Abstract
An elderly female patient presented to surgical outpatient clinic with complaint of gradual onset of painless submental and sublingual midline swellings for 6 months of duration. The swellings were noncompressible, nontranslucent, nonpulsatile, and nontender on palpation. Clinical diagnosis was plunging ranula or dermoid cysts. Ultrasound examination of sublingual swelling showed cystic lesion with particulate content. Submental swelling showed cystic swelling with few echogenic floating lobules inside suggesting possibility of epidermoid/dermoid cyst. Magnetic resonance imaging of the face showed homogeneous fluid content within the sublingual cystic lesion and heterogeneous fluid content with few floating nodules within submental swelling. Both cystic lesions were noncommunicative and were showing diffusion restriction and no fat signal. Radiological diagnosis was sublingual and submental epidermoid cysts. She was operated under general anesthesia, and two separate cystic masses were excised with intact capsule. Histopathological diagnosis of masses confirms epidermoid cyst. Several literature have reported isolated sublingual or submandibular epidermoid cyst. However, concurrent sublingual and submental epidermoid cysts with different imaging appearance are rarely reported.
Keywords: Dermoid cyst, epidermoid cyst, sublingual, submandibular
Introduction
Epidermoid and dermoid cysts are slow-growing benign swellings and can occur anywhere in the body. It is seen over the head and neck area in about 7% of cases and within oral cavity in 1.6% of cases.[1] These cystic lesions are categorized as epidermoid, dermoid, and teratoid variant. Epidermoid cyst shows squamous epithelial lining with fibrous wall with no skin appendage while true dermoid cyst shows epithelial wall lining with identifiable skin appendageal structure. The teratoid cyst lining varies from squamous to ciliated respiratory epithelium with derivatives from ectoderm, mesoderm, and/or endoderm.[2] Epidermoid cysts develop due to inclusion of the ectodermal elements at the fusion sites between the first and second branchial arches during the third and fourth embryonic weeks.[3] PubMed literature search was done with the words “sublingual, submental, and epidermoid cyst” and eight case reports of epidermoid cysts in sublingual and/or submental area were found [Table 1]. Only two cases of concurrent sublingual and submental epidermoid cysts have been published.[6,7] We report our case, a rare case of large concurrent sublingual and submental epidermoid cysts in an elderly woman, and discuss the pertinent literature briefly.
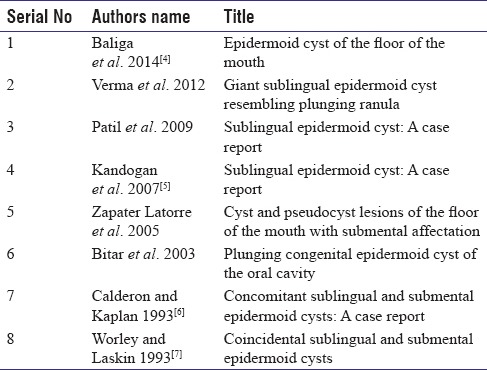
Table 1.
Details of intraoral/submental epidermoid reported in literature
Case Report
A 55-year-old female patient came to surgical outpatient clinic with complaint of gradual increasing painless swelling of the floor of the mouth and submental region under the tongue and beneath the chin with difficulty in speech and swallowing for 6 months of duration. No history of trauma, operation, or prolonged fever was present. She was nondiabetic, nonhypertensive and had no history of tuberculosis or chronic illness. On clinical examination, her vitals were within normal limit. Central nervous system, cardiovascular, and chest and abdominal examination revealed no abnormality. Local examination revealed cystic, nonpulsatile, noncompressible, nontender, and nontranslucent sublingual and submental swellings [Figure 1a and b]. The submental swelling was not moving with tongue protrusion. No sign of inflammation was present. No transmitted pulsation over the sublingual swelling was felt during compression of submental swelling and vice versa. Clinical diagnosis was plunging ranula or dermoid/epidermoid cyst. Ultrasound examination of the sublingual swelling showed cystic swelling with uniform low-level echogenicity, internal particulate content with no internal vascularity on the color Doppler study [Figure 1d]. The submental lesion revealed particulate internal content with multiple floating echogenic lobules (like stalk of marble) inside the cystic swelling with no posterior acoustic shadow and no evidence of internal vascularity on color Doppler study [Figure 1c]. Noncontrast-enhanced computed tomography (CT) of the face shows hypodense cystic lesion in the sublingual and submental region [Figure 2a]. Magnetic resonance imaging of the face revealed two separate sublingual and submental cystic lesions showing T1-weighted hyperintense, T2-weighted/short tau inversion recovery (STIR) hyperintense signal and diffusion restriction in diffusion weighted image (DWI), and apparent diffusion coefficient (ADC) sequences [Figure 2b–f]. The submental swelling shows T1-/T2-weighted hypointense discrete nodular structures within the fluid content. No fat signal was seen within the both swellings. Radiological diagnosis was sublingual and submental epidermoid cysts. She was operated under general anesthesia. Both cystic lesions were enucleated by intraoral sublingual dissection with intact capsules, and the opening in the floor of the mouth was marsupialized [Figure 3a–c]. The sublingual cyst was below the floor of mouth mucosa and the submental cyst was between genioglossus muscles. The cystic lesions were pearly white and revealed epidermoid cyst on histopathological examination [Figure 4a and b]. The echogenic nodules of submental lesion in ultrasonography (USG) study were keratin accumulation. Her postoperative period was uneventful. She was advised for 6 monthly follow-up for 2 years. No recurrence was seen during 18 months of postoperative follow-up.
Figure 1.

Submental swelling with “double chin” appearance (a), sublingual swelling (b). Ultrasonography of submental swelling shows thick walled unilocular cystic swelling with fluid content and floating nonshadowing echogenic nodules like “stack of marbles” (c) and sublingual swelling shows unilocular cystic lesion with internal homogeneous particulate component (d)
Figure 2.
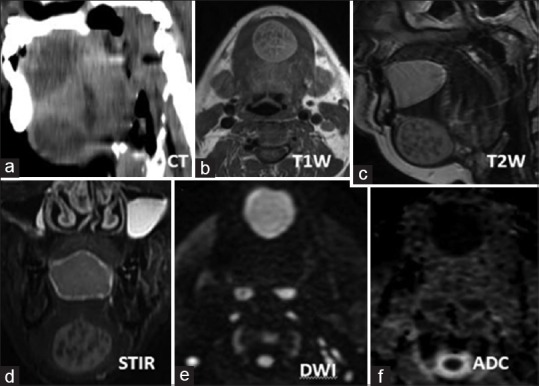
Hypodense cystic sublingual and submental swelling (a) which on magnetic resonance imaging images shows T1-weighted hyperintense (b), T2-weighted/short tau inversion recovery hyperintense signal (c and d), diffusion restriction in diffusion weighted image/apparent diffusion coefficient (e and f). The submental lesion shows T1-weighted/T2-weighted/short tau inversion recovery hypointense nodules within the fluid content
Figure 3.
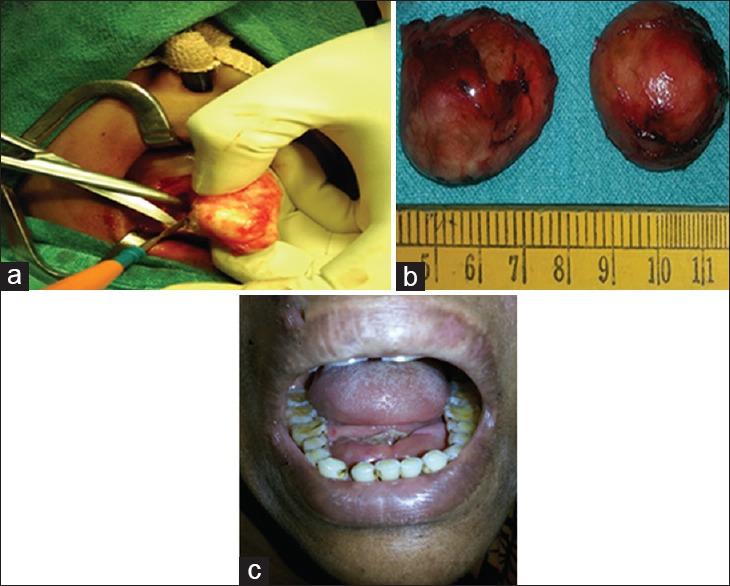
Intraoperative picture of sublingual mass dissection and enucleation of epidermoid cyst (a) and excised epidermoid cysts with intact capsule on the table (b). The postoperative picture (c) shows postoperative scar underneath the tongue and disappearance of sublingual swelling
Figure 4.
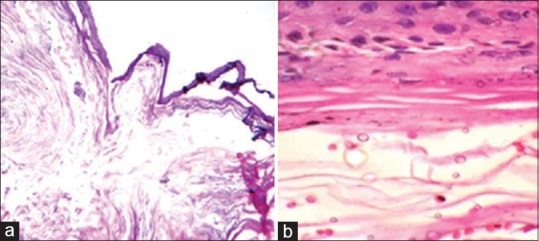
Microscopic examination of the lesions showing stratified squamous epithelial lining with accumulated keratin and underlying fibrous tissue with small blood vessels in low and high magnification (a and b)
Discussion
Epidermoid cysts are categorized into congenital and acquired type depending on its development. The congenital epidermoid cysts develop due to entrapment of ectodermal element between the first and second branchial arches during the 3rd and 4th weeks of intrauterine life. Acquired epidermoid cyst arises from the traumatic/iatrogenic inclusion of ectoderm or occlusion of sebaceous gland duct. Some other authors suggest that these are the variant of thyroglossal cyst. Epidermoid and dermoid cysts constitute < 0.01% of all oral cavity cysts.[5]
The floor of the mouth and submandibular area are affected by various pathological conditions which are classified into congenital, inflammatory, obstructive, and neoplastic lesions. The benign congenital/acquired cystic lesions show delayed presentation due to its slow, painless growth pattern and often present during 15–35 years of age.[8] Patient with intraoral lesion presents with difficult in swallowing, phonation, breathing, tongue movement, and buggy feeling in the floor of mouth while submental/submandibular lesions manifest as painless double chin appearance.[4,5] Our case presented with difficulty in speech, swallowing, and double chin appearance. On palpation, swelling was nontender and seen with doughy/firm consistency and without associated lymphadenopathy.
The differential diagnosis of submental and sublingual benign lesions are plunging ranula, thyroglossal cyst, lymphatic malformation (cystic hygroma), mucocele, branchial cleft cyst, hemangioma, enlarged lymph nodes, and infective lesions.[4] Bimanual palpation and conventional radiography cannot differentiate the lesions. Ultrasound, CT, magnetic resonance imaging (MRI), and fine-needle aspiration cytology (FNAC) are the preferred modality for the preoperative diagnosis.[8] The epidermoid cyst shows cystic/solid appearing structure with homogeneous/heterogeneous internal content. CT scan of the lesions shows thin-walled unilocular cystic lesion with low attenuated (CT Hounsfield unit 0–18) intracystic content with multiple low-dense nodules giving sac of marble appearance which is pathognomic for dermoid cyst. MRI of the lesions shows thin-walled unilocular cystic lesion with T1-weighted hypointense, T2-weighted hyperintense intracystic content with diffusion restriction. The cyst may show increased T1 signal due to fat or protein component. The fat signal will be suppressed in STIR sequence. MRI has got advantage of better soft tissue visualization, characterization, and multiplanar acquisition. The dermoid may show multiple intracystic nodules due to fat globules, whereas epidermoid cyst may show similar finding due to keratin globules. Postcontrast-enhanced image may show peripheral rim enhancement.[9] Plunging ranula has communication between sublingual and submandibular component and shows homogeneous appearance in MRI/CT/USG images and is indistinguishable from epidermoid/dermoid with homogeneous internal content on imaging. In our case, there was no communication between the lesions, and the submental lesion was heterogeneous in appearance. Intraoral lipoma is differentiated due to fat signal in MRI. Lymphatic malformation shows nonenhancing multiple septation and locule. Malignant mass of the region shows enhancing solid component. Intraoral abscess is painful and show perilesional inflammatory signs on imaging. In our case, both the sublingual and submental lesions were painless lesions and showed imaging features of epidermoid/dermoid. FNAC of the sublingual lesion revealed putty-like material suggesting keratin content of epidermoid cyst.
Surgical excision with complete capsule removal is the treatment of choice for sublingual and submandibular/submental benign cystic lesion. The lesions above the mylohyoid muscle are approached intraorally and lesions below the mylohyoid muscles are removed by extraoral approach.[8] In our case, intraoral approach was used for excision of both the lesions with intact capsule. Histopathological examination confirms the cystic lesions as epidermoid cyst as no skin appendageal structure was found within the lesions. The submental lesion shows intracystic keratinized nodules.
Recurrence of epidermoid in the floor of the mouth is low as complete enucleation of cysts along with its fibrous capsule is possible. Malignant transformation of sublingual epidermoid cysts is rare and can occur.[10,11]
Conclusion
Concurrent sublingual and submandibular epidermoid is a rare occurrence. USG, CT/MRI, and FNAC are essential for preoperative diagnosis and planning of surgical approach. Complete surgical excision with intact capsule is the treatment of choice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Turetschek K, Hospodka H, Steiner E. Case report: Epidermoid cyst of the floor of the mouth: Diagnostic imaging by sonography, computed tomography and magnetic resonance imaging. Br J Radiol. 1995;68:205–7. doi: 10.1259/0007-1285-68-806-205. [DOI] [PubMed] [Google Scholar]
- 2.Meyer I. Dermoid cysts (dermoids) of the floor of the mouth. Oral Surg Oral Med Oral Pathol. 1955;8:1149–64. doi: 10.1016/0030-4220(55)90380-7. [DOI] [PubMed] [Google Scholar]
- 3.De Ponte FS, Brunelli A, Marchetti E, Bottini DJ. Sublingual epidermoid cyst. J Craniofac Surg. 2002;13:308–10. doi: 10.1097/00001665-200203000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Baliga M, Shenoy N, Poojary D, Mohan R, Naik R. Epidermoid cyst of the floor of the mouth. Natl J Maxillofac Surg. 2014;5:79–83. doi: 10.4103/0975-5950.140185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kandogan T, Koç M, Vardar E, Selek E, Sezgin O. Sublingual epidermoid cyst: A case report. J Med Case Rep. 2007;1:87. doi: 10.1186/1752-1947-1-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calderon S, Kaplan I. Concomitant sublingual and submental epidermoid cysts: A case report. J Oral Maxillofac Surg. 1993;51:790–2. doi: 10.1016/s0278-2391(10)80425-2. [DOI] [PubMed] [Google Scholar]
- 7.Worley CM, Laskin DM. Coincidental sublingual and submental epidermoid cysts. J Oral Maxillofac Surg. 1993;51:787–90. doi: 10.1016/s0278-2391(10)80424-0. [DOI] [PubMed] [Google Scholar]
- 8.Yoshida N, Kodama K, Iino Y. Sublingual epidermoid cyst presenting with distinctive magnetic resonance imaging findings. Clin Pract. 2014;4:664. doi: 10.4081/cp.2014.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ariyoshi Y, Shimahara M. Magnetic resonance imaging of a submental dermoid cyst: Report of a case. J Oral Maxillofac Surg. 2003;61:507–10. doi: 10.1053/joms.2003.50097. [DOI] [PubMed] [Google Scholar]
- 10.Devine JC, Jones DC. Carcinomatous transformation of a sublingual dermoid cyst. A case report. Int J Oral Maxillofac Surg. 2000;29:126–7. [PubMed] [Google Scholar]
- 11.Kudoh M, Harada H, Omura K, Ishii Y. Epidermoid cyst arising in the submandibular region. Case Rep Med 2013. 2013 doi: 10.1155/2013/419289. 419289. [DOI] [PMC free article] [PubMed] [Google Scholar]


