Abstract
Background
Stress caused by hospitalisations and transition periods can place patients at a heightened risk for adverse health outcomes. Additionally, hospitalisations and transitions to home may be experienced in different ways by families with different resources and support systems. Such differences may perpetuate postdischarge disparities.
Objective
We sought to determine, qualitatively, how the hospitalisation and transition experiences differed among families of varying socioeconomic status (SES).
Methods
Focus groups and individual interviews were held with caregivers of children recently discharged from a children's hospital. Sessions were stratified based on SES, determined by the percentage of individuals living below the federal poverty level in the census tract or neighbourhood in which the family lived. An open-ended, semistructured question guide was developed to assess the family's experience. Responses were systematically compared across two SES strata (tract poverty rate of <15% or ≥15%).
Results
A total of 61 caregivers who were 87% female and 46% non-white participated; 56% resided in census tracts with ≥15% of residents living in poverty (ie, low SES). Interrelated logistical (eg, disruption in-home life, ability to adhere to discharge instructions), emotional (eg, overwhelming and exhausting nature of the experience) and financial (eg, cost of transportation and meals, missed work) themes were identified. These themes, which were seen as key to the hospitalisation and transition experiences, were emphasised and described in qualitatively different ways across SES strata.
Conclusions
Families of lower SES may experience challenges and stress from hospitalisations and transitions in different ways than those of higher SES. Care delivery models and discharge planning that account for such challenges could facilitate smoother transitions that prevent adverse events and reduce disparities in the postdischarge period.
Trial registration number NCT02081846; Pre-results.
Introduction
Hospitalisations can be traumatic, stressful events for children, parents and families. Families must deal with the stress of an acute illness while also managing transitions into and out of the hospital.12 If stress is not effectively buffered, vulnerable patients and families will be at heightened risk for adverse postdischarge health outcomes, including readmissions and emergency department revisits.3–6 Such persistent stress can challenge a family's ability to navigate responsibilities related to postdischarge care (eg, medication administration and outpatient follow-up).7–10
These challenges may prove especially burdensome for families living in poverty.11 Qualitative studies of adult patients have detailed how the hospital-to-home transition is experienced differently for those of varying socioeconomic status (SES), how financial stressors, barriers to accessing follow-up care and limited health literacy can complicate recovery from acute illnesses.12–18 Such poor transitions and complicated recoveries that disproportionately affect those of low SES perpetuate existing socioeconomic disparities across a range of health outcomes.
Just as adult hospitalisations challenge patients and immediate family members, a child's hospitalisation represents challenges for parents and the entire family.19,20 This may be particularly true for those living in poverty and those without adequate support systems. To mitigate the stress of the hospitalisation and transition, interventions may benefit from taking family needs and contextual factors such as SES into account.21 Studies suggest that interventions are most likely to be successful if they directly address family-identified barriers and challenges to successful re-entry into daily routines and adherence to postdischarge care plans.4,22–28 Indeed, the family ‘voice’ could be a powerful addition to the design and delivery of interventions that aim to improve outcomes and reduce disparities. Therefore, we sought to determine, qualitatively, how the hospitalisation and hospital-to-home transition experiences differed between families of varying SES.
Methods
Study design
This was completed as part of the Hospital-to-Home Outcomes Study (H2O) at Cincinnati Children's Hospital Medical Center (CCHMC). H2O was designed to identify barriers to successful transitions as perceived by parents or caregivers and to use such knowledge in the design, implementation and evaluation of postdischarge nurse-led home visits.29,30 This qualitative study allowed us to gather and explain parents' experiences potentially affected by SES to more directly inform the structure and iterative adaptation of the intervention. The study was approved by the CCHMC Institutional Review Board.
Setting
CCHMC is Southwest Ohio's primary inpatient paediatric facility with ∼600 inpatient beds. Those living in CCHMC's primary service area are spread across diverse urban, suburban and rural neighbourhoods, with the percentage of individuals living below the federal poverty level ranging from 0% to 83%.31
Sample design
Parents or caregivers were eligible for participation if their child had been discharged from the hospital medicine or neurology/neurosurgery services in the preceding 30 days. We excluded non-English speaking parents, <3% of those otherwise eligible, as we did not have the resources to provide interpreter services during focus groups. Also, those with children eligible for in-home skilled nursing services (eg, intravenous therapy, tube feeding) were excluded, so as to focus on those admitted for self-limiting disease processes or acute manifestations of chronic conditions. Finally, participants were excluded if their child was hospitalised for a psychiatric diagnosis or was in the custody of the county or state.
To facilitate open communication,32,33 we employed a SES-stratified purposeful sampling design. We defined socioeconomic strata using the degree of poverty present in each participant's home census tract. We saw this neighbourhood-level indicator of poverty as being a useful approximation of social and environmental determinants of health (eg, housing stock, transportation access, exposure to crime). In the USA, census tracts are administrative geographical units that are structured and defined to be sociodemo-graphically homogenous. They are composed of ∼4000 individuals. Tracts were chosen as our geographical unit given their ability to parallel locally defined neighbourhood boundaries and their utility in detecting socioeconomic gradients in health outcomes.34–38
Home addresses for potentially eligible participants were obtained from the electronic health record and mapped to the potential participants' home census tract. The tract's corresponding poverty rate was determined using the data from the 2008–2012 US Census American Community Survey.31 We used the poverty rate, defined as the in-tract percentage of all individuals living below the federal poverty level, as a proxy of family SES. Before we started enrolment, we queried the electronic health record for historical patients who would potentially meet eligibility criteria. We determined the distribution of poverty rates within this group and used this distribution to identify tract-level poverty cut-points that would ensure a sufficient number of eligible focus group participants within each stratum. As such, ‘low SES' participants were defined as those living within tracts with ≥15% of the population living in poverty; ‘high SES’ participants were defined as those within tracts with <15% in poverty.
Data collection
Parents or caregivers were recruited and consented during their child's hospitalisation. Those who agreed to participate returned to CCHMC facilities for the focus group within 30 days of discharge. Focus groups were scheduled on weekdays, evenings and weekends. We provided childcare when needed; all participants received incentives for attending.
An open-ended semistructured question guide was developed de novo for use with all participants after a review of the literature and discussion with the multi-disciplinary H2O team.30 The intent of the guide was to direct an open-ended discussion around aspects of the inpatient experience, discharge/transition processes and health system and family factors. As data collection progressed, the question guide was refined to incorporate new issues raised. An experienced moderator used follow-up probes to clarify, expand and contextualise responses. All sessions were held in private conference rooms and lasted ∼90 min. Responses were audio-taped, transcribed verbatim and stored in an electronic database. Identifiers were removed and transcripts were reviewed for accuracy. After conducting 15 sessions—11 focus groups (generally 5–10 participants) and 4 interviews (when just one participant attended)––we determined that saturation was achieved.39,40
Data analysis
As a check on the use of area-level poverty as a way to stratify participants, we compared the two predefined SES groups with respect to available participant demographic characteristics (gender, categorised age, marital status and race/ethnicity) and self-reported socioeconomic factors (educational attainment and employment) using the χ2 or Fisher's exact test for categorical variables or the Wilcoxon rank-sum test for continuous variables. These data were collected by paper survey at the focus group or interview. Basic information about the participant's child was extracted from the electronic health record.
An inductive, thematic approach was then used for qualitative analyses.41,42 During multiple analytical rounds, transcripts were independently reviewed, discussed and coded by a team of two paediatricians, a clinical research coordinator and a qualitative methods expert to identify emerging themes. The diverse background of analysts added breadth and varied perspectives to the iterative analysis process. Regular team meetings ensured that alternative interpretations were voiced and consensus was reached in an unbiased manner. All findings, and interpretation of those findings, were reviewed with key stakeholders—parents, inpatient and outpatient paediatricians and nurses—with the goal of enhancing the credibility of our findings.40,41
The first phase of analysis, presented elsewhere, focused on recurring patterns of experiences highlighted by all participants.30 This second analytical phase then stratified the coded transcripts according to the group's SES. Coded quotes from the database representing all individuals in one SES grouping were reviewed, and group-specific content was identified. This process was then repeated in the other SES grouping. Findings were then juxtaposed, put side by side to highlight qualitative differences across the two groups using dual screen projection of the database. This allowed the analytical team to delineate subthe-matic content differences and differences in emphases across the SES subgroups.
Below, we provide verbatim quotes from participants. The proportion of quotes depicted for each identified theme reflects the emphasis given by participants in each of the low and high SES groups.
Results
Study participants Sixty-one parents or caregivers participated; 56% resided in areas defined as low SES (table 1). Those from low SES tracts were significantly more likely to be single (53% vs 15%), black/African-American (65% vs 11%) and have higher rates of high school non-completion (12% vs 0%) when compared with those from high SES tracts (all p≤0.01). The median census tract poverty rate in the low SES group was 30.3% (IQR 23.9 to 42.6) compared with 7.4% in the high SES group (IQR 3.4 to 11.4); p<0.0001.
Table 1. Participant demographic and socioeconomic characteristics stratified by their census tract's rate of poverty.
| Participant characteristic | Participants living in census tract with <15% of residents living in poverty N=27 (44%) N (%) | Participants living in census tract with ≥15% of residents living in poverty N=34 (56%) N (%) | p Value* |
|---|---|---|---|
| Gender | 0.7 | ||
| Male | 3 (11.1) | 5 (14.7) | |
| Female | 24 (88.9) | 29 (85.3) | |
| Age range (years) | 0.6 | ||
| 18–24 | 3 (11.1) | 2 (5.9) | |
| 25–34 | 11 (40.7) | 17 (50.0) | |
| 35–44 | 9 (33.3) | 13 (38.2) | |
| 45–54 | 4 (14.8) | 2 (5.9) | |
| Marital status | 0.01 | ||
| Single | 4 (14.8) | 18 (52.9) | |
| Single, living with partner | 4 (14.8) | 4 (11.8) | |
| Married | 16 (59.3) | 8 (23.5) | |
| Separated, divorced, widowed | 3 (11.1) | 4 (11.8) | |
| Race | <0.0001 | ||
| Black or | 3 (11.1) | 22 (64.7) | |
| African-American | |||
| White | 22 (81.5) | 10 (29.4) | |
| Multiracial/other | 2 (7.4) | 2 (5.9) | |
| Ethnicity | 0.5 | ||
| Non-Hispanic | 27 (100) | 32 (94.1) | |
| Hispanic | 0 (0) | 2 (5.9) | |
| Highest level of education completed | 0.003 | ||
| Less than high | 0 (0) | 4 (11.8) | |
| school | |||
| High school/GED | 10 (37.0) | 21 (61.8) | |
| 2-year college | 4 (14.8) | 7 (20.6) | |
| 4-year college or more | 13 (48.1) | 2 (5.9) | |
| Currently employed | 0.2 | ||
| No | 9 (33.3) | 19 (55.9) | |
| Full-time | 13 (48.1) | 10 (29.4) | |
| Part-time | 3 (11.1) | 5 (14.7) | |
| Missing | 2 (7.4) | 0 (0) | |
| Number of adults in the household | 0.001 | ||
| One | 4 (14.8) | 19 (55.9) | |
| Two | 22 (81.5) | 12 (35.3) | |
| Three or more | 1 (3.7) | 3 (8.8) | |
| Number of children in the household | 0.6 | ||
| One | 8 (29.6) | 11 (32.3) | |
| Two | 8 (29.6) | 7 (20.6) | |
| Three | 6 (22.2) | 5 (14.7) | |
| Four or more | 5 (18.5) | 11 (32.3) | |
p Values obtained using either the χ2 test or the Fisher's exact test. GED, General Educational Development Diploma.
Participants' children had a median age of 3.0 years (IQR 1.5 to 9.0) and were 54% male. The most common reasons for hospitalisation were asthma and bronchiolitis. There were no significant differences in child age, sex or diagnosis across SES groups.
Major themes
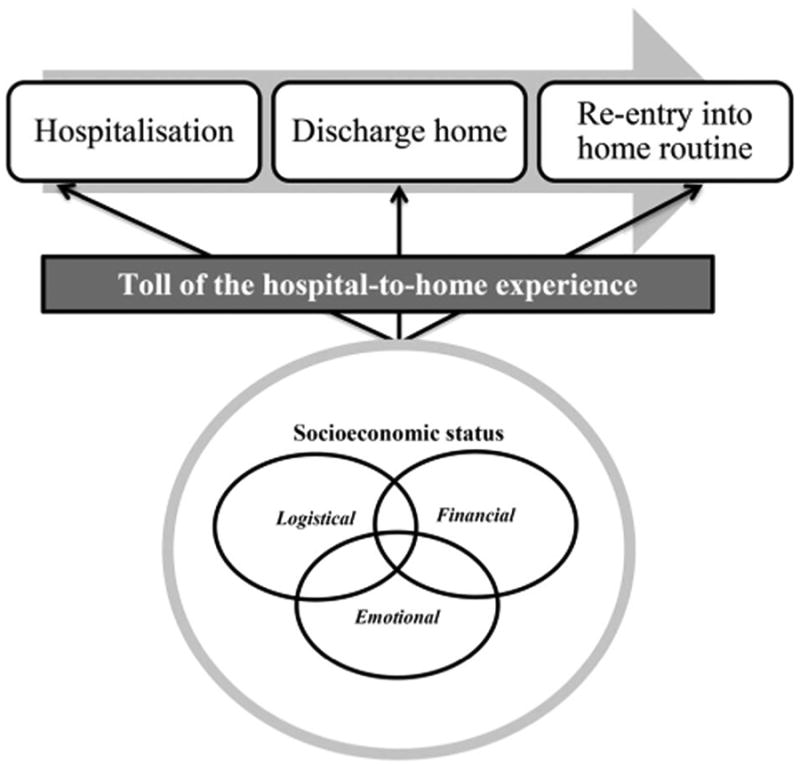
All participants highlighted stress that resulted from the hospitalisation and transition experiences. Many described this stress on them, their child and the family as ‘taking a hit’. Figure 1 illustrates a simplified conceptualisation of the relevance of this ‘hit’ to our specific period of interest—the hospitalisation and transition from hospital-to-home. We see each patient (and family) moving along a trajectory. This trajectory can be affected by the outpatient experience; it may also follow a non-linear path. For our purposes, however, we were most interested in the experience of the family, starting during the hospitalisation and extending to the transition home. We conceived the ‘toll of the hospital-to-home experience' to be affected, exacerbated or qualitatively modified by interrelated logistical, emotional and financial themes. The impact and characteristics of these themes can, in turn, be magnified or distorted by SES. The considerable qualitative variation in the experiences of families of varying SES within each of these themes is highlighted with quotes in the results and online supplementary tables (appendix).
Figure 1. Conceptual model for how a family's socioeconomic status modifies the hospital-to-home transition.
Logistical themes ‘No–leeway at all’
Low SES participants frequently cited a lack of available supports to cushion the blow dealt by the hospitalisation and the postdischarge periods (see online supplementary table S1). They highlighted an unease or inability, ‘I just can’t do it' (Mother, Session #14), regarding how they would maintain, or return to, their standard routine. Many were particularly concerned about juggling work, caring for their ill child and for their other children, with limited assistance from family or friends. Although many did receive help, this help often came at a cost with children missing school and family members missing work. One mother reported that:
My two daughters that go to school and my boyfriend going to work, it was hard. I had to send [the patient] with my mom and my grandma. [My other children] would miss school because they live in a completely different neighbourhood from the school… They were out of school for four days and then when I got home I had to catch up on the homework.
Mother, Session #12
Although this mother had supports, a lack of available support systems among low SES participants was a common refrain. Another parent noted:
We don't have any family. It's just [my partner], me and the kids, so we have to depend on each other to do the tasks and things.
Mother, Session #14
Related to this frequently cited lack of reliable supports, many also described barriers to accessing primary care clinics or pharmacies, barriers frequently related to insurance, transportation or appointment availability:
It takes me two to three weeks to get [an appointment at the clinic]… I only got like [sub-optimal] insurance… that's why I came to the emergency room.
Father, Session #8
These challenges accessing resources potentially precluded families from adequately adhering to the discharge instructions (and medications) prescribed by the inpatient team:
It takes about four hours [to get to pharmacy]… Two hours to get there walking and two hours to get back.
Mother, Session #14
Alternatively, high SES participants frequently described supports received from family, coworkers or friends, and the relative ease with which they could access postdischarge health services. This facilitated a more rapid perceived return to normalcy. Others noted their relief at coming home to a house kept ‘beautiful’ by family or friends, or at having colleagues or friends who were forthcoming with meals as they re-entered their home environment. They knew who to call and had ‘people’ who could quickly come to their aid:
I'm lucky; my mother lives [close]. So I was able to call her before we even got admitted and say, ‘He's being admitted to the hospital, so I need you to come down and help out'. My husband and I could split between the kids and she could be with our older son when both of us need to be here. We were able to make things work.
Mother, Session #7
It was very rare that high SES participants voiced challenges related to support systems or limited access to resources. Instead, the stress most commonly articulated related to uncertainties around timing of discharge and delays in discharge processes. Many described concerns over family schedules, challenges with having ‘five bags of laundry and… baseball games on Saturday' (Mother, Session #7), while trying to care for a still-recovering child. Nevertheless, trepidation with transition home was, generally, mitigated by existing support systems and relatively easy access to health-promoting resources. High SES participants never reported having issues with scheduling appointments or obtaining medications. Although some cited difficulty fitting follow-up clinic visits into their schedules, these same respondents also noted the flexibility of their primary care offices:
I did have one of the nurses say, ‘If you call your paediatrician's office, are you going to be able to get in within the next 48 hours? Is your office good about that?' And my response was, ‘Yeah, with a sick kid or a follow-up they’ll get you in the same day'. So I don't know what… if I had answered, ‘Oh no, it takes three weeks to get into my doctor’, how that might have been different?
Mother, Session #9
Emotional themes-‘It was really hard’
Participants from both SES levels reported feeling overwhelmed and exhausted as a result of their child's acute illness; yet, their emphases often differed (see online supplementary table S2). The varying support systems described above, and the relative frequency of social isolation among the low SES participants, often shaped how parents described their abilities to deal with the emotional ramifications of their child's hospitalisation.
Low SES participants often reported feeling alone. They voiced stress over maintaining order in their life and the lives of their children, difficulty in balancing their emotions, the illness of their child and other responsibilities:
Your child is sick, you're upset and… overwhelmed with everything. I mean I'm exhausted… because I'm always working.
Mother, Session #15
Another parent reiterated this concept, saying ‘I'm trying to keep my outside life going to be OK for my children’. (Mother, Session #12)
High SES participants also reported feeling stressed and exhausted. Still, many reported being able to fall back on existing support systems and networks that were often either stretched or absent for those of lower SES. Indeed, whereas discussion of social isolation was frequent within low SES groups, such discussion was essentially absent from higher SES groups. Instead, high SES participants tended to voice stress in terms of physical exhaustion and the mounting tasks or logistical issues described above, tasks that complicated participants' ability to handle the emotional ramifications of the hospitalisation and transition experiences:
I'm still doing laundry… I haven't cooked at home in two weeks… I'm so tired of fast food… But the kids are back on track and that's the main thing for me. I' ll eventually get there, but the kids got to get back.
Mother, Session #7
Another reported, ‘I was going to be hospitalized soon because I was so stressed out', (Mother, Session #9) a comment that had immediately followed this parent's description of the emotional ramifications of the shock of having an ill child and the mounting tasks present at home.
Financial themes-‘I was pretty plumbed out’
Participants across SES strata highlighted out-of-pocket expenses, even if insurance covered most medical costs. Expenses, however, seemed to particularly challenge those of low SES who emphasised occasionally insurmountable hospital costs, including that for food and transportation (see online supplementary table S3). They described not eating, or stealing food from their child's tray, for lack of money.
I was in the hospital with no money with no one, no food, no gas… It was just horrible because I was breastfeeding… and I'm basically eating nothing but cereal or a little scrap that [patient] don't eat that I could sneak in before the doctors come and see.
Mother, Session #8
Expenses were also often confronted in the context of lost wages. As a result, many had to make difficult decisions about how to spend limited resources:
My [husband] missed work… [It] affects our economy because I'm here and he is watching the kids… [Bills] pile up, and it hurts you.
Mother, Session #14
These worries related, for some, to their perceived readiness for discharge. Some expressed a desire to get out of the hospital as quickly as possible to enable a return to home and work. Others worried that leaving too soon would prompt subsequent health service utilisation and co-pays they could not afford:
I don't think the doctors realize the financial toll that the parents take. It's just, ‘OK, we're going to send you home; you can always come back if there's a problem’. Well, that's another $150 deductible from me to go to the [emergency room].
Father, Session #14
Although high SES participants similarly worried about postdischarge co-pays and missed work, the worries they voiced were frequently buffered by the presence of more resources. Many voiced secure, stable relationships with their employers, including flexibility with time off and the ability to work remotely:
[My employer] let us work from the hospital while we were here. I took a day [off], the day of his first day home.
Mother, Session #7
Although high SES participants did lament the cost of food or gas, no one said they went without something they needed due to financial worries. More commonly, they described having to get more fast food because of delays in discharge and disruptions to their home routines.
Discussion
Having a child hospitalised for an acute illness takes a considerable toll on patients, parents and families. We use the parent (or caregiver) voice to illustrate that SES, measured at the census tract level, qualitatively modifies how the period surrounding this event is experienced. We suggest that SES be taken into account if hospital-based and community-based interventions are to successfully support a family through a hospitalisation and the accompanying transition home in ways that improve outcomes and reduce disparities in those outcomes. Determining how interventions can be tailored to the varying logistical, emotional and financial needs of patients and families, across socioeconomic strata, is vital. The qualitative results presented here should prompt hypothesis generation, providing a framework onto which future interventions can be adapted or developed, implemented and evaluated.
Logistical themes centred upon support networks, domestic tasks and accessing health-promoting resources. Our findings are consistent with a previous work in geriatrics. Greysen et al15 described how low-income adults experience ‘missing pieces’ during transitions, often including limited support from family or friends. Families of injured children also reported how support systems, including peer support groups, helped reduce the burden imposed by the seemingly endless list of unfinished tasks (eg, caring for recovering child, errands); though, this latter study did not pursue their analyses in the context of SES.21 Transition-related interventions may be more effectively deployed if support systems are identified during the inpatient stay. Similarly, patients and families may benefit if SES-related differences in support systems are more clearly anticipated.22,43 Interventions, including home visitation, care coordination or concierge-type services (assistance with domestic task completion), may also help ease family-felt burdens and warrant further evaluation.29,44,45
Access to follow-up care is a fundamental component of family-centred transitions,24 but our findings suggest that such access, for some, can be limited. Our findings align with adult studies that highlight feelings of ‘abandonment’ at discharge, with many knowing that they would be unable to fill prescriptions or follow-up as instructed.14,17 This discontinuity in care across the transition is especially stark for vulnerable patients and families, placing many at heightened risk for suboptimal postdischarge outcomes that could widen already existing disparities.16 Thus, the care team may work with families to ensure that post-discharge plans can be realistically and effectively integrated into their routines.22,23 This may require changes in how family-level risk is assessed, ancillary staff (eg, home health nurses, social workers) are trained and postdischarge interventions are deployed.44 For example, if families have limited access to follow-up medical care or prescriptions, alternative means of resource provision could be considered (eg, home visitation, phone follow-up, transportation assistance and/or medication delivery).25,29,30 That being said, a common refrain across nearly all participants, regardless of SES, was the desire to balance the potential benefit of supports aimed at lingering stress with the hope to quickly return to normalcy.
In paediatrics, the roles of poverty and the social determinants of health are being increasingly recognised as vital to improving health outcomes, especially as disparities widen for many conditions.43,46–48 This has, in part, driven the recent focus on identifying and mitigating ‘toxic stressors’, defined as experiences that prompt prolonged activation of the physiological stress response in the absence of buffering supports.37,49 Perhaps, defining discharge readiness, and the postdischarge safety net, more broadly, in a way that takes family-level risks and assets into account, may smooth the transition home and prevent the stress of a hospitalisation from becoming ‘toxic’.6,37,50
Additional connections with buffering community-based mental health and/or social service resources may be considered as discharge plans are developed. Interventions related to these discharge plans (eg, medication delivery, transportation assistance, postdischarge phone calls or home visits) that take SES into account should be evaluated to determine their effect on health outcomes and on disparities.
Our qualitative findings also suggest that the financial ramifications of a child's illness are felt in unequal ways across families of varying SES. Indeed, the experience of the child's illness dealt a financial blow to many families' ‘economy’, particularly for those with limited resources.51 Low SES participants repeatedly expressed that concerns related to financial stressors magnified their worries about a child's illness. Such concerns were directly linked to their perceived ability to meet in-hospital and postdischarge needs, consistent with studies highlighting how low-income adult patients faced ‘competing issues and financial barriers’ to performing discharge instructions.17,52
Perhaps, easing the financial burden faced by low SES families by providing financial assistance with vouchers for meals, parking or transportation should be considered a component of preventive, family-centred care.
There were limitations to this study. First, our findings may not be generalisable to different types of hospitals in different regions or countries. For example, we have a relatively low percentage of non-English speakers (∼3% of otherwise eligible participants) who were excluded from this study. These families may have different experiences from native speakers. Still, those cared for at CCHMC are otherwise diverse demographically and clinically. Second, participants may have been self-selective in who came to our sessions (selection bias). Yet, the demographic characteristics and the distribution of diagnoses of participants align closely to those hospitalised at CCHMC. Third, census tract poverty rates may not accurately reflect the reality felt by participants; dichotomisation at 15% may also limit the variability uncovered. Fourth, there is the possibility of participant recall bias. We attempted to minimise this potential limitation by holding sessions within 30 days of hospital discharge. Finally, although not itself a limitation, qualitative methods do not allow us to directly assess causality between SES and specific outcomes. Instead, these methods are hypothesis-generating, providing a framework on which future studies and interventions can be developed, implemented and evaluated.
Conclusions
Our findings suggest that SES influences hospitalisa-tion and transition experiences. Healthcare providers, hospitals and payers that account for SES may more effectively integrate medical plans into realities faced by families as they transition from hospital back to home, improving outcomes and reducing disparities.
Supplementary Material
Acknowledgments
Funding National Institute of Allergy and Infectious Diseases (1K23AI112916). Patient-Centered Outcomes Research Institute (HIS-1306-0081).
Footnotes
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/bmjqs-2016-005421)
Collaborators H2O study group members Katherine A Auger, MD, MSc; Stephanie A Brunswick, BS; JoAnne Bachus, BSN; Kathleen Bell, BA; Monica L Borell, BSN; Lenisa Chang, MA, PhD; Judy A Heilman, RN; Joseph Jabour, BA; Jane C Khoury, PhD; Logan Maag, BA; Margo J Moore, BSN, CCRP; Cory Pfefferman, BA; Rita H Pickler, RN, PNP, PhD; Anita N Shah, DO; Angela M Statile, MD, MEd; Heidi J Sucharew, PhD; Karen P Sullivan, BSN; Hadley S Sauers-Ford, MPH; Samir S Shah, MD, MSCE; Susan N Sherman, DPA; Jeffrey M Simmons, MD, MSc; Lauren G Solan, MD, MEd; Heather LTubbs-Cooley, RN, PhD; Susan Wade-Murphy, MSN and Christine M White, MD, MAT.
Contributors AFB, LGS, SAB and SNS participated in the conceptualisation and design of the study, designed the question guide, participated in data collection, reviewed audio transcripts for accuracy, analysed the data, drafted the initial manuscript and approved the final manuscript as submitted. HS-F, JMS, SS and JG conceptualised and designed the study, participated in final data analysis, critically reviewed the manuscript and approved the final manuscript as submitted. The H2O study group members listed also conceptualised and designed the study, participated in final data analysis and approved the final manuscript as submitted.
Competing interests None declared. Ethics approval Cincinnati Children's Hospital Medical Center Institutional Review Board. Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Current data available to H2O study group members (approved through the Cincinnati Children's Hospital Medical Center Institutional Review Board) include the coded dataset of the focus groups that were completed.
References
- 1.Diaz-Caneja A, Gledhill J, Weaver T, et al. A child's admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med. 2005;31:1248–54. doi: 10.1007/s00134-005-2728-8. [DOI] [PubMed] [Google Scholar]
- 2.Lerret SM, Weiss ME, Stendahl G, et al. Transition from hospital to home following pediatric solid organ transplant: qualitative findings of parent experience. Pediatr Transplant. 2014;18:527–37. doi: 10.1111/petr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berry JG, Ziniel SI, Freeman L, et al. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013;25:573–81. doi: 10.1093/intqhc/mzt051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309:372–80. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311:2169–70. doi: 10.1001/jama.2014.3695. [DOI] [PubMed] [Google Scholar]
- 7.Kaushal R, Jaggi T, Walsh K, et al. Pediatric medication errors: what do we know? What gaps remain? Ambul Pediatr. 2004;4:73–81. doi: 10.1367/1539-4409(2004)004<0073:pmewdw>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 8.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–20. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 9.Ruth JL, Geskey JM, Shaffer ML, et al. Evaluating communication between pediatric primary care physicians and hospitalists. Clin Pediatr (Phila) 2011;50:923–8. doi: 10.1177/0009922811407179. [DOI] [PubMed] [Google Scholar]
- 10.Johnson JK, Farnan JM, Barach P, et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21(Suppl 1):i97–105. doi: 10.1136/bmjqs-2012-001215. [DOI] [PubMed] [Google Scholar]
- 11.Smith LA, Bokhour B, Hohman KH, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–9. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 12.Kangovi S, Levy K, Barg FK, et al. Perspectives of older adults of low socioeconomic status on the post-hospital transition. J Health Care Poor Underserved. 2014;25:746–56. doi: 10.1353/hpu.2014.0111. [DOI] [PubMed] [Google Scholar]
- 13.Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med. 2014;29:283–9. doi: 10.1007/s11606-013-2571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cain CH, Neuwirth E, Bellows J, et al. Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7:382–7. doi: 10.1002/jhm.1918. [DOI] [PubMed] [Google Scholar]
- 15.Greysen SR, Hoi-Cheung D, Garcia V, et al. ‘Missing pieces’— functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. 2014;62:1556–61. doi: 10.1111/jgs.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Groene RO, Orrego C, Suñol R, et al. ‘It's like two worlds apart’: an analysis of vulnerable patient handover practices at discharge from hospital. BMJ Qual Saf. 2012;21(Suppl 1):i67–75. doi: 10.1136/bmjqs-2012-001174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernheim SM, Ross JS. Hospital discharge and the transition home for poor patients: ‘I knew I couldn't do what they were asking me’. J Gen Intern Med. 2014;29:269–70. doi: 10.1007/s11606-013-2698-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foust JB, Vuckovic N, Henriquez E. Hospital to home health care transition: patient, caregiver, and clinician perspectives. West J Nurs Res. 2012;34:194–212. doi: 10.1177/0193945911400448. [DOI] [PubMed] [Google Scholar]
- 19.Fowlie PW, McHaffie H. Supporting parents in the neonatal unit. BMJ. 2004;329:1336–8. doi: 10.1136/bmj.329.7478.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss M, Johnson NL, Malin S, et al. Readiness for discharge in parents of hospitalized children. J Pediatr Nurs. 2008;23:282–95. doi: 10.1016/j.pedn.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Aitken ME, Mele N, Barrett KW. Recovery of injured children: parent perspectives on family needs. Arch Phys Med Rehabil. 2004;85:567–73. doi: 10.1016/j.apmr.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 22.Faultner J. Integrating medical plans within family life. JAMA Pediatr. 2014;168:891–2. doi: 10.1001/jamapediatrics.2014.1031. [DOI] [PubMed] [Google Scholar]
- 23.Apkon M, Friedman JN. Planning for effective hospital discharge. JAMA Pediatr. 2014;168:890–1. doi: 10.1001/jamapediatrics.2014.1028. [DOI] [PubMed] [Google Scholar]
- 24.Desai AD, Popalisky J, Simon TD, et al. The Effectiveness of family-centered transition processes from hospital settings to home: a review of the literature. Hosp Pediatr. 2015;5:219–31. doi: 10.1542/hpeds.2014-0097. [DOI] [PubMed] [Google Scholar]
- 25.Berry JG, Blaine K, Rogers J, et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168:955–62. doi: 10.1001/jamapediatrics.2014.891. quiz 65-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith L, Daughtrey H. Weaving the seamless web of care: an analysis of parents' perceptions of their needs following discharge of their child from hospital. J Adv Nurs. 2000;31:812–20. doi: 10.1046/j.1365-2648.2000.01339.x. [DOI] [PubMed] [Google Scholar]
- 27.Worthington RC. Effective transitions for families: life beyond the hospital. Pediatr Nurs. 1995;21:86–7. [PubMed] [Google Scholar]
- 28.Lerret SM. Discharge readiness: an integrative review focusing on discharge following pediatric hospitalization. J Spec Pediatr Nurs. 2009;14:245–55. doi: 10.1111/j.1744-6155.2009.00205.x. [DOI] [PubMed] [Google Scholar]
- 29.Tubbs-Cooley HL, Pickler RH, Simmons JM, et al. Testing a post-discharge nurse-led transitional home visit in acute care pediatrics: the Hospital-To-Home Outcomes (H2O) study protocol. J Adv Nurs. 2016;72:915–25. doi: 10.1111/jan.12882. [DOI] [PubMed] [Google Scholar]
- 30.Solan LG, Beck AF, Brunswick SA, et al. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136:e1539–49. doi: 10.1542/peds.2015-2098. [DOI] [PubMed] [Google Scholar]
- 31.American Factfinder. US Census Bureau. 2014. [accessed 25 May 2015];2015 http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- 32.Crabtree BF, Miller WL. Doing qualitative research. 2nd. xvii. Thousand Oaks, CA: Sage Publications; 1999. p. 406. [Google Scholar]
- 33.Stewart D, Shamdasani P, Rook D. Focus groups: theory and practice. 2nd. Thousand Oaks, CA: SAGE; 2007. [Google Scholar]
- 34.Krieger N, Chen JT, Waterman PD, et al. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95:312–23. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? inequalities: the Public Health Disparities Geocoding Project. Am J Epidemiology. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 36.Krieger N, Waterman P, Chen JT, et al. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas—the Public Health Disparities Geocoding Project. Am J Public Health. 2002;92:1100–2. doi: 10.2105/ajph.92.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shonkoff JP, Garner AS Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 38.Beck AF, Simmons JM, Huang B, et al. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102:2308–14. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuzel A. In: Doing qualitative research. 2nd. Crabtree BF, Miller WL, editors. xvii. Thousand Oaks, CA: Sage Publications; 1999. p. 406p. [Google Scholar]
- 40.Patton MQ, Patton MQ. Qualitative research and evaluation methods. 3rd. xxiv. Thousand Oaks, CA: Sage Publications; 2002. pp. 598–65. [Google Scholar]
- 41.Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: a methods sourcebook. 3rd. xxiii. Thousand Oaks, CA: Sage Publications, Inc; 2014. p. 381. [Google Scholar]
- 42.Guest G, MacQueen KM, Namey EE. Applied thematic analysis. xx. Los Angeles: Sage Publications; 2012. p. 295. [Google Scholar]
- 43.Council on Community Pediatrics. Poverty and Child Health in the United States. Pediatrics. 2016;137(ii):e20160339. doi: 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- 44.Monterio C, Arnold J, Locke S, et al. Social workers as care coordinators: leaders in ensuring effective, compassionate care. Soc Work Health Care. 2016;55:195–213. doi: 10.1080/00981389.2015.1093579. [DOI] [PubMed] [Google Scholar]
- 45.Naber MK, Joseph E. Providing customized services Concierge services put patients' and employees' minds at ease. Healthc Exec. 2007;22:40–1. [PubMed] [Google Scholar]
- 46.Fierman AH, Beck AF, Chung EK, et al. Redesigning health care practices to address childhood poverty. Acad Pediatr. 2016;16(3 Suppl):S136–46. doi: 10.1016/j.acap.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132:e1592–601. doi: 10.1542/peds.2013-0619. [DOI] [PubMed] [Google Scholar]
- 48.Shackleton N, Hale D, Viner RM. Trends and socioeconomic disparities in preadolescent's health in the UK: evidence from two birth cohorts 32 years apart. J Epidemiol Community Health. 2016;70:140–6. doi: 10.1136/jech-2015-205603. [DOI] [PubMed] [Google Scholar]
- 49.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–9. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 50.Shah AN, Jerardi KE, Auger KA et al. Can Hospitalization Precipitate Toxic Stress? Pediatrics. 2016;137(ii):e20160204. doi: 10.1542/peds.2016-0204. [DOI] [PubMed] [Google Scholar]
- 51.Callery P Paying to participate: financial, social and personal costs to parents of involvement in their children's care in hospital. J Adv Nurs. 1997;25:746–52. doi: 10.1046/j.1365-2648.1997.t01-1-1997025746.x. [DOI] [PubMed] [Google Scholar]
- 52.Kangovi S, Grande D, Meehan P, et al. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709–12. doi: 10.1002/jhm.1966. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


