Abstract
Objectives
It is unknown whether increased endovascular treatment of chronic mesenteric ischemia has led to decreases in open surgery, acute mesenteric ischemia, or overall mortality. The present study evaluates the trends in endovascular and open treatment over time for chronic and acute mesenteric ischemia.
Methods
We identified patients with chronic or acute mesenteric ischemia in the Nationwide Inpatient Sample and CDC database from 2000–2012. Trends in revascularization, mortality, and total deaths were evaluated over time. Data were adjusted to account for population growth.
Results
There were 14,810 revascularizations for chronic mesenteric ischemia (10,453 endovascular, 4,358 open), and 11,294 revascularizations for acute mesenteric ischemia (4,983 endovascular, 6,311 open). Endovascular treatment increased for both chronic (0.6 to 4.5/Million, P < 0.01) and acute mesenteric ischemia (0.6 to 1.8/Million, P < 0.01). However, concurrent declines in open surgery did not occur (chronic: 1 to 1.1/Million, acute: 1.8 to 1.7/Million). Among patients with acute mesenteric ischemia, the proportion with atrial fibrillation (18%) and frequency of embolectomy (1/Million per year) remained stable. In-hospital mortality rates decreased for both endovascular (chronic: 8% to 3%, P < 0.01; acute: 28% to 17%, P < 0.01) and open treatment (chronic: 21% to 9%, P < 0.01; acute: 40% to 25%, P < 0.01). Annual population-based mortality remained stable for chronic mesenteric ischemia (0.7 to 0.6 deaths per Million/year), but decreased for acute mesenteric ischemia (12.9 to 5.3 deaths per Million/year, P < 0.01).
Conclusions
Population mortality from acute mesenteric ischemia declined from 2000–2012, correlated with dramatic increases in endovascular intervention for chronic mesenteric ischemia, and in spite of a stable rate of embolization. However, open surgery for both chronic and acute ischemia remained stable.
Keywords: Mesenteric Ischemia, Mesenteric Artery, Embolism, Revascularization, Mortality
Introduction
Over the last decade, mesenteric angioplasty and stenting has replaced open surgical repair as first-line treatment in patients with chronic mesenteric ischemia and favorable anatomy owing to its association with lower early postoperative morbidity and mortality compared to open repair. However, it is well known that endovascular treatment leads to higher rates of restenosis, symptom recurrence, and reintervention. Moreover, each reintervention carries with it its own additional risk of morbidity and mortality, and the potential impact of this cumulative risk is unknown.1–5 Acute mesenteric ischemia is also increasingly being managed by endovascular means, although the role of mesenteric angioplasty and stenting in acute mesenteric ischemia remains to be defined.6, 7
Prior reports demonstrated an increased use of endovascular revascularization for both chronic and acute mesenteric ischemia, yet an expected decline in open surgery has not been documented.4 In addition to the increased use of endovascular techniques, medical management of disease entities associated with mesenteric ischemia including atrial fibrillation and atherosclerotic disease has changed in the last 15 years with dramatic increases in the use of warfarin, statins, and antiplatelet medications, as well as pharmacologic and ablative techniques to maintain sinus rhythm.8–11 While these improvements have been associated with prevention of stroke and cardiac events, it is not clear if the increase in medical management is associated with a decline in acute mesenteric ischemia or patient mortality following revascularization.9, 12–16
Given these gaps in knowledge, this study aims to evaluate recent trends in the treatment of mesenteric ischemia and utilization of endovascular and open surgery. Furthermore, this study aims to assess whether trends in treatment are correlated with changes in in-hospital mortality, total deaths from mesenteric ischemia, and the frequency of embolectomy and atrial fibrillation among patients with mesenteric ischemia.
Methods
The Nationwide Inpatient Sample (NIS) was utilized to examine trends in admissions and treatment of acute and chronic mesenteric ischemia between 2000 and 2012. The NIS is one of several publicly available health care databases offered by the Healthcare Cost and Utilization Project. Representing the largest all-payer inpatient care database in the United States, the NIS approximates a 20 percent stratified sample and captures close to 8 million hospital discharges each year. Trend weighting is used produce national and regional estimates. Further detailed information may be found at http://www.hcup-us.ahrq.gov.
We identified all patients with International Classification of Diseases, 9th Revision (ICD-9) classified primary diagnosis codes for acute (557.0) or chronic (557.1) mesenteric ischemia, and those with ICD-9 code 557.9 (unspecified vascular insufficiency of the intestine) were excluded. Mesenteric revascularizations were categorized as endovascular interventions including mesenteric angioplasty (39.50) and stent placement (39.90), or open surgical interventions, including mesenteric bypass (39.26, 38.36, 38.46), mesenteric embolectomy (38.06), or mesenteric endarterectomy (38.16). Thrombolysis (99.10) was classified as an endovascular intervention if it was performed alone. Any thrombolysis performed concurrently with an open surgical intervention was classified as open surgery. Arrhythmia including atrial fibrillation and flutter was also identified from ICD-9 coding (427.3, 427.31, 427.32). Patients undergoing aortic reconstruction and individuals younger than 18 years of age were excluded from analysis. Because bowel ischemia may occur at presentation in patients with acute mesenteric ischemia, it was evaluated as a baseline characteristic for patients with acute mesenteric ischemia, and was adjusted for in multivariable analysis. Among patients with chronic mesenteric ischemia, bowel ischemia was considered an adverse outcome and therefore not listed in table 1.
Table 1.
Admissions for Mesenteric Ischemia 2000–2012
| Total | % | Acute Mesenteric Ischemia | % | Chronic Mesenteric Ischemia | % | |
|---|---|---|---|---|---|---|
| All Patients | 364,034 | 100 | 293236 | 100 | 70797 | 100 |
| No Intervention | 336,619 | 92 | 280719 | 96 | 55900 | 79 |
| Any Intervention | 27,415 | 7.5 | 12517 | 4.3 | 14897 | 21 |
| Endovascular | 16,746 | 4.6 | 6206 | 2.1 | 10540 | 15 |
| Open | 10,668 | 2.9 | 6311 | 2.2 | 4358 | 6.2 |
| Bypass | 6,631 | 1.8 | 2574 | 0.9 | 4057 | 5.7 |
| Embolectomy | 3,380 | 0.9 | 3270 | 1.1 | 110 | 0.2 |
| Endarterectomy | 657 | 0.2 | 466 | 0.2 | 191 | 0.3 |
Trends in total population mesenteric ischemia related deaths were obtained from the Center for Disease Control (CDC) WONDER Underlying Cause of Death database. This database contains mortality data derived from death certificates of U.S. residents in all 50 states and Washington D.C. The underlying cause of death is recorded on each death certificate using the International Classification of Diseases, 10th Revision (ICD-10) classification (K55.0: acute mesenteric ischemia and K55.1: chronic mesenteric ischemia). These CDC data were used to identify trends in mortality among all patients who died of mesenteric ischemia over the age of 18 and compare overall population mortality to the operative mortality identified in the NIS. More information may be found at: http://wonder.cdc.gov. The Institution Review Board of Beth Israel Deaconess Medical Center approved this study and waived consent due to the de-identified nature of the NIS database.
Statistical Analysis
Results were indexed to the population and expressed per million using data provided by the U.S. Census Bureau.17 Comparisons between subgroups were made using the χ2 test for categorical data and the Student’s t-test or Wilcoxon rank sum test for continuous data. Statistical significance was defined as P < 0.05. Univariate and multivariable logistic regression analysis were performed to identify predictors of in-hospital mortality. Purposeful selection was used to select variables for inclusion into each model.18 This included all variables with P < 0.1 on univariate screen as well as those variables shown to be predictive of each evaluated endpoint in previous studies. Each logistic regression model was evaluated for goodness of fit using Hosmer-Lemeshow testing. Statistical analyses were performed using SPSS (version 22.0) and graphical analysis was completed using GraphPad (version 6.0)
RESULTS
Between 2000 and 2012, 27,415 revascularization procedures were performed for mesenteric ischemia (12,517 for acute mesenteric ischemia, 14,897 for chronic mesenteric ischemia). Among patients with chronic mesenteric ischemia, 4,358 (29%) underwent open surgery and 10,540 (71%) underwent endovascular intervention. Among patients with acute mesenteric ischemia 6,311 (50%) patients underwent open surgery and 6,206 (50%) underwent endovascular intervention (Table 1).
Demographics
The baseline demographics and comorbidities of patients undergoing revascularization for chronic mesenteric ischemia and acute mesenteric ischemia are listed in Table 2. The majority of patients undergoing interventions for both chronic (Open: 78%, Endovascular: 72%) and acute mesenteric ischemia (Open: 64%, Endovascular: 66%) were female. More patients with chronic mesenteric ischemia underwent endovascular treatment compared to open (Endovascular: 10,540, Open: 4,358), and those undergoing endovascular treatment were older (74 years vs. 68 years, P < 0.01), less likely to be female (72% vs. 78%, P < 0.01), and had a higher incidence of comorbidities including: hypertension (68% vs. 55%, P < 0.01), peripheral arterial disease (43% vs. 35%, P < 0.01), coronary artery disease (46% vs. 30%, P < 0.01), myocardial infarction (9% vs. 7%, P < 0.01), congestive heart failure (18% vs. 14%, P < 0.01), diabetes (28% vs. 17%, P < 0.01), chronic obstructive pulmonary disease (29% vs. 26%, P < 0.01), chronic kidney disease (16% vs. 6%, P < 0.01). Atrial fibrillation and stroke rates did not differ between patients undergoing endovascular and open intervention for chronic mesenteric ischemia. Alternatively, slightly more patients with acute mesenteric ischemia underwent open repair compared to endovascular intervention (Endovascular: 6,206, Open: 6,311) and gender was not significantly different between the two treatment groups. Older age (72 vs. 71 years, P < 0.01) and comorbid conditions remained more common among patients undergoing endovascular treatment. The notable exception of atrial fibrillation (39% vs. 22%, P < 0.01) and a history of stroke (5% vs. 4%, P < 0.01) were more prevalent in those undergoing open repair for acute mesenteric ischemia, which reflects that acute mesenteric ischemia due to embolism was more likely to be treated with open surgery.
Table 2.
Demographic and Comorbidity Data
| Chronic Mesenteric Ischemia | Acute Mesenteric Ischemia | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Endo N=10540 |
Open N=4358 |
P-value | Endo N=6206 |
Open N=6310 |
P-value | |
| Age — median (IQR) | 74 (65–80) | 68 (59–76) | <0.001 | 72 (62–79) | 71 (60–79) | <0.001 |
| Gender (% Female) | 72 | 78 | <0.001 | 66 | 64 | 0.17 |
| Comorbidities (%) | ||||||
| Hypertension | 68 | 55 | <0.001 | 55 | 49 | <0.001 |
| PAD | 43 | 35 | <0.001 | 42 | 23 | <0.001 |
| CAD | 46 | 30 | <0.001 | 36 | 23 | <0.001 |
| Atrial Fibrillation | 15 | 15 | 0.59 | 22 | 39 | <0.001 |
| Myocardial Infarction | 9.3 | 7.1 | <0.001 | 7.3 | 5.1 | <0.001 |
| Congestive Heart Failure | 18 | 14 | <0.001 | 21 | 23 | 0.008 |
| Diabetes | 28 | 17 | <0.001 | 24 | 19 | <0.001 |
| COPD | 29 | 26 | <0.001 | 27 | 22 | <0.001 |
| Chronic Kidney Disease | 15.6 | 6.1 | <0.001 | 10 | 7.8 | <0.001 |
| Stroke | 6.9 | 7.8 | 0.06 | 4.3 | 5.1 | <0.001 |
| Bowel Resection* | – | – | – | 26 | 47 | <0.001 |
CAD: Coronary Artery Disease; COPD: chronic obstructive pulmonary disease; IQR: Interquartile Range; PAD: peripheral arterial disease
Due to the presence of bowel ischemia on presentation it was considered a comorbid condition for patients with acute mesenteric ischemia only
Trends in Treatment
Over time, the total number of revascularizations among patients with chronic mesenteric ischemia has increased (1.8 to 5.6 per million, P < 0.01) (Figure 1). However, the volume of open revascularizations remained stable (1 to 1.1 per million), thus the rise in chronic mesenteric ischemia interventions was driven by endovascular treatment (0.8 to 4.6 per million, P < 0.01), which surpassed open surgery as the dominant method of revascularization in 2002.
Figure 1. Trends in the Number of Procedures Performed for Mesenteric Ischemia.
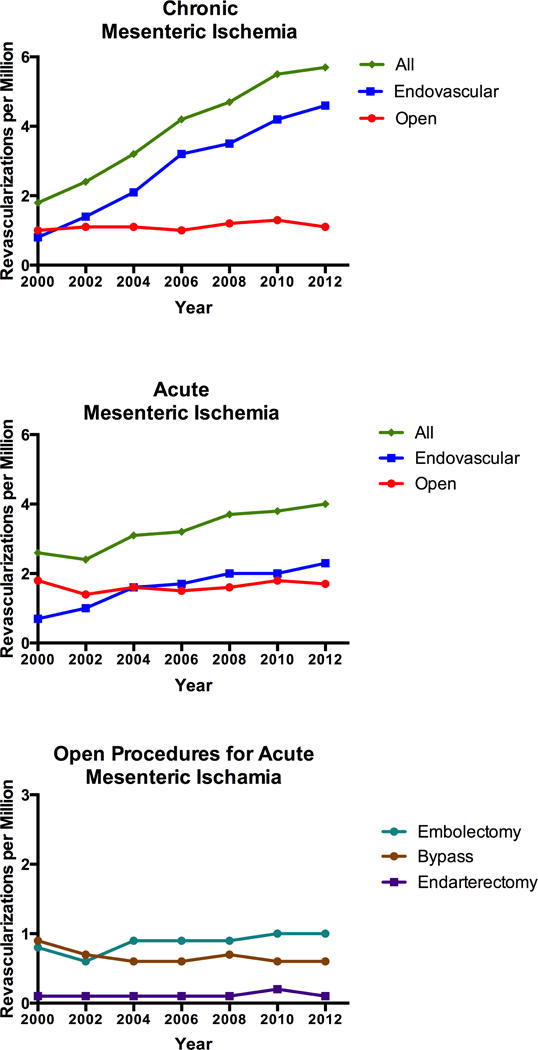
The total number of revascularizations for mesenteric ischemia from 2000–2012 correlated with increased used of endovascular interventions; while open surgery has remained stable.
Similar to chronic mesenteric ischemia, the number of patients undergoing revascularization for acute mesenteric ischemia increased over time (2.6 to 4.0 per million, P < 0.01), driven by an increase in endovascular intervention (0.7 to 2.3 per million, P < 0.01), while the number of open procedures remained stable (1.8 to 1.7 per million).
Given the increased use of anticoagulation for atrial fibrillation,9, 12, 19, 20 we next evaluated the trends in type of open procedures completed and frequency of atrial fibrillation among patients with acute mesenteric ischemia. Embolectomy (0.8 to 1.0 per million), bypass (0.9 to 0.6 per million), and endarterectomy (0.1 to 0.1 per million) all remained relatively stable between 2000 and 2012. Additionally, despite improved medical therapy, the frequency of atrial fibrillation among patients with acute mesenteric ischemia was 18% and remained stable over time (18.1% to 17.9%).
Trends in Population Mortality
The total number of deaths among all patients with chronic mesenteric ischemia in the United States remained stable between 2000 and 2012 as reported by CDC Wonder database (0.7 to 0.6 per million). Total population mortality among patients with acute mesenteric ischemia declined from 12.9 to 5.3 deaths per million over the same time period (P < 0.01) (Table 3).
Table 3.
Total Deaths from Mesenteric Ischemia 2000–2012 (CDC Wonder)
| Chronic | Acute | |||
|---|---|---|---|---|
|
|
||||
| Year | Deaths per Million | Percent of Total Deaths (%) | Deaths per Million | Percent of Total Deaths (%) |
| 2000 | 0.7 | 7.8 | 12.9 | 10.6 |
| 2001 | 0.7 | 8.3 | 11.8 | 9.8 |
| 2002 | 0.7 | 8.1 | 10.9 | 9.1 |
| 2003 | 0.6 | 6.9 | 10.5 | 8.9 |
| 2004 | 0.6 | 6.4 | 9.6 | 8.2 |
| 2005 | 0.5 | 5.9 | 8.5 | 7.3 |
| 2006 | 0.5 | 6.2 | 7.9 | 6.8 |
| 2007 | 0.4 | 5.2 | 7.5 | 6.6 |
| 2008 | 0.5 | 5.6 | 7.1 | 6.3 |
| 2009 | 0.6 | 7.8 | 6.5 | 5.8 |
| 2010 | 0.7 | 8.6 | 6.1 | 5.5 |
| 2011 | 0.7 | 8.2 | 6.0 | 5.5 |
| 2012 | 0.6 | 7.2 | 5.3 | 4.9 |
Trends in In-Hospital Mortality
Over the entire study period, in-hospital mortality among patients treated for chronic mesenteric ischemia was higher following open surgery than endovascular intervention (13% vs. 4%, P < 0.01). Similar results were found following intervention for acute mesenteric ischemia (37% vs. 16%, P < 0.01). However, patients undergoing open surgery for acute mesenteric ischemia were more likely to undergo a bowel resection (47% vs. 26%, P < 0.01) likely reflecting presentation at a more advanced stage of disease. When differences in patient demographics and comorbid conditions were accounted for, open surgery remained independently predictive of mortality for both chronic mesenteric ischemia (Odds ratio (OR): 3.6, 95% Confidence Interval (CI) 3.2–4.2, P < 0.01) and acute mesenteric ischemia. (OR: 2.7, 95% CI: 2.5–3.0, P < 0.01).
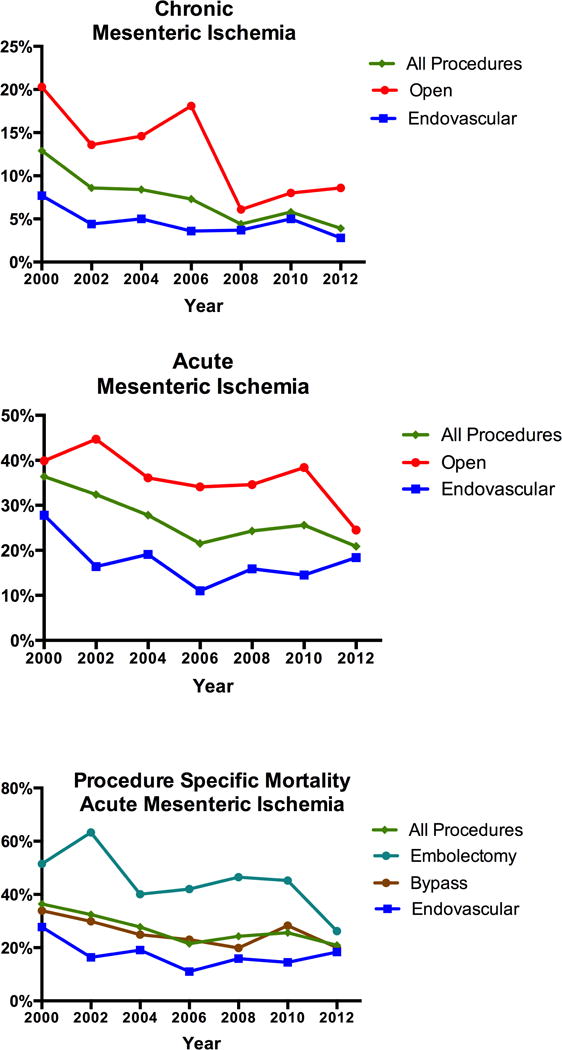
Overall, in-hospital mortality rates declined from 13% to 4% among patients undergoing revascularization for chronic mesenteric ischemia (P < 0.01) (Figure 2). The declines were greatest among patients undergoing open treatment, with rates declining from 20% in 2000 to 9% in 2012 (P < 0.01). The mortality rate associated with endovascular treatment also decreased from 8% to 3% over the same time period (P < 0.01). The total number of deaths following revascularization remained stable with a decline among patients undergoing open procedures from 0.2 to 0.1 deaths per million and an increase from 0.02 to 0.1 deaths per million (P < 0.01) among patients treated with endovascular intervention, reflecting changing practice patterns (Figure 3).
Figure 2. Trends in In-Hospital Mortality Rates following Revascularization.
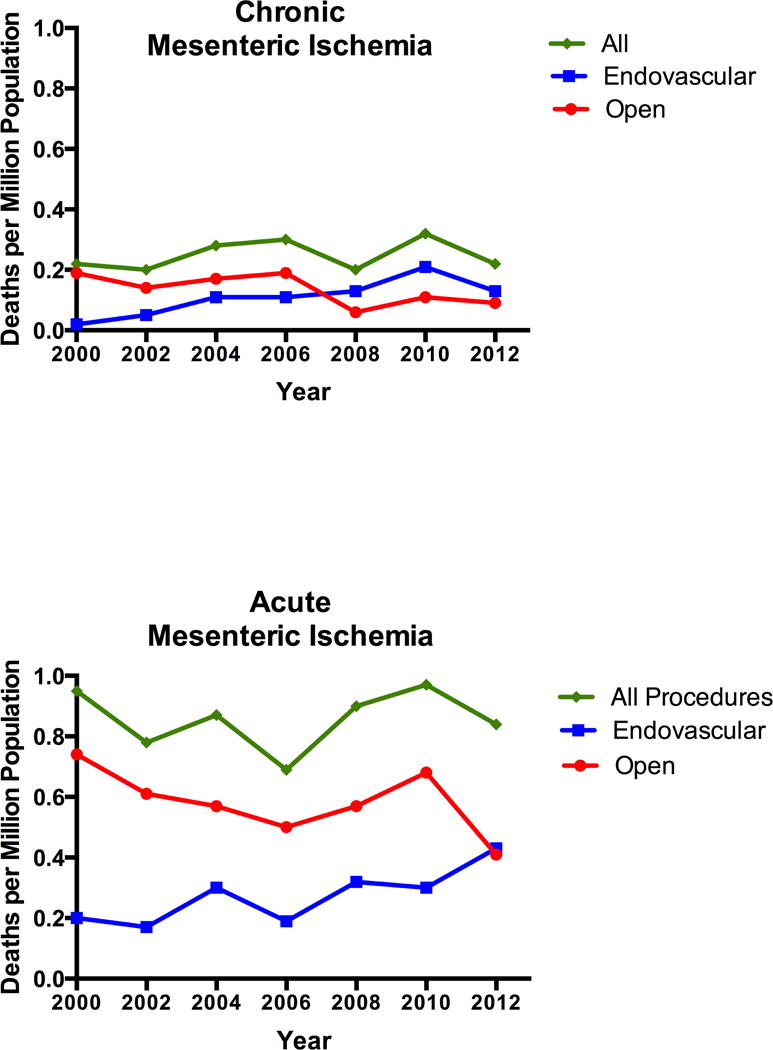
Mortality rates following both open and endovascular revascularization for mesenteric ischemia declined from 2000–2012.
Figure 3. Total Number of Deaths following Revascularization.
The total number of deaths following revascularization did not decline from 2000–2012.
In-hospital mortality also declined dramatically among patients undergoing revascularization for acute mesenteric ischemia (37% to 21%, P < 0.01) (Figure 2). Following endovascular intervention mortality rates declined from 28% in 2000 to 18% in 2012 (P < .01). Mortality rates following open surgery also declined from 40% to 25% over the same time period (P < 0.01). Among patients with open treatment, the decline in mortality rate was driven by embolectomy, the most common open procedure for acute mesenteric ischemia, which had a dramatic decline in mortality from 52% to 26% over the study period (P < 0.01). The total number of deaths following open revascularization decreased from 0.7 to 0.4 deaths per million (P < 0.01) while total deaths after endovascular treatment remained increased (0.2 to 0.4 deaths per million, P < 0.01) likely due to the noted increase in the number of patients treated with endovascular intervention over time (Figure 3).
Discussion
Our study found that between 2000 and 2012 revascularization for both chronic and acute mesenteric ischemia increased due to significant growth in endovascular intervention. Additionally, in-hospital mortality rates following revascularization for both chronic and acute mesenteric ischemia declined for open and endovascular intervention. The total deaths following revascularization for chronic mesenteric ischemia remained stable and total deaths following revascularization for acute mesenteric ischemia declined despite stable rates of embolectomy.
There are multiple factors which likely contributed to the decreased in–hospital mortality associated with revascularization for both acute and chronic mesenteric ischemia including: improved disease recognition, earlier disease recognition, more frequent treatment, risk factor reduction including a national decline in the prevalence of smoking, and improved medical management through the increased use of statins, antiplatelet agents, and anticoagulation.21 These findings parallel secular trends in declining mortality from atherosclerotic heart disease and stroke.22 Additionally, improvements in critical care and changes in operative practice likely played a major role in improved patient outcomes. Our study highlights the increased use of endovascular treatment, which has been associated with decreased mortality compared to open surgery both here and in previous studies.1, 4, 5, 23 However, the increase in endovascular treatment alone cannot explain the dramatic mortality declines. Among patients with chronic mesenteric ischemia, the overall increase in number of patients being treated, may suggest an increased use of abdominal imaging, broadening of inclusion criteria for revascularization to treat patients with an equivocal diagnosis of chronic mesenteric ischemia, but in whom endovascular intervention is considered low risk, subsequently lowering the overall risk of mortality for all patients. Additionally, high-risk patients with malnutrition are likely being treated with endovascular intervention and may undergo open surgery only after improvement in their nutritional status leading to a decrease in the mortality rate in the open cohort as well.
While our study identified improved mortality rates following revascularization for both acute and chronic mesenteric ischemia, our data and CDC Wonder revealed that the total number of deaths from chronic mesenteric ischemia have remained stable while acute mesenteric ischemia deaths have declined. Of note, the CDC Wonder database can only be used to assess the total number of deaths in the population (i.e. deaths/population size), whereas the NIS can be used to determine rates of death (deaths/interventions). The total number of deaths in both databases were stable for chronic mesenteric ischemia and lower for acute mesenteric ischemia, but only the NIS can be used to measure the rates of death per interventions. Given the dramatic increase in intervention for chronic mesenteric ischemia and low likelihood of dying from this condition, a stable number of people are dying as a result of intervention despite a lower mortality rate. Among patients with acute mesenteric ischemia, the decline in total number of deaths is in part the result of declining mortality rates with revascularization. It can be further hypothesized that the increase in endovascular revascularization for chronic mesenteric ischemia may also be contributing to the decline deaths from acute mesenteric ischemia by preventing the progression among patients with chronic disease. Additionally, the rise in endovascular treatment of acute mesenteric ischemia may be in part related to treatment of those with acute on chronic ischemia due to restenosis after prior endovascular intervention for chronic ischemia. However, these hypotheses cannot be proven by this study.
In addition to improved mortality rates following intervention, this study found an increase in revascularizations for both chronic and acute mesenteric ischemia. Operatively, treatment of mesenteric ischemia was revolutionized by the introduction of endovascular techniques. For patients with chronic mesenteric ischemia, endovascular treatment surpassed open surgery as the dominant technique for revascularization in 2002 due to the lower morbidity and mortality associated with the approach, and today, endovascular intervention is considered the preferred first-line approach for most patients with chronic mesenteric ischemic, regardless of the patient’s operative risk.24 An aging population and the decrease in morbidity and mortality associated with endovascular procedures has also led to broader inclusion of patients who previously may have been considered unfit for open surgical repair and is a potential factor driving the growth in revascularization found in our study.4 High rates of restenosis and reintervention associated with the endovascular approach have also likely contributed to the increased number of revascularizations.1, 3, 25
Although endovascular treatment has been increasingly employed, embolectomy has not decreased for the treatment of acute mesenteric ischemia, and there are only a few moderate sized retrospective reports comparing the utility of open and endovascular intervention among patients with acute mesenteric ischemia. Arthurs et al. reported their experience treating acute mesenteric ischemia in 70 consecutive patients from 1998 to 2008 and found despite initial technical success rate of 87%, only 30% of patients were able to avoid laparotomy, and 13% of endovascular patients required subsequent open revascularization despite shorter segments of ischemic bowel and longer symptom duration in the endovascular group suggesting a lesser disease burden among endovascular patients.6 Even at centers of excellence in endovascular treatment, 88% of patients between 1999 and 2010 underwent open revascularization, without dramatic changes in open treatment over time.7 These studies in conjunction with the results from our study suggest that the need to evaluate intestinal viability and perform embolectomy may explain why the open approach is still often preferred.
In addition to the importance of changing operative technique, the medical management of atrial fibrillation and atherosclerotic disease has changed dramatically over the last decade. Data from multiple national studies have demonstrated a considerable increase in the prevalence of statin, antiplatelet, and anticoagulation use over time.8, 9, 11, 12, 19, 20 Interestingly, Kirley et al. found that anticoagulation and antiplatelet use has plateaued in more recent years.26 Additionally, several studies have found significant increases in the utilization of ablation, cardioversion, and amiodarone in an effort to maintain sinus rhythm.10, 20 These combined efforts have been utilized in an attempt to decrease the prevalence of atrial fibrillation and to reduce the risk of adverse cardiovascular and thromboembolic events (particularly embolic events in patients with atrial fibrillation).27–30 Unfortunately, our study found that among patients with acute mesenteric ischemia, the proportion of patients with atrial fibrillation and the proportion of surgical patients undergoing embolectomy have remained nearly the same between 2000 and 2012, suggesting that increased medical management efforts aimed at preventing thromboembolic events have not resulted in a decreased risk of acute embolic mesenteric ischemia. These findings are similar to those found by Ryer et al., which found that the frequency of embolectomy did not decline, but rather increased in their study period of 1990–1999 and 2000–2010 at the Mayo Clinic.7
This study found changes in the trends of operative treatment of mesenteric ischemia over time. However, additional answers are needed to further improve morbidity and mortality associated with mesenteric ischemia and to identify the optimal treatment modalities for specific patient populations. First, it should be noted that this study was unable to evaluate the long-term outcomes of patients with mesenteric ischemia or the frequency of reintervention due to limitations of the NIS database. Given the dramatic increase in endovascular intervention and the high likelihood of reintervention, these data are pertinent to understanding the long-term impacts of this change in paradigm. Moreover, despite clear improvements in morbidity and mortality for patients undergoing endovascular treatment, the rate of open revascularization remains stable for both chronic and acute mesenteric ischemia. This leads to important questions regarding who continues to perform open operations and for what type of patient. More clinical detail is needed to appropriately stratify populations in order to identify those that may benefit most from one intervention over another. Finally, given the significant cost associated with medical management of atrial fibrillation and decreased incidence in stroke associated with the treatment of this condition, it is unclear why the rates of embolectomy and atrial fibrillation among patients persist without improvement in patients with acute mesenteric ischemia.9 While these questions are unable to be discerned from the current study, the results of our analysis provide important data to guide future research.
This study has several further limitations that must be acknowledged. This study is limited by the nature of the databases. In addition to potential problems with coding, there is no ability to track patients within the NIS longitudinally, making it difficult to identify reintervention and conversion from chronic to acute mesenteric ischemia. This is particularly important for analyzing the long-term outcomes of patients undergoing endovascular treatment for chronic mesenteric ischemia, for whom the perioperative mortality following each endovascular procedure may be lower relative to open repair, but for whom cumulative mortality after repeated reinterventions is unknown, and risk for conversion to acute mesenteric ischemia remains unclear. Additionally, the NIS tracks inpatients only, and any patient treated in ambulatory surgery centers cannot be accounted for. Finally, no detailed procedural or anatomic information is available, which may influence the decision of operative approach, and it is likely that open surgery was reserved for patients with a greater burden of disease which could not be accounted for.
Conclusion
The mortality rates following revascularization and total deaths from acute mesenteric ischemia have declined in the last 12 years in correlation with dramatic increases in the endovascular treatment of chronic mesenteric ischemia. However, despite increased intervention and improvements in medical management, the frequency of embolectomy for acute mesenteric ischemia remains unchanged. Surprisingly, the rate of open surgery for both chronic and acute mesenteric ischemia remains stable. Further research is warranted to better understand the long-term impact of changing revascularization practice patterns and identify how to best prevent acute mesenteric ischemia in patients with arrhythmia.
Acknowledgments
Funding Sources: National Institutes of Health Harvard-Longwood T32 Research Training in Vascular Surgery Grant HL-007734 to Sara L. Zettervall, Ruby C. Lo, Peter A. Soden, and Sarah E. Deery.
Abbreviation List
- NIS
Nationwide Inpatient Sample
- ICD-9
International Classification of Diseases, 9th Revision
- CDC
Center for Disease Control and Prevention
- ICD-10
International Classification of Diseases, 10th Revision
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Marc L. Schermerhorn is a consultant for Endologix and Medtronic. Duane S. Pinto is a consultant for Medtronic. All other authors have nothing to disclose.
References
- 1.Oderich GS, Bower TC, Sullivan TM, Bjarnason H, Cha S, Gloviczki P. Open versus endovascular revascularization for chronic mesenteric ischemia: risk-stratified outcomes. J Vasc Surg. 2009;49(6):1472–9 e3. doi: 10.1016/j.jvs.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Atkins MD, Kwolek CJ, LaMuraglia GM, Brewster DC, Chung TK, Cambria RP. Surgical revascularization versus endovascular therapy for chronic mesenteric ischemia: a comparative experience. J Vasc Surg. 2007;45(6):1162–71. doi: 10.1016/j.jvs.2007.01.067. [DOI] [PubMed] [Google Scholar]
- 3.Davies RS, Wall ML, Silverman SH, Simms MH, Vohra RK, Bradbury AW, et al. Surgical versus endovascular reconstruction for chronic mesenteric ischemia: a contemporary UK series. Vascular and endovascular surgery. 2009;43(2):157–64. doi: 10.1177/1538574408328665. [DOI] [PubMed] [Google Scholar]
- 4.Schermerhorn ML, Giles KA, Hamdan AD, Wyers MC, Pomposelli FB. Mesenteric revascularization: management and outcomes in the United States, 1988–2006. J Vasc Surg. 2009;50(2):341–8 e1. doi: 10.1016/j.jvs.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aburahma AF, Campbell JE, Stone PA, Hass SM, Mousa AY, Srivastava M, et al. Perioperative and late clinical outcomes of 105 percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. J Vasc Surg. 2013;54(4):1052–61. doi: 10.1016/j.jvs.2012.10.082. [DOI] [PubMed] [Google Scholar]
- 6.Arthurs ZM, Titus J, Bannazadeh M, Eagleton MJ, Srivastava S, Sarac TP, et al. A comparison of endovascular revascularization with traditional therapy for the treatment of acute mesenteric ischemia. J Vasc Surg. 2011;53(3):698–704. doi: 10.1016/j.jvs.2010.09.049. discussion-5. [DOI] [PubMed] [Google Scholar]
- 7.Ryer EJ, Kalra M, Oderich GS, Duncan AA, Gloviczki P, Cha S, et al. Revascularization for acute mesenteric ischemia. J Vasc Surg. 2012;55(6):1682–9. doi: 10.1016/j.jvs.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 8.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. The Annals of pharmacotherapy. 2008;42(9):1208–15. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 9.Shroff GR, Solid CA, Herzog CA. Atrial fibrillation, stroke, and anticoagulation in Medicare beneficiaries: trends by age, sex, and race, 1992–2010. Journal of the American Heart Association. 2014;3(3):e000756. doi: 10.1161/JAHA.113.000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin-Doyle W, Essebag V, Zimetbaum P, Reynolds MR. Trends in US hospitalization rates and rhythm control therapies following publication of the AFFIRM and RACE trials. Journal of cardiovascular electrophysiology. 2011;22(5):548–53. doi: 10.1111/j.1540-8167.2010.01950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Y, Boudreau DM, Freedman AN. Trends in the use of aspirin and nonsteroidal anti-inflammatory drugs in the general U.S. population. Pharmacoepidemiology and drug safety. 2014;23(1):43–50. doi: 10.1002/pds.3463. [DOI] [PubMed] [Google Scholar]
- 12.Shroff GR, Solid CA, Herzog CA. Temporal trends in ischemic stroke and anticoagulation therapy among medicare patients with atrial fibrillation: A 15-year perspective (1992–2007) JAMA Internal Medicine. 2013;173(2):159–60. doi: 10.1001/jamainternmed.2013.1579. [DOI] [PubMed] [Google Scholar]
- 13.Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Circulation. 2006;113(10):e409–49. [PubMed] [Google Scholar]
- 14.Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke; a journal of cerebral circulation. 2011;42(1):227–76. doi: 10.1161/STR.0b013e3181f7d043. [DOI] [PubMed] [Google Scholar]
- 15.Bhatt DL. Role of antiplatelet therapy across the spectrum of patients with coronary artery disease. The American journal of cardiology. 2009;103(3 Suppl):11a–9a. doi: 10.1016/j.amjcard.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 16.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. Statins for the primary prevention of cardiovascular disease. The Cochrane database of systematic reviews. 2013;1:Cd004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Population and Housing Unit Estimates. United States Census Bureau. 2013 [22 February 2016]; Available from: http://www.census.gov/popest/
- 18.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):1–8. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rowan SB, Bailey DN, Bublitz CE, Anderson RJ. Trends in anticoagulation for atrial fibrillation in the U.S.: an analysis of the national ambulatory medical care survey database. Journal of the American College of Cardiology. 2007;49(14):1561–5. doi: 10.1016/j.jacc.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 20.Fang MC, Stafford RS, Ruskin JN, Singer DE. National trends in antiarrhythmic and antithrombotic medication use in atrial fibrillation. Arch Intern Med. 2004;164(1):55–60. doi: 10.1001/archinte.164.1.55. [DOI] [PubMed] [Google Scholar]
- 21.Trends in Current Cigarette Smoking Among High School Students and Adults, United States, 1965–2011. Centers for Disease Control and Prevention; 2013. [22 February 2016] Available from: http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/ [Google Scholar]
- 22.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 23.Pecoraro F, Rancic Z, Lachat M, Mayer D, Amann-Vesti B, Pfammatter T, et al. Chronic mesenteric ischemia: critical review and guidelines for management. Annals of vascular surgery. 2013;27(1):113–22. doi: 10.1016/j.avsg.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Oderich GS, Gloviczki P, Bower TC. Open surgical treatment for chronic mesenteric ischemia in the endovascular era: when it is necessary and what is the preferred technique? Seminars in vascular surgery. 2010;23(1):36–46. doi: 10.1053/j.semvascsurg.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 25.Tallarita T, Oderich GS, Macedo TA, Gloviczki P, Misra S, Duncan AA, et al. Reinterventions for stent restenosis in patients treated for atherosclerotic mesenteric artery disease. J Vasc Surg. 2011;54(5):1422–9 e1. doi: 10.1016/j.jvs.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circulation Cardiovascular quality and outcomes. 2012;5(5):615–21. doi: 10.1161/CIRCOUTCOMES.112.967299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Savelieva I, Bajpai A, Camm AJ. Stroke in atrial fibrillation: update on pathophysiology, new antithrombotic therapies, and evolution of procedures and devices. Ann Med. 2007;39(5):371–91. doi: 10.1080/07853890701320662. [DOI] [PubMed] [Google Scholar]
- 28.Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy: recent data and ideas. Stroke; a journal of cerebral circulation. 2005;36(7):1588–93. doi: 10.1161/01.STR.0000170642.39876.f2. [DOI] [PubMed] [Google Scholar]
- 29.Eikelboom JW, Hirsh J, Spencer FA, Baglin TP, Weitz JI. Antiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e89S–119S. doi: 10.1378/chest.11-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith SC, Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113(19):2363–72. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]


