Abstract
The epidermoid cyst is a development cyst, skin, filled with keratin and imprisoned by stratified squamous epithelium similar to skin. They are more frequent in males. Clinically presenting as flabby, prevalent over the face, neck and back. They are usually asymptomatic and its etiology is directly linked to trauma, as well as the imprisonment of epithelial rests during embryonic fusion. This study aims to present a case report of a patient 54 years old, with an epidermal cyst in the face, which was treated surgically.
Keywords: Diagnostics, epidermal cyst, surgery
Introduction
Epidermoid cyst is considered benign lesion that usually affect the scalp regions, face, neck, back, and torso. It is commonly asymptomatic, however, it may become symptomatic due to secondary infection or when it reaches dimensions that can cause damage to the surrounding anatomical structures.[1] It occurs in a wide age range, that is, from birth to 72 years and frequently arises in individuals between 15 and 35 years. It can develop in any part of the body; it has a slow growth and is rare. 7% of these cysts occur in the head and neck, oral cavity representing only 1.6%.[2]
These skin structures are represented by hair, sebaceous glands, hair follicles, and sweat glands. Epidermoid cysts are either congenital or acquired.[3]
Epidermoid cysts have prevalence for males and originate from the infundibular epithelium hyperplasia in response to an inflammatory process in the hair follicle. They can develop in isolation or multifocal form, as can be seen in Gardner's syndrome. Surgical enucleation if the recommended treatment for epidermoid cysts.[4]
This work aims to report a case of a patient 54-year-old, with an epidermal cyst in the face.
Case Report
Male patient, 54-year-old, feoderm attended the university hospital Oral and Maxillofacial Surgery and Traumatology Department of the Federal University of Mato Grosso do Sul, Mato Grosso do Sul, Brazil, on referral by a public health professional. Ovoid swelling was found >5 cm in diameter on the right submandibular region [Figures 1 and 2]. Clinical examination showed a mobile lesion, well defined and soft on palpation. The patient denied having suffered any trauma or having undergone any surgical procedure in that region. He reported that the lesion began to develop 10 years ago and decided to seek expert help mainly for esthetic reasons, as this 10-year period had no symptoms. The patient had no significant medical history.
Figure 1.

Extensive edema in the right hemiface causing asymmetry from the region of the outer corner of the mouth to the submandibular region
Figure 2.

In a lower view, one can better visualize the limits of the lesion. Oval and well delimited
Computed tomography (CT), ultrasound and fine needle aspiration (FNA) were performed. A CT scan showed large encapsulated homogeneous mass, near the right mandibular angle. The lesion was >5.0 cm in diameter, with a clear boundary, [Figure 3].
Figure 3.

Axial computed tomography. Homogeneous mass, well circumscribed with more than five centimeters in its greatest extensionagreement
Ultrasound image showed hypoechoic cystic lesion, well outlined, without the Doppler vascularity without calcifications and measuring 5.3 cm × 4.6 cm × 5.1 cm [Figure 4].
Figure 4.
Ultrasound of the cystic lesion. Hypoechoic cystic lesion measuring 5.3 cm × 4.6 cm × 5.1 cm
FNA produced a very characteristic odor when the contents of the cyst was aspirated. The material collected with FNA had a thick consistency. Report of FNA cytology revealed the presence of rare vacuoles of fat and no malignancy criteria, which was very nonspecific. Therefore, based on the clinical information and laboratory test, it was decided to perform an excisional biopsy of the lesion. The enucleation of the lesion was performed under general anesthesia, and surgical specimen was sent for histopathological examination to confirm the diagnosis [Figure 5]. Microscopic examination showed cystic lesion lined by stratified flat epithelium. Granular layer well developed and it showed the presence of ortoceratina in light of the cyst [Figure 6].
Figure 5.

Well delimited mass being removed in a single block, surgically
Figure 6.
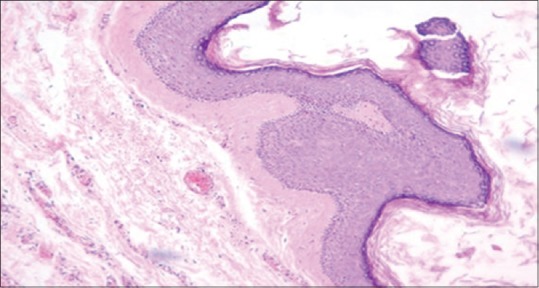
Epidermal cyst-cystic cavity lined by stratified squamous epithelium and filled with corneal lamellae anucleate
A skin track was removed to compensate for the excessive presence of expanded skin and prevent its sagging [Figure 7]. The patient returned after 7 days, for review. The surgical wound was in the repair process within the normal range. The patient is in outpatient follow-up [Figure 8].
Figure 7.

Excess skin removed to facilitate primary closure and improvement in esthetic quality after removal of cystic masswithout
Figure 8.
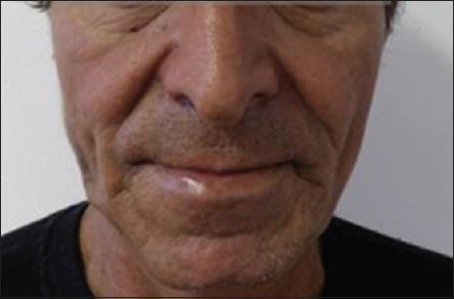
Postoperative appearance of 1 month. Esthetic quality. Facial symmetry
Discussion
Epidermoid cysts are benign, slow growing high, round, firm, subcutaneous, or intradermal which usually grow 1–5 cm in diameter and are usually asymptomatic.[5] The clinical characteristics presented by the lesion of this report are in agreement with what has been described by Kalgutkar et al.,[5] in 2006. It is noteworthy that an epidermoid cyst with a diameter ≥5 cm is rare.[6]
Epidermoid cysts of exacerbated sizes are easier to break, being more susceptible to secondary infection. Another important point is when these giant cysts develop in the head and neck region, as due to the high visibility of these regions the patient may experience depression and anxiety caused by the esthetic appearance of the lesion.[1] In this case report, when the patient was asked about some disruption, infection or pain in relation to cystic lesion, he said he never felt pain and that the cyst had never cracked or suffered infections. He said the “massive” lesion was already growing for 10 years and he sought treatment for esthetic reasons. Park et al.[1] in 2014, reported a case of giant epidermoid cyst in the posterior region of the neck which had developed for more than 40 years, without inflammation or rupture of the lesion.
For the development of an epidermoid cyst, a combination of factors may be responsible, trauma, epithelial proliferation or minimal inflammation. It is difficult to predict that these factors may occur concomitantly, which might explain the rarity of these cases. As epidermoid cysts are usually asymptomatic and slow growing, usually, the patient cannot associate lesion with a possible suffered trauma.[7] The patient, in this case, did not report any history of trauma or surgical procedure in the region of the cyst, as expounded Kini et al.,[7] in 2013. Without trauma as a cause of the appearance of epidermal cyst in our patient; he opened room for believing in a possible congenital strain to the case, as Kudoh et al.[3] in 2013, reported a congenital variant of epidermal cyst involving the ectodermal tissues. We do not know for sure if the cause of the appearance of this pathological entity, in this case report is linked to trauma or is congenital. Regarding the differential diagnosis should include conditions that are linked to development processes, infectious, and neoplastic.[7]
In our case clinical signs of infection were not present. Neoplastic conditions were excluded since lesion was benign without nodal involvement. Other conditions to be taken into account are lipomas, and salivary vascular lesions, but the meticulous physical examination and the help of additional investigations such as ultrasound, helped us to rule out these other pathological conditions. Importantly, there are reports in the literature of malignant changes in epidermoid cysts.[8] In our case, the specimen submitted to pathology analysis showed no malignancy.
Dermoid cysts also feature as differential diagnosis for epidermoid cysts; however, one should not overlook the etiology and location of each. The dermoid cysts arise from the imprisonment of epithelial rests during embryonic fusion, so they are seen in fusion areas, especially in the midline. Unlike the dermoid cysts, epidermoid cysts can develop in any part of the body.[2]
Epidermoid cysts are commonly seen affecting young males, and constitute 79% of cutaneous cysts.[4,9] Treatment for cysts is through surgical enucleation, where it is recommended to remove as much of the capsule of the cystic contents, so that it has no recurrence.[4,7,10] The approach adopted in this clinical case was surgical enucleation of the epidermoid cyst.
Conclusion
In this case report, we present an epidermoid cyst larger than 5 centimeters in diameter, which is rare in the literature. Thus, we hope to contribute to the current scientific literary collection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Park TW, Kim JK, Kim JR. Giant epidermal cyst in the posterior neck developing over 40 years: A case report. Exp Ther Med. 2014;7:287–9. doi: 10.3892/etm.2013.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janarthanam J, Mahadevan S. Epidermoid cyst of submandibular region. J Oral Maxillofac Pathol. 2012;16:435–7. doi: 10.4103/0973-029X.102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kudoh M, Harada H, Omura K, Ishii Y. Epidermoid cyst arising in the submandibular region. Case Rep Med 2013. 2013 doi: 10.1155/2013/419289. 419289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tancredi ARC, Ribeiro-Júnior O, Higo CD, Pedron IG, Lemos-Júnior CA. Epidermoid cyst in the labial comissure region: Case report. Clin Pesq Odontol. 2006;2:329–32. [Google Scholar]
- 5.Kalgutkar A, Kini S, Jambhekar N, Das S. Intradiploic primary epithelial inclusion cyst of the skull. Ann Diagn Pathol. 2006;10:20–3. doi: 10.1016/j.anndiagpath.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Kang SG, Kim CH, Cho HK, Park MY, Lee YJ, Cho MK. Two cases of giant epidermal cyst occurring in the neck. Ann Dermatol. 2011;23(Suppl 1):S135–8. doi: 10.5021/ad.2011.23.S1.S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kini YK, Kharkar VR, Rudagi BM, Kalburge JV. An unusual occurrence of epidermoid cyst in the buccal mucosa: A case report with review of literature. J Maxillofac Oral Surg. 2013;12:90–3. doi: 10.1007/s12663-011-0188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López-Ríos F, Rodríguez-Peralto JL, Castaño E, Benito A. Squamous cell carcinoma arising in a cutaneous epidermal cyst: Case report and literature review. Am J Dermatopathol. 1999;21:174–7. doi: 10.1097/00000372-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Golden BA, Zide MF. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2005;63:1613–9. doi: 10.1016/j.joms.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Barbieri L, Hideo Kajita R, Matielo Galli A, Flório Mediotti G, Cozar Figueiredo K, Martins Fontes T, Parreira SF. Epidermal cyst: a case review. Conscientiae Saúde. 2006;5:115–20. [Google Scholar]


