Abstract
Objectives/Hypothesis
The objective of this study was to assess the appropriateness of hearing aid fittings within a sample of adult cochlear implant recipients who use a hearing aid in the contralateral ear (i.e., bimodal stimulation).
Methods
The hearing aid gain was measured using real ear testing for 14 post-lingually deaf English speaking adults who use a cochlear implant in the contralateral ear. Unaided and aided audiometric testing assessed the degree of functional gain derived from hearing aid use.
Results
On average, the target to actual output level difference was within 10 dB only at the tested frequencies of 750 Hz and 1000 Hz. Only 1 of the 14 study participants had a hearing aid for which the majority of the tested frequencies were within 10 dB of the target gain. In addition, a greater amount of functional gain (i.e., the increase in unaided behavioral thresholds after amplification) was provided for lower frequencies than the higher frequencies.
Conclusions
Hearing aid settings in our sample were suboptimal and may be regarded as a contributing factor to the variability in bimodal benefit. Refining hearing aid fitting strategies tailored to the needs of the concurrent cochlear implant and hearing aid user is recommended.
Keywords: Adult, bimodal stimulation, cochlear implants, deafness, hearing aids
INTRODUCTION
Historically, the indications for cochlear implants (CIs) in adults were limited to bilateral, severe-to-profound deafness with little or no appreciable benefit from conventional acoustic amplification.1 Advances in technology, surgical practice and greater familiarity and acceptance of CIs among patients have lead to expansion of the indications for implantation. Currently many adult CI candidates present with some degree of residual hearing in the contralateral ear. In these individuals, concurrent use of electrical stimulation from a CI in one ear and acoustical stimulation from a hearing aid (HA) in the contralateral ear confers functionally significant advantages compared to CI use alone. Improvements are noted in sound localization and measures of speech perception in both quiet and noisy conditions.2–7 Superior performance on vowel and consonant identification and sentence recognition tasks has been reported as early as 6 month post-CI with demonstrable improvement for up to 12 months post-CI.8 These benefits are believed to be derived from the processing of speech via a cochlear implant in addition to the low-frequency speech cues that may be provided by a HA.9
There is a great deal of unexplained variability, however, in the degree of functional benefit observed with concurrent CI and HA use.3 For example, some individuals demonstrate benefit of bimodal stimulation under quiet, but not noisy conditions. Furthermore, some individuals even demonstrate poorer performance on measures of speech perception when HA input is added.9 Variability could be introduced by differences in the degree of baseline hearing loss in the non-implanted ear or divergent HA and CI usage among participants. Another possible contributing factor is relative inadequacy of HA fittings in the setting of concurrent CI and HA use. Although work has been done demonstrating the enhancement of bimodal benefits by fine-tuning HA fitting with the CI in children, this issue has gone unaddressed in adults.2 Ching et al. report in their assessment of amplification requirements of 16 children with CIs that the frequency response prescribed by the National Acoustics Labs, Revised, Profound (NAL-RP) algorithm was appropriate on average, but fine-tuning may be necessary for the individual. The purpose of the current study was to assess appropriateness of HA fitting in post-lingually deaf adults concurrently using CI’s.
MATERIALS AND METHODS
Fourteen post-lingually deaf English speaking adults – 9 female and 5 male – concurrently using a behind-the-ear (BTE) HA and a multichannel CI were included in this study. All study participants had fully inserted electrode arrays and were implanted at Indiana University School of Medicine between the years of 1998 and 2008. All had at least 6 months of CI experience at the time of testing. Prior to implantation, all participants had pure tone averages (i.e., behavioral threshold average of 500 Hz, 1000 Hz, and 2000 Hz) in the severe-to-profound range (i.e., ≥ 71 dB HL). Participant characteristics and information on CI and HA model are shown in Table I.
Table I.
Study participant demographics
| Participant ID | Age at testing (yr) | CI Model | Duration CI Use (yrs) | PTA (dB HL) | HA Model | Duration HA Use (yrs) |
|---|---|---|---|---|---|---|
| I. | 75.45 | ME-Combi 40+ H | 5.15 | 87 | Unitron digital SF | 34.75 |
| II. | 57.08 | N24-CI24R (CS) | 7.28 | 105 | Unitron US 80-PP | 47.38 |
| III. | 60.52 | ME-Combi 40+ H | 5.22 | 100 | Marcon | 49.52 |
| IV. | 70.79 | CL-HiFocus | 9.19 | 95 | Widex Senso | 52.09 |
| V. | 76.22 | N24-CI24M | 11.22 | 98 | Widex Q32 | 24.02 |
| VI. | 59.74 | N24-CI24RE (CA) | 3.04 | 100 | CN Resound 780 D | 51.14 |
| VII. | 72.14 | N24-CI24RE (CA) | 2.94 | 82 | Phonak Perseo 311 DAZ | 29.74 |
| VIII. | 66.44 | ME-Combi 40+ H | 4.74 | 93 | Phonak Senso-Forte 331X | 47.64 |
| IX. | 52.44 | N24-CI24R (CA) | 3.24 | 97 | Oticon 390 PL | 3.74 |
| X. | 70.48 | N24-CI24RE (CA) | 0.58 | 105 | Oticon Digifocus II SP | 20.08 |
| XI. | 75.34 | ME-Combi 40+ H | 9.64 | 78 | Starkey A575 Sequel AH | 13.64 |
| XII. | 71.34 | N24-CI24RE (CA) | 4.34 | 88 | CN Resound | 40.74 |
| XIII. | 59.21 | CL-HiRes 90K | 4.11 | 92 | CN Resound 780 D | 46.51 |
| XIV. | 40.07 | N24-CI24RE (CA) | 2.17 | 95 | Rexton Energy | 26.57 |
| Mean | 64.80 | 5.20 | 95 | 34.83 | ||
| SD | 10.46 | 3.07 | 9 | 15.48 |
CI = cochlear implant; LF-PTA = low frequency pure-tone average; PTA = pure-tone average; HL = hearing level; HA = hearing aid; SD = standard deviation
Unaided and aided audiometric testing was completed using a Grason-Stadler GSI-61 audiometer (Eden Prairie, MN) in a sound attenuated booth. Aided behavioral thresholds were obtained with the participant’s HA on user-preferred settings and their CI turned off. A tone stimulus transduced through a ten-inch wall-mounted speaker was presented at 0° azimuth. Unaided behavioral thresholds were obtained using tones routed through foam ear inserts to the non-implanted ear. The standard clinical ascending/descending method with incremental increases of 5 dB and decreases of 10 dB was used.
Real-ear testing was conducted using the RM500SL portable real ear/HA analyzer (AudioScan, Dorchester, Ontario, Canada). Target gain measures were obtained using the Desired Sensation Level [input/output] algorithm for adults (DSL – Adult[i/o]). The objective of the DSL-Adult[i/o] algorithm is to provide maximum audibility while maintaining comfortable loudness across all listening environments and to provide hearing instrument output limiting targets that vary as a function of frequency and hearing level.9
Actual real-ear measurements were performed after inputting the unaided behavioral thresholds and selecting the real-ear analyzer’s “Speechmap” function. The “Carrot Passage” was used to assess HA output. This speech-shaped stimulus can be presented at multiple signal levels (i.e., 55 dB SPL, 65 dB SPL, 70 dB SPL, and 75dB SPL). For this study, data from the 65 dB SPL presentation level was obtained; this level represents average conversational speech.
A 1-mm diameter silicone probe-microphone was inserted into the study participant’s ear canal (28 mm for women; 30 mm for men) distal to the reinserted and activated HA in order to reach within 2–3 mm of the tympanic membrane. Prior to testing, the system was calibrated per the manufacturer’s instructions. Participants were positioned approximately 24 inches from the test speaker and instructed to minimize head movement during testing. Otoscopy was performed prior to initiation of real-ear measurements to ensure canal patency. Participants were tested using their preferred HA volume control settings.
RESULTS
An example real-ear HA target output gain from participant I’s HA is presented in Table II. The target and actual output in dB SPL is provided for the frequencies 250 Hz, 500 Hz, 750 Hz, 1000 Hz, 2000 Hz, 4000 Hz, and 6000 Hz. In addition, the difference between these two measures in dB SPL is provided for each frequency. A positive value indicates that the HA was providing more gain than the suggested target, and a negative number indicates that the HA was providing less gain than the suggested target. For participant I, only one target was met (i.e., 250 Hz). All other actual outputs were greater than 5 dB below the target gain as prescribed by the DSL – Adult[i/o] algorithm.
Table II.
Target and actual gain measures at 65 dB SPL for participant I.
| 250 Hz | 500 Hz | 750 Hz | 1000 Hz | 2000 Hz | 4000 Hz | 6000 Hz | |
|---|---|---|---|---|---|---|---|
| Target (dB SPL) | 48 | 82 | 103 | 114 | 124 | 124 | 124 |
| Actual Output (dB SPL) | 57 | 75 | 91 | 97 | 91 | 64 | 49 |
| Target/Output Difference (dB SPL) | 9 | −7 | −12 | −17 | −33 | −60 | −75 |
Hz = Hertz; dB = decibel; SPL = sound pressure level
Table III provides the difference measures for the target and actual HA output for all study participants. For 4 out of 14 study participants target outputs were generated at all frequencies. Blank cells represent frequencies for which targets could not be accurately generated due to inaccurate entry of behavioral threshold data. None of these particular behavioral thresholds, though, could be obtained to the limits of the audiometer. One participant’s hearing aid out of the 14 came close to matching the desired level (participant VI.). At 250 Hz, 2/13 participants’ hearing aids were within 2 dB of the target, 2/13 were within 5 dB of the target, and 5/13 were within 10 dB of the target. At 500 Hz, 0/14 participants’ hearing aids were within 2 dB of the target, 1/14 was within 5 dB of the target, and 5/14 were within 10 dB of the target. At 750 Hz, 3/12 participants’ hearing aids were within 2 dB of the target, 4/12 were within 5 dB of the target, and 6/12 were within 10 dB of the target. At 1000 Hz, 1/12 participants’ hearing aids were within 2 dB of target, 4/12 were within 5 dB, and 6/12 were within 10 dB. At 2000 Hz, 0/8 were within 2 dB of the target, 1/8 was within 5 dB, and 1/8 was within 10 dB of the target. At 4000 Hz, 0/10 were within 2, 5 or 10 dB of the target. At 6000 Hz, 0/6 were within 2, 5, or 10 dB of the target.
Table III.
Target to actual output difference data for all study participants
| Participant ID | 250 Hz | 500 Hz | 750 Hz | 1000 Hz | 2000 Hz | 4000 Hz | 6000 Hz |
|---|---|---|---|---|---|---|---|
| I. | 9 | −7 | −12 | −17 | −33 | −60 | −75 |
| II. | −17 | −16 | −17 | 3 | −16 | −18 | |
| III. | −31 | −25 | |||||
| IV. | 2 | −7 | 4 | 26 | |||
| V. | −16 | −11 | −21 | −34 | −70 | ||
| VI. | −1 | −6 | 0 | 12 | |||
| VII. | −8 | −13 | −22 | −50 | |||
| VIII. | −9 | −3 | −1 | 0 | 4 | −13 | −34 |
| IX. | −33 | −21 | −17 | −7 | −14 | −26 | |
| X. | −22 | −17 | −16 | −16 | −14 | −38 | −65 |
| XI. | −47 | −24 | −6 | −5 | −12 | −39 | |
| XII. | −12 | −14 | −16 | −31 | −37 | −48 | −70 |
| XIII. | −22 | −9 | −2 | −4 | |||
| XIV. | −17 | −8 | −9 | −17 | −13 | −40 | |
| AVERAGE | −15.92 | −13.57 | −9.42 | −5.75 | −19.63 | −37.30 | −50.33 |
| SD | 15.41 | 7.04 | 8.79 | 15.93 | 15.09 | 19.27 | 25.01 |
Hz = Hertz; SD = standard deviation
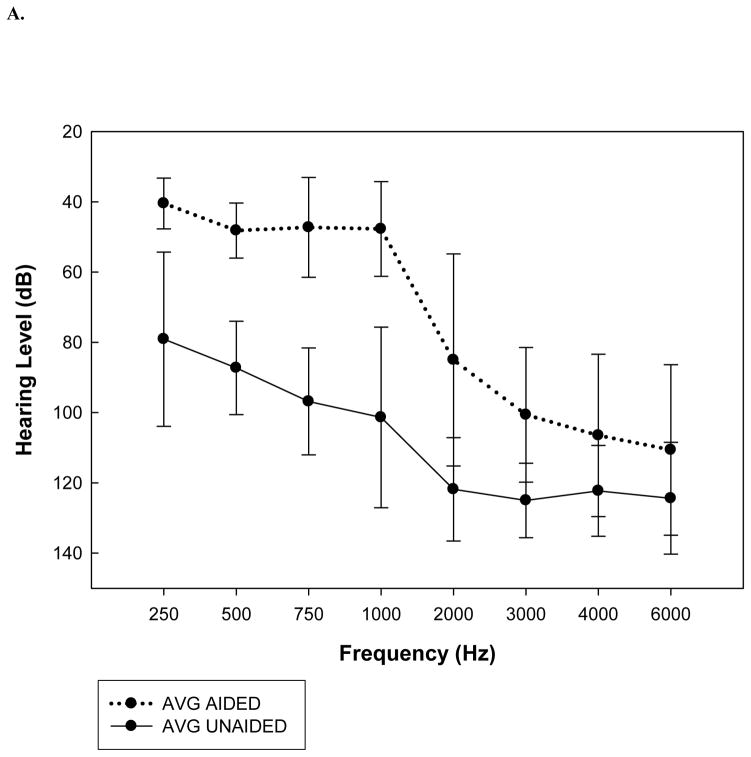
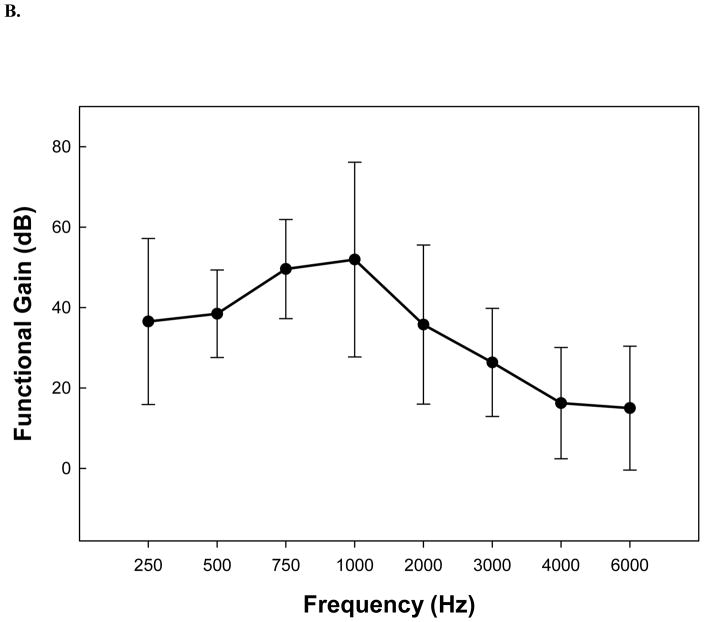
Thresholds as a function of frequency in the unaided and aided condition are shown in Figure 1A. Mean functional gain from HA use as a function of frequency is shown in Figure 1B. For instances where no response was obtained to the limit of the audiometer, 130 dB was used as the threshold to estimate functional gain at that frequency. Participants demonstrated higher functional gain for 250 Hz, 500 Hz, 750 Hz, and 1000 Hz compared to the gain at 2000 Hz, 3000 Hz, 4000 Hz and 6000 Hz. A one-way ANOVA analysis revealed that the functional gain was significantly different across frequencies [F(8,89) = 6.51, p<0.0001. Post hoc Bonferroni analyses revealed that the gain at 750 Hz was significantly greater than the gain at 4000 Hz (p < 0.0001) and at 6000 Hz (p < 0.0001).
Fig. 1.
(A) Hearing level (dB) as a function of frequency (Hz) for aided (dashed line) and unaided (solid line) conditions. (B) Hearing aid functional gain (dB) as a function of frequency (Hz). The x-axis represents frequency for each study participant. The y-axis represents mean functional gain across all participants. Error bars show one standard deviation from the mean.
DISCUSSION
With evolving indications, more patients are presenting for implantation with some degree of serviceable hearing in the contralateral ear. Bimodal aural stimulation has been shown to positively affect several dimensions of speech and language.3–4, 9 Significant, unexplained variability, however, has been observed in the benefit that can be obtained from a contralateral hearing aid.10 Suboptimal HA fitting is one explanation that has received little attention as a source of this variance. The purpose of our study was to determine if the HA settings used in a sample of concurrent CI users provided appropriate amplification and functional gain.
We found a minority of participants with optimal HA target-to-actual output performance upon real-ear testing. Frequencies 750 Hz and 1000 Hz were the only for which the average mean difference from target gain to actual HA output across all participants was within 10 dB (Table III). Only one of fourteen hearing aids (i.e., participant VI) had a majority of actual outputs within 10 dB of the target range. It should also be noted, however, that providing appropriate gain beyond 2000 Hz for profound hearing losses is challenging if not impossible.11 All of the participants in this study had profound hearing losses beyond 2000 Hz, and consequently, adequate hearing aid gain cannot be provided for these individuals at higher frequencies. Considering the amount of aidable hearing in the low frequencies, however, it is somewhat surprising that more appropriate gain was not provided at the low frequencies (i.e., 250 Hz and 500 Hz).
It has been demonstrated that optimal HA fittings provide gain within 10 dB of the target gain.12 Jenstad et al. demonstrated that optimal performance on speech intelligibility – indexed by consonant identification –was maintained in the low frequency range from 5 dB above DSL[i/o] targets to 10 dB below DSL[i/o] targets; and in the high frequency range optimal performance was maintained from DSL[i/o] targets to 10 dB below DSL[i/o] targets. Our finding that none of the 7 frequencies tested here were on average within 5 dB of the DSL[i/o] target and only 2 frequencies (750 Hz, 1000 Hz) on average were within 10 dB of the DSL[i/o] target is, therefore, clinically significant. Inadequate fitting may be a major contributing factor to the variability reported in benefit from bimodal stimulation – why some individuals benefit in terms of terms of improved speech perception, especially in noisy conditions, and others do not.3, 9
The purpose of the DSL[i/o] algorithm is to provide maximum audibility while maintaining comfortable loudness across all listening environments.12–13 There is, however, no validated procedure for selecting HA settings for individuals concurrently receiving electrical input from a CI.2 Most individuals receiving bimodal input are fitted with their HA prior to and independently from their CI. It has been shown in children that fine-tuning HA’s by an average of 6 dB from the prescribed level to achieve a better loudness balance with a CI confers superior performance on measures of speech perception and sound localization than CI use alone.2 Some have recently advocated the use of a structured bimodal fitting strategy using loudness scaling for both CI’s and HA.14–15
Although the target outputs were almost universally suboptimal, participants in our sample did demonstrate a degree of functional gain in the low frequency range as revealed in Figure 1B. Considering the fact that the study participants had behavioral thresholds within an aidable range at the lower frequencies (i.e., 250 Hz, 500 Hz, and 750 Hz) it is not surprising that more functional gain was obtained for the low frequencies compared to the higher frequencies. It is recognized that individuals with high frequency hearing loss do not enjoy the same degree of benefit from amplification as those with a predominantly low frequency or combined low-high frequency loss and the degree of benefit reported is often unrelated to hearing aid gain and frequency response.11
CONCLUSION
These data suggests that HA settings are suboptimal in deaf adults concurrently using CIs. It might be possible that the large degree of variability observed in performance with bimodal stimulation could be in part related to poor HA fitting. Despite the poor target-to-actual output performance of HA’s in this sample, participants demonstrated functional gain with their HA, especially in the low frequency range. More appropriate HA settings achieved by refining fitting strategies tailored to the needs of concurrent CI/HA users may broaden the degree of benefit observed from bimodal stimulation.
Acknowledgments
This work was supported by NIH/NIDCD R03DC008383 and NIH/NIDCD T32 DC00012
Footnotes
Conflict of Interest: None
Level of Evidence: 2c
BIBLIOGRAPHY
- 1.Cochlear implants in adults and children. NIH Consensus Statement. 1995;13:1–30. [PubMed] [Google Scholar]
- 2.Ching T, Psarros C, Hill M, Dillon H, Incerti P. Should children who use cochlear implants wear hearing aids in the opposite ear? Ear Hearing. 2001;22:365–380. doi: 10.1097/00003446-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Ching T, Incerti P, Hill M. Binaural benefits for adults who use hearing aids and cochlear implants in opposite ears. Ear Hearing. 2004;25:9–21. doi: 10.1097/01.AUD.0000111261.84611.C8. [DOI] [PubMed] [Google Scholar]
- 4.Kiefer J, Pok M, Adunka O, et al. Combined electric and acoustic stimulation of the auditory system: Results of a clinical study. Audiol Neuro-Otol. 2005;10:134–144. doi: 10.1159/000084023. [DOI] [PubMed] [Google Scholar]
- 5.Morera C, Manrique M, Ramos A, et al. Advantages of binaural hearing provided through bimodal stimulation via a cochlear implant and a conventional hearing aid: A 6-month comparative study. Acta Oto-Laryngologica. 2005;125:596–606. doi: 10.1080/00016480510027493. [DOI] [PubMed] [Google Scholar]
- 6.Potts L, Skinner MW, Litovsky RA, Strube MJ, Kuk F. Recognition and localization of speech by adult cochlear implant recipients wearing a digital hearing aid in the nonimplant ear (bimodal hearing) J Am Acad Audiol. 2009;20(6):353–373. doi: 10.3766/jaaa.20.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turner CW, Gantz BJ, Vidal C, Behrens A, Henry BA. Speech recognition in noise for cochlear implant listeners: Benefits of residual acoustic hearing. J Acoust Soc Am. 2004;115:1729–1735. doi: 10.1121/1.1687425. [DOI] [PubMed] [Google Scholar]
- 8.Shallop JK, Arndt PL, Turnacliff KA. Expanded indications for cochlear implantation: perceptual results in seven adults with residual hearing. J Speech Lang Pathol Audiol. 1992;16:141–148. [Google Scholar]
- 9.Holt RF, Kirk KI, Eisenberg LS, Martinez AS, Campbell W. Spoken word recognition development in children with residual hearing using cochlear implants and hearing aids in opposite ears. Ear Hearing. 2005;26:82S–91S. doi: 10.1097/00003446-200508001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Dunn CC, Tyler RS, Witt SA. Benefit of wearing a hearing aid on the unimplanted ear in adult users of a cochlear implant. J Speech Hear Res. 2005;48:668–680. doi: 10.1044/1092-4388(2005/046). [DOI] [PubMed] [Google Scholar]
- 11.Beamer S, Grant KW, Walden BE. Hearing aid benefit in patients with high-frequency hearing loss. J Am Audiol Soc. 2000;11(8):429–437. This journal should be J Am Acad Audiol. [PubMed] [Google Scholar]
- 12.Jenstad L, Bagatto MP, Seewald RC, Scollie SD, Cornelisse LE, Scicluna R. Evaluation of the desired sensation level [input/output] algorithm for adults with hearing loss: the acceptable range for amplified conversational speech. Ear Hearing. 2007;28(6):793–811. doi: 10.1097/AUD.0b013e318157670a. [DOI] [PubMed] [Google Scholar]
- 13.Scollie S, Seewald R, Cornelisse L, et al. The Desired Sensation Level Multistage Input/Output Algorithm. Trends Amplif. 2005;9(4):159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seewald RC, Ross M, Spiro MK. Selecting amplification characteristics for young hearing-impaired children. Ear Hearing. 1985;6(1):48–50. doi: 10.1097/00003446-198501000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Annerose K, Andrea B, Jan G, Wolf M. Cochlear implant and hearing aid: a new approach to optimizing the fitting in this bimodal situation. Eur Arch Oto-Rhino-L. 2009;266(12):1879–1884. doi: 10.1007/s00405-009-0993-9. (1876) [DOI] [PubMed] [Google Scholar]