Abstract
Objective
To assess the cost of adopting a plant-based diet.
Methods
Breast cancer survivors randomized to dietary intervention (n=1109) or comparison (n=1145) group; baseline and 12-month data on diet and grocery costs.
Results
At baseline, both groups reported similar food costs and dietary intake. At 12 months, only the intervention group changed their diet (vegetable-fruit:6.3 to 8.9 serv/d.; fiber: 21.6 to 29.8 g/d; fat: 28.2 to 22.3% of E). The intervention change was associated with a significant increase of $1.22/person/week (multivariate model, p=0.027).
Conclusions
A major change to a plant-based diet was associated with a minimal increase in grocery costs.
Keywords: breast cancer, fruit-vegetable consumption, grocery costs
A healthy dietary pattern is well recognized as a potentially useful strategy in the prevention of chronic disease.1 However, only about 5% of Americans have dietary patterns that adhere to the vegetable, fruit or dietary fat recommendations of the Healthy People 2010 dietary guidelines. USDHHS, 2000 #261 Numerous studies have developed interventions to help people adopt and adhere to recommended intakes of vegetables, fruits, fiber and energy from fat, although the majority have been unable to sustain changes in the longer term.2 The following key barriers to adherence have been identified: food taste, convenience, perceived nutritional value, and perceived costs, specifically perceived greater food costs associated with increased fruit and vegetable intake.3–5
Multiple observational studies relying on survey data have reported that people who purchase more vegetables and fruit have higher overall grocery expenditures, but they tend to be of higher socio-economic status as well, which may confound this association.6–9 In ecologic-level analyses, energy-dense diets, typically low in vegetable-fruit intake, are considered to be less expensive on a per-calorie basis.10 A recent focus group study conducted among African American, Hispanic, and Caucasian men and women in the United States concluded that perceived high-cost and high-spoilage rates of fruits and vegetables deterred many participants from trying to meet dietary recommendations.11 Yet, data from the US Department of Agriculture on actual costs of eating healthy, independent of socio-economic status, suggest that an intake of 7 servings of vegetables and fruits per day (n = 7,195 homes) was associated with an average cost of only 64 cents/person per day.12 In the most relevant examination of this question, 20 families who increased the nutrient density of their diets showed no statistically significant increase in costs per calorie, although the analysis used local grocery store prices as a proxy for actual grocery expenditures.13 This suggests that higher costs may be more a perceived barrier rather than necessarily reflecting what will happen with major dietary change.
Some studies suggest that economic incentives, such as coupons, may be necessary to overcome the barrier of perceived higher costs to increasing vegetable and fruit intake.14, 15 In this paper we present prospective data from the Women’s Healthy Eating and Living (WHEL) Study, a large, randomized, controlled trial of whether adopting a plant-based dietary pattern would improve prognosis among women previously diagnosed with early stage breast cancer. Rather than use economic incentives as the main motivator for participants to make and maintain such a dietary change, an intensive one-on-one intervention delivered by lay counselors over the telephone emphasized overcoming barriers to health behavior change. We report on the dietary changes achieved with this intervention approach and their impact on the participants’ estimate of grocery costs over a 12-month period.
METHODS
Study Design and Population
Between 1995 and 2000, the Women’s Healthy Eating and Living (WHEL) Study randomized 3088 women diagnosed with early stage breast cancer within the previous 4 years to either a diet intervention or comparison group.16 Eligibility criteria included diagnosis of a primary operable invasive breast carcinoma categorized using American Joint Committee on Cancer (edition IV) criteria as stage I (≥1 cm), stage II, or stage IIIA within the past 4 years; age at diagnosis between 18 and 70 years; treatment with axillary dissection and total mastectomy or lumpectomy followed by primary breast radiation; no current or planned chemotherapy; no evidence of recurrent disease or new breast cancer since completion of initial local treatment; and no other cancer in the past 10 years. Participants were recruited at seven sites located in Arizona, California, Oregon and Texas.
The intervention group was asked to consume a daily intake of 5 vegetable servings, 2 cups (473 mL) of 100% vegetable juice, 3 fruit servings, 30 g of fiber, and 15–20% energy from fat, while the comparison group was advised to follow the 5-A-Day diet.17, 18 The study anticipated that vegetable juice consumption would be the most challenging goal for most participants. Accordingly, to reduce barriers to adherence and provide options beyond purchasing fresh vegetable juice, which is expensive, the study bulk-purchased juice extractors and offered them to participants at a 25% discount over wholesale cost. However, the study did not offer coupons or any economic incentive to purchase food. Participant-centered counseling delivered over the telephone helped intervention participants maximize their dietary change.19 This study was approved by the Institutional Review Boards at all participating centers including University of California San Diego, University of California Davis, Stanford University/University of California, San Francisco, The University of Arizona, MD Anderson Cancer Center, Kaiser Permanente Northern California, and the Center for Health Research, Portland, Oregon.
Data Collection
This report examines data collected at baseline and 12 months in the WHEL Study. At these timepoints, dietary intake was assessed on 94% of WHEL participants, and 85% of participants attended clinic visits (attendance was equivalent for intervention and comparison group participants). Before clinic visits, participants were mailed a series of questionnaires to complete and hand in when they attended the clinic. One questionnaire focused on patterns of food purchasing, preparation, and meal consumption including meals eaten at restaurants or take-out. Approximately 80% of the sample attended the 12-month clinic visit and this questionnaire was completed at baseline and 12 months for 72% of the intervention group and 74% of the comparison group participants. This report considers the 2254 women who had dietary intake and cost data at both baseline and 12 months.
Dietary Assessment
The study used three separate measures to assess dietary intake: a set of 24-hour dietary recalls, a food frequency questionnaire, and plasma carotenoid concentrations, a recognized biomarker of vegetable and fruit intake.20 Using change in the biomarker of carotenoids as the gold standard, carotenoid assessment from the 24-hour dietary recall had a higher validity (0.44) than the FFQ (0.39) as well as less systematic error (28% vs 50%).21 Thus, our 24 hour recall methodology is our self-report measure of choice. In the full study population, we have reported that the study intervention was associated with a 65% increase in vegetable and fruit intake 22 and this change was validated with a 51% increase in plasma carotenoid concentrations.20
Four 24-hour dietary recalls were collected by telephone over a 3-week period before a participant’s randomization (baseline) and again at 12 months; these recalls followed a standard protocol using trained dietary assessors who were blinded to diet group assignment and were not involved in the dietary counseling. The multi-pass Minnesota Nutrition Data System software was used for dietary data collection and for estimating nutrient intakes (NDS version 4.01, 2001, University of Minnesota, Minneapolis MN). Using the NDS database, we calculated serving sizes using metric weight, including all forms of vegetables and fruits (frozen, canned, fresh, or dried). We defined a vegetable serving as ½ cup of cut-up vegetables (90 g), 1 cup of raw leafy green vegetables (55 g); a fruit serving as ¼ cup of dried fruit (60 g), ½ cup of cut-up fruit (120 g); 1 cup melon (165 g), or 1 medium piece of fruit (120 g). We report 100% vegetable and fruit juices separately as total fluid ounces.
Grocery Costs Assessment
A feasibility study examining participants’ collection of grocery store receipts identified significant data gaps. Nearly all participants were the primary food purchaser in their household and were confident that they could estimate how much they spent. Accordingly, we developed questions that asked participants to provide an overall assessment of their household grocery costs as part of a food purchasing and preparation questionnaire that was self-completed and collected at clinic visits. The following two questions were used to estimate per person grocery expenditures: “For how many people is food purchased in your household?” and “Approximately how much does your household spend on grocery purchases each week?” Interpretation of these questions was left open to respondents and the questionnaire did not query information on food stamp use, coupon use, or food pantry use. Weekly per person grocery costs were then obtained by dividing the weekly amount spent on groceries by the number of people in the household for whom food was purchased; we imputed 7 missing values for the number of people in the household at 12 months (3 from intervention and 4 from comparison) using baseline values.
To determine the number of meals per week for which groceries were purchased, i.e., meals prepared at home, participants were asked to indicate both the number of weekdays and weekend days they (a) ate breakfast at home, (b) prepared or ate lunch at home, and (c) prepared dinner at home.
Measurement of Other Variables
At the baseline and 12-month clinic visit, height and weight were measured using standard research procedures.16 BMI was calculated as weight (kg)/height (m2). Current physical activity was estimated using a brief self-reported personal habits questionnaire developed for the Women’s Health Initiative23 and validated for this study.24 Other variables including age, education, race/ethnicity, were ascertained at enrollment using a general demographic questionnaire. Stage of breast cancer was collected from medical record review.
Statistical Analysis
Chi-square tests, Student’s t-tests or Wilcoxon Rank Sum tests were used to establish the comparability of the study groups in demographic, clinical, and diet-related characteristics at baseline. Paired and two-sample t-tests (or Wilcoxon Rank Sum tests) were used respectively to examine within- and between-group baseline to 12-month changes in diet and food costs.
Multiple linear regression models were used to test between-group differences in grocery costs at 12-months, after adjusting for potential confounders including initial cost (baseline), number of meals eaten or prepared at home per week at 12 months, education, clinical site, age at randomization, race/ethnicity, 12-month BMI, and physical activity level. The outcome was log-transformed to ensure the residuals followed a normal distribution with a constant variance; Cook’s distance was also plotted for outlier detection. Prior to transformation the variance of the residuals increased with fitted values of the outcome. Log-transforming the outcome stabilized the variance. All analyses were performed using R, version 2.5.1 (http://www.R-project.org).
RESULTS
Breast cancer survivors with complete grocery costs data were comparable to the overall WHEL Study population.16 The majority were non-Hispanic white females (86.3%), middle-aged (mean 53.8 years), well-educated (55.4% with a college degree) and overweight (56.2% with BMI>25.0) (Table 1). The intervention (n=1109) and comparison groups (n=1145) did not differ on the severity of their original breast cancer (not shown). Nor did they differ significantly at baseline on demographic characteristics or level of physical activity, household size or number of meals eaten and prepared at home each week (mean 14.4 ± 4.4 (SD) meals/wk) or weekly grocery expenditures at baseline (I= $39.70± $24.60 versus C= $39.70 ± $20.30; p=0.98).
Table 1.
Comparability of WHEL Study groups at baseline
| Baseline | P-valuea | ||||
|---|---|---|---|---|---|
| Intervention Group (N =1109) | Comparison Group (N =1145) | ||||
| N | % | N | % | ||
| Race/ethnicity | |||||
| Non-Hispanic White | 956 | 86.2 | 990 | 86.5 | 0.91 |
| Other | 153 | 13.8 | 155 | 13.5 | |
| Education level | |||||
| No college degree | 483 | 43.6 | 522 | 45.6 | 0.35 |
| College degree | 626 | 56.4 | 623 | 54.4 | |
| Age at randomization (years) | |||||
| MEAN (SD) | 1109 | 54.0 (8.8) | 1145 | 53.6(8.9) | 0.25 |
| Body Mass Indexb (kg/m2) | |||||
| 17.5 – 24.9 (normal + underweight)c | 475 | 42.8 | 512 | 44.7 | 0.56 |
| 25.0 – 29.9 (overweight) | 347 | 31.3 | 357 | 31.2 | |
| 30.0 – 52.5 (obese) | 287 | 25.9 | 276 | 24.1 | |
| Physical activity,d N(%) | |||||
| < 300 | 313 | 28.6 | 320 | 28.7 | 0.89 |
| 300 – 900 | 362 | 33.1 | 361 | 32.2 | |
| 901 – 6420 | 418 | 38.2 | 438 | 39.1 | |
| Household occupancy | |||||
| MEAN (SD) | 1109 | 2.5 (1.2) | 1145 | 2.4 (1.1) | 0.33 |
| Number of meals eaten/prepared at home (per week) | |||||
| MEAN (SD) | 1109 | 14.4 (4.5) | 1145 | 14.3 (4.4) | 0.63 |
| Weekly food cost per person at baseline | |||||
| MEANe | 1109 | $39.70 | 1145 | $39.70 | 0.98 |
Chi-square and independent t-test p-values. No significant differences between intervention and comparison groups were found.
Cut-off points defined by USDHHS34
Normal = 18.5 – 24.9, underweight ≤18.5
Measured in metabolic equivalents (METs)
SD for intervention group was $20.30 and $24.60 for comparison group
As shown in Table 2, baseline consumption of vegetables and fruit did not differ significantly between the intervention and comparison groups (mean servings/d for intervention and comparison, respectively: 6.3, SD 3.0 versus 6.2, SD 2.8, p=0.29. Over half of all women (63.9%), regardless of randomization group (p=0.58), consumed at least 5 servings of vegetables and fruit a day. At 12 months, participants in the intervention group increased their daily servings of vegetables and fruit, on average, to 8.9 (SD 3.4), for an increase of 2.5 (SD 3.2) servings per person per day from baseline levels (p<0.001). Conversely, the comparison group showed no significant change in intakes of vegetables and fruit over the same time period. Women in the comparison group averaged 6.3 (SD 2.8) daily servings, for an average per person increase of 0.12 (SD; 2.6; p=0.11). Total vegetable and fruit intake in this analytical cohort of study participants reporting grocery cost data as compared to the total WHEL cohort showed no significant difference in mean consumption of these foods (data not shown) at baseline.
Table 2.
Comparison of baseline and 12-month total vegetable and fruit servings, percentage of daily calories from fat, total daily fiber, and weekly food cost per person by study group
| Intervention | Comparison | |||||
|---|---|---|---|---|---|---|
| Baseline (mean, SD) | Month 12 (mean, SD) | Pa | Baseline (mean, SD) | Month 12 (mean, SD) | Pa | |
| Total vegetable/fruit servings/day | 6.3 (3.0) | 8.9 (3.4) | <0.0001 | 6.2 (2.8) | 6.3 (2.8) | 0.11 |
| Daily juice consumption (ounces) | 4.0 (4.6) | 12.4 (7.0) | <0.0001 | 4.2 (4.8) | 4.1 (4.70) | 0.46 |
| Percentage of calories from fat | 28.2 (7.1) | 22.3 (7.1) | <0.0001 | 28.5 (6.8) | 28.2 (7) | 0.20 |
| Total daily fiber intake (g) | 21.6 (8.5) | 29.8 (10.2) | <0.0001 | 21.5 (8.1) | 21.5 (8.3) | 0.82 |
| Total daily caloric intake (kcal) | 1721.72 (385.55) | 1617.49 (347.73) | <0.0001 | 1742.39 (410.29) | 1620.96 (390.56) | <0.0001 |
| Food cost per person per week | 39.7 ($24.6) | 43.2 ($21.5) | <0.0001 | 39.7 ($20.3) | 42.1 ($20.5) | <0.0001 |
p-values testing if there is a significant change from baseline to month 12 within each group based on paired t-tests
Comparison of juice consumption showed similar patterns. Baseline consumption did not differ by group (overall mean (SD): 4.14 (4.71) ounces, p=0.35), but after 12 months the mean (SD) consumption in the intervention group was 12.36 (7.04) ounces daily (mainly vegetable) versus 4.13 (4.70) ounces in the comparison group (p<0.001).
Both study arms had comparable caloric intake at baseline (1721 vs 1742 kcals, p=0.22 ). While the dietary assessment indicated lower caloric intake at 12 months, the decrease was similar in both groups so that there was no significant difference between study groups at 12 months (I=1617, C=1621, p=0.83). At baseline, percentage of energy intake from fat did not differ between groups, with the study sample reporting an average of 28.4 (SD: 7.0) percent of energy from fat. At baseline, 58.8% of participants in each group consumed the generally recommended level of <30% total energy intake from fat, but after 12 months, 86.2% in the intervention group met these guidelines, compared to 60.6% in the comparison group (p<0.001). At 12 months, the intervention group reduced their mean percent energy intake from fat by 5.8 percentage points versus average 0.3 percentage point reduction in the comparison group, with mean percent energy intake from fat of 22.3 (SD : 7.1) and 28.2 (SD: 7.0), respectively (p<0.001).
Fiber intake also did not differ significantly across study groups at baseline, with an overall average daily intake of 21.6 g (SD: 8.3, p=0.80). However, by 12 months the intervention group significantly increased (p < 0.0001) their mean daily total fiber intake by 8.1 g to 29.8 g (SD: 10.2) compared to no increase for the comparison group (21.5 g, SD: 8.3).
To validate reported intakes of vegetables and fruit, plasma carotenoids, lutein, beta-cryptoxanthin, lycopene, alpha-carotene and beta-carotene) were compared at baseline and 12 months. Carotenoid concentrations were equivalent across groups at baseline, and increased 51% (p<0.001) by 12 months in the intervention group only (not shown).
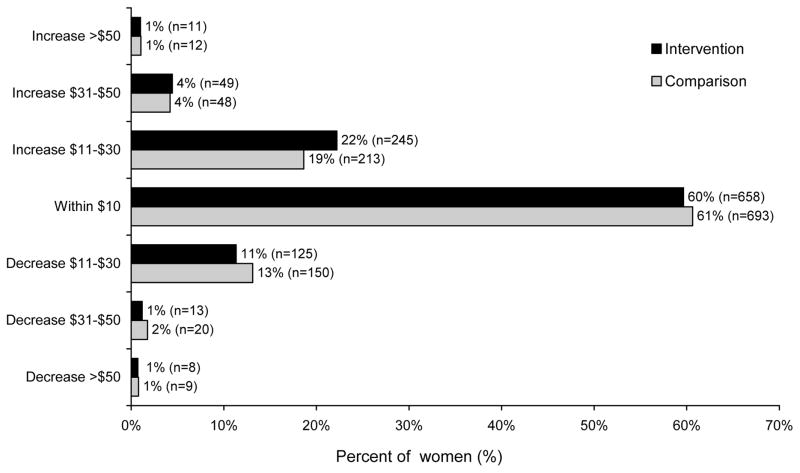
At 12 months, intervention group participants reported spending a mean of $43.24 [SD $21.53] on groceries compared to the comparison group mean of $42.05 [SD $20.45]. This difference of $1.22 in the increase in reported grocery costs was statistically significant (I=$3.55, SD: $23.55, C=$2.33, SD: $18.70, p=0.007). We categorized the change in grocery costs per participant and present the proportion of each group in each of these categories (Figure 1). The majority of participants (~60%) in both groups reported a similar expenditure on grocery costs at both points in time (within $10). The significant difference between the groups can be seen in the proportion with an $11–30 difference on the second survey compared to baseline. An increase of this amount occurred with 22% of the intervention and 19% of the comparison group and a decrease of this amount occurred with 11% of the intervention and 13% of the comparison group.
Figure 1.
Change in food costs from baseline to month 12, by group.1
However, while there was no between-group change in the size of households over this time period (p=0.74), adherence to the study dietary pattern was associated with the intervention group significantly increasing the number of meals they prepared at home (I=+1.04, SD 3.7; C=+0.4 SD 3.8, p=0.001). In a regression model, we adjusted for baseline grocery costs, clinical site, age at randomization, race/ethnicity, education, 12-month values of the number of meals eaten or prepared at home, BMI, and physical activity (Table 3). A Cook’s distance plot identified four potentially influential observations. Excluding these outliers did not change the results. Accordingly, the final model included all available data. After controlling for other variables, the 12-month weekly per person grocery cost was 3.6% greater in the intervention group than in the comparison group (3.6%; 95 % CI: 0.4–6.8%; p=0.027).
Table 3.
Linear regression modeling of grocery cost per person (log transformed) at 12 months for WHEL Study participants
| Model 1a | (log) Grocery Cost (SE) | p-value |
|---|---|---|
| Group difference (intervention vs. comparison) | 0.037 (0.016)c | 0.018 |
| Baseline grocery costs (log) | 0.613 (0.017) | <0.0001 |
|
| ||
| Model 2b | (log) Grocery Cost (SE) | p-value |
|
| ||
| Group difference (intervention vs comparison) | 0.035 (0.016)c | 0.027 |
| Baseline grocery costs (log) | 0.59 (0.018) | <0.0001 |
| Meals prepared at home (at 12 months) | −0.001 (0.002) | 0.487 |
Adjusted for baseline grocery costs only; adjusted R2for the model =0.37
Further adjusted for meals prepared at home at month 12, level of education, clinical site, age at randomization, race and 12-month measures of body mass index and physical activity (in metabolic equivalents); adjusted R2for the model =0.39
After exponentiation, the estimates in Model 1 became exp (0.037) = 1.038, (i.e., 3.8% higher costs in the intervention group) and the estimates in Model 2 became exp (0.035) = 1.036 (i.e. 3.6% higher cost in the intervention group)
DISCUSSION
The WHEL Study intervention was successful in encouraging participants to adopt a plant-based dietary pattern while dietary intake in the comparison was relatively unchanged. The intervention group increased daily intake of vegetables and fruit by 2.5 servings, reduced energy from fat by almost 6%, increased fiber intake by 8.1 g, and added an additional 8 ounces of juice. This dramatic dietary change was associated with an estimated increase of just over $1/week in grocery costs per person. Given the very large study sample, this additional cost was statistically significant, however, this small amount would be unlikely to discourage shoppers from purchasing healthier options like vegetables and fruits.
This study uses self-reported dietary intake from the sets of four 24-hour dietary recalls collected by telephone. However, the study also collected dietary data using a food frequency questionnaire. As self-reported dietary data are known to be prone to both random and systematic measurement error21, 25, the WHEL Study collected blood samples from all participants and measured plasma carotenoids, a well-recognized biomarker of vegetable and fruit intake.26 We used changes in this biological measure in the comparison group to choose the self-reported measure with least random and systematic error.21 The validity problems of self-reported dietary measurement are exposed with the estimates of energy intake over the two study time points. In both groups, caloric intake declined by approximately 6% between baseline and 12 months, although we observed no between-group difference. Such declines are commonly observed with repeated self-reported dietary intake, and one of the reasons postulated for this is that participants try to reduce the participant burden associated with this reporting task.27 Were such declines true, then we would expect that they would be associated with weight loss, all other things being equal. We have previously reported that there was less than 1 kg difference in body weight between the WHEL Study’s intervention and comparison groups at both the baseline and 12-month time-points.28 Over 12 months, the WHEL Study intervention was associated with a 51% increase in total plasma carotenoid concentration with no change in the comparison group.20 As carotenoids are not regulated in humans and vegetable and fruit intake is the major source, this biomarker data adds more evidence that the WHEL Study intervention group achieved a major change to a plant-based dietary pattern.
For our measure of grocery costs, we asked participants to estimate their current household grocery costs at baseline and 12 months. The majority of participants were the primary food purchaser for their household. As such they were in the best position to provide an accurate estimate of household grocery costs, however, such a measure is subject to recall and other biases. During the pilot study, we asked participants to keep grocery receipts but abandoned this measure as there were too many incomplete records to provide a reasonable assessment of expenditures. Other studies estimated grocery costs for foods reported by dietary recall by checking the costs of these foods at a local supermarket. Such measures do not account for the many efforts people take to reduce their grocery costs, such as use of coupons or other price discounting, or purchasing from alternative less expensive venues. Further, produce prices can vary dramatically with quality and freshness, seasonal availability, farmers market versus grocery versus convenience store sources as well as with inventory levels, supply and demand. Such price variations are particularly common for products with short shelf lives such as fresh produce. These price variations appear unrelated to the nutrient content of the food, but do influence food choices, although perhaps more among those of lower socioeconomic status than in our study population.29, 30 Another approach has been to use ecological-level analyses of wholesale costs of food production to argue that increasing vegetables and fruit consumption must increase household grocery costs.10, 29–31 However, there are many reasons why such a crude approach can lead to a biased estimate.
Our measure of cost also has limitations. Reported grocery costs are per person estimates based on household costs, while dietary intake data are for a single member of the household. In addition, the cost data include only grocery purchases, while dietary data reflect all foods eaten whether in the house or outside the house. While our measure of grocery costs is not optimal, we do confirm the results of the US Department of Agriculture study that there is little additional cost associated with increasing vegetable and fruit consumption, regardless of socioeconomic status.32 The mean weekly food costs per person across groups in this study sample at baseline and 12 months ranged from $39.70 to $42.60, equivalent to the USDA $37.70 low cost food plan for 1999, when much of our data were being accrued.32, 33
Participants in our study were well educated and most were from middle socio-economic status groups. On average both study groups were eating healthy dietary patterns at baseline with an average of 6 vegetable servings and 28% energy from fat. Thus, their food purchasing habits will not be representative of the general population. Further, the study used a participant-centered telephone counseling program to help women substantially change their diets. If participants considered price as a possible barrier to purchasing certain foods, counselors suggested lower-cost alternatives. Also, the study provided easy-to-prepare, healthy recipes emphasizing vegetables, fruits, legumes, and whole grains to facilitate experimentation and regular consumption and monthly cooking classes in the first year (attended by about half of study participants) featured these recipes However, the intervention promoted consuming vegetable juice, emphasizing a variety of fresh vegetables. This was frequently reported by participants as burdensome and many appeared to take the more costly option of purchasing juice. Further, time was more commonly mentioned as a barrier by our participants than cost. Accordingly, both counselors and printed intervention material focused on quick and convenient sources of vegetables such as pre-cut carrots and pre-washed greens. Thus, if participants did not mention costs, our intervention did not promote the lowest cost alternatives. Even with this emphasis, the additional costs of adhering to the study intervention were approximately $1 per week. Nevertheless, caution is needed in generalizing our results to a population who might be very concerned about costs.
The factors that influence eating habits and food choices are many and diverse.9 Even if individuals can adopt healthier eating patterns at a similar cost, this does not mean they will do so. Our study demonstrates that motivated individuals can be encouraged to adopt a plant-based dietary pattern that involves a significant increase in vegetables, fruit, and fiber and reduction in fat, and that such a change does not necessitate an appreciable increase in household grocery expenditures. This suggests that concerns about the cost of adopting a healthy dietary pattern should not restrain public health efforts to improve dietary patterns to reduce health consequences
Acknowledgments
Financial support: This research was supported by NCI grant CA69375; University of California, San Diego, General Clinical Research Center NIH grant M01-RR00827; University of California, San Francisco, General Clinical Research Center NIH grant M01-RR00079; Stanford University General Clinical Research Center NIH grant M01-RR00070; and the Walton Family Foundation.
The Women’s Healthy Eating and Living (WHEL) Study Group include the Study Coordinating Center and Clinical Sites. Key personnel at each are as follows. Study Coordinating Center: University of California, San Diego Cancer Prevention and Control Program, San Diego, CA: John P. Pierce, PhD (Principal Investigator); Cheryl L. Rock, PhD, RD; Barbara A. Parker, MD; Loki Natarajan, PhD; Susan Faerber, BA (Project Director); Vicky A. Newman, MS, RD; Shirley W. Flatt, MS; Sheila Kealey, MPH; Linda Wasserman MD, PhD. WHEL Study Clinical Sites: Kaiser Permanente Northern California, Oakland, CA: Bette J. Caan, DrPH; Lou Ferenbacher, MD; Stanford University, Palo Alto, CA: Marcia L. Stefanick, PhD; Robert Carlson, MD; University of Arizona, Tucson & Phoenix, AZ: Cynthia Thomson, PhD, RD; James Warnecke, MD; University of California, Davis, Davis, CA: Ellen Gold PhD; Sidney Scudder, MD; University of California, San Diego Cancer Center, San Diego, CA: Kathryn Hollenbach, PhD; Linda Wasserman MD, University of Texas MD Anderson Cancer Center, Houston, TX: Lovell A. Jones, PhD; Richard Theriault, DO, Richard Hajek PhD; Center for Health Research - Portland, Portland, OR: Cheryl Ritenbaugh, PhD, Mark Rarick, MD.
References
- 1.Eyre H, Kahn R, Robertson RM, et al. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Circulation. 2004;109(25):3244–55. doi: 10.1161/01.CIR.0000133321.00456.00. [DOI] [PubMed] [Google Scholar]
- 2.Ammerman AS, Lindquist CH, Lohr KN, et al. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med. 2002;35(1):25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- 3.Glanz K, Basil M, Maibach E, et al. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98(10):1118–26. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 4.Vastine A, Gittelsohn J, Ethelbah B, et al. Formative research and stakeholder participation in intervention development. Am J Health Behav. 2005;29(1):57–69. doi: 10.5993/ajhb.29.1.5. [DOI] [PubMed] [Google Scholar]
- 5.Bogers RP, Assema P, Brug J, et al. Psychosocial predictors of increases in fruit and vegetable consumption. Am J Health Behav. 2007;31(2):135–45. doi: 10.5555/ajhb.2007.31.2.135. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman PR, MacDonald JM, Lutz SM, et al. Agricultural Economics Report No. (AER759) Washington, D.C: U.S. Department of Agriculture; 1997. Do the Poor Pay More for Food? Item Selection and Price Differences Affect Low-Income Household Food Costs. [Google Scholar]
- 7.Cade J, Upmeier H, Calvert C, et al. Costs of a healthy diet: analysis from the UK Women’s Cohort Study. Public Health Nutr. 1999;2(4):505–12. doi: 10.1017/s1368980099000683. [DOI] [PubMed] [Google Scholar]
- 8.Cox DN, van Galen M, Hedderley D, et al. Sensory and hedonic judgments of common foods by lean consumers and consumers with obesity. Obes Res. 1998;6(6):438–47. doi: 10.1002/j.1550-8528.1998.tb00376.x. [DOI] [PubMed] [Google Scholar]
- 9.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 10.Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133(3):838S–840S. doi: 10.1093/jn/133.3.838S. [DOI] [PubMed] [Google Scholar]
- 11.Yeh MC, Ickes SB, Lowenstein LM, et al. Understanding barriers and facilitators of fruit and vegetable consumption among a diverse multi-ethnic population in the USA. Health Promot Int. 2008;23(1):42–51. doi: 10.1093/heapro/dam044. [DOI] [PubMed] [Google Scholar]
- 12.Reed J, Frazao E, Itskowitz R. Economic Research Service. Washington, D.C: U.S. Department of Agriculture; 2004. How much do Americans pay for fruits and vegetables? Agriculture Information Bulletin 792–4. [Google Scholar]
- 13.Raynor HA, Kilanowski CK, Esterlis I, et al. A cost-analysis of adopting a healthful diet in a family-based obesity treatment program. J Am Diet Assoc. 2002;102(5):645–56. doi: 10.1016/s0002-8223(02)90148-3. [DOI] [PubMed] [Google Scholar]
- 14.Anderson JV, Bybee DI, Brown RM, et al. 5 a day fruit and vegetable intervention improves consumption in a low income population. J Am Diet Assoc. 2001;101(2):195–202. doi: 10.1016/S0002-8223(01)00052-9. [DOI] [PubMed] [Google Scholar]
- 15.Sooman A, Macintyre S, Anderson A. Scotland’s health--a more difficult challenge for some? The price and availability of healthy foods in socially contrasting localities in the west of Scotland. Health Bull (Edinb) 1993;51(5):276–84. [PubMed] [Google Scholar]
- 16.Pierce JP, Faerber S, Wright FA, et al. A randomized trial of the effect of a plant-based dietary pattern on additional breast cancer events and survival: the Women’s Healthy Eating and Living (WHEL) Study. Control Clin Trials. 2002;23(6):728–56. doi: 10.1016/s0197-2456(02)00241-6. [DOI] [PubMed] [Google Scholar]
- 17.NCI. Eat 5 Fruits and Vegetables a Day. Washington, DC: National Cancer Institute; 1995. [Google Scholar]
- 18.NCI. Action Guide for Healthy Eating. Bethesda, MD: National Cancer Institute; 1995. [Google Scholar]
- 19.Newman VA, Thomson CA, Rock CL, et al. Achieving substantial changes in eating behavior among women previously treated for breast cancer--an overview of the intervention. J Am Diet Assoc. 2005;105(3):382–91. doi: 10.1016/j.jada.2004.12.008. quiz 488. [DOI] [PubMed] [Google Scholar]
- 20.Pierce JP, Natarajan L, Sun S, et al. Increases in plasma carotenoid concentrations in response to a major dietary change in the women’s healthy eating and living study. Cancer Epidemiol Biomarkers Prev. 2006;15(10):1886–92. doi: 10.1158/1055-9965.EPI-05-0928. [DOI] [PubMed] [Google Scholar]
- 21.Natarajan L, Flatt SW, Sun X, et al. Validity and systematic error in measuring carotenoid consumption with dietary self-report instruments. Am J Epidemiol. 2006;163(8):770–8. doi: 10.1093/aje/kwj082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pierce JP, Newman VA, Natarajan L, et al. Telephone counseling helps maintain long-term adherence to a high-vegetable dietary pattern. J Nutr. 2007;137(10):2291–6. doi: 10.1093/jn/137.10.2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matthews KA, Shumaker SA, Bowen DJ, et al. Women’s Health Initiative. Why now? What it is? What’s new? Am Psychol. 1997;52(2):101–116. doi: 10.1037//0003-066x.52.2.101. [DOI] [PubMed] [Google Scholar]
- 24.Johnson-Kozlow M, Sallis JF, Gilpin EA, et al. Comparative validation of the IPAQ and the 7-Day PAR among women diagnosed with breast cancer. Int J Behav Nutr Phys Act. 2006;3:7. doi: 10.1186/1479-5868-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Black AE, Cole TJ. Biased over- or under-reporting is characteristic of individuals whether over time or by different assessment methods. J Am Diet Assoc. 2001;101(1):70–80. doi: 10.1016/S0002-8223(01)00018-9. [DOI] [PubMed] [Google Scholar]
- 26.Rock CL, Flatt SW, Wright FA, et al. Responsiveness of carotenoids to a high vegetable diet intervention designed to prevent breast cancer recurrence. Cancer Epidemiol Biomarkers Prev. 1997;6(8):617–23. [PubMed] [Google Scholar]
- 27.Caan BJ, Flatt SW, Rock CL, et al. Low-energy reporting in women at risk for breast cancer recurrence. Women’s Healthy Eating and Living Group. Cancer Epidemiol Biomarkers Prev. 2000;9(10):1091–7. [PubMed] [Google Scholar]
- 28.Saquib N, Natarajan L, Rock CL, et al. The impact of a long-term reduction in dietary energy density on body weight within a randomized diet trial. Nutr Cancer. 2008;60(1):31–8. doi: 10.1080/01635580701621320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.French SA. Pricing effects on food choices. J Nutr. 2003;133(3):841S–843S. doi: 10.1093/jn/133.3.841S. [DOI] [PubMed] [Google Scholar]
- 30.Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr. 2002;132(12):3764–71. doi: 10.1093/jn/132.12.3764. [DOI] [PubMed] [Google Scholar]
- 31.Inglis V, Ball K, Crawford D. Why do women of low socioeconomic status have poorer dietary behaviours than women of higher socioeconomic status? A qualitative exploration. Appetite. 2005;45(3):334–43. doi: 10.1016/j.appet.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 32.USDA. Food Cosumer Price Index, Prices, and Expenditure Tables. Economic Research Service: U.S. Department of Agriculture; 2003. http://www.ers.usda.gov/Briefing/CPIFoodAndExpenditures/data/ [Google Scholar]
- 33.USDA. Official USDA Food Plans: Cost of Food at Home and at Four Levels. Washington, D.C: U.S. Department of Agriculture; [accessed 6-12-08]. http://www.cnpp.usda.gov/usdafoodplanscostoffood.htm. [Google Scholar]
- 34.USDHHS. The evidence report. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH publication no. 98–4083. [Google Scholar]