Abstract
Our review establishes the empirical evidence for patient mobility for elective secondary care services in countries that allow patients to choose their health care provider. PubMed and Embase were searched for relevant articles between 1990 and 2015. Of 5,994 titles/abstracts reviewed, 26 studies were included. The studies used three main methodological models to establish mobility. Variation in the extent of patient mobility was observed across the studies. Mobility was positively associated with lower waiting times, indicators of better service quality, and access to advanced technology. It was negatively associated with advanced age or lower socioeconomic backgrounds. From a policy perspective we demonstrate that a significant proportion of patients are prepared to travel beyond their nearest provider for elective services. As a consequence, some providers are likely to be “winners” and others “losers,” which could result in overall decreased provider capacity or inefficient utilization of existing services. Equity also remains a key concern.
Keywords: patient choice, provider competition, patient mobility, hospital bypassing
Introduction
A number of high-income countries have introduced policies that enable patients to select a health care provider of their choice with the aim of increasing service capacity, enhancing efficiency, and improving the quality of health care delivered (Dixon, Robertson, & Bal, 2010; France & Taroni, 2005; Magnussen, Vrangbæk, & Saltman, 2009). It is expected that by publicly reporting information on the quality of providers’ services, patients will select a provider that best meets their needs. From the provider perspective, it is anticipated that this “competition in the market” offers a stimulus to become more responsive and patient-centered, thus improving performance (Berwick, James, & Coye, 2003).
Given the costs associated with reconfiguring the health care system to support patient choice and to encourage competition between providers, it is essential to understand how patients have responded to the introduction of these policies. A key question is therefore whether “patient choice” policies have encouraged patients to actively choose their provider (Dusheiko, 2014).
Studies attempting to answer this question have predominantly used data derived from surveys, asking individuals about recent health care episodes or their responses to hypothetical scenarios (Dixon, Robertson, Appleby, Burge, & Devlin, 2010; Finlayson, Birkmeyer, Tosteson, & Nease, 1999; Schwartz, Woloshin, & Birkmeyer, 2005; Victoor, Delnoij, Friele, & Rademakers, 2012). Other studies have used actual patient data from hospital or primary care episodes (Haynes, Lovett, & Sunnenberg, 2003). However, the latter studies are limited as they can only ascertain where patients were being treated and not whether they made an active choice. Furthermore, it is not possible to determine to what extent these choices were influenced by primary care physicians.
Given the inherent challenges associated with establishing active choice, one can instead ask a different empirical question: namely, whether there is evidence that patients seek care at hospitals other than their nearest. This question is related to the concept of “patient mobility.”
Even accounting for individual characteristics, the extent to which patients are able to move to alternative providers will depend on a number of circumstances, including area characteristics (e.g., urban vs. rural), the health care setting (e.g., primary vs. secondary care), the urgency of the clinical condition requiring medical support (e.g., emergency vs. elective), and the severity of the intervention (e.g., cataract surgery vs. coronary artery bypass grafting). Furthermore, the configuration of the health care market varies significantly between countries, with patient opportunity to choose dependent on organizational structures, systems of financing, and the geographical organization of specialist services.
Therefore, in this systematic review we aim to establish the evidence for patient mobility for elective services in the secondary care setting in countries that have introduced policies that enable patients to choose their health care provider. We also assess the methodological approaches used to describe patient mobility and analyze to what extent patient mobility is associated with patient, provider, and area characteristics.
Method
Search Strategy
A combined search was performed in Pubmed and Embase for articles published between January 1, 1990 and June 30, 2015 (Appendix A). Search terms were defined and modified iteratively following an initial broad search of the literature and a consultation with the authors of some retrieved studies.
Inclusion Criteria
Published full text empirical studies that investigated patient mobility and its determinants using information on the patients’ residence (e.g., zip code, county) and their actual secondary care episodes were considered for inclusion.
Two distinct types of study relating to patient mobility were identified from the preliminary analysis. The first type determines whether or not patients travel beyond their nearest secondary care provider(s) to receive care. The second type assesses the relative impact that distance on one hand and provider characteristics (e.g., quality) on the other hand have on patients’ choice of provider. Both study types were considered for inclusion and we describe the different models within these types in our “Results” section.
Only studies investigating patient mobility in European, North American (Canada and the United States) and Australasian countries, (Australia and New Zealand only) were considered. Countries had to have introduced patient choice policies in which providers are expected to compete on the basis of quality, mainly through publicly reporting indicators of provider-level performance (http://www.nhs.uk/pages/home.aspx; http://www.kiesbeter.nl/; Swedish Association of Local Authorities and Regions, 2013; Vrangbæk, Robertson, Winblad, Van de Bovenkamp, & Dixon, 2012)
Study participants must have been enrolled in a voluntary, tax-based, or social health insurance scheme and received elective (or non-emergency) outpatient/inpatient services in a secondary care setting. Only studies published in English and in peer-reviewed journals were considered for inclusion.
Exclusion Criteria
A key aspect of our study is to understand the patient and provider factors that influence where patients receive care. Therefore, we excluded studies that review patterns of mobility primarily reflecting insurer preferences for particular providers (e.g., through selective contracting and use of explicit financial incentives to channel patients to preferred providers; Boonen, Donkers, & Schut, 2011; Rosenthal, Li, & Milstein, 2009). For the same reason, we also excluded studies focusing on physician referral patterns because they primarily reflect physician preferences (Ringard, 2010).
Studies reviewing cross-border mobility were excluded. Also, studies reviewing patient mobility in the acute care setting (i.e., emergency hospital visits) were excluded as decisions regarding location of secondary care are constrained by the patients’ clinical condition and the necessity for urgent treatment.
Longitudinal studies that looked at the impact of the publication of performance indicators on hospital volumes or the effect of hospital competition on treatment outcomes, were excluded as they provide no explicit information on the impact of patient and provider characteristics on mobility or assessment of where patients are expected to receive their treatment based on their residence (Cooper, Gibbons, Jones, & McGuire, 2011; Cutler, Huckman, & Landrum, 2004; Laverty et al., 2012).
Articles that were published after 1990 but which used pre-1990 patient-level data were also excluded for the following reasons. First, introduction of provider choice policies did not occur before 1990 in most European countries. Second, reconfiguration of specialist services due to centralization after 1990 has influenced the choice of available providers. Third, there has been an increase in the quantity and quality of publicly available information to inform provider choice over the same period.
Data Selection
AA and DL independently selected articles that met the inclusion criteria based on titles and abstracts. When there was uncertainty about whether an article fulfilled the inclusion criteria, it was included for full text review. In the next stage, full text articles were reviewed independently by AA and DL. Final inclusion was based on consensus. Disagreements were resolved following discussion with JvdM. Reference lists from included studies were hand-searched for additional potentially relevant articles.
Data Extraction
AA independently extracted study data and consulted DL and JvdM in case of uncertainty. Data extracted included: location of study; geographical unit of analysis (regional vs. national); secondary care context (intervention/service[s] patients received), source of data (e.g., hospital discharge records); time-frame of analysis; study sample size and exclusion criteria; model for estimating patient mobility; definition of “expected” provider; construction of hospital “choice sets”; proportion of patients travelling beyond their expected provider(s); patient and provider characteristics analyzed; statistical analysis.
For “expected” provider(s) we refer to the nearest provider(s) offering the relevant intervention given the patient’s clinical condition. For hospital “choice sets,” we refer to the selection of hospitals that offer the relevant intervention as defined by the study authors. For example, this may include all hospitals within a threshold distance or region.
Study Assessment
The studies selected are best described as cross-sectional studies. A review of published checklists and scoring scales for systematic reviews was undertaken to identify the appropriate tool to assess the selected studies (Higgins & Green, 2008; Sanderson, Tatt, & Higgins, 2007); however, no suitable tool was found. A 10-item checklist was therefore created and validated (Appendix B) with reference to previously published relevant checklists for observational studies (Loney, Chambers, Bennett, Roberts, & Stratford, 1998; Munn, Moola, Riitano, & Lisy, 2014; Vandenbroucke et al., 2007).
One of the methodological challenges faced in using patient mobility as a proxy for patient choice is to separate the impact of patient choice from that of other factors. Patient mobility has been conceptualized as conforming to three distinct categories (Ringard, Rico, & Hagen, 2005; Tessier, Contandriopoulos, & Dionne, 1985). First, mobility due to patient choice; second, mobility due to primary care or secondary care referral preferences induced by physicians; and third, mobility due to insufficient local supply. In reality there are inherent difficulties in separating mobility due to patient choice and physician preferences given that these decisions are rarely mutually exclusive.
A key component of our checklist was therefore to assess whether the authors had accounted for, and adequately measured, relevant patient and health system factors that influenced patient mobility in order to identify “true movers.” “True movers” are considered to be individuals who travel beyond their nearest provider to an alternative provider without the biasing effect of health system factors (e.g., explicit financial incentives to choose particular providers). AA and DL independently assessed the selected articles according to each item on the checklist. Disagreements were resolved following discussion with JvdM.
Results
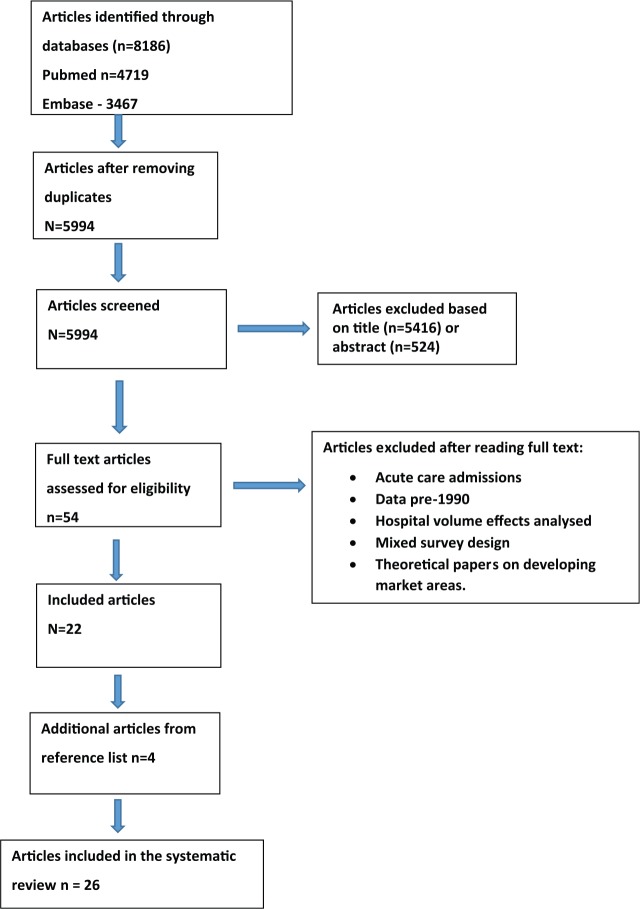
A total of 5,994 titles and abstracts were assessed for eligibility of which 54 were selected for full text review (Figure 1). Twenty-two publications were included in the final analysis (Balia, Brau, & Marrocu, 2014; Basu, 2005; Beukers, Kemp, & Varkevisser, 2014; Chernew, Scanlon, & Hayward, 1998; Cook et al., 2009; Escarce & Kapur, 2009; Fabbri & Robone, 2010; Fattore, Petrarca, & Torbica, 2014; Hanning, Ahs, Winblad, & Lundstrom, 2012; Howard, 2006; Kronebusch, 2009; Losina et al., 2007; Messina, Forni, Collini, Quercioli, & Nante, 2013; Nostedt et al., 2014; Pope, 2009; Radcliff, Brasure, Moscovice, & Stensland, 2003; Roh, Lee, & Fottler, 2008; Roh & Moon, 2005; Saunders, Bellamy, Menachemi, Chukmaitov, & Brooks, 2009; Sivey, 2012; Varkevisser & van der Geest, 2007; Varkevisser, van der Geest, & Schut, 2010, 2012). The reference lists of selected articles were hand-searched and a further four articles (Beckert, Christensen, & Collyer, 2012; Ho, 2006; Moscone, Tosetti, & Vittadini, 2012; Roh & Moon, 2005) met the inclusion criteria. A total of 26 articles were included in the final analysis. All articles were retrospective cross-sectional studies using administrative data on actual patient visits.
Figure 1.
Flowchart of study selection.
Models to Assess Patient Mobility
We found that the studies used three main methodological models to assess mobility. Two of the models fit within the first type of studies (determining whether or not patients travel beyond their nearest provider; see the “Method” section). We refer to these as the “hospital bypassing model” (estimating the proportion of patients travelling beyond their expected provider for a particular intervention/service) and as the “regional model” (estimating the proportion of patients traveling outside a predefined geographical region based on their place of residence).
A third model fits within the second type of studies (assessing the relative impact of distance and provider characteristics on the choice of provider). In this article, this is referred to as the “patient choice model.”
Table 1 outlines the key characteristics of each study according to the three models that we used to assess mobility. The studies were conducted in six countries: United States—12 studies; Italy—5 studies; Netherlands—4 studies; England—3 studies; Sweden—1 study; and Canada—1 study. Of the five studies analyzing regional mobility, four were from Italy. Seven of the 10 studies using the hospital bypassing model were undertaken in the United States.
Table 1.
Descriptive Analysis of Selected Articles (n = 26) Stratified According to Methodological Model.
| Study and setting | Geographical unit | Time period analyzed | Secondary care discipline | Intervention | Number of patient hospital episodes | Definition of expected provider(s) | Definition of “choice set” | Percentage travelling beyond expected provider (s) | Determinants of mobility |
|---|---|---|---|---|---|---|---|---|---|
| Hospital bypassing model | |||||||||
| Nostedt (2014) Canada | One region | 2004-2006 | Surgery | Colorectal cancer surgery (Type NS) | 2,086 | 8 nearest rural hospitals performing cancer surgery | Any hospital beyond eight nearest rural cancer surgery providers | (1) 46.5% bypass all rural cancer centers for rectal cancer surgery. (2) 28.8% bypass all rural cancer centers for colon cancer surgery | Provider characteristics—Provider reputation; Patient characteristics—Disease severity |
| Cook (2009) England | One region | January 2005-June 2006 | Medicine | HIV (mixed services) | 3,983 | Nearest hospital offering HIV care | Any hospital beyond nearest provider offering HIV care | 50% | Patient characteristics—Socioeconomic status, age |
| Escarce (2009) USA | One region | 2000 | (1) Surgery(2) Medicine(3) Obstetrics(4) Pediatrics | NA | 224,990 | All hospitals within threshold distance | Any hospital beyond threshold distance | 76.30% | Accessibility—Distance; Provider characteristics—Hospital size, advanced technology; Patient characteristics—Health insurance plan |
| Saunders (2009) USA | One region | 1997-2004 | (1) Medicine(2) Surgery | (1) Colonoscopy, (2) Endoscopy | 3,543,194 | Hospitals within patient zip code providing endoscopy services | Any hospital or ambulatory care center beyond patient zip code offering endoscopy services | 52.5% for Colonoscopy, 45.4% for Upper GI endoscopy | Accessibility—Distance; Patient characteristics—Health insurance plan, ethnicity |
| Roh (2008) USA | One region | 2000-2003 | Obstetrics and Gynecology | NA | 10,384 | Nearest rural hospital | Any hospital beyond nearest rural provider | 36.30% | Accessibility—Distance; Provider characteristics—Degree of market competition; Patient Characteristics—Health insurance plan |
| Losina (2007) USA | National | 2000 | Surgery | Knee replacement | 113,015 | Nearest hospital plus any hospitals within 2 miles of that hospital | Any hospital beyond 2 miles of patient’s nearest provider | 42.70% | Provider characteristics—Provider quality; Patient characteristics—Ethnicity, socioeconomic status, urban residence |
| Varkevisser (2007) Netherlands | National | 2003 | Surgery | Neurosurgical/orthopedic outpatient visit | 58,475 | Nearest hospital providing neurosurgical or orthopedic services | Any hospital beyond nearest provider offering orthopedic or neurosurgical services | 40% for orthopedic services. 50% for neurosurgical services | Accessibility—Travel time Provider characteristics—Waiting times, provider quality; Patient characteristics—Patient comorbidity, age, socioeconomic status, intervention type |
| Basu (2005) USA | Four regions | 1997 | (1) Surgery, (2) Medicine | (1) Hip/joint replacement, (2) Breast reconstruction post mastectomy, (3) Organ transplantation, (4) Bone marrow transplantation, (5) CABG, (6) PCI, (7) Pacemaker insertion | 40,665 | All hospitals within threshold distance | Any hospital beyond threshold distance | 45% | Patient characteristics—Age, ethnicity, disease severity, health insurance plan, residence adjacent to metropolitan center |
| Roh (2005) USA | One region | 1993-2000 | Obstetrics | NA | 19,618 | Nearest rural hospital | Any hospital beyond nearest rural provider | NA | Provider characteristics—Advanced technology; Patient characteristics—Health insurance plan, disease severity, age, ethnicity |
| Radcliff (2003) USA | Seven regions | 1991-1996 | (1) Obstetrics, (2) Surgery | NA | 1,473,755 | 1. Nearest rural hospital, 2. Any hospital within threshold distance 15 miles (Bypass 15) | 1. Any hospital beyond nearest provider, 2. Any hospital beyond 15 miles of patient residence | Bypass 15 rate—23.3% obstetrics, 50.1% specialty surgery, 31% general surgery. | Patient Characteristics —Region of residence, disease type, health insurance plan |
| Patient choice model | |||||||||
| Beukers (2014) Netherlands | National | 2008-2010 | Surgery | Hip replacement | 56,256 | Nearest hospital providing orthopedic services | All 92 hospitals providing orthopedic services in Netherlands | NA | Accessibility—Travel time; Provider Characteristics—Waiting time, Provider quality; Patient characteristics—Gender, Age > 60 years |
| Beckert (2012) England | National | 2008-2009 | Surgery | Hip replacement | 39,060 | Nearest hospital | 30 nearest hospitals to the patient providing orthopedic services | 40% bypass nearest hospital | Accessibility—Distance; Provider characteristics—Provider quality, waiting times; Patient characteristics—Age, socioeconomic status |
| Moscone (2012) Italy | National | 2004-2007 | (1) Surgery, (2) Medicine | (1) CABG, (2) PCI | 230,600 | Nearest hospital | All hospitals within region (n = 144) | 45% bypass hospitals within 15km of residence. 19% bypass hospitals within 50 km of residence | Accessibility—Distance; Provider characteristics—Hospital size, private hospital; Patient Characteristics—Social network effect, prior hospital use |
| Varkevisser (2012) Netherlands | National | 2006 | Medicine | PCI | 2,670 | Nearest hospital providing neurosurgery services | All hospitals within threshold travel time providing neurosugery services | NA | Provider characteristics—Provider quality, provider reputation (clinical/nonclinical staff assessment) |
| Sivey (2012) England | National | 2001-2004 | Surgery | Cataract | 87,128 | Nearest hospital receiving >30 cataract referrals for each GP practice | Nearest 10 hospitals receiving >30 cataract referrals for each GP practice | NA | Accessibility—Travel time, waiting time; Patient Characteristics—Rural residence |
| Varkevisser (2010) Netherlands | National | 2003 | Surgery | Neurosurgical outpatient visit | 5,389 | Nearest hospital providing PCI | All hospitals within threshold travel time providing PCI | NA | Accessibility—Travel time; Provider characteristics—Provider reputation (clinical/nonclinical staff assessment), waiting time; Patient Characteristics —Gender, retired status, lower socioeconomic status |
| Kronebusch (2009) USA | Four regions | 1995-1996. 2001-2002 | Surgery | (1) CABG, (2) Hip replacement, (3) Knee replacement, (4) Breast cancer surgery, (5) Colorectal cancer surgery, (6) Thoracic cancer surgery, (7) Open prostatectomy, (8) Transurethral resection of the prostate (TURP) | 1,595,597 (1995-1996). 1,836,078 (2001-2002) | Nearest hospital | All hospitals within threshold distance | NA | Accessibility—Distance; Provider Characteristics—Degree of market competition, provider quality |
| Pope (2009) USA | One state plus sample of other states | 1998-2004 | Medicine | Cardiology (Mixed services) | 28,647 | Nearest hospital | All hospitals within statewide sample (n = 164) | NA | Provider Characteristics—Provider quality |
| Ho (2006) USA | Five regions | 1997-1998 | (1) Cancer, (2) Obstetrics, (3) Surgery, (4) Medicine | NA | 28,866 | Nearest hospital | All hospitals within threshold distance | NA | Accessibility—Distance; Provider Characteristics—Advanced technology |
| Howard (2006) USA | National | 2000-2002 | Surgery | Kidney transplant | 36,991 | Nearest kidney transplant center | Individualized for each patient based on threshold distance and location of nearest kidney transplant provider | NA | Accessibility—Distance; Provider Characteristics—Provider quality; Patient Characteristics—Age, ethnicity, socioeconomic status, health insurance plan, disease severity |
| Chernew (1998) USA | One region | 1991 | Surgery | CABG | 8,000 | Nearest hospital providing CABG | All hospitals within threshold distance performing CABG | NA | Accessibility—Distance; Provider Characteristics—Provider quality; Patient Characteristics—Health insurance plan |
| Regional model | |||||||||
| Balia (2014) Italy | National | 2008 | (1) Surgery, (2) Medicine | NA | 863,953 | All hospitals within patient’s administrative region of residence | All administrative regions within Italy | 25.10% | Accessibility—Distance; Region Characteristics —Provider capacity (beds), GDP per capita of region, advanced technology, proportion of population >65 years |
| Fattore (2014) Italy | National | 2009 | Surgery | Aortic valve replacement | 11,531 | All hospitals within patient’s administrative region of residence | All administrative regions within Italy | 13.60% | Provider Characteristics—Private center; Patient Characteristics—Age; Region Characteristics—Region of residence, region size, |
| Messina (2013) Italy | One region | 2001-2007 | Surgery | Cardiac (Type NS) | 23,645 | All cardiac units within patient’s health area | All three health areas within patient’s region | 27% | Patient Characteristics—Disease severity; Region Characteristics—Local health area |
| Hanning (2012) Sweden | National | 2005-2008 | Surgery | Cataract | 293,608 | All hospitals within patient’s administrative region of residence | All administrative regions within Sweden | 4% | Patient Characteristics—Age, patient comorbidity; Provider Characteristics—Waiting times |
| Fabbri (2010) Italy | National | 2001 | (1) Medicine, (2) Surgery | (1) Cancer (Mixed services), (2) Complex surgery (Type NS) | 5,674 | All hospitals within patient’s local health authority of residence | 171 local health authorities within Italy | 42% for cancer treatment. 58% for complex surgery. | Region Characteristics—GDP per capita of region, advanced technology, regional contiguity |
Note. NA = not applicable; NS = not stated; PCI = percutaneous coronary intervention; CABG = coronary artery bypass grafting. Refer to the “Results” section for description of methodological models. “Expected Provider” defined as the nearest provider(s) offering the relevant intervention given the patient’s clinical condition. “Choice Set” defined as the selection of hospitals that offer the relevant intervention as defined by the study authors. Studies by Beckert (2012) and Moscone (2012) classified as patient choice model, but also used hospital bypass model as part of an initial analysis to quantify extent of mobility.
Coronary artery bypass grafting, percutaneous coronary intervention (Chernew et al., 1998; Moscone et al., 2012), cataract surgery, and joint replacement surgery (Beckert et al., 2012; Beukers et al., 2014; Losina et al., 2007) were the commonest elective interventions analyzed. Other studies looked at a mix of surgical and medical admissions or a variety of admission types related to a particular secondary care discipline (e.g., neurosurgical services, HIV services, cancer; Cook et al., 2009; Varkevisser & van der Geest, 2007).
Definition of “Expected Provider” and “Choice Set”
A number of different definitions for the expected provider were used across the selected studies (Table 1). In the majority of studies using the hospital bypassing model this was the nearest provider. However, other definitions included all providers within a threshold distance or a specific area code (Escarce & Kapur, 2009; Saunders et al., 2009). The expected provider(s) in studies using the regional model were all hospitals within an administrative or governmental region.
The choice set was constrained in some of the studies using the patient choice model to providers within a defined regional area (Moscone et al., 2012; Pope, 2009). However, other definitions were evident. For example, in a Dutch study using the patient choice model for neurosurgical services, only hospitals within an hour of the patient’s residence were included in the choice set. The authors assumed that individuals traveling further were away from home when they needed health care (Varkevisser et al., 2010). Similarly in a U.K. study, the choice set only included the nearest 10 hospitals receiving more than 30 cataract referrals from the patients’ primary care physicians (Sivey, 2012).
Extent of Mobility
All studies showed evidence of patient mobility in response to provider choice policies. For those studies using the hospital bypassing mode, rates ranged from 23% to 76% (Basu, 2005; Cook et al., 2009; Escarce & Kapur, 2009; Losina et al., 2007; Nostedt et al., 2014; Radcliff et al., 2003; Roh et al., 2008; Saunders et al., 2009; Varkevisser & van der Geest, 2007).
Distant Admission
Threshold distances were also used to define local and distant admissions (Basu, 2005; Escarce & Kapur, 2009; Radcliff et al., 2003; Saunders et al., 2009). In most cases, these thresholds were defined arbitrarily; however, one study created a threshold based on average distances travelled to local hospitals by patients living within the same county. Different thresholds were subsequently created according to admission type and county of residence (Basu, 2005).
Two studies used a series of increasing threshold distances to analyze patterns of mobility (Radcliff et al., 2003; Saunders et al., 2009). The results of both studies demonstrated that while patients are prepared to bypass their nearest provider, there is a threshold distance above which patients are rarely prepared to travel to receive care at an alternative center. Furthermore, the Saunders study showed that rates of hospital bypassing increased between 10 and 20 miles to 30 to 50 miles but sharply decreased beyond 30 to 50 miles (Saunders et al., 2009).
Other studies, assessed not only whether rural patients bypassed their nearest provider but whether their destination provider was a rural or urban center (Roh et al., 2008; Roh & Moon, 2005). Urban admissions were considered as a proxy for distant admission and analyzed separately to those admissions at other rural providers.
Determinants of Patient Mobility
As can be expected, all studies, irrespective of the model they used to study patient mobility, showed that accessibility to a provider has an important effect on patient mobility. Patients are more likely to receive treatment from their nearest provider (either measured in terms of distance or travel time) or at a hospital located within their region (Balia et al., 2014; Beckert et al., 2012; Beukers et al., 2014; Chernew et al., 1998; Escarce & Kapur, 2009; Ho, 2006; Howard, 2006; Kronebusch, 2009; Moscone et al., 2012; Roh et al., 2008; Saunders et al., 2009; Sivey, 2012; Varkevisser et al., 2010, 2012; Varkevisser & van der Geest, 2007).
Studies using the hospital bypassing or patient choice models considered the impact of patient and provider characteristics at the patient level on decisions to bypass or choose a particular provider (Tables 1 and 2). In contrast, the studies using the regional model considered measures describing providers at a regional level and their impact on the flow of patients between regions.
Table 2.
Study Checklist (Articles Listed by Date of Publication)—See Appendix B for a More Detailed Description of the Items.
| Patient factors |
Health system factors |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Study described in detail? | Study design | Datasource | Inclusion/exclusion criteria specified? | Was the study population representative? | Secondary care context described in detail? | Appropriate hospital choice set? | Appropriate statistical analysis? | Age | Gender | Ethnicity | Socio-economic status | Insurance status | Disease severity | Comor-bidities | Provider capacity | GP Referral patters | Copay-ments | Provider charact-eristics | Provider quality | Regional charact-eristics |
| Balia (2014) Italy |
Yes | Patient choice model | National administrative database | Yes | Yes | No | No | Yes | × | × | × | × | N/A | × | × | × | × | N/A | ✓ | × | ✓ |
| Beukers (2014) Netherlands | Yes | Patient choice model | National administrative database | No | Yes | Yes | Yes | Yes | ✓ | ✓ | × | × | × | × | × | ✓ | × | N/A | ✓ | ✓ | × |
| Fattore (2014) Italy | Yes | Inter-regional model | National administrative database | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | × | × | N/A | × | × | × | × | N/A | ✓ | × | ✓ |
| Nostedt (2014) Canada | No | Hospital bypassing model | Disease-specific registry | No | No | Yes | Yes | No | ✓ | ✓ | × | × | N/A | ✓ | × | × | × | N/A | × | × | × |
| Messina (2013) Italy | Yes | Inter-regional model | Regional administrative database | Yes | Yes | Yes | Yes | No | × | × | × | × | N/A | ✓ | × | × | × | N/A | × | × | × |
| Beckert (2012) England | Yes | Patient choice model | National administrative database | Yes | Yes | Yes | Yes | Yes | ✓ | × | × | ✓ | N/A | × | × | ✓ | ✓ | N/A | ✓ | ✓ | × |
| Hanning (2012) Sweden | Yes | Inter-regional model | Disease speciifc registry | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | × | × | N/A | ✓ | × | ✓ | × | N/A | × | × | × |
| Moscone (2012) Italy | Yes | Patient choice model | Regional administrative database | Yes | Yes | Yes | No | Yes | ✓ | ✓ | × | × | N/A | × | × | × | ✓ | N/A | ✓ | × | × |
| Varkevisser (2012) Netherlands | Yes | Patient choice model | Health insurer claims database | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | × | × | ✓ | × | × | × | × | N/A | ✓ | ✓ | × |
| Sivey (2011) England | Yes | Patient choice model | National administrative database | Yes | No | Yes | Yes | Yes | ✓ | × | × | ✓ | N/A | × | × | ✓ | ✓ | N/A | × | × | × |
| Fabbri (2010) Italy | Yes | Interregional model | National administrative database | No | Yes | No | No | Yes | × | × | × | × | N/A | × | × | × | × | N/A | ✓ | × | ✓ |
| Varkevisser (2010) Netherlands | Yes | Patient choice model | Health insurer claims database | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | × | ✓ | ✓ | × | × | × | × | N/A | ✓ | × | × |
| Cook (2009) England | Yes | Hospital bypassing model | Disease-specific registry | Yes | Yes | Yes | No | Yes | ✓ | ✓ | ✓ | ✓ | N/A | × | × | × | × | N/A | ✓ | × | NA |
| Escarce (2009) USA | Yes | Hospital bypassing model | Regional administrative database | No | No | No | No | Unclear | × | × | × | × | ✓ | × | × | × | × | × | ✓ | × | × |
| Kronebusch (2009) USA | Yes | Patient choice model | Regional administrative database | No | Yes | Yes | Yes | Yes | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | × | × | × | × | ✓ | × |
| Pope (2009) USA | No | Patient choice model | Regional administrative database | Unclear | No | No | No | Yes | × | × | × | × | ✓ | × | × | × | × | N/A | × | ✓ | × |
| Saunders (2009) USA | Yes | Hospital bypassing model | Regional administrative database | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | ✓ | × | ✓ | × | ✓ | × | × | × | ✓ | × | × |
| Roh (2008) USA | Yes | Hospital bypassing model | Regional administrative database | Yes | Unclear | No | No | Yes | ✓ | × | ✓ | × | ✓ | × | × | × | × | × | ✓ | × | × |
| Losina (2007) USA | No | Patient choice model | Health insurer claims database | Yes | Yes | Yes | Yes | Yes | × | × | ✓ | ✓ | ✓ | × | × | × | × | N/A | × | ✓ | ✓ |
| Varkevisser (2007) Netherlands | Yes | Hospital bypassing model | Health insurer claims database | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | × | ✓ | ✓ | × | × | ✓ | × | N/A | ✓ | × | × |
| Ho (2006) USA | No | Patient choice model | Other | Unclear | No | No | No | Yes | × | × | × | × | ✓ | × | × | × | × | × | ✓ | × | × |
| Howard (2006) USA | Yes | Patient choice model | Disease-specific registry | Yes | Yes | Yes | Yes | Yes | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | × | ✓ | ✓ | × |
| Basu (2005) USA | No | Hospital bypassing model | Regional administrative database | No | Unclear | Unclear | No | Yes | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | × | × | × | ✓ |
| Roh (2005) USA | Yes | Hospital bypassing model | Regional administrative database | Yes | No | No | No | Yes | ✓ | × | ✓ | × | ✓ | ✓ | ✓ | × | × | × | ✓ | × | × |
| Radcliff (2003) USA | Yes | Hospital bypassing model | Regional administrative database | Yes | Yes | No | No | No | × | × | × | × | ✓ | × | × | × | × | × | × | × | × |
| Chernew (1998) USA | Yes | Patient choice model | Regional administrative database | Yes | Unclear | Yes | No | Yes | × | × | × | × | ✓ | × | × | × | × | × | ✓ | ✓ | N/A |
Note. N/A = not applicable; ✓= factor accounted for in study; ×= factor not accounted for in study.
For patient characteristics, 10 out of the 17 studies that reported results demonstrated that older patients were more likely to receive treatment from their nearest hospital (Balia et al., 2014; Basu, 2005; Beckert et al., 2012; Beukers et al., 2014; Cook et al., 2009; Fattore et al., 2014; Hanning et al., 2012; Howard, 2006; Roh & Moon, 2005; Varkevisser & van der Geest, 2007). Six out of nine studies demonstrated that patients in lower socioeconomic groups were more likely to receive treatment from their nearest providers (Beckert et al., 2012; Cook et al., 2009; Howard, 2006; Losina et al., 2007; Varkevisser et al., 2010; Varkevisser & van der Geest, 2007).
Six of the eight studies reviewing the impact of ethnicity on patterns of mobility found a statistically significant association (Table 1). Of these, four studies demonstrated that non-White patients were less likely to bypass local rural hospitals than White patients when controlling for all other factors (Basu, 2005; Roh et al., 2008; Roh & Moon, 2005; Saunders et al., 2009). These studies also demonstrated that non-White patients are less likely to travel as far as White patients to receive treatment, especially to providers based in out-of-area urban settings. Two studies found that non-White men and women were less likely to receive care at higher quality hospitals for total hip replacement surgery and kidney transplantation (Howard & Kaplan, 2006; Losina et al., 2004).
In eight of the nine U.S. studies that included patients affiliated with different health insurance plans, the extent of mobility varied depending on health plan type (Basu, 2005; Chernew et al., 1998; Escarce & Kapur, 2009; Howard, 2006; Radcliff et al., 2003; Roh et al., 2008; Roh & Moon, 2005; Saunders et al., 2009). It is not possible to make comprehensive conclusions as to overall trend in patient mobility according to insurance plan type. However, the increased rates of mobility reported for patients with commercial health insurance plans may be due to the potentially greater number of alternative providers that are available to choose from compared with what would be the case with Health Maintenance Organizations, Medicaid, and Medicare plans (Basu, 2005; Roh et al., 2008). Another explanation could be that younger patients and those with employer-sponsored coverage were more responsive to quality-of-care differences between providers and had the means (physical/financial) to access more distant hospitals (Radcliff et al., 2003).
All six studies analyzing the effect of provider capacity (i.e., measured in terms of waiting times for a particular treatment) on patient mobility demonstrated that patients were more likely to move to providers with shorter waiting times (Beckert et al., 2012; Beukers et al., 2014; Hanning et al., 2012; Sivey, 2012; Varkevisser et al., 2010; Varkevisser & van der Geest, 2007).
All eight studies analyzing the effect of proxy measures for provider quality on patient mobility demonstrated that patients are more likely to travel further to receive treatment from providers who deliver a better quality of care according to these measures (Beckert et al., 2012; Beukers et al., 2014; Chernew et al., 1998; Howard, 2006; Kronebusch, 2009; Losina et al., 2007; Moscone et al., 2012; Pope, 2009; Varkevisser et al., 2012; Varkevisser & van der Geest, 2007). Different measures of provider quality were used in each of the studies (e.g., generic mortality rates, hospital infection rates, heart failure readmission rates, transplant failure rates, high volume surgical unit, hospital ranking). Other provider factors that are associated with a willingness to travel further are the availability of advanced technology (although not necessarily for the specialty in question) and a larger hospital (Balia et al., 2014; Escarce & Kapur, 2009; Fabbri & Robone, 2010; Ho, 2006; Roh & Moon, 2005).
In administrative regions with older populations (age >65 years) and high levels of affluence (measured as GDP per capita) patients were less likely to move to providers outside their region. Similarly patients were more likely to seek care within regions that were accessible by public and private transport (Balia et al., 2014; Fabbri & Robone, 2010; Fattore et al., 2014).
Study Assessment
Articles were assessed according to the checklist described in the “Method” section (Table 2). When reviewing the hospital choice sets, we found that 12 of the 26 studies did not state explicitly whether the alternative hospitals offered the particular service in question (Balia et al., 2014; Basu, 2005; Chernew et al., 1998; Cook et al., 2009; Escarce & Kapur, 2009; Fabbri & Robone, 2010; Ho, 2006; Moscone et al., 2012; Pope, 2009; Radcliff et al., 2003; Roh et al., 2008; Roh & Moon, 2005). Also, it is likely that the fitness of the patients and severity of the disease will have an effect on patient mobility, but only six studies assessed disease severity (Basu, 2005; Hanning et al., 2012; Howard, 2006; Messina et al., 2013; Nostedt et al., 2014; Roh & Moon, 2005) and three comorbidity (Kronebusch, 2009; Roh & Moon, 2005; Saunders et al., 2009).
Another important checklist item was that studies accounted for possible effects of copayments on decisions where to have their care or treatment. While some of the U.S. studies chose particular subpopulations (e.g., Medicare patients for whom copayments are generally fixed between providers; Losina et al., 2007; Pope, 2009), 10 of the 12 studies which looked at patients enrolled in a variety of insurance schemes made no account of the impact of variation in copayments on their destination hospital (Basu, 2005; Chernew et al., 1998; Escarce & Kapur, 2009; Ho, 2006; Howard, 2006; Kronebusch, 2009; Radcliff et al., 2003; Roh et al., 2008; Roh & Moon, 2005; Saunders et al., 2009).
Discussion
This is the first review to systematically describe and analyze the published empirical literature on patient mobility for elective services in the secondary care setting. Our review demonstrates that patients travel to a hospital other than their nearest provider for a wide variety of health care interventions.
A further major finding of this review is the identification of three main methodological models (hospital bypassing, regional, and patient choice models) used to analyze patient mobility in different health care markets. Our results demonstrate that the model used to define mobility is influenced by the health care context with no single model providing a single policy frame. For instance, the regional model has been used almost exclusively in the Italian studies, with the key variable being whether or not patients receive treatment in the administrative region they reside in. This is because the organization and administration of publicly financed health care in Italy was decentralized to 20 regions following constitutional reform in 2001 (Balia et al., 2014). Rates of inflow and outflow of patients are analyzed to assess the effectiveness of regional health care supply, and look for flow imbalances which may have an impact on regional budgets (France, Taroni, & Donatini, 2005). Sweden adopts a similar system with health care decentralized to county councils (Vrangbæk, Østergren, Birk, & Winblad, 2007).
In contrast, the United Kingdom, Netherlands, and the United States do not exhibit the same level of regional decentralization and therefore the hospital bypassing and patient choice models were used to study mobility between health care providers. While clear differences in the nature of the health care market and extent of competition exist, the response of patients to perceived differences in provider quality is an essential component of all these three countries.
A number of the U.S. studies in our review used the hospital bypassing model to analyze the extent of “rural hospital bypassing” (i.e., the proportion of rural residents bypassing their nearest rural provider[s] to access an urban center for a particular intervention; Escarce & Kapur, 2009; Roh & Moon, 2005). The extent to which this is occurring is a particular concern in the United States due to long-standing concerns related to the availability and quality of health care resources in rural settings (Bronstein & Morrisey, 1991; Buczko, 1997; Escarce & Kapur, 2009).
The review demonstrated that variation exists in the proportion of patients moving to alternative providers for elective secondary services (23%-77%). However, we found that the extent of mobility depends on a number of factors. These include, apart from the secondary health care intervention in question, the study methods used and the geographical unit of analysis (national vs. regional).
It is unclear from the available evidence whether such mobility is sufficient for effective competition and improvements in quality. However, the results of this review demonstrate that there are actual changes in market share which may represent a major driver given the extent of mobility reported.
We found that patients were more likely to move to providers considered to be of higher quality, or that offered advanced technologies. However, mobility may have a negative effect on competition by providing increased incentives for risk selection of patients by providers in order to improve their apparent performance according to the selected indicators.
Service capacity may also be an emerging issue for high-performing centers that receive a net gain of patients due to mobility. Without adequate planning, an increased flow of patients from outside the provider catchment area may result in lengthening waiting lists. At the same time, it may result in unused capacity and resources within centers that have a net loss of patients, creating health system inefficiencies.
The effect of patient choice policies on equity remains a key concern, given that older patients and lower socioeconomic groups are less likely to travel beyond their nearest health care provider. The impact of disease complexity or comorbidities on the decision to move between providers is unclear. On the other hand, the outflow of patients from hospitals located in socioeconomically deprived settings may provide the necessary stimulus to improve provider performance and in this way benefit the majority of nonmovers.
One of the challenges in reviewing these studies is to ascertain whether they are able to identify true movers (i.e., mobility due to patient choice rather than health system factors). Our checklist sought to assess the extent to which these factors have been accounted for (Table 2). We found, particularly in the U.S. studies, that there was limited information on the choice set of hospitals available to each patient. As a result, it was not always possible to ascertain whether the choice of available hospitals considered in the study actually provided the service or intervention in question.
It was also not possible to assess the extent of selective contracting of providers by different insurers in the U.S. market, and how centralization of services contributed to patterns of mobility. A further issue in the U.S. studies was the paucity of information on the extent of variation in copayments. It was therefore not always possible to disentangle the impact between price and quality on mobility.
Primary care referral patterns and capacity of available providers (e.g., waiting lists) were rarely considered in the selected studies (Table 2), predominantly because of data constraints. Provider capacity as measured through waiting lists is an important health system factor (Dawson, Gravelle, Jacobs, Martin, & Smith, 2007) which can directly affect patient mobility (Beckert et al., 2012; Beukers et al., 2014; Sivey, 2012).
Conclusion
Provider choice policies have previously been criticized due to the lack of empirical evidence that such policies influence where patients receive treatment (Pollock et al., 2012). Our findings provide substantial evidence that patients are prepared to travel beyond their nearest provider for their care or treatment. It has been hypothesized that the driver for improving provider performance would be the threat of losing market share and that even movement of only 5% to 10% of patients would provide the necessary incentive to improve quality (Berwick et al., 2003; Le Grand, 2009). However, these results suggest that there are likely to be “winners” and “losers” from health care market reforms, which could have an impact on the configuration of existing health care markets if some providers continue to lose market share. There is therefore potentially a trade-off between the effects of mobility on improving provider quality but at the same time decreasing provider capacity.
Equity also remains an issue given that the elderly and low socioeconomic groups are less likely to travel beyond their nearest provider for health care. This in turn may result in hospitals within socioeconomically deprived areas with older demographic profiles having to manage far more complex patient cohorts (both medically and socially), which subsequently affects their quality outcomes.
Further work is required to understand the drivers of patient mobility (e.g., quality, reputation, referral patterns) and its impact on equity in access to services and patient outcomes. In this regard, our checklist for studies of patient mobility provides a framework for developing future research facilitating the comparability of study results.
Appendix A
PubMed Search String
Search ((((((((((((((((patient choice*[Title/Abstract]) OR consumer choice*[Title/Abstract]) OR patient preference*[MeSH Terms]) OR patient preference*[Title/Abstract]) OR patient mobility[Title/Abstract]) OR patient travel[Title/Abstract]) OR hospital referral*[MeSH Terms]) OR hospital referral[Title/Abstract])) OR hospital bypassing)) OR hospital choice[Title/Abstract])) OR hospital market[Title/Abstract]))) AND (((((((health care provider[MeSH Terms]) OR provider*[Title/Abstract]) OR hospital*[Title/Abstract]) OR doctor*[Title/Abstract]) OR Physician*[Title/Abstract]) OR “specialist care”[Title/Abstract]))
Appendix B
Study Checklist
1. Was the study setting described in detail? (Yes/No/unclear/Not applicable)
The study setting should be described in sufficient detail so that others can determine if it is comparable to the population of interest to them. This includes information on the health care environment for a particular country and differences between regions relating to provider choice policy, organization of providers, and system of reimbursement.
- 2. What study design was used to capture “mobility” (State one of the following):
- Patient choice model
- Hospital bypassing model
- Interregional model
- 3. What was the main data source? (state one of the following):
- National administrative database
- Regional administrative database
- Disease-specific registry
- Health insurer claims database
- Other
4. Were both inclusion and exclusion criteria specified? (Yes/No/unclear/Not applicable)
This includes information on the sampling frame (e.g., entire population, random sample) and an adequate description of the inclusion and exclusion criteria in order to enable a researcher to determine if it is comparable to the population of interest to them.
5. Was the study population representative of the target population? (Yes/No/unclear/Not applicable)
The study subjects should be described in sufficient detail to ascertain whether those subjects who participated were representative of the entire population from which they were recruited.
6. Was the secondary health care context described in detail? (Yes/No/unclear/Not applicable)
The methods should be described in detail providing information on the clinical discipline being analyzed, whether the health care episodes reviewed are inpatient or outpatient based and whether they are elective or emergency care episodes. In addition, there should be information on the intervention (s) that are being analyzed. If multiple interventions or medical disciplines are included, there should be evidence of detailed subgroup analysis to allow an interpretation of differences between different sets of conditions.
7. Is the “hospital choice set” appropriate given intervention and disease status (i.e., do all hospitals offer the intervention being assessed or account for technical requirement of patient) (Yes/No/unclear/Not applicable)
- 8. Were the following patient characteristics influencing mobility taken into account? (✓ or × or N/A, i.e., Yes or No or Not applicable)
- Age
- Gender
- Disease severity (e.g., cancer stage)
- Comorbidities
- Socioeconomic status
- Ethnicity
- Health insurance status (e.g., medicare vs. private insurer)
There has to be evidence that relevant patient characteristics have been included in the analysis either as confounding factors, or as exposures of interest.
- 9. Were the following health system characteristics influencing mobility taken into account? (✓ or × or N/A)
- Forced mobility due to insufficient provider capacity (e.g., Waiting time)
- Physician-induced mobility (e.g., GP referral patterns)
- Copayments for health care services
- Characteristics of the provider (e.g., size, academic status, advanced technology availability)
- Provider quality metrics (e.g., disease-specific mortality, ranking)
- Characteristics of region (e.g., urban/rural, region size, GDP per capita)
As above, these factors must be quantified and used in the analysis as confounding factors or exposures of interest.
10. Have the authors used a statistical analysis technique that enables the reader to assess the effect of each patient or system factor (as per the papers’ specific research question[s]) on the likelihood or magnitude of patient mobility (Yes/No/unclear/Not applicable)
Footnotes
Authors’ Note: The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Ajay Aggarwal is funded by a Doctoral Research Fellowship from the National Institute for Health Research.
References
- Balia S., Brau R., Marrocu E. (2014). What drives patient mobility across Italian regions? Evidence from hospital discharge data. Developments in Health Economics and Public Policy, 12, 133-154. [DOI] [PubMed] [Google Scholar]
- Basu J. (2005). Severity of illness, race, and choice of local versus distant hospitals among the elderly. Journal of Health Care for the Poor and Underserved, 16, 391-405. [DOI] [PubMed] [Google Scholar]
- Beckert W., Christensen M., Collyer K. (2012). Choice of NHS-funded Hospital Services in England. Economic Journal, 122, 400-417. Doi: 10.1111/j.1468-0297.2012.02496.x [DOI] [Google Scholar]
- Berwick D. M., James B., Coye M. J. (2003). Connections between quality measurement and improvement. Medical Care, 41(Suppl. 1), I-30-I-38. [DOI] [PubMed] [Google Scholar]
- Beukers P. D., Kemp R. G., Varkevisser M. (2014). Patient hospital choice for hip replacement: Empirical evidence from the Netherlands. European Journal of Health Economics, 15, 927-936. Doi: 10.1007/s10198-013-0535-7 [DOI] [PubMed] [Google Scholar]
- Boonen L. H. H. M., Donkers B., Schut F. T. (2011). Channeling consumers to preferred providers and the impact of status quo bias: Does type of provider matter? Health Services Research, 46, 510-530. Doi: 10.1111/j.1475-6773.2010.01196.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronstein J. M., Morrisey M. A. (1991). Bypassing rural hospitals for obstetrics care. Journal of Health Politics, Policy and Law, 16, 87-118. [DOI] [PubMed] [Google Scholar]
- Buczko W. (1997). Nonuse of local hospitals by rural Medicare beneficiaries. Journal of Health and Human Services Administration, 19, 319-340. [PubMed] [Google Scholar]
- Chernew M., Scanlon D., Hayward R. (1998). Insurance type and choice of hospital for coronary artery bypass graft surgery. Health Services Research, 33(3, Pt. 1), 447-466. [PMC free article] [PubMed] [Google Scholar]
- Cook P. A., Downing J., Wheater C. P., Bellis M. A., Tocque K., Syed Q., Phillips-Howard P. A. (2009). Influence of socio-demographic factors on distances travelled to access HIV services: Enhanced surveillance of HIV patients in north west England. BMC Public Health, 9, 78 Doi: 10.1186/1471-2458-9-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Z., Gibbons S., Jones S., McGuire A. (2011). Does hospital competition save lives? Evidence from the English NHS Patient Choice Reforms. Economic Journal, 121, F228-F260. Doi: 10.1111/j.1468-0297.2011.02449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D. M., Huckman R. S., Landrum M. B. (2004). The role of information in medical markets: An analysis of publicly reported outcomes in cardiac surgery. Cambridge, MA: National Bureau of Economic Research. [DOI] [PubMed] [Google Scholar]
- Dawson D., Gravelle H., Jacobs R., Martin S., Smith P. C. (2007). The effects of expanding patient choice of provider on waiting times: Evidence from a policy experiment. Health Economics, 16, 113-128. Doi: 10.1002/hec.1146 [DOI] [PubMed] [Google Scholar]
- Dixon A., Robertson R., Appleby J., Burge P., Devlin N. J. (2010). Patient choice: How patients choose and how providers respond. London, England: The King’s Fund. [Google Scholar]
- Dixon A., Robertson R., Bal R. (2010). The experience of implementing choice at point of referral: A comparison of the Netherlands and England. Health Economics, Policy and Law, 5, 295-317. [DOI] [PubMed] [Google Scholar]
- Dusheiko M. (2014). Patient choice and mobility in the UK health system: Internal and external markets. In Levaggi R., Montefiori M. (Eds.), Health care provision and patient mobility (pp. 81-132). New York, NY: Springer. [DOI] [PubMed] [Google Scholar]
- Escarce J. J., Kapur K. (2009). Do patients bypass rural hospitals? Determinants of inpatient hospital choice in rural California. Journal of Health Care for the Poor and Underserved, 20, 625-644. [DOI] [PubMed] [Google Scholar]
- Fabbri D., Robone S. (2010). The geography of hospital admission in a national health service with patient choice. Health Economics, 19, 1029-1047. [DOI] [PubMed] [Google Scholar]
- Fattore G., Petrarca G., Torbica A. (2014). Traveling for care: Inter-regional mobility for aortic valve substitution in Italy. Health Policy, 117, 90-97. [DOI] [PubMed] [Google Scholar]
- Finlayson S. R., Birkmeyer J. D., Tosteson A. N., Nease R. F., Jr. (1999). Patient preferences for location of care: Implications for regionalization. Medical Care, 37, 204-209. [DOI] [PubMed] [Google Scholar]
- France G., Taroni F. (2005). The evolution of health-policy making in Italy. Journal of Health Politics, Policy and Law, 30, 169-188. [DOI] [PubMed] [Google Scholar]
- France G., Taroni F., Donatini A. (2005). The Italian health-care system. Health Economics, 14(Suppl. 1), S187-S202. Doi: 10.1002/hec.1035 [DOI] [PubMed] [Google Scholar]
- Hanning M., Ahs A., Winblad U., Lundstrom M. (2012). Impact of increased patient choice of providers in Sweden: Cataract surgery. Journal of Health Services Research and Policy, 17, 101-105. [DOI] [PubMed] [Google Scholar]
- Haynes R., Lovett A., Sunnenberg G. (2003). Potential accessibility, travel time, and consumer choice: Geographical variations in general medical practice registrations in Eastern England. Environment and Planning A, 35, 1733-1750. [Google Scholar]
- Higgins J. P., Green S. (2008). Cochrane handbook for systematic reviews of interventions (Vol. 5). Wiley Online Library. [Google Scholar]
- Ho K. (2006). The welfare effects of restricted hospital choice in the US medical care market. Journal of Applied Econometrics, 21, 1039-1079. [Google Scholar]
- Howard D. H. (2006). Quality and consumer choice in healthcare: Evidence from kidney transplantation. Topics in Economic Analysis and Policy, 5(1), 1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard D. H., Kaplan B. (2006). Do report cards influence hospital choice? The case of kidney transplantation. Inquiry, 43, 150-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronebusch K. (2009). Quality information and fragmented markets: Patient responses to hospital volume thresholds. Journal of Health Politics, Policy and Law, 34, 777-827. [DOI] [PubMed] [Google Scholar]
- Laverty A. A., Smith P. C., Pape U. J., Mears A., Wachter R. M., Millett C. (2012). High-profile investigations into hospital safety problems in England did not prompt patients to switch providers. Health Affairs (Millwood), 31, 593-601. Doi: 10.1377/hlthaff.2011.0810 [DOI] [PubMed] [Google Scholar]
- Le Grand J. (2009). The other invisible hand: Delivering public services through choice and competition. Princeton, NJ: Princeton University Press. [Google Scholar]
- Loney P. L., Chambers L. W., Bennett K. J., Roberts J. G., Stratford P. W. (1998). Critical appraisal of the health research literature: Prevalence or incidence of a health problem. Chronic Diseases in Canada, 19, 170-176. [PubMed] [Google Scholar]
- Losina E., Barrett J., Baron J. A., Levy M., Phillips C. B., Katz J. N. (2004). Utilization of low-volume hospitals for total hip replacement. Arthritis Care and Research, 51, 836-842. [DOI] [PubMed] [Google Scholar]
- Losina E., Wright E. A., Kessler C. L., Barrett J. A., Fossel A. H., Creel A. H., . . . Katz J. N. (2007). Neighborhoods matter: Use of hospitals with worse outcomes following total knee replacement by patients from vulnerable populations. Archives of Internal Medicine, 167, 182-187. Doi: 10.1001/archinte.167.2.182 [DOI] [PubMed] [Google Scholar]
- Magnussen J., Vrangbæk K., Saltman R. (2009). Nordic health care systems: Recent reforms and current policy challenges. London, England: McGraw-Hill Education. [Google Scholar]
- Messina G., Forni S., Collini F., Quercioli C., Nante N. (2013). Patient mobility for cardiac problems: A risk-adjusted analysis in Italy. BMC Health Services Research, 13, 56 Doi: 10.1186/1472-6963-13-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscone F., Tosetti E., Vittadini G. (2012). Social interaction in patients’ hospital choice: Evidence from Italy. Journal of the Royal Statistical Society: Series A (Statistics in Society), 175, 453-472. Doi: 10.1111/j.1467-985X.2011.01008.x [DOI] [Google Scholar]
- Munn Z., Moola S., Riitano D., Lisy K. (2014). The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. International Journal of Health Policy and Management, 3, 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nostedt M. C., McKay A. M., Hochman D. J., Wirtzfeld D. A., Yaffe C. S., Yip B., . . . Park J. (2014). The location of surgical care for rural patients with rectal cancer: Patterns of treatment and patient perspectives. Canadian Journal of Surgery, 57, 398-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock A., Macfarlane A., Kirkwood G., Majeed F. A., Greener I., Morelli C., . . . Price D. (2012). No evidence that patient choice in the NHS saves lives. Lancet, 378, 2057-2060. [DOI] [PubMed] [Google Scholar]
- Pope D. G. (2009). Reacting to rankings: Evidence from “America’s Best Hospitals”. Journal of Health Economics, 28, 1154-1165. [DOI] [PubMed] [Google Scholar]
- Radcliff T. A., Brasure M., Moscovice I. S., Stensland J. T. (2003). Understanding rural hospital bypass behavior. Journal of Rural Health, 19, 252-259. [DOI] [PubMed] [Google Scholar]
- Ringard Å. (2010). Why do general practitioners abandon the local hospital? An analysis of referral decisions related to elective treatment. Scandinavian Journal of Public Health, 38, 597-604. [DOI] [PubMed] [Google Scholar]
- Ringard Å., Rico A., Hagen T. P. (2005, January). Expanded patient choice in Norway and the UK: Will it succeed? Paper presented at the Scandinavian Academy of Management (NFF) conference, Aarhus School of Business, Denmark. [Google Scholar]
- Roh C.-Y., Lee K. H., Fottler M. D. (2008). Determinants of hospital choice of rural hospital patients: The impact of networks, service scopes, and market competition. Journal of Medical Systems, 32, 343-353. [DOI] [PubMed] [Google Scholar]
- Roh C.-Y., Moon M. J. (2005). Nearby, but not wanted? The bypassing of rural hospitals and policy implications for rural health care systems. Policy Studies Journal, 33, 377-394. doi: 10.1111/j.1541-0072.2005.00121.x [DOI] [Google Scholar]
- Rosenthal M. B., Li Z., Milstein A. (2009). Do patients continue to see physicians who are removed from a PPO network? American Journal of Managed Care, 15, 713-719. [PubMed] [Google Scholar]
- Sanderson S., Tatt I. D., Higgins J. P. (2007). Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. International Journal of Epidemiology, 36, 666-676. [DOI] [PubMed] [Google Scholar]
- Saunders C., Bellamy G. R., Menachemi N., Chukmaitov A. S., Brooks R. G. (2009). Bypassing the local rural hospital for outpatient procedures. Journal of Rural Health, 25, 174-181. doi: 10.1111/j.1748-0361.2009.00214.x [DOI] [PubMed] [Google Scholar]
- Schwartz L. M., Woloshin S., Birkmeyer J. D. (2005). How do elderly patients decide where to go for major surgery? Telephone interview survey. BMJ, 331(7520), 821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivey P. (2012). The effect of waiting time and distance on hospital choice for English cataract patients. Health Economics, 21, 444-456. [DOI] [PubMed] [Google Scholar]
- Swedish Association of Local Authorities and Regions. (2013). Quality and efficiency in Swedish health Care—Regional comparisons 2012. Stockholm, Sweden: Author. [Google Scholar]
- Tessier G., Contandriopoulos A.-P., Dionne G. (1985). Patient mobility for elective surgical interventions. Social Science & Medicine, 20, 1307-1312. [DOI] [PubMed] [Google Scholar]
- Vandenbroucke J. P., Von Elm E., Altman D. G., Gøtzsche P. C., Mulrow C. D., Pocock S. J., . . . Egger M. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Annals of Internal Medicine, 147, W-163-W-194. [DOI] [PubMed] [Google Scholar]
- Varkevisser M., van der Geest S. A. (2007). Why do patients bypass the nearest hospital? An empirical analysis for orthopaedic care and neurosurgery in the Netherlands. European Journal of Health Economics, 8, 287-295. [DOI] [PubMed] [Google Scholar]
- Varkevisser M., van der Geest S. A., Schut F. T. (2010). Assessing hospital competition when prices don’t matter to patients: The use of time-elasticities. International Journal of Health Care Finance and Economics, 10, 43-60. [DOI] [PubMed] [Google Scholar]
- Varkevisser M., van der Geest S. A., Schut F. T. (2012). Do patients choose hospitals with high quality ratings? Empirical evidence from the market for angioplasty in the Netherlands. Journal of Health Economics, 31, 371-378. [DOI] [PubMed] [Google Scholar]
- Victoor A., Delnoij D. M., Friele R. D., Rademakers J. J. (2012). Determinants of patient choice of healthcare providers: A scoping review. BMC Health Services Research, 12, 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrangbæk K., Østergren K., Birk H. O., Winblad U. (2007). Patient reactions to hospital choice in Norway, Denmark, and Sweden. Health Economics, Policy and Law, 2, 125-152. [DOI] [PubMed] [Google Scholar]
- Vrangbæk K., Robertson R., Winblad U., Van de Bovenkamp H., Dixon A. (2012). Choice policies in Northern European health systems. Health Economics, Policy and Law, 7, 47-71. [DOI] [PubMed] [Google Scholar]