Council. R. Facchini was a recipient of a Bloodwise PhD fellowship, and O. Chowdhury received a Wellcome Trust Clinical fellowship. This work was also supported by the MRC-funded Oxford Consortium for Single-Cell Biology (MR/M00919X/1). The authors acknowledge the contributions of the WIMM Flow Cytometry Facility, supported by the MRC Human Immunology Unit; MRC Molecular Haematology Unit (MC_UU_12009); National Institute for Health Research Oxford Biomedical Research Centre and John Fell Fund (131/030 and 101/517); the E.P. Abraham Research Fund (CF182 and CF170); and the WIMM Strategic Alliance awards G0902418 and MC_UU_12025.
The authors declare no competing financial interests.
Author contributions: A.J. Mead designed, performed, and analyzed experiments and wrote the manuscript. W.H. Neo, R. Facchini, C.A.G. Booth, N. Fordham, D. Atkinson, O. Chowdhury, S. Kharazi, S.-A. Clark, L. Jamieson, C. Di Genua, T. Bouriez, and P. Woll were involved in FACS analysis/sorting and provided other technical assistance. S. Matsuoka carried out immunohistochemistry analyses. N. Barkas, E. Repapi, N. Gray, and S. Thongjuea carried out bioinformatics analysis. A. Giustacchini and S. Thongjuea analyzed RNA-sequencing and single-cell gene expression data. T. Suda and C. Nerlov provided input on experimental design and analysis. S.E.W. Jacobsen conceived and supervised the project, designed and analyzed experiments, and wrote the manuscript. All authors read and approved the final manuscript.
Footnotes
Abbreviations used:
- AML
- acute myeloid leukemia
- BLC
- bone lining cell
- EC
- endothelial cell
- FL
- fetal liver
- FLT3L
- FLT3 ligand
- HSC
- hematopoietic stem cell
- ITD
- internal tandem duplication
- LMPP
- lymphoid-primed multipotent progenitor
- MNC
- mononuclear cell
- MPP
- multipotent progenitor
- MSC
- mesenchymal stromal cell
- RPKM
- reads per kilobase of transcript per million mapped reads
- SCF
- stem cell factor
- t-SNE
- t-distributed stochastic neighbor embedding
References
- Adolfsson J., Borge O.J., Bryder D., Theilgaard-Mönch K., Astrand-Grundström I., Sitnicka E., Sasaki Y., and Jacobsen S.E.. 2001. Upregulation of Flt3 expression within the bone marrow Lin(-)Sca1(+)c-kit(+) stem cell compartment is accompanied by loss of self-renewal capacity. Immunity. 15:659–669. 10.1016/S1074-7613(01)00220-5 [DOI] [PubMed] [Google Scholar]
- Adolfsson J., Månsson R., Buza-Vidas N., Hultquist A., Liuba K., Jensen C.T., Bryder D., Yang L., Borge O.J., Thoren L.A., et al. . 2005. Identification of Flt3+ lympho-myeloid stem cells lacking erythro-megakaryocytic potential a revised road map for adult blood lineage commitment. Cell. 121:295–306. 10.1016/j.cell.2005.02.013 [DOI] [PubMed] [Google Scholar]
- Anders S., and Huber W.. 2010. Differential expression analysis for sequence count data. Genome Biol. 11:R106 10.1186/gb-2010-11-10-r106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böiers C., Buza-Vidas N., Jensen C.T., Pronk C.J., Kharazi S., Wittmann L., Sitnicka E., Hultquist A., and Jacobsen S.E.. 2010. Expression and role of FLT3 in regulation of the earliest stage of normal granulocyte-monocyte progenitor development. Blood. 115:5061–5068. 10.1182/blood-2009-12-258756 [DOI] [PubMed] [Google Scholar]
- Böiers C., Carrelha J., Lutteropp M., Luc S., Green J.C., Azzoni E., Woll P.S., Mead A.J., Hultquist A., Swiers G., et al. . 2013. Lymphomyeloid contribution of an immune-restricted progenitor emerging prior to definitive hematopoietic stem cells. Cell Stem Cell. 13:535–548. 10.1016/j.stem.2013.08.012 [DOI] [PubMed] [Google Scholar]
- Bowie M.B., Kent D.G., Dykstra B., McKnight K.D., McCaffrey L., Hoodless P.A., and Eaves C.J.. 2007. Identification of a new intrinsically timed developmental checkpoint that reprograms key hematopoietic stem cell properties. Proc. Natl. Acad. Sci. USA. 104:5878–5882. 10.1073/pnas.0700460104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyer S.W., Schroeder A.V., Smith-Berdan S., and Forsberg E.C.. 2011. All hematopoietic cells develop from hematopoietic stem cells through Flk2/Flt3-positive progenitor cells. Cell Stem Cell. 9:64–73. 10.1016/j.stem.2011.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyer S.W., Beaudin A.E., and Forsberg E.C.. 2012. Mapping differentiation pathways from hematopoietic stem cells using Flk2/Flt3 lineage tracing. Cell Cycle. 11:3180–3188. 10.4161/cc.21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breier G. 2000. Functions of the VEGF/VEGF receptor system in the vascular system. Semin. Thromb. Hemost. 26:553–560. 10.1055/s-2000-13212 [DOI] [PubMed] [Google Scholar]
- Buza-Vidas N., Cheng M., Duarte S., Charoudeh H.N., Jacobsen S.E., and Sitnicka E.. 2009. FLT3 receptor and ligand are dispensable for maintenance and posttransplantation expansion of mouse hematopoietic stem cells. Blood. 113:3453–3460. 10.1182/blood-2008-08-174060 [DOI] [PubMed] [Google Scholar]
- Buza-Vidas N., Woll P., Hultquist A., Duarte S., Lutteropp M., Bouriez-Jones T., Ferry H., Luc S., and Jacobsen S.E.. 2011. FLT3 expression initiates in fully multipotent mouse hematopoietic progenitor cells. Blood. 118:1544–1548. 10.1182/blood-2010-10-316232 [DOI] [PubMed] [Google Scholar]
- Chen S., Zambetti N.A., Bindels E.M., Kenswill K., Mylona A.M., Adisty N.M., Hoogenboezem R.M., Sanders M.A., Cremers E.M., Westers T.M., et al. . 2016. Massive parallel RNA sequencing of highly purified mesenchymal elements in low-risk MDS reveals tissue-context-dependent activation of inflammatory programs. Leukemia. 30:1938–1942. 10.1038/leu.2016.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen J.L., and Weissman I.L.. 2001. Flk-2 is a marker in hematopoietic stem cell differentiation: A simple method to isolate long-term stem cells. Proc. Natl. Acad. Sci. USA. 98:14541–14546. 10.1073/pnas.261562798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu S.H., Heiser D., Li L., Kaplan I., Collector M., Huso D., Sharkis S.J., Civin C., and Small D.. 2012. FLT3-ITD knockin impairs hematopoietic stem cell quiescence/homeostasis, leading to myeloproliferative neoplasm. Cell Stem Cell. 11:346–358. 10.1016/j.stem.2012.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colmone A., Amorim M., Pontier A.L., Wang S., Jablonski E., and Sipkins D.A.. 2008. Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science. 322:1861–1865. 10.1126/science.1164390 [DOI] [PubMed] [Google Scholar]
- Ding L., Ley T.J., Larson D.E., Miller C.A., Koboldt D.C., Welch J.S., Ritchey J.K., Young M.A., Lamprecht T., McLellan M.D., et al. . 2012. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature. 481:506–510. 10.1038/nature10738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale R.E., Green C., Allen C., Mead A.J., Burnett A.K., Hills R.K., and Linch D.C.. Medical Research Council Adult Leukaemia Working Party . 2008. The impact of FLT3 internal tandem duplication mutant level, number, size, and interaction with NPM1 mutations in a large cohort of young adult patients with acute myeloid leukemia. Blood. 111:2776–2784. 10.1182/blood-2007-08-109090 [DOI] [PubMed] [Google Scholar]
- Goardon N., Marchi E., Atzberger A., Quek L., Schuh A., Soneji S., Woll P., Mead A., Alford K.A., Rout R., et al. . 2011. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell. 19:138–152. 10.1016/j.ccr.2010.12.012 [DOI] [PubMed] [Google Scholar]
- Houlihan D.D., Mabuchi Y., Morikawa S., Niibe K., Araki D., Suzuki S., Okano H., and Matsuzaki Y.. 2012. Isolation of mouse mesenchymal stem cells on the basis of expression of Sca-1 and PDGFR-α. Nat. Protoc. 7:2103–2111. 10.1038/nprot.2012.125 [DOI] [PubMed] [Google Scholar]
- Ikuta K., and Weissman I.L.. 1992. Evidence that hematopoietic stem cells express mouse c-kit but do not depend on steel factor for their generation. Proc. Natl. Acad. Sci. USA. 89:1502–1506. 10.1073/pnas.89.4.1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imaizumi T., Itaya H., Fujita K., Kudoh D., Kudoh S., Mori K., Fujimoto K., Matsumiya T., Yoshida H., and Satoh K.. 2000. Expression of tumor necrosis factor-α in cultured human endothelial cells stimulated with lipopolysaccharide or interleukin-1α. Arterioscler. Thromb. Vasc. Biol. 20:410–415. 10.1161/01.ATV.20.2.410 [DOI] [PubMed] [Google Scholar]
- Jan M., Snyder T.M., Corces-Zimmerman M.R., Vyas P., Weissman I.L., Quake S.R., and Majeti R.. 2012. Clonal evolution of preleukemic hematopoietic stem cells precedes human acute myeloid leukemia. Sci. Transl. Med. 4:149ra118 10.1126/scitranslmed.3004315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M., Chase J., Brinkmeier M., Xu J., Weinberg D.N., Schira J., Friedman A., Malek S., Grembecka J., Cierpicki T., et al. . 2015. Ash1l controls quiescence and self-renewal potential in hematopoietic stem cells. J. Clin. Invest. 125:2007–2020. 10.1172/JCI78124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser S., and Levis M.J.. 2014. FLT3 tyrosine kinase inhibitors in acute myeloid leukemia: Clinical implications and limitations. Leuk. Lymphoma. 55:243–255. 10.3109/10428194.2013.800198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharazi S., Mead A.J., Mansour A., Hultquist A., Böiers C., Luc S., Buza-Vidas N., Ma Z., Ferry H., Atkinson D., et al. . 2011. Impact of gene dosage, loss of wild-type allele, and FLT3 ligand on Flt3-ITD-induced myeloproliferation. Blood. 118:3613–3621. 10.1182/blood-2010-06-289207 [DOI] [PubMed] [Google Scholar]
- King K.Y., and Goodell M.A.. 2011. Inflammatory modulation of HSCs: Viewing the HSC as a foundation for the immune response. Nat. Rev. Immunol. 11:685–692. 10.1038/nri3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koschmieder S., Mughal T.I., Hasselbalch H.C., Barosi G., Valent P., Kiladjian J.J., Jeryczynski G., Gisslinger H., Jutzi J.S., Pahl H.L., et al. . 2016. Myeloproliferative neoplasms and inflammation: Whether to target the malignant clone or the inflammatory process or both. Leukemia. 30:1018–1024. 10.1038/leu.2016.12 [DOI] [PubMed] [Google Scholar]
- Langmead B., Trapnell C., Pop M., and Salzberg S.L.. 2009. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 10:R25 10.1186/gb-2009-10-3-r25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B.H., Tothova Z., Levine R.L., Anderson K., Buza-Vidas N., Cullen D.E., McDowell E.P., Adelsperger J., Fröhling S., Huntly B.J., et al. . 2007. FLT3 mutations confer enhanced proliferation and survival properties to multipotent progenitors in a murine model of chronic myelomonocytic leukemia. Cancer Cell. 12:367–380. 10.1016/j.ccr.2007.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levis M., Murphy K.M., Pham R., Kim K.T., Stine A., Li L., McNiece I., Smith B.D., and Small D.. 2005. Internal tandem duplications of the FLT3 gene are present in leukemia stem cells. Blood. 106:673–680. 10.1182/blood-2004-05-1902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., and Dewey C.N.. 2011. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinformatics. 12:323 10.1186/1471-2105-12-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwenberg B., Downing J.R., and Burnett A.. 1999. Acute myeloid leukemia. N. Engl. J. Med. 341:1051–1062. 10.1056/NEJM199909303411407 [DOI] [PubMed] [Google Scholar]
- Luc S., Buza-Vidas N., and Jacobsen S.E.. 2007. Biological and molecular evidence for existence of lymphoid-primed multipotent progenitors. Ann. N. Y. Acad. Sci. 1106:89–94. 10.1196/annals.1392.023 [DOI] [PubMed] [Google Scholar]
- Luc S., Luis T.C., Boukarabila H., Macaulay I.C., Buza-Vidas N., Bouriez-Jones T., Lutteropp M., Woll P.S., Loughran S.J., Mead A.J., et al. . 2012. The earliest thymic T cell progenitors sustain B cell and myeloid lineage potential. Nat. Immunol. 13:412–419. 10.1038/ni.2255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead A.J., Kharazi S., Atkinson D., Macaulay I., Pecquet C., Loughran S., Lutteropp M., Woll P., Chowdhury O., Luc S., et al. . 2013. FLT3-ITDs instruct a myeloid differentiation and transformation bias in lymphomyeloid multipotent progenitors. Cell Reports. 3:1766–1776. 10.1016/j.celrep.2013.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meshinchi S., and Appelbaum F.R.. 2009. Structural and functional alterations of FLT3 in acute myeloid leukemia. Clin. Cancer Res. 15:4263–4269. 10.1158/1078-0432.CCR-08-1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison S.J., and Scadden D.T.. 2014. The bone marrow niche for haematopoietic stem cells. Nature. 505:327–334. 10.1038/nature12984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura Y., Arai F., Iwasaki H., Hosokawa K., Kobayashi I., Gomei Y., Matsumoto Y., Yoshihara H., and Suda T.. 2010. Isolation and characterization of endosteal niche cell populations that regulate hematopoietic stem cells. Blood. 116:1422–1432. 10.1182/blood-2009-08-239194 [DOI] [PubMed] [Google Scholar]
- Osawa M., Hanada K., Hamada H., and Nakauchi H.. 1996. Long-term lymphohematopoietic reconstitution by a single CD34-low/negative hematopoietic stem cell. Science. 273:242–245. 10.1126/science.273.5272.242 [DOI] [PubMed] [Google Scholar]
- Pronk C.J., Veiby O.P., Bryder D., and Jacobsen S.E.. 2011. Tumor necrosis factor restricts hematopoietic stem cell activity in mice: Involvement of two distinct receptors. J. Exp. Med. 208:1563–1570. 10.1084/jem.20110752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purton L.E., and Scadden D.T.. 2007. Limiting factors in murine hematopoietic stem cell assays. Cell Stem Cell. 1:263–270. 10.1016/j.stem.2007.08.016 [DOI] [PubMed] [Google Scholar]
- Ranta V., Orpana A., Carpén O., Turpeinen U., Ylikorkala O., and Viinikka L.. 1999. Human vascular endothelial cells produce tumor necrosis factor-α in response to proinflammatory cytokine stimulation. Crit. Care Med. 27:2184–2187. 10.1097/00003246-199910000-00019 [DOI] [PubMed] [Google Scholar]
- Robinson M.D., McCarthy D.J., and Smyth G.K.. 2010. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 26:139–140. 10.1093/bioinformatics/btp616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Correa B., Bergua J.M., Campos C., Gayoso I., Arcos M.J., Bañas H., Morgado S., Casado J.G., Solana R., and Tarazona R.. 2013. Cytokine profiles in acute myeloid leukemia patients at diagnosis: Survival is inversely correlated with IL-6 and directly correlated with IL-10 levels. Cytokine. 61:885–891. 10.1016/j.cyto.2012.12.023 [DOI] [PubMed] [Google Scholar]
- Sanjuan-Pla A., Macaulay I.C., Jensen C.T., Woll P.S., Luis T.C., Mead A., Moore S., Carella C., Matsuoka S., Bouriez Jones T., et al. . 2013. Platelet-biased stem cells reside at the apex of the haematopoietic stem-cell hierarchy. Nature. 502:232–236. 10.1038/nature12495 [DOI] [PubMed] [Google Scholar]
- Schepers K., Pietras E.M., Reynaud D., Flach J., Binnewies M., Garg T., Wagers A.J., Hsiao E.C., and Passegué E.. 2013. Myeloproliferative neoplasia remodels the endosteal bone marrow niche into a self-reinforcing leukemic niche. Cell Stem Cell. 13:285–299. 10.1016/j.stem.2013.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepers K., Campbell T.B., and Passegué E.. 2015. Normal and leukemic stem cell niches: insights and therapeutic opportunities. Cell Stem Cell. 16:254–267. 10.1016/j.stem.2015.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuettpelz L.G., and Link D.C.. 2013. Regulation of hematopoietic stem cell activity by inflammation. Front. Immunol. 4:204 10.3389/fimmu.2013.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sitnicka E., Bryder D., Theilgaard-Mönch K., Buza-Vidas N., Adolfsson J., and Jacobsen S.E.. 2002. Key role of flt3 ligand in regulation of the common lymphoid progenitor but not in maintenance of the hematopoietic stem cell pool. Immunity. 17:463–472. 10.1016/S1074-7613(02)00419-3 [DOI] [PubMed] [Google Scholar]
- Smith C.C., Wang Q., Chin C.S., Salerno S., Damon L.E., Levis M.J., Perl A.E., Travers K.J., Wang S., Hunt J.P., et al. . 2012. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia. Nature. 485:260–263. 10.1038/nature11016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian A., Tamayo P., Mootha V.K., Mukherjee S., Ebert B.L., Gillette M.A., Paulovich A., Pomeroy S.L., Golub T.R., Lander E.S., and Mesirov J.P.. 2005. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA. 102:15545–15550. 10.1073/pnas.0506580102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsimberidou A.M., Estey E., Wen S., Pierce S., Kantarjian H., Albitar M., and Kurzrock R.. 2008. The prognostic significance of cytokine levels in newly diagnosed acute myeloid leukemia and high-risk myelodysplastic syndromes. Cancer. 113:1605–1613. 10.1002/cncr.23785 [DOI] [PubMed] [Google Scholar]
- van der Maaten L. 2014. Accelerating t-SNE using tree-based algorithms. J. Mach. Learn. Res. 15:3221–3245. [Google Scholar]
- van der Maaten L., and Hinton G.. 2008. Visualizing data using t-SNE. J. Mach. Learn. Res. 9:2579–2605. [Google Scholar]
- Veiby O.P., Jacobsen F.W., Cui L., Lyman S.D., and Jacobsen S.E.. 1996. The flt3 ligand promotes the survival of primitive hemopoietic progenitor cells with myeloid as well as B lymphoid potential. Suppression of apoptosis and counteraction by TNF-α and TGF-β. J. Immunol. 157:2953–2960. [PubMed] [Google Scholar]
- Wills Q.F., and Mead A.J.. 2015. Application of single-cell genomics in cancer: Promise and challenges. Hum. Mol. Genet. 24(R1):R74–R84. 10.1093/hmg/ddv235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woll P.S., Kjällquist U., Chowdhury O., Doolittle H., Wedge D.C., Thongjuea S., Erlandsson R., Ngara M., Anderson K., Deng Q., et al. . 2014. Myelodysplastic syndromes are propagated by rare and distinct human cancer stem cells in vivo. Cancer Cell. 25:794–808. 10.1016/j.ccr.2014.03.036 [DOI] [PubMed] [Google Scholar]
- Wu A.R., Neff N.F., Kalisky T., Dalerba P., Treutlein B., Rothenberg M.E., Mburu F.M., Mantalas G.L., Sim S., Clarke M.F., and Quake S.R.. 2014. Quantitative assessment of single-cell RNA-sequencing methods. Nat. Methods. 11:41–46. 10.1038/nmeth.2694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Bryder D., Adolfsson J., Nygren J., Månsson R., Sigvardsson M., and Jacobsen S.E.. 2005. Identification of Lin(-)Sca1(+)kit(+)CD34(+)Flt3- short-term hematopoietic stem cells capable of rapidly reconstituting and rescuing myeloablated transplant recipients. Blood. 105:2717–2723. 10.1182/blood-2004-06-2159 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.