A part of the rapid rise in U.S. health care costs is attributable to the enlarging group of adult congenital heart disease (ACHD) patients (1–3). We examined predictors of annual inpatient cost among patients with ACHD, to better understand which clinical variables have the greatest influence on inpatient spending.
We analyzed data from the State Inpatient Databases (SID) from Arkansas (2008–2010), California (2003–2012), Florida (2005–2012), Hawaii (2006–2010), Nebraska (2003–2011), and New York (2005–2012) in the Healthcare Cost and Utilization Project (HCUP) (4). These SIDs were selected because they uniquely track hospitalizations in individual patients longitudinally. The primary outcome was financial burden accrued over a 12-month period for care of individual ACHD patients. We identified patients by selecting patients with an age of >18 having a 3-digit ICD-9 code of 745, 746, or 747. To this group of patients we applied a validated hierarchical algorithm described by Broberg et al., excluding any patients who failed to be classified according to this algorithm (5). We then excluded patients with an index hospitalization within the first or last 12 months of the investigated period, patients for whom there was no cost data available and trimmed the top and bottom 1% of patients based on total annual cost as likely outliers.
We next compared clinical characteristics and demographics between patients above versus below the overall median cost and used these analyses in combination with published data and clinical experience to identify a group of variables for further analysis.
We then built a hierarchical multivariable mixed model using this set of independent variables with total cost as the dependent variable. Since our patients were grouped by hospital, we treated hospital as a random effect in the model. The beta cost estimates, 95% confidence intervals, and p-values are reported from this model and all significance tests are two-sided with type I error set to 5%, i.e. α = 0.05. All analyses were conducted in SAS v9.4 (SAS Institute Inc., Cary, North Carolina).
We identified 155,297 index admissions, and 619,720 readmissions. After excluding readmissions which fell outside the 365 day time window after an index admission, this left 112,113 readmissions linked to index admissions. After excluding patients who failed to be categorized according to the algorithm described by Broberg et al. (n = 45,847), patients with index hospitalizations within the first or last twelve months (n = 25,703), patients for whom there was no cost data available for any given hospitalization (n = 14,038) and trimming (n = 1,395), this yielded a final sample size of 68,314.
The average age of ACHD patients analyzed was 57 ± 18.6 and 51% were women. Seventy percent of patients were white, and the most common payers at the time of hospitalization were Medicare (42%) and private insurance (38%). Forty percent of patients underwent an operative procedure during the study period.
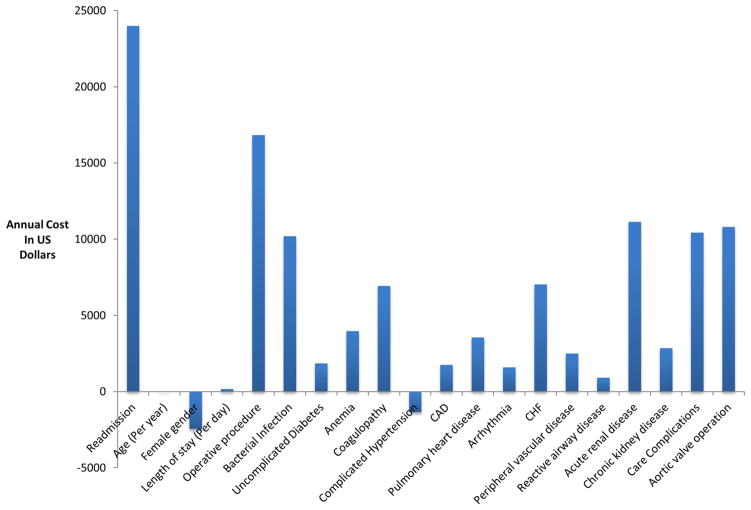
Readmitted patients had greater annual costs than non-readmitted patients by $23,993 (95% CI: $23,400–$24,586, p <0.001). Cost was $16,822 greater for patients having operative procedures (95% CI: $16,151–17,493, p <0.001), with aortic valve operations in particular responsible for $10,795 increased cost (95% CI: $9,728–11,861; p <0.001). The estimated increase or decrease in cost for all variables included in the model are depicted in Figure 1.
Figure 1. Increase in annual inpatient cost for ACHD patients with the indicated variables.
Bar graph depicting the additional annual cost in U.S. dollars of having each of the investigated variables.
We investigated the relative contribution of clinical factors to annual inpatient care cost among patients with ACHD. We found that readmission was responsible for the largest portion of cost variability, followed closely by operative procedures. This fact suggests that, unlike the demographic factors driving increases in ACHD spending, some portion of overall expenditure may be preventable and a target for improved efficiency.
There are multiple limitations to the present study related to the use of administrative data which has unverifiable completeness and accuracy. In addition, tracking of individual patients does not cross state lines and the present analysis does not account for death, thus the reported individual patient costs reported may be an underestimate. Finally, in spite of the known influence of geography on outcomes, we did not include state of hospitalization as a variable due to incomplete state representation. Limited state representation may have biased our overall results.
Acknowledgments
Funding: Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Opotowsky AR, Siddiqi OK, Webb GD. Trends in hospitalizations for adults with congenital heart disease in the U. S J Am Coll Cardiol. 2009;54:460–467. doi: 10.1016/j.jacc.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 2.Rothberg MB, Cohen J, Lindenauer P, et al. Little Evidence Of Correlation Between Growth In Health Care Spending And Reduced Mortality. Health Aff. 2010;29:1523–1531. doi: 10.1377/hlthaff.2009.0287. [DOI] [PubMed] [Google Scholar]
- 3.Auerbach DI, Kellermann AL. A decade of health care cost growth has wiped out real income gains for an average US family. Health Aff (Millwood) 2011;30:1630–6. doi: 10.1377/hlthaff.2011.0585. [DOI] [PubMed] [Google Scholar]
- 4.Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 5:143–51. [PubMed] [Google Scholar]
- 5.Broberg C, McLarry J, Mitchell J, et al. Accuracy of administrative data for detection and categorization of adult congenital heart disease patients from an electronic medical record. Pediatr Cardiol. 2015;36:719–25. doi: 10.1007/s00246-014-1068-2. [DOI] [PubMed] [Google Scholar]