Abstract
Modern dentistry has changed tremendously with implant therapy. For the successful implant therapy, making a proper treatment plan considering both surgical and prosthetic part in mind is the key of success. Often practitioners tend to create a treatment plan overlooking the basic principles of prosthetic part. This present review has discussed various prosthetic consideration of implant-supported prosthesis. A step-by-step detailed prosthetic option with their indications has been discussed to help all dental implant practitioners in making of an optimal treatment plan for each case.
KEYWORDS: Diagnosis, implant supported prosthesis, surgical guide, treatment planning
INTRODUCTION
The goal of modern dentistry is to restore the normal contour, function, comfort esthetics, speech, and health regardless of the atrophy, disease, or injury of the stomatognathic system.[1] However, the more the number of teeth missing in a patient, it becomes more difficult to achieve this goal with traditional dentistry. Dental implantology is a term used today to describe anchoring of alloplastic material into the jaws to provide support and retention for prosthetic replacement of teeth that has been lost.[2] To date, overall positive experiences and generation of new knowledge have targeted the immediate future as a time to establish endosteal dental implants as a routinely applied treatment modality in dentistry. As a result of research, advances in implant designs, materials, and techniques have led to predictable success in their application, and several types of implants are now available for use in rehabilitation of different clinical problems. The patient's function when wearing a conventional complete denture prosthesis may be reduced to 60% of that formerly experienced with natural dentition. Implant prosthesis offers a predictable treatment course than the traditional restorations.[3]
The increased need and use of implant-related treatments result from the combined effect of a number of factors including psychological aspects of tooth loss, aging population, tooth loss related to age, anatomic consequences of edentulism, poor performance of removable prosthesis, and predictable long-term results of implant-supported prostheses.[3]
TREATMENT PLANNING: A SEQUENTIAL ANALYSIS
Over the last decade, reconstruction with dental implants has changed considerably. Rather than merely focusing on the tooth or teeth to be replaced, today's implant practitioner considers a broad and complex set of interwoven factors before formulating a treatment plan. The treatment planning phase is divided into three stages.[4]
INITIAL CONSULTATION
The initial consultation is the first step in determining whether a patient qualifies for a reconstructive procedure. A preliminary treatment plan based on chief complaint of the patient, history of present illness, medical history, and clinical and radiographic examination, to be made. Diagnostic impressions should be made to obtain accurate study models. Bone mapping procedures may be carried out to assess the available bone volume. Based on this clinical examination, an appropriate imaging modality is selected to attain information about the proposed implant site. The patient's facial appearance should be documented with preoperative extraoral and intraoral photographs. The initial consultation should also serve to educate and orientate the patient. Visual aids (such as educational models, photographs, and videos) and printed literature are useful in this regard.
JOINT TREATMENT PLANNING
The next phase in the treatment planning process involves the entire implant team including the surgeon (if separate), prosthodontist, and other specialists. The hygienist or laboratory technician may also be included. The planning conferences provide opportunities for the team to review the patient's chief complaints, expectations, history, and current medical and dental status. Based on all this information, team members can formulate a detailed treatment plan.
FINAL TREATMENT CONSIDERATIONS
Various treatment options can be presented to the patient for approval. The patient should be informed to the anticipated number of implants and whether any ancillary procedures are required. If a grafting procedure is indicated, the patient must also be aware of the various materials available for the graft. There should also be full disclosure as to whether these procedures will be performed under local anesthesia, local anesthesia supplemented with intravenous sedation, or general anesthesia. The benefit–risk ratio of all these procedures should be presented. The postoperative course should be carefully described to patients. Written consents should be secured for both the surgical and restorative procedures. A full disclosure of potential complications is essential. The best course for the implant practitioner is to present the patient with global and domestic statistics for implant success rates as documented in the literature.[5]
PATIENT SELECTION: ORAL AND SYSTEMIC CONSIDERATIONS
The bone and soft tissue response following endosseous dental implant placement is controlled by wound healing factors, biomechanics, and mineral metabolism. Due to the complexity of the tissue response, osseointegration and maintenance of endosseous dental implants may be influenced by many factors including age, diet, drugs, systemic disease, and oral disease.[6] In general, endosseous dental implant may be considered for any patient in reasonable health who desires the replacement of missing teeth and has enough bone in the area or can undergo a bone augmentation procedure.[6] Various factors and their influence on dental implant therapy are physical status and age of patient, hypohidrotic ectodermal dysplasia, smoking, osteoporosis, diabetes mellitus, scleroderma, multiple myeloma, Parkinson's disease, etc.[7]
RADIOGRAPHIC ASSESSMENT: DECISION-MAKING CRITERIA
An acceptable clinical examination and an appropriate radiographic examination are mandatory before every implant surgery. Diagnostic imaging and techniques help develop and implement a cohesive and comprehensive implant treatment plan.[8] The purpose of implant imaging is to provide accurate and reliable diagnostic information on the patient's anatomy at the proposed implant sites. Current radiation protection regulations are based on justification and the as low as reasonably achievable principle. This implies that every radiographic examination must be carried out to the benefit of the patient by application of the lowest possible dose. Therefore, the selection of imaging technique is already part of radiation protection measures.[9]
DIAGNOSTIC CASTS
Diagnostic casts or study models are essential to help guide both the preimplant and treatment phases of implant therapy.[3] Many patients have been partially edentulous for an extended period of time. The combination of continued bone loss and dentition changes related to missing teeth greatly increases the factors that must be considered for oral rehabilitation with implants. Diagnostic casts enable these prosthodontic factors, for example, maxillomandibular relationships, existing occlusion, and potential future occlusal schemes to be evaluated in the absence of the patient.
DIAGNOSTIC TEMPLATES
COMPUTED TOMOGRAPHY
Although computed tomography (CT) procedures can identify the available bone height and width accurately at a proposed implant site, the exact position and orientation of the implant (which many times determine the actual length and diameter of the implant) often are dictated by the prosthesis.[3] A diagnostic template is most beneficial with this imaging technique.[3,10]
TYPES OF DIAGNOSTIC TEMPLATES
Vacuform template
This is produced by a vacuform reproduction of the diagnostic cast and has a number of variations:
The proposed restoration on the diagnostic wax-up is coated with a thin film of barium sulfate. This coating should be done before the fabrication of template. Due to this, on CT examination, restorations become evident, but exact position and orientation of proposed implant cannot be identified
Blend of 10% barium sulfate and 90% cold cure acrylic are used to fill proposed restoration sites in vacuform of diagnostic wax-up. This leads to radiopaque appearance on CT examination at the proposed restorations. However, the precise position and orientation of proposed implant cannot be identified
The previous design is modified by drilling a 2 mm channel through the occlusal surface of the proposed restoration using a twist drill. This corresponds to the ideal position and orientation of the implant and is identified on CT examination.
Acrylic template
Diagnostic wax-up provides an acrylic template.[11] This is modified by a thin coating of barium sulfate, and a hole drilled the occlusal surface of proposed restorations followed by filling this hole by gutta-percha.[3] This provides radiopacity of the proposed restoration on CT examination, and precise position and orientation of proposed implant may be identified by radiopaque plug of gutta-percha.
Template fabricated with radiopaque denture teeth
These radiopaque denture teeth are specifically manufactured for implant imaging purposes and are used for the diagnostic wax–up and subsequently are incorporated into the template. If acceptable, it may be modified into a surgical template at a later stage. This serves to transfer these findings to the patient at the time of surgery.
COMPLEX TOMOGRAPHY
Diagnostic templates of CT examination are generally more precise than tomography examination.[3] The simple method to produce tomography template is by placing 3 mm ball bearing at proposed implant positions in vacuform of diagnostic cast. Ball bearing can serve as a measure of magnification of the image.
PANORAMIC RADIOGRAPHY
A diagnostic template can be used with panoramic radiographs to assess the amount of magnification. Five millimeters ball bearings or wires are incorporated around the curvature of the arch while fabricating the template. The amount of magnification can subsequently be determined in the radiograph which helps in offsetting the inherent inaccuracy in this technique.[9]
PROSTHETIC OPTIONS IN IMPLANT DENTISTRY
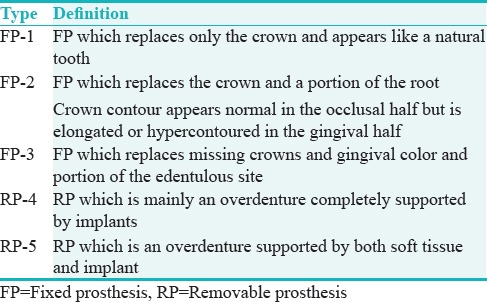
Implant dentistry is unique because additional foundation units may be created for a desired prosthodontic result. Thus, a range of treatment options are available to most partially and completely edentulous patients. In the past, greater emphasis has been placed on the bone available for implant insertion which determines the position and number of implants and consequently, the final prosthesis design.[12] However, the implant treatment plan of choice is both patient and problem centered and requires a shift in this traditional approach. The benefits of implant dentistry can be realized only when the full range of available options for the final prosthesis is first evaluated by the practitioner and then presented to the patient. Thus, it is important to first visualize the intended final prosthesis based on which the existing bone is evaluated to determine the type and number of implants necessary to support the intended prosthesis.[13] In 1989, Misch proposed five prosthetic options FP-1, FP-2, FP-3, RP-4 and RP-5 [Table 1].
Table 1.
Prosthodontic options[3]
AVAILABLE BONE: INFLUENCE ON PROSTHETIC TREATMENT PLANNING
Different bone volume requires treatment plan approached dental implant placement. Misch and Judy (1985) given a classification system for the available bone with treatment options for all categories.[14,15]
PROSTHETIC OPTIONS AVAILABLE IN DIVISION A BONE
FP-1 restorations: For ideal implant placement and natural esthetic appearance of final prosthesis require Division A bone
FP-2 or FP-3 restorations: These prosthetic options may be considered depending on amount of bone loss and lip positions
RP-4 or RP-5 restorations: These conditions may require osteoplasty considering interarch space to accommodate denture teeth.
PROSTHETIC OPTIONS AVAILABLE IN DIVISION B BONE
FP-2 or FP-3 restorations are indicated in this condition to compensate increased clinical height.[16] Osteoplasty to get Division A ridge is mostly indicated in anterior mandible because of fewer esthetic concerns in this region.
PROSTHETIC OPTIONS AVAILABLE IN DIVISION C BONE
More number of implants are required to expand implant-bone surface area. In edentulous patients, RP-5 prosthesis may be considered. Recent studies have advocated the use of shorter textured implant more suitable option in posterior maxilla and mandible with compromised bone height.[17]
PROSTHETIC OPTIONS AVAILABLE IN DIVISION D BONE
Autogenous with bone grafts is indicated to upgrade the division. Endosteal or subperiosteal implants may be inserted depending on the division of bone attained.[18]
BONE DENSITY: INFLUENCE ON PROSTHETIC TREATMENT PLANNING
Besides its external architecture, bone also has an internal architecture represented by its density. The strength of the bone supporting the endosteal implant is directly related to its density.[3] Therefore, bone density exerts a significant influence on the clinical success of implant therapy.[19,20] A range of implant survival has been found relative to location. The anterior mandible has greater bone density than the anterior maxilla.[21] The posterior mandible has poorer bone density than the anterior mandible. The poorest bone density exists in the posterior maxilla and is associated with dramatic failure rates.[21]
As the bone density decreases, the biomechanical loads on the implants must be reduced.[3,22] This can be accomplished in several ways by considering the following prosthetic design.[23,24,25]
Angle of load on the implant body should be more axial and offset loads minimized
Narrower occlusal tables should be designed
Splinting the crowns of adjacent implants with relatively stiff
Restorative materials may be considered
Cantilever length may be shortened or eliminated in case of full-arch restorations for edentulous patients
RP-4 rather than FP prosthesis may be considered in edentulous patients to reduce nocturnal parafunctional forces
RP-5 prosthesis may be considered to permit the soft tissue to share the occlusal force
Night guards and acrylic occlusal surfaces distribute and dissipate the parafunctional forces on an implant system
By considering progressive bone loading.
FORCE FACTORS RELATED TO PATIENT CONDITIONS
Various patient conditions exert different amounts of force in terms of magnitude, duration, type, and direction.[25] These factors such as parafunction (bruxism, clenching, and tongue thrust), direction of load forces, and nature of opposing arch influence the stress environment of the implant and prosthesis.[26] The treatment plan may need to be modified depending on the force factors pertaining to the individual patient.
INFLUENCE ON PROSTHETIC TREATMENT PLANNING
Elimination of premature contacts
An occlusal analysis should be carried out to identify any premature contacts during mandibular excursions. An elimination of eccentric contacts may allow recovery of the periodontal ligament health and muscle activity within 1–4 weeks.[27]
Night guard
A night guard should then be given with even occlusal contacts around the arch in centric occlusion and posterior disocclusion with anterior guidance in all excursive movements. The patient is advised to wear the device for a period of 4 weeks at night. The night guard is then re-fabricated with 0.5–1 mm of colored acrylic resin on the occlusal surface.[28]
Implant considerations in the posterior region
Additional implants – increased implant dimensions are often necessary in the bruxing patient
Occlusal considerations – the anterior teeth may be modified to recreate the proper incisal guidance to avoid posterior interferences during excursions.[29]
Implant considerations in the anterior region
Additional implants preferably of greater diameter are indicated
In the presence of natural, healthy canines, a canine-guided occlusion is the occlusal scheme of choice
If the canine is absent and is restored, then a mutually protected occlusion is indicated.
Clenching
Alteration of the anterior occlusal scheme is not as critical due to the absence of detrimental horizontal forces. A soft night guard with a hard acrylic outer shell and inner soft resilient liner, with slight relief over the implants, is often beneficial in reducing the impact of the forces during parafunction.
Additional occlusal considerations
Centric vertical contacts aligned with the long axis of the implant whenever possible.[3]
Narrow posterior occlusal tables prevent inadvertent lateral forces, decrease the forces necessary for mastication, and leave greater space for the tongue. Adjacent implant crowns may be splinted together.
Enameloplasty of the cusp tips of the opposing natural teeth is indicated to help improve the direction of vertical forces, within the guidelines of the intended occlusion.
Completely edentulous patients
If anatomical conditions do not permit the placement of additional implants in the presence of parafunction, a removable overdenture (RP-4 or RP-5) should be considered. The prosthesis may be removed during periods conducive to noxious habits.
PROSTHETIC OPTIONS IN FIXED FULL-ARCH RESTORATIONS
PORCELAIN-METAL RESTORATION
The main problem encountered with this restoration is related to the added bulk of metal used in the substructure to keep porcelain to its ideal 2 mm thickness. This amount of metal acts as a heat sink during casting procedures which results in porosities and increases the risks of fracture after loading.[30]
HYBRID PROSTHESIS
An alternative option in such situations is the hybrid prosthesis. Because acrylic acts as an intermediary between the porcelain teeth and metal substructure, the impact force during dynamic occlusal loading also may be reduced. Hence, hybrid prostheses are indicated for implant restoration in large crown height spaces as a general rule.[3,30]
MAXILLOMANDIBULAR ARCH RELATIONSHIP: PROSTHETIC CONSIDERATION
Arch relationships often are affected in edentulous ridges due to the faciolingual direction of resorption. As a result, implants often need to be placed more lingual in comparison to the original incisal tooth position. The final restoration is subsequently overcontoured facially to restore the incisal two-thirds for improved esthetics. This results in a cantilevered force on the anterior implant body. The maxilla is affected more often than the mandible because the incisal edge position cannot be modified and is dictated by esthetics, speech, lip position, and occlusion. Furthermore, the hygiene of the prosthesis is compromised due to the overcontour.[31]
TREATMENT CONSIDERATIONS
Anterior cantilevered crowns often require additional implants splinted together and an increase in the anteroposterior (A-P) distance between the most distal and most anterior implants to compensate for the increased lateral loads and moment forces, especially during mandibular excursions.[3,31]
CLASS II RELATION
An anterior cantilever on implants in the mandibular arch may correct an Angle's skeletal Class II jaw relationship.[32] To counteract this force multiplier, the treatment plan is modified by:[3,33]
Increase in implant number, size, and surface area of design
Increase in A-P distance between splinted implants
A RP-4 restoration may be indicated, rather than a FP-3, to prevent food impaction and to facilitate daily care.
CLASS III RELATION
Because the edentulous premaxilla resorbs toward the palate, a Class III relationship is often observed. However, these patients often do not exhibit Class III mandibular mechanics (primarily vertical chewers with little to no anterior excursions during mastication or parafunction). To the contrary, these patients have a full range of mandibular excursions. This exerts significant lateral forces on the maxillary restoration, which is cantilevered off the implant base to obtain a Class I esthetic restoration.
Additional splinted implants in the maxilla are advocated with the widest A-P distance available. This usually requires sinus graft procedures to be incorporated into the treatment plan.
ARCH FORM: PROSTHETIC CONSIDERATION
The edentulous arch form is described as ovoid, tapering, or square. The ovoid arch form is the most common, followed by the square, then the tapered form. The tapering arch form is most often found in skeletal Class II patients. The presence of a square arch form is more common in maxillary edentulous patients due to resorption of the premaxilla region. The arch form is a critical element when anterior implants are splinted with posterior implants to minimize cantilever forces. The distance from the center of the most anterior implant to a line joining the distal aspect of the two most distal implants is called the anteroposterior distance or A-P spread. A greater A-P spread is required in the presence of anterior cantilevers. Thus, a square arch form provides a poorer prognosis than a tapered arch form in this regard. When five anterior implants in the mandible are used for prosthesis support, it has been recommended that the ratio of the distal cantilever to the A-P spread should not exceed 2:5. The other arch form to be considered is that of the replacement teeth which may be cantilevered off position for esthetic reasons. In this regard, a tapered arrangement of teeth offers the poorest prognosis due to the greater offset forces applied. The worst combination of these two arch forms is observed in the edentulous maxilla when a square arch form of bone is used to restore a tapered arch form of teeth. The cantilever of the bone is greatest in this combination.[34,35] The most ideal biomechanical arch form depends on the restorative situation:
The tapering arch form of residual bone is favorable for anterior implants supporting posterior cantilevers due to a greater A-P spread
The square arch form of residual bone is preferred when canine and posterior implants are used to support anterior teeth in either arch
The recommended anterior cantilever dimension in the maxilla is less than that of the posterior cantilever in the mandible because the bone is less dense and forces are directed outside the arch during excursions.
IMPLANT PERMUCOSAL POSITION: PROSTHETIC CONSIDERATION
An implant placed in the improper position can compromise the final results in terms of esthetics, biomechanics, and maintenance. The most compromising position for an implant is too facial because no prosthetic ' “trick” exists to mask it, resulting in compromised esthetics, phonetics, lip position, and function. The permucosal position of the implant abutment is of particular importance for FP-1 prostheses. The ideal position is directly under the incisal edge position of the anterior natural tooth and under the central fossa of posterior natural teeth to be replaced.
NUMBER OF MISSING TEETH: PROSTHETIC CONSIDERATION
Replacement of three adjacent missing teeth in the posterior regions of the mouth with a fixed bridge also usually is contraindicated due to the greater span between abutments. The deflection or bending of a fixed prosthesis varies directly with the cube of the length. Therefore, a fixed prosthesis with one pontic deflects 8 times <1 with two pontics and 27 times less than a restoration with three pontics, all other factors being equal. This greater movement increases the occurrence of porcelain fracture, cement breakage, or screw loosening in the restoration.[3,22]
The number of implants used to support a completely implant-supported restoration in the edentulous mandible usually ranges from 5 to 9 in the mandible, with at least four of these implants inserted between the mental foramens.
A greater implant number in the completely edentulous maxilla is indicated to compensate for the less dense bone and more unfavorable biomechanics and ranges from 6 to 10.[22] At least two or three of these implants should be placed in the premaxilla, depending on the arch shape and other force factors.
For a square maxillary arch form (most favorable), implants may be placed in the canine position, whereas in an ovoid arch form, additional implants in the anterior region should be planned
A tapered anterior maxillary arch form combined with other force factors may require the placement of four implants from canine to canine.
All implants in either arch should be splinted together when fewer implants are used. The final restoration may be segmented (canine to canine and two posterior segments) when the number of implants permits so. Posterior cantilevers in the fixed prosthesis should be limited in the maxilla and rarely extend more than one tooth. However, posterior cantilevers in full arch mandibular restorations are not uncommon, but the cantilever length rarely extends more than two teeth. Of course, the number of cantilevered pontics in both arches depends directly on overall stress conditions.[36,37,38,39]
CONCLUSION
Implants have become the treatment of choice in many, if not most, situations when missing teeth require replacement. Studies of the interaction between implant-supported restorations and the surrounding oral environment appear, fortuitously, to support the conclusion that the human host response to oral implants is favorable. The treatment planning for an implant restoration is unique regarding the number of variables that may influence the therapy. Of prime importance is the recognition of the fact that a definitive treatment plan should be developed sequentially to ensure the best possible service. With appropriate diagnosis and conscientious treatment planning, the use of endosseous oral implants enjoys good prognosis.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Dewan SK, Arora A, Sehgal M, Khullar A. Implant failures: A broader perspective. J Dent Implant. 2015;5:53–9. [Google Scholar]
- 2.Dholam KP, Gurav SV. Dental implants in irradiated jaws: A literature review. J Cancer Res Ther. 2012;8(Suppl 1):S85–93. doi: 10.4103/0973-1482.92220. [DOI] [PubMed] [Google Scholar]
- 3.Misch CE. Dental Implant Prosthetics. 2nd ed. Amsterdam, Netherlands: Elsevier Health Sciences; 2014. [Google Scholar]
- 4.Mehrotra G, Iyer S, Verma M. Treatment planning the implant patient. Int J Clin Implant Dent. 2009;1:12–21. [Google Scholar]
- 5.Babbush CA, Hahn JA, Krauser JT, Rosenlicht JL. Dental Implants – E-Book: The Art and Science. 2nd ed. Philadelphia- United States: Saunders; 2010. [Google Scholar]
- 6.Sugerman PB, Barber MT. Patient selection for endosseous dental implants: Oral and systemic considerations. Int J Oral Maxillofac Implants. 2002;17:191–201. [PubMed] [Google Scholar]
- 7.Guobis Z, Pacauskiene I, Astramskaite I. General diseases influence on peri-implantitis development: A systematic review. J Oral Maxillofac Res. 2016;7:e5. doi: 10.5037/jomr.2016.7305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Binsu S, Nair KC, Nayar S, Tella S. An innovative simplified method for assessing available bone in mandible for implant. J Indian Prosthodont Soc. 2016;16:213–5. doi: 10.4103/0972-4052.167946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shannoun F, Blettner M, Schmidberger H, Zeeb H. Radiation protection in diagnostic radiology. Dtsch črztebl Int. 2008;105:41–6. doi: 10.3238/arztebl.2008.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pal US, Chand P, Dhiman NK, Singh RK, Kumar V. Role of surgical stents in determining the position of implants. Natl J Maxillofac Surg. 2010;1:20–3. doi: 10.4103/0975-5950.69153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asher ES, Evans JH, Wright RF, Wazen JJ. Fabrication and use of a surgical template for placing implants to retain an auricular prosthesis. J Prosthet Dent. 1999;81:228–33. doi: 10.1016/s0022-3913(99)70254-4. [DOI] [PubMed] [Google Scholar]
- 12.Monteiro DR, Silva EV, Pellizzer EP, Filho OM, Goiato MC. Posterior partially edentulous jaws, planning a rehabilitation with dental implants. World J Clin Cases. 2015;3:65–76. doi: 10.12998/wjcc.v3.i1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leles CR, Freire Mdo C. A sociodental approach in prosthodontic treatment decision making. J Appl Oral Sci. 2004;12:127–32. doi: 10.1590/s1678-77572004000200009. [DOI] [PubMed] [Google Scholar]
- 14.Misch CE, Judy KW. Classification of partially edentulous arches for implant dentistry. Int J Oral Implantol. 1987;4:7–13. [PubMed] [Google Scholar]
- 15.Juodzbalys G, Kubilius M. Clinical and radiological classification of the jawbone anatomy in endosseous dental implant treatment. J Oral Maxillofac Res. 2013;4:e2. doi: 10.5037/jomr.2013.4202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nugala B, Kumar BS, Sahitya S, Krishna PM. Biologic width and its importance in periodontal and restorative dentistry. J Conserv Dent. 2012;15:12–7. doi: 10.4103/0972-0707.92599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tutak M, Smektala T, Schneider K, Golebiewska E, Sporniak-Tutak K. Short dental implants in reduced alveolar bone height: A review of the literature. Med Sci Monit. 2013;19:1037–42. doi: 10.12659/MSM.889665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Misch CE, Dietsh F. Autogenous bone grafts for endosteal implants – indications and failures. Int J Oral Implantol. 1991;8:13–20. [PubMed] [Google Scholar]
- 19.Koszuta P, Grafka A, Koszuta A, Lopucki M, Szymanska J. Effects of selected factors on the osseointegration of dental implants. Prz Menopauzalny. 2015;14:184–7. doi: 10.5114/pm.2015.54343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turkyilmaz I, McGlumphy EA. Influence of bone density on implant stability parameters and implant success: A retrospective clinical study. BMC Oral Health. 2008;8:32. doi: 10.1186/1472-6831-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HJ, Yu SK, Lee MH, Lee HJ, Kim HJ, Chung CH. Cortical and cancellous bone thickness on the anterior region of alveolar bone in Korean: A study of dentate human cadavers. J Adv Prosthodont. 2012;4:146–52. doi: 10.4047/jap.2012.4.3.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winter W, Klein D, Karl M. Micromotion of dental implants: Basic mechanical considerations. J Med Eng. 2013;2013:265412. doi: 10.1155/2013/265412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vasconcellos LG, Nishioka RS, Vasconcellos LM, Nishioka LN. Effect of axial loads on implant-supported partial fixed prostheses by strain gauge analysis. J Appl Oral Sci. 2011;19:610–5. doi: 10.1590/S1678-77572011000600011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies SJ, Gray RJ, Young MP. Good occlusal practice in the provision of implant borne prostheses. Br Dent J. 2002;192:79–88. doi: 10.1038/sj.bdj.4801298. [DOI] [PubMed] [Google Scholar]
- 25.Yuan JC, Sukotjo C. Occlusion for implant-supported fixed dental prostheses in partially edentulous patients: A literature review and current concepts. J Periodontal Implant Sci. 2013;43:51–7. doi: 10.5051/jpis.2013.43.2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Misch CE. Consideration of biomechanical stress in treatment with dental implants. Dent Today. 2006;25:80, 82, 84–5. [PubMed] [Google Scholar]
- 27.Verma M, Nanda A, Sood A. Principles of occlusion in implant dentistry. J Int Clin Dent Res Organ. 2015;7(Suppl S1):27–33. [Google Scholar]
- 28.Komiyama O, Lobbezoo F, De Laat A, Iida T, Kitagawa T, Murakami H, et al. Clinical management of implant prostheses in patients with bruxism. Int J Biomater. 2012;2012:369063. doi: 10.1155/2012/369063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monteiro DR, Silva EV, Pellizzer EP, Filho OM, Goiato MC. Posterior partially edentulous jaws, planning a rehabilitation with dental implants. World J Clin Cases. 2015;3:65–76. doi: 10.12998/wjcc.v3.i1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Egilmez F, Ergun G, Cekic-Nagas I, Bozkaya S. Implant-supported hybrid prosthesis: Conventional treatment method for borderline cases. Eur J Dent. 2015;9:442–8. doi: 10.4103/1305-7456.163324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain AR, Nallaswamy D, Ariga P, Philip JM. Full mouth rehabilitation of a patient with mandibular implant screw retained Fp-3 prosthesis opposing maxillary acrylic removable over-denture. Contemp Clin Dent. 2013;4:231–5. doi: 10.4103/0976-237X.114862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brosky ME, Korioth TW, Hodges J. The anterior cantilever in the implant-supported screw-retained mandibular prosthesis. J Prosthet Dent. 2003;89:244–9. doi: 10.1067/mpr.2003.43. [DOI] [PubMed] [Google Scholar]
- 33.Drago C. Ratios of Cantilever Lengths and Anterior-Posterior Spreads of Definitive Hybrid Full-Arch, Screw-Retained Prostheses: Results of a Clinical Study. J Prosthodont. 2016 Jul 14; doi: 10.1111/jopr.12519. doi: 10.1111/jopr.12519. [DOI] [PubMed] [Google Scholar]
- 34.Falk H. On occlusal forces in dentitions with implant-supported fixed cantilever prostheses. Swed Dent J Suppl. 1990;69:1–40. [PubMed] [Google Scholar]
- 35.Michalakis KX, Calvani P, Hirayama H. Biomechanical considerations on tooth-implant supported fixed partial dentures. Journal of Dental Biomechanics. 2012;3 doi: 10.1177/1758736012462025. 1758736012462025. doi:10.1177/1758736012462025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eraslan O, Inan O, Secilmis A. The effect of framework design on stress distribution in implant-supported FPDs: A 3-D FEM study. Eur J Dent. 2010;4:374–82. [PMC free article] [PubMed] [Google Scholar]
- 37.Becker CM, Kaiser DA. Implant-retained cantilever fixed prosthesis: Where and when. J Prosthet Dent. 2000;84:432–5. doi: 10.1067/mpr.2000.110259. [DOI] [PubMed] [Google Scholar]
- 38.Papaspyridakos P, Kim YJ, Finkelman M, El-Rafie K, Weber HP. Digital evaluation of three splinting materials used to fabricate verification jigs for full-arch implant prostheses: A comparative study. J Esthet Restor Dent. 2017;29:102–9. doi: 10.1111/jerd.12274. [DOI] [PubMed] [Google Scholar]
- 39.Maroulakos G, Nagy WW, Ahmed A, Artopoulou II. Prosthetic rehabilitation following lateral resection of the mandible with a long cantilever implant-supported fixed prosthesis: A 3-year clinical report. J Prosthet Dent. 2017:pii:S0022-3913(17)30084-7. doi: 10.1016/j.prosdent.2017.01.019. [DOI] [PubMed] [Google Scholar]


