Abstract
Introduction
Migration is seen as a risk factor for developing psychiatric symptoms and experiencing social exclusion. In the Netherlands, the Moroccan-Dutch population is the second largest migrant group. 70% of all young Moroccan-Dutch people meet each other in the online community www.marokko.nl. Within this community, we investigated the association between experiences of social exclusion and self-reported depressive symptoms and psychotic experiences.
Materials and methods
Participants were recruited via the website www.marokko.nl. They completed an online survey, with screening instruments for depressive symptoms (K10) and psychotic experiences (PQ-16), measures of social exclusion (perceived discrimination, social defeat and social support), and questions about demographical information. With regression analysis the association between social exclusion and psychiatric symptoms was investigated.
Results
We included 267 participants; 87% were female. 27% of the sample has received mental healthcare in the past. Over 50% of these people screened positive for depressive symptoms and psychotic experiences. Perceived discrimination and social defeat were significantly associated with psychotic experiences and social defeat was associated with depressive symptoms. Social support and higher education were associated with less depressive symptoms and psychotic experiences.
Discussion
Our findings suggest that the online environment allows for epidemiological research and early symptom detection. Levels of psychopathology were high in our sample. This suggests that a part of this young ethnic minority population might not get adequate mental healthcare. Since this population can be reached through Internet, the online environment may therefore also offer an appropriate setting for intervention, to increase resilience towards social exclusion.
Introduction
Across countries, migration is a risk factor for the development of a range of psychiatric disorders. Two meta-analyses have shown a strong association between migration and psychotic disorders [1,2]. A recent meta-analysis showed that the risk for non-affective psychosis and subclinical psychotic symptoms was increased in male, but not female, migrants from Morocco and surrounding countries [3]. An association between migration status and mood disorders was also found in a meta-analysis [4] and confirmed in several epidemiological studies [5,6]. In 2013, Cantor-Graae and Pederson showed an increased risk for the full spectrum of psychiatric disorders in migrants, with the second generation migrants having increased risk for more psychiatric disorders compared to the first generation [7]. Also in the Netherlands, migrants have increased risk for psychiatric disorders. The risk for schizophrenia spectrum disorders is increased in first and second generation migrants. [8,9] There is also evidence that the prevalence of depressive disorders is increased in Turkish-Dutch and Moroccan-Dutch people compared to native Dutch people [9,10]. The incidence of psychotic disorders is not only increased in first generation migrants, but also in second-generation migrants [1,2]. Furthermore, the age of migration has been found to be negatively correlated with the risk of developing a psychotic disorder.[11]. This suggests that (social) factors in the country of destination are important [12,13]. In other words: the ethnic minority status is more important than the actual migration itself [1,2,14].
Which factors make the ethnic minority status a risk factor for mental health problems? In the meta-analysis of Cantor-Graae et al (2005), ‘black skin colour’ was associated with a higher relative risk for psychosis compared to migrants with a non-black skin colour. This finding points towards an underlying mechanism of discrimination, since people with black skin colour are more often discriminated against [2]. Indeed, discrimination has previously been associated with psychotic symptoms and mood disorders [15–21]. Several other social concepts are associated with psychopathology. Social defeat, which is defined as ‘being in a subordinate position’, by Gilbert and Allan in 1998, is associated with depression [22–25] and has been associated with psychosis [26]. A review about older Asian migrants in the USA describes a link between the prevalence of depression and several social factors, including social support and acculturation [27].
Psychiatric disorders like psychosis and depression can be considered as a continuum in early stages of the disorder [28] and were shown to co-occur more frequently in Moroccan- and Turkish-Dutch migrants compared to native Dutch people [8]. Early detection of individuals with high risk of developing psychopathology is important, in order to deliver adequate preventive measures [29,30]. Early detection is mostly performed in persons who actively seek help [29]. This study is performed in a ‘general population’ online community of Moroccan-Dutch people. With this study, we can test the feasibility of early detection within this population. Furthermore, the main results might give clues for developing preventive measures.
The Moroccan-Dutch population is the second largest migrant population in the Netherlands (380,755 inhabitants, reflecting 2,3% of the total Dutch population) [31]. Since this Moroccan-Dutch population is at increased risk for psychiatric disorders, we would like to identify high-risk individuals within this subgroup of the general population. Although this population is geographically spread across the Netherlands, they meet each other online. The majority (70%) of young Moroccan-Dutch people actively visit the website Marokko.nl, which is a news site and discussion forum, where they exchange information and opinions on many different subjects. This creates the opportunity to reach this population via the Internet for research purposes [32]. In this online community visitors are protected by anonymity. Interestingly, the website contains many forum discussions about psychiatric problems, a subject which is otherwise taboo in this population. This platform therefore creates an opportunity to investigate mental health problems in a high-risk ethnic minority population outside of the conventional mental healthcare setting.
Aim of the study
In the MEDINA (Migrants Examined for Determinants of psychopathology through INternet Assessment) study, we used the online platform www.marokko.nl to investigate the association between symptoms of psychopathology (depressive symptoms and psychotic experiences) and experiences of social exclusion (reported measures of social defeat, perceived discrimination and social support) in a cross-sectional sample of young Moroccan-Dutch participants.
Material and methods
We performed an online survey in a cross-sectional convenience sample of the Moroccan-Dutch population, using a combination of several self-report questionnaires. The research protocol of this study is described in a design paper [32]. We will here summarize the methods.
Ethics
The protocol was presented to the Medical Ethical Committee (METc) of the University Medical Center Groningen (UMCG) and they decided that, due to the very limited burden and risks for participants, it was exempted from further review (reference number M12.124959). We obtained informed consent from participants (see further). Data were anonymously obtained via internet. IP addresses were not recorded. Privacy sensitive information (email addresses) was anonymised before analysis.
Participants
Inclusion criteria were: Dutch citizenship; participant is born in Morocco or at least one of the parents is born in Morocco; having sufficient knowledge of the Dutch language and being a visitor to the website Marokko.nl. Exclusion criteria were: age younger than 18 years.
Recruitment and consent
Marokko.nl is a very popular website, which is regularly visited by 70% of all young Moroccan-Dutch people. We invited participants via advertisement on the website Marokko.nl, shown as banners. For these advertisements, we used two different approaches.
In the first approach, we invited people to fill out the K10 as a depression self-test. As this measurement is part of the survey, these questions could be skipped at a later stage. The advertisement text was: ‘are you feeling down? Fill out the test!’. In the second approach, we asked people to participate in scientific research. The advertisement text for the second approach was: ‘Do you want to participate in scientific research?’. For the third recruitment strategy, we approached visitors of the website marokko.ziekofbezeten.nl (translation: being ill or being possessed). This is an add-on website of Marokko.nl, where information about psychiatric disorders and related religious phenomena is given and healthcare workers can be contacted. On this website, we used an opt-in method to ask if people agreed to be contacted on a later moment for scientific research. The people who agreed were invited for the MEDINA-study with an email invitation. We recorded for all participants via which approach they were recruited for the survey. We raffled gift vouchers between participants as an incentive.
At the first webpage of the survey, information about the study was presented, including the link to a file with complete participant information. At the same webpage, participants had to give informed consent, using a checkbox. After consent was given, people had to declare that their age was above 18 years old, before they could proceed to the survey.
Measurements
The survey combines several, previously validated, short questionnaires, presented to the participants as a single online survey, which takes about ten minutes to complete. We used the Kessler Psychological Distress Scale 10 (K10), which has originally been designed for measuring distress, but has been validated within the Moroccan-Dutch population as a screening instrument for detecting clinically relevant depressive symptoms [33–35]. We used the Prodromal Questionnaire-16 (PQ-16) for screening for psychotic experiences [36]. The PQ-16 included an impact scale, that assesses the distress of the experience. For each item this distress was scored between 1 (no impact) and 4 (high impact). We measured perceived discrimination with the Every Day Discrimination Scale, which contains questions about recent experiences of personal discrimination [37–40]. Social support was measured with the ‘Oslo Social Support Questionnaire’ [41] and social defeat was measured with the ‘Social Defeat Scale’ [22]. Furthermore, we included socio-demographic items assessing age, gender, first/second generation migrant status, previous mental healthcare and highest completed level of education. All demographic items were dichotomised. Age was based on median value (23 years). Education was split in ‘low’ (no diploma, primary school, (preparation) lower and intermediate vocational education) and ‘high’ (secondary education, higher vocational education, university). After filling out the online survey, participants received feedback about their personal scores on the psychopathology screeners.
Additional questionnaires
At the end of the survey, we asked participants if they were interested in filling out two additional questionnaires. The first was social comparison, measured by the Social Comparison Scale [42]. This scale reflects participants’ self-image, compared to native Dutch people. Lower scores correspond with feeling inferior to others. The second questionnaire is the Acculturation Scale [43]. This scale is based on Berry’s model, which measures two dimensions of acculturation: to which extent people are oriented towards the Dutch society and to what extent towards the Moroccan society. With this scale, four acculturation style can be determined: Integration (high orientation towards Dutch society, high orientation towards Moroccan society); Segregation (low orientation towards Dutch society, high orientation towards Moroccan society); Marginalization (low orientation towards Dutch society, low orientation towards Moroccan society); Assimilation (high orientation towards Dutch society, low orientation towards Moroccan society) [44]. Grouping of individuals into different acculturation styles was based on median scores within our sample [45,46].
Statistical analyses
Levels of depressive symptoms and psychotic experiences were measured on continuous scales with the K10 and the PQ-16 respectively. Proportions of participants with clinically relevant symptoms were calculated using cut-off scores as described in the literature. For the paper-and-pencil K10, the best cut-off was 22,5 for Moroccan and Turkish participants, compared to 16,5 for Dutch participants [33]. In an online Dutch population, the cut-off scores with the best sensitivity and specificity were 29, 31 and 32 [45]. We selected the most conservative cut-off score that was recommended in the online sample, which is 32 [45]. The only available cut-off score for the PQ-16 is 6, which is based on an offline sample of young adults seeking help for nonpsychotic disorders [35]. There is no other information about this instrument in an online or migrant populations.
We created sum scores for the social exclusion variables: social defeat, perceived discrimination and social support. We used Pearson correlation to evaluate the association between depressive symptoms and psychotic experiences.
For the main outcomes, we used regression analyses, consisting of three steps: In step one, we performed separate linear regression analyses for the two main outcomes: depressive symptoms (K10 sum score, continuous outcome measure) and psychotic experiences (PQ-16 sum score, continuous outcome measure). Both main outcomes were investigated in separate analyses with the variables social defeat, perceived discrimination, and social support to examine their unique contribution. These factors of social exclusion are overlapping concepts (Pearson correlation: social support and social defeat r = -0.470; social support and discrimination r = -0.312; discrimination and social defeat r = 0.287) and were therefore investigated separately. In step two, we performed multivariate linear regression, extending the previously described models with demographic parameters, using the ‘Enter’ method. The demographic parameters added were: gender (male/female) age (low <23 / high ≥ 23), migrant status (first/second generation), education (low/high). In step three, the variable social support was added to the analyses of perceived discrimination and social defeat, to investigate the hypothesized beneficial effect for social support on the outcome. We assessed whether the beta coefficient for social support was statistically significant. and evaluated whether the beta coefficients of the other social exclusion variables changed. If so, we added an interaction term to the regression model of the social exclusion variables and social support. All analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago).
Additional analyses
A subset of the participants completed additional questionnaires on social comparison and acculturation. For social comparison, the subsequent data analysis was similar as what had been done for the other variables: step one: linear regression with the dependent variables depressive symptoms and psychotic experiences; step two: multivariate linear regression including demographic parameters, and step three: adding social support. For acculturation, we created three dummy variables, based on the acculturation styles: ‘separation’, ‘assimilation’ and ‘marginalisation’. The acculturation style ‘integration’ was used as comparison. We thus examined the difference in psychopathology between integration and the three other acculturation styles. For the regression analysis, the three steps were followed, as described above.
Sensitivity analysis
Within this cross-sectional design, by definition, we do not have information about temporality of the investigated associations. We hypothesize that social exclusion is a risk factor for developing psychiatric disorders. An association in the opposite direction is a possible bias of reversed causality. We do however have information about whether participants received previous mental healthcare. When social exclusion would be the consequence of having a psychiatric disorder, it can be expected that experiences of social exclusion are higher and associations between social exclusion and symptoms are stronger within the group with previous mental health complaints compared to the group of treatment-naïve participants. To explore this possible bias, we compared the levels of social exclusion between these groups. Furthermore, we performed regression analyses for the participants with and without a history of mental healthcare, using split file analyses. We assessed whether the explained variance of the model would be higher in the group with previous treatment, compared with the treatment-naive group. Furthermore, we compared whether the strength of the associations would change in the split file analyses, comparing the beta coefficients for the total sample with the beta coefficients for the treatment-naïve group.
Results
Sample characteristics
A total of 267 participants were included in the study between November 2012 and august 2014, see flow-chart in Fig 1. 87% (N = 231) of the participants were female. 81% were second generation Moroccan migrant, meaning they were born in the Netherlands and one or both of the participants’ parents were born in Morocco. The remaining 19% were first generation migrant. The mean age of the participants was 24,5 years (range 18–57). 27% percent of the sample received mental healthcare in the past. Demographic variables are shown in Table 1.
Fig 1. Flow-chart participants.
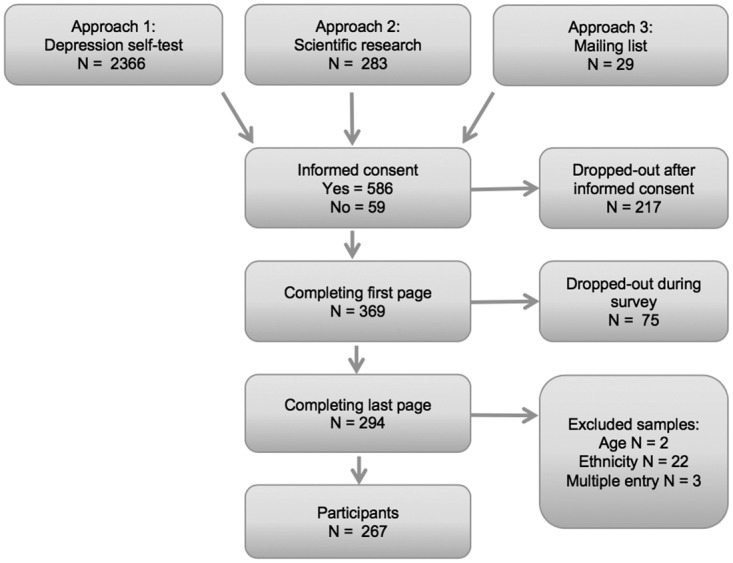
Table 1. Demographic information, psychiatric symptoms and measures of social exclusion.
| Demographic information | Number | Percentage | |
| Female gender | 226 | 86.6% | |
| Second generation migrant | 211 | 80.8% | |
| Previous mental healthcare treatment | 69 | 27.2% | |
| Higher education | 76 | 29.5% | |
| Median | Mean | Std. Dev. | |
| Age (range 18–57) | 23 | 24,5 | 6,7 |
| Symptoms | |||
| Depressive symptoms (range 10–50) | 33 | 32 | 9,6 |
| Psychotic experiences (range 0–16) | 6 | 6 | 4 |
| Social Exclusion | |||
| Social defeat (range 20–80) | 55 | 54 | 16 |
| Perceived discrimination (range 9–36) | 20 | 20 | 6,7 |
| Social support (Z-scores range -4,32–4,88) | 0.016 | -0,096 | 2,3 |
Measures: K10 (depressive symptoms); PQ-16 (psychotic experiences); Social Defeat Scale; Everyday Discrimination Scale, Oslo Social Support Questionnaire.
‘lower education’ (no diploma, primary school, (preparation) lower and intermediate vocational education); ‘higher education’ (secondary education, higher vocational education, university).
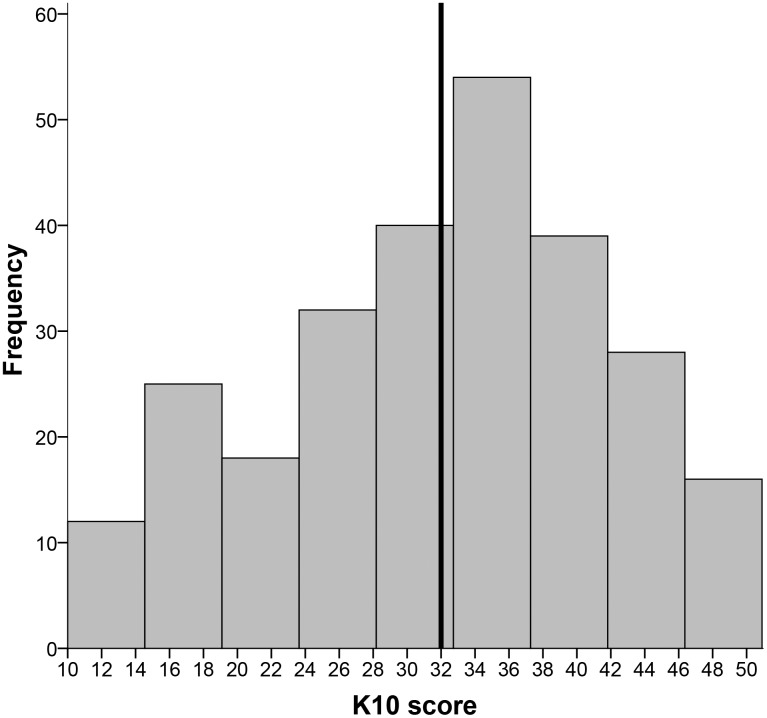
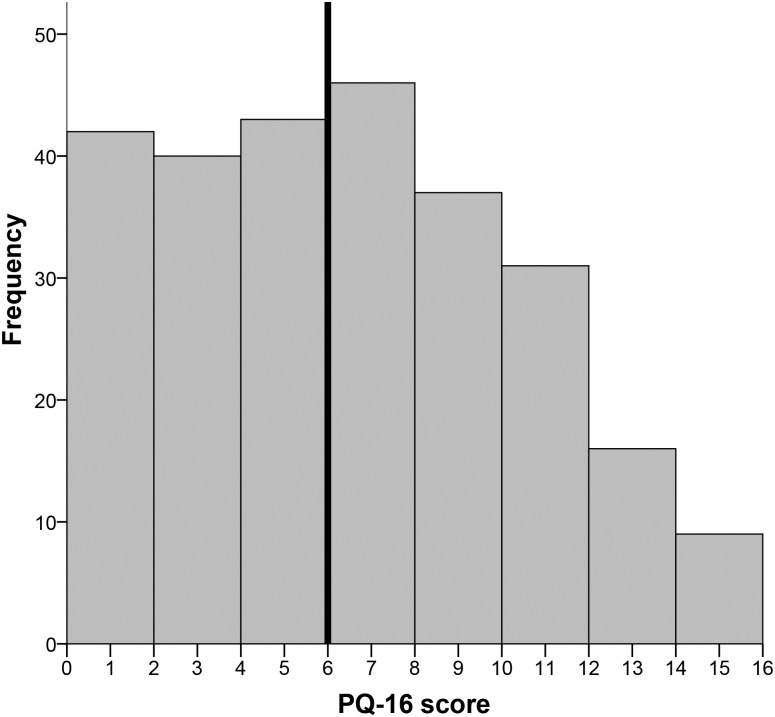
The median score on the K10 (depressive symptoms) was 33, which means that over 50% of the sample scores above the cut-off for depression, see Fig 2. The median score for the PQ-16 (psychotic experiences) was 6, which means that 50% scores above the cut-off for psychotic experiences, see Fig 3. Pearson correlation analysis showed a high correlation between depressive symptoms and psychotic experiences (r = .551, p <0.01).
Fig 2. Distribution of depressive symptoms.
Fig 3. Distribution of psychotic experiences.
Social exclusion and psychiatric symptoms
Reports of social defeat and perceived discrimination were associated with more psychotic and depressive symptoms. Higher level of social support, on the other hand, predicted less psychotic experiences and depressive symptoms, see Table 2.
Table 2. Results of regression analyses into the associations between psychiatric symptoms and experiences of social exclusion.
| Psychotic experiences | Depressive symptoms | ||||||
|---|---|---|---|---|---|---|---|
| social support | predictor | beta | adjusted R2 | social support | predictor | beta | adjusted R2 |
| model 1*** | social support | -0.252*** | 0.060 | model 1*** | social support | -0.383*** | 0.143 |
| model 2*** | social support | -0.221*** | 0.148 | model 2*** | social support | -0.363*** | 0.180 |
| education | -0.310*** | education | -0.184** | ||||
| age | 0.156* | ||||||
| social defeat | social defeat | ||||||
| model 1*** | social defeat | 0.535*** | 0.284 | model 1*** | social defeat | 0.725*** | 0.524 |
| model 2*** | social defeat | 0.490*** | 0.334 | model 2*** | social defeat | 0.718*** | 0.545 |
| model 3*** | social defeat | 0.503*** | 0.332 | model 3*** | social defeat | 0.708*** | 0.543 |
| social support | 0.024 | social support | -0.020 | ||||
| education | -0.226*** | age | 0.183*** | ||||
| first/second generation | 0.113* | ||||||
| perceived discrimination | perceived discrimination | ||||||
| model 1*** | discrimination | 0.257*** | 0.062 | model 1** | discrimination | 0.179*** | 0.028 |
| model 2*** | discrimination | 0.251*** | 0.161 | model 2** | discrimination | 0.187** | 0.082 |
| model 3*** | discrimination | 0.197** | 0.179 | model 3*** | discrimination | 0.070 | 0.181 |
| social support | -0.154* | social support | -0.339*** | ||||
| education | -0.316*** | education | -0.186** | ||||
| age | 0.159* | ||||||
| Interaction analysis | Discrimination x social support | 0.077# | 0.176 | ||||
model 1: unadjusted;
model 2: adjusted for age, gender, education, first/second generation migrant;
model 3: adjusted + social support
* p < 0.05;
** p < 0.01;
*** p < 0.001;
# p = 0.670
When demographic variables were added to the regression models, associations between the social exclusion factors (social defeat, discrimination and social support) and symptoms (psychotic experiences and depressive symptoms) all remained statistically significant. Higher education reduced the impact of social exclusion on levels of symptoms, higher age contributed to associations between all social exclusion factors and depressive symptoms. Compared to first generation migrants, being a second-generation migrant was a significant factor in the regression model of social defeat as predictor of depressive symptoms.
Adding social support to the model did not change the association between social defeat and depressive symptoms nor the association between social defeat and psychotic experiences. Social support was statistically significant in the regression model of perceived discrimination and psychotic experiences. The explained variance improved slightly (adjusted R2 = 0.179 with social support versus 0.161 without, R2 change 0.021, p = 0.013) and the beta coefficient for discrimination decreased somewhat (0.197 with social support versus 0.251). The association between perceived discrimination and depressive symptoms was not significant anymore when social support was added, and the explained variance of the model improved (adjusted R2 = 0.181 with social support versus 0.082 without, R2 change 1.000, p < 0.001). We added an interaction term for discrimination and social support to the model. There was no moderation effect of social support on the relationship between discrimination and depressive symptoms.
Social comparison and acculturation
The additional questionnaires about social comparison and acculturation were completed by a subset of 111 participants. Compared to the participants who did not continue with the additional questions, they were older (26 versus 23 years, p <0.01). There were no significant differences in gender, previous treatment, depressive symptoms and psychotic experiences.
Integration was the most common acculturation style (N = 38, 34%), followed by segregation (N = 32, 29%) assimilation (N = 27, 24%), and marginalization (N = 14, 13%). Levels of depressive symptoms and psychotic experiences did not differ significantly between acculturation styles.
On the social comparison scale, a lower score means a more negative self-image compared to Dutch natives. In the regression analysis with the K10 score, a negative self-image was associated with more depressive symptoms, also when adjusted for demographic parameters (beta -0.306; p = 0.001). Both social support (beta -0.207; p = 0.021) and education (beta -0.272; p = 0.001) were associated with less depressive symptoms. In the regression analysis with the PQ-16 score, a more negative self-image was associated with psychotic experiences (beta -0.204, p = 0.019), but this effect disappeared when social support was added to the model, although social support itself was also not significantly associated. Only education remained a significant protective factor in the analysis for psychotic experiences (beta -0.354; p < 0.001). Results of the regression analysis are shown in Table 3.
Table 3. Results of regression analysis into the associations between psychotic experiences, depressive symptoms and social comparison.
| N | Median | Mean | Std. dev. | |
|---|---|---|---|---|
| Social comparison | 118 | 63 | 63,1 | 22,2 |
| Regression analyses | ||||
| Psychotic experiences | predictor | beta | adjusted R2 | |
| model 1*** | -0.267** | 0.063 | ||
| model 2*** | -0.204* | 0.179 | ||
| model 3*** | social comparison | -0.138 | 0.193 | |
| higher education | -0.359*** | |||
| Depressive symptoms | predictor | beta | adjusted R2 | |
| model 1*** | -0.422*** | 0.171 | ||
| model 2*** | -0.391*** | 0.267 | ||
| model 3*** | social comparison | -0.306** | 0.295 | |
| higher education | -0.272** | |||
| social support | -0.207* | |||
model 1: unadjusted;
model 2: adjusted for age, gender, education, first/second generation migrant;
model 3: adjusted + social support
* p < 0.05;
** p < 0.01;
*** p < 0.001
Sensitivity analysis
We compared the measures of social exclusion between the groups with and without previous mental healthcare. There were no significant differences in the scores on social defeat, discrimination and social support, suggesting that levels of social exclusion were not a consequence of any mental health problems. The regression analyses were performed again, using split file, based on previous use of mental healthcare. For all models, the adjusted R2-value was higher in the group without a history of previous mental healthcare, compared to the group with previous mental healthcare. This shows that the models have a better fit in the treatment-naive group. Furthermore, the betas of the explaining variables did not change in the group without a history of previous mental healthcare.
Discussion
In this online study, over 50% of young Moroccan-Dutch young adults reported depressive symptoms and 50% reported psychotic experiences. Social defeat and perceived discrimination were associated with more psychotic experiences, and social defeat was associated with more depressive symptoms. Social support and higher level of education were associated with lower level of depressive symptoms and psychotic experiences. However, social support did not decrease the effect of perceived discrimination and social defeat.
The rates of reported psychiatric symptoms are high. This is especially remarkable for psychotic experiences, since 87% of the studied participants were women, whereas the increased incidence of psychotic disorders in migrants has to our knowledge only been reported in men [3]. The high rates of psychiatric symptoms suggest that we reached people who may have a need for (professional) support. Since the Moroccan-Dutch population is already at increased risk for developing psychiatric disorders, early intervention for psychiatric symptoms might have important beneficial effects. However, while the measures that we used, the K10 and PQ-16, are valid screening instruments for depressive disorder and for risk of psychotic disorder respectively, they do not give enough information to assess actual need for care. To overcome this, a high score on the K10 and PQ-16 instruments, combined with another instrument that can assess the needs for care, might enable online identification of individuals that would benefit from intervention. For psychotic experiences, we checked whether it would be more informative to (also) use the impact scale of the PQ-16, but this did not change results.
Social support was a protective factor for both depressive symptoms and psychotic experiences, but it did not diminish the effect of the risk factors. This is in line with two overview articles, which reported that social support in most studies did not have a buffering effect on the association between perceived discrimination and depressive symptoms [47,48], although it did have a protective effect on depression itself [48]. A recent study found a buffering effect for having many same-ethnicity friends in several populations, but not in Moroccan-Dutch migrants [21]. The online forum website Marokko.nl itself can also be a source of social support and is sometimes used to share private stories and receive support. Although this will help some people with mild symptoms, it will probably not be a sufficient intervention for people with more severe symptoms or who experience more negative social factors, like discrimination.
Higher education was a protective factor for both depressive symptoms and psychotic experiences. In previous studies, lower level of education was one of the indicators of social disadvantage which was associated with psychotic disorder [49] and was associated with higher level of depressive and/or anxiety disorders [50]. This finding is not limited to mixed or migrant populations [51,52]. Our interpretation is that a higher level of education is associated with better social integration (starting in school), better job perspectives, and therefore less social exclusion.
We found high rates of psychiatric symptoms in this sample (with 87% being females). Although Moroccan-Dutch people in general are not underrepresented in mental healthcare, there are gender differences. Moroccan-Dutch males use mental healthcare more often than Dutch males, whereas Moroccan-Dutch females use mental healthcare less often then Dutch females [53]. In a study into the perceived mental healthcare needs in migrants, Moroccan-Dutch people reported a low perceived need for regular care. The suggested explanation is that the Moroccan-Dutch population is a relatively conservative community, in which mental healthcare problems are more often attributed to traditional explanations, such as being possessed by a spirit, and help is also sought from traditional healers [54]. In a qualitative study in Israel, it was found that young Moroccan females felt they were part of the Western society, but that they suffered from an internal conflict between this western world and their traditional background. This increased their fear for stigma, and consequently decreased the probability that they would seek psychiatric help [55].
Given the high burden of psychiatric symptoms and the mismatch between mental healthcare and Moroccan-Dutch females, this population can benefit from an alternative way of offering help. Since we recruited our sample in an online community, it is logical to use the Internet to reach this at risk population for treatment purposes. Furthermore, the online environment is anonymous, which diminishes the fear for stigmatisation. On the website Marokko.nl, people indeed anonymously discuss mental health problems. We therefore created an add-on website to Marokko.nl, to deliver information about psychiatric disorders and traditional explanations, like being possessed, self-tests for depression and substance abuse and provided email contacts with healthcare workers and specially trained Imams [56]. The online setting enabled us to create this platform with a culturally sensitive look-and-feel, which helps to connect with the target population. Also for future interventions, this may help to fit the needs of Moroccan-Dutch females better. An online intervention would best fit with our results when it aims to increase the resilience for negative social factors, increase the access to social resources, and improve the social identity of participants. Since anonymity is important, we recommend an ‘online-only’ e-health intervention, in contrast to the frequent finding that blended care has better results [57–59]. An example is the web-based intervention ‘GET.ON Mood Enhancer Prevention training’, which consists of six interactive sessions and an online trainer [60]. Another possibility is mindfulness training, which focusses on increasing resilience in many different situations and problems and can be performed without guidance [61]. A one-session only intervention could be based on online contact with mental healthcare workers (chat, WhatsApp or email), in which the mental healthcare worker can explore the problems and social context of the person and deliver tailored support.
Our study has several strengths and limitations. A strength of our study is that we used different measures of social exclusion to investigate their association with depressive symptoms and psychotic experiences. This resulted in associations with great consistency: all in the same, hypothesized, direction. Our results in this online population extend on previous studies, which have described the link between social factors and psychotic disorder or depression in conventional study designs. Our findings should be viewed in the context of several limitations. Most of them are related to the online recruitment strategy. We collected a convenience sample and the cohort was collected based on self-selection, which leads to bias. Recruitment with the depression self-test probably will attract participants with depressive symptoms. Indeed, we found that the K10 score was significantly higher in the self-test subgroup compared to the research subgroup (35 vs 28). However, this means that also in the other group, 37% scored above the cut-off for depressive symptoms. Differences between the recruitment strategies in all variables are presented in the supplemental material, see S1 Table. Another example of self-selection is that 26% of the participants has received psychiatric treatment. In a Danish study, the cumulative risk for psychiatric treatment was 23% for males and 25% for females at age 50 [62]. In our study the mean age is 24,5 years, meaning that people with a history of psychiatric treatment are overrepresented in our sample. Another example of self-selection bias in our sample is that 87% of our participants were female (compared to 51% of the Marokko.nl users). Underrepresentation of males is reported in several other [63–66], but not all [26] online (mental health) studies. Women may be more interested in this type of research, but it cannot be excluded that Moroccan-Dutch males are for some reason less likely to participate in online mental health surveys than Dutch males would be. Interestingly, previous studies have reported high levels of psychopathology in Moroccan-Dutch men and not in Moroccan-Dutch women for psychotic disorder [3,67] and depressive disorder. High rates of psychiatric symptoms within the female Moroccan-Dutch population are thus a new finding. Furthermore, the 267 participants are just a small percentage of the > 2000 people who filled out the depression self-test and these 267 samples reflect 40% of the people who gave informed consent for the study. This self-selection bias decreases the generalizability of our study results. With online recruitment, it is not possible to collect a probability sample [68]. Incidence or prevalence figures can therefore not be calculated; we can only report that psychopathology scores are high, compared to cut-off scores from the literature. Furthermore, the PQ-16 for psychotic experiences was not designed for a migrant population, and not for a population that is not help-seeking. This can affect the interpretation of items by participants and the cut-off score, possibly leading to an overestimation of the psychotic experiences in our cohort. In our cross-sectional study, we did not collect information about the temporal relationship between social exclusion and psychopathology. We are therefore not able to prove causality. However, some longitudinal studies have shown that perceived discrimination precedes depression [69–71]. Furthermore, we compared the group with and without previous psychiatric treatment in the sensitivity analysis and we did not find evidence for reversed causality.
Due to the quantitative nature of our study, we have limited information about the mechanism behind the identified associations. We would like to know how participants reflect on the negative effect of social exclusion on their mental wellbeing, since awareness of this association could be the first step to increase empowerment and reduce the disease burden. We therefore are currently preparing a qualitative study, to further explore the perception of participants about the association between social exclusion and psychopathology.
Our study shows that the Moroccan-Dutch experience social exclusion and that this experience is related to their mental wellbeing. Within the Dutch society, there are currently strong antimigrant and anti-Muslim sentiments, which increase feelings of social exclusion. Furthermore, when psychopathology is already present, stigmatisation can result in further social exclusion. Preventive measures should aim to improve the development of a positive social identity in ethnic minorities, given the current negative social context. On the society level, we would like to emphasize the importance of social cohesion to improve mental wellbeing. Ethnic minority organisations can enhance social cohesion within migrant populations as well as between ethnic groups in the Netherlands, which can be stimulated by governmental funding programmes. Finally, it is important to stimulate initiatives to destigmatise mental health problems. An important measure to decrease stigma is delivering adequate information and approachable support, adapted to the migrant population.
Supporting information
(DOCX)
(PDF)
(DOCX)
Data Availability
Privacy restrictions prevent us from publicly sharing the raw dataset. Data are available upon request for other researchers by contacting the corresponding author or at the following institutional address: Commission scientific research, Dimence Groep; Tav Diana Westerkamp; Burg. Roelenweg 9; Postbus 473; 8000 AL Zwolle; The Netherlands; onderzoek@dimencegroep.nl.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41: 897–910. doi: 10.1017/S0033291710001406 [DOI] [PubMed] [Google Scholar]
- 2.Cantor-Graae E, Selten JP. Schizophrenia and migration: A meta-analysis and review. Am J Psychiatry. 2005;162: 12–24. doi: 10.1176/appi.ajp.162.1.12 [DOI] [PubMed] [Google Scholar]
- 3.van der Ven E, Veling W, Tortelli A, Tarricone I, Berardi D, Bourque F, et al. Evidence of an excessive gender gap in the risk of psychotic disorder among North African immigrants in Europe: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. Springer Berlin Heidelberg; 2016; doi: 10.1007/s00127-016-1261-0 [DOI] [PubMed] [Google Scholar]
- 4.Swinnen SGHA, Selten JP. Mood disorders and migration: Meta-analysis. Br J Psychiatry. 2007;190: 6–10. doi: 10.1192/bjp.bp.105.020800 [DOI] [PubMed] [Google Scholar]
- 5.Missinne S, Bracke P. Depressive symptoms among immigrants and ethnic minorities: A population based study in 23 European countries. Soc Psychiatry Psychiatr Epidemiol. 2012;47: 97–109. doi: 10.1007/s00127-010-0321-0 [DOI] [PubMed] [Google Scholar]
- 6.Levecque K, Lodewyckx I, Vranken J. Depression and generalised anxiety in the general population in Belgium: a comparison between native and immigrant groups. J Affect Disord. 2007;97: 229–239. doi: 10.1016/j.jad.2006.06.022 [DOI] [PubMed] [Google Scholar]
- 7.Cantor-Graae E, Pedersen CB. Full Spectrum of Psychiatric Disorders Related to Foreign Migration. JAMA Psychiatry. 2013;70: 427 doi: 10.1001/jamapsychiatry.2013.441 [DOI] [PubMed] [Google Scholar]
- 8.Veling W, Selten JP, Mackenbach JP, Hoek HW. Symptoms at first contact for psychotic disorder: Comparison between native Dutch and ethnic minorities. Schizophr Res. 2007;95: 30–38. doi: 10.1016/j.schres.2007.06.024 [DOI] [PubMed] [Google Scholar]
- 9.Selten JP, Laan W, Kupka R, Smeets HM, van Os J. Risk of psychiatric treatment for mood disorders and psychotic disorders among migrants and Dutch nationals in Utrecht, The Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2012;47: 271–278. doi: 10.1007/s00127-010-0335-7 [DOI] [PubMed] [Google Scholar]
- 10.de Wit MAS, Tuinebreijer WC, Dekker J, Beekman A-JTF, Gorissen WHM, Schrier AC, et al. Depressive and anxiety disorders in different ethnic groups: A population based study among native Dutch, and Turkish, Moroccan and Surinamese migrants in Amsterdam. Soc Psychiatry Psychiatr Epidemiol. 2008;43: 905–912. doi: 10.1007/s00127-008-0382-5 [DOI] [PubMed] [Google Scholar]
- 11.Veling W, Hoek HW, Selten JP, Susser E. Age at migration and future risk of psychotic disorders among immigrants in the Netherlands: A 7-year incidence study. Am J Psychiatry. 2011;168: 1278–1285. doi: 10.1176/appi.ajp.2011.11010110 [DOI] [PubMed] [Google Scholar]
- 12.van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. 2010;468: 203–212. doi: 10.1038/nature09563 [DOI] [PubMed] [Google Scholar]
- 13.Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: Toward a sociodevelopmental model. Schizophr Bull. 2010;36: 655–664. doi: 10.1093/schbul/sbq051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veling W. Ethnic minority position and risk for psychotic disorders. Curr Opin Psychiatry. 2013;26: 166–171. doi: 10.1097/YCO.0b013e32835d9e43 [DOI] [PubMed] [Google Scholar]
- 15.Janssen I, Hanssen M, Bak M, Bijl R V., De Graaf R, Vollebergh W, et al. Discrimination and delusional ideation. Br J Psychiatry. 2003;182: 71–76. doi: 10.1192/bjp.182.1.71 [DOI] [PubMed] [Google Scholar]
- 16.Veling W, Selten JP, Susser E, Laan W, Mackenbach JP, Hoek HW. Discrimination and the incidence of psychotic disorders among ethnic minorities in The Netherlands. Int J Epidemiol. 2007;36: 761–768. doi: 10.1093/ije/dym085 [DOI] [PubMed] [Google Scholar]
- 17.Karlsen S, Nazroo JY, McKenzie K, Bhui K, Weich S. Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychol Med. 2005;35: 1795–1803. doi: 10.1017/S0033291705005830 [DOI] [PubMed] [Google Scholar]
- 18.Van Dijk TK, Agyemang C, De Wit M, Hosper K. The relationship between perceived discrimination and depressive symptoms among young Turkish-Dutch and Moroccan-Dutch. Eur J Public Health. 2011;21: 477–483. doi: 10.1093/eurpub/ckq093 [DOI] [PubMed] [Google Scholar]
- 19.Wamala S, Bostrom G, Nyqvist K. Perceived discrimination and psychological distress in Sweden. Br J Psychiatry. 2007;190: 75–76. doi: 10.1192/bjp.bp.105.021188 [DOI] [PubMed] [Google Scholar]
- 20.Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc Sci Med. 2007;64: 1984–1996. doi: 10.1016/j.socscimed.2007.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ikram UZ, Snijder MB, de Wit MAS, Schene AH, Stronks K, Kunst AE. Perceived ethnic discrimination and depressive symptoms: the buffering effects of ethnic identity, religion and ethnic social network. Soc Psychiatry Psychiatr Epidemiol. 2016;51: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilbert P, Allan S. The role of defeat and entrapment (arrested flight) in depression: an exploration of an evolutionary view. Psychol Med. 1998;28: 585–598. [DOI] [PubMed] [Google Scholar]
- 23.Cantor-Graae E. The contribution of social factors to the development of schizophrenia: a review of recent findings. Can J Psychiatry. 2007;52: 277–286. doi: 10.1177/070674370705200502 [DOI] [PubMed] [Google Scholar]
- 24.Selten JP, Cantor-Graae E. Social defeat: Risk factor for schizophrenia? Br J Psychiatry. 2005;187: 101–102. doi: 10.1192/bjp.187.2.101 [DOI] [PubMed] [Google Scholar]
- 25.Taylor PJ, Gooding P, Wood AM, Tarrier N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychol Bull. 2011;137: 391–420. Available: http://search.ebscohost.com/login.aspx?direct=true&db=pdh&AN=bul-137-3-391&site=ehost-live&scope=site doi: 10.1037/a0022935 [DOI] [PubMed] [Google Scholar]
- 26.Jaya ES, Lincoln TM. Social adversities and psychotic symptoms: A test of predictions derived from the social defeat hypothesis. Psychiatry Res. 2016;245: 466–472. doi: 10.1016/j.psychres.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 27.Kuo BCH, Chong V, Joseph J. Depression and its psychosocial correlates among older Asian immigrants in North America: a critical review of two decades’ research. J Aging Health. 2008;20: 615–52. doi: 10.1177/0898264308321001 [DOI] [PubMed] [Google Scholar]
- 28.Van Os J. The dynamics of subthreshold psychopathology: Implications for diagnosis and treatment. Am J Psychiatry. 2013;170: 695–698. doi: 10.1176/appi.ajp.2013.13040474 [DOI] [PubMed] [Google Scholar]
- 29.Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F, et al. The psychosis at risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70: 107–120. doi: 10.1001/jamapsychiatry.2013.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGorry P. Transition to adulthood: The critical period for pre-emptive, disease-modifying care for schizophrenia and related disorders. Schizophr Bull. 2011;37: 524–530. doi: 10.1093/schbul/sbr027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Federal Statistical Office. Population—Key Figures. In: Centraal Bureau voor de Statistiek [Internet]. The Hague / Heerlen; 2016. http://statline.cbs.nl/Statweb/publication/?VW=T&DM=SLEN&PA=37325eng&D1=a&D2=0&D3=0&D4=0&D5=0-4,139,145,216,231&D6=0,4,9,14,(l-1),l&HD=161003-1222&HDR=G2,G1,G3,T&STB=G4,G5
- 32.van de Beek MH, van der Krieke L, Schoevers RA. Migrants Examined for Determinants of psychopathology through INternet Assessment (MEDINA) study: a cross-sectional study among visitors of an Internet community. BMJ Open. 2014;4: e003980 doi: 10.1136/bmjopen-2013-003980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32: 959–976. [DOI] [PubMed] [Google Scholar]
- 34.Fassaert T, De Wit MA, Tuinebreijer WC, Wouters H, Verhoeff AP, Beekman AT, et al. Psychometric properties of an interviewer-administered version of the Kessler Psychological Distress scale (K10) among Dutch, Moroccan and Turkish respondents. Int J Methods Psychiatr Res. 2009;18: 159–168. doi: 10.1002/mpr.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Donker T, Comijs H, Cuijpers P, Terluin B, Nolen W, Zitman F, et al. The validity of the Dutch K10 and extended K10 screening scales for depressive and anxiety disorders. Psychiatry Res. 2010;176: 45–50. doi: 10.1016/j.psychres.2009.01.012 [DOI] [PubMed] [Google Scholar]
- 36.Ising HK, Veling W, Loewy RL, Rietveld MW, Rietdijk J, Dragt S, et al. The validity of the 16-item version of the Prodromal Questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr Bull. 2012;38: 1288–1296. doi: 10.1093/schbul/sbs068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ikram UZ, Snijder MB, Fassaert TJL, Schene AH, Kunst AE, Stronks K. The contribution of perceived ethnic discrimination to the prevalence of depression. Eur J Public Health. 2015;25: 243–248. doi: 10.1093/eurpub/cku180 [DOI] [PubMed] [Google Scholar]
- 38.Williams DR, Yan Y, Jackson J, Anderson N. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol. 1997;2: 335–51. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- 39.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61: 1576–1596. doi: 10.1016/j.socscimed.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 40.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived in the United States. J Health Soc Behav. 1999;40: 208–230. doi: 10.2307/2676349 [PubMed] [Google Scholar]
- 41.Meltzer H. Development of a common instrument for mental health. EUROHIS Dev common instruments Heal Surv; 2003; 35–60. [Google Scholar]
- 42.Allan S, Gilbert P. A social comparison scale: Psychometric properties and relationship to psychopathology. Pers Individ Dif. 1995;19: 293–299. Available: http://www.sciencedirect.com/science/article/pii/019188699500086L [Google Scholar]
- 43.Instituut voor Sociale Geneeskunde. Acculturatieschaal. 2004.
- 44.Berry JW. Acculturation: Living successfully in two cultures. Int J Intercult Relations. 2005;29: 697–712. doi: 10.1016/j.ijintrel.2005.07.013 [Google Scholar]
- 45.Celenk O, Van De Vijver FJR. Assessment of Acculturation: Issues and Overview of Measures. Online Readings Psychol Cult. 2011;8 Available: http://dx.doi.org/10.9707/ [Google Scholar]
- 46.Berry JW. Immigration, acculturation and adaptation. Appl Psychol. 1997;46: 5–34. Available: http://onlinelibrary.wiley.com/doi/10.1111/j.1464-0597.1997.tb01087.x/pdf [Google Scholar]
- 47.Pascoe EA, Richman LS. Perceived discrimination and health: A meta-analytic review. Psychol Bull. 2009;135: 531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brondolo E, Ver Halen NB, Pencille M, Beatty D, Contrada RJ. Coping With Racism: A Selective Review of the Literature and a Theoretical and Methodological Critique. J Behav Med. 2012;32: 64–88. doi: 10.1007/s10865-008-9193-0 Coping [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morgan C, Kirkbride J, Hutchinson G, Craig T, Morgan K, Dazzan P, et al. Cumulative social disadvantage, ethnicity and first-episode psychosis: a case-control study. Psychol Med. 2008;38: 1701 doi: 10.1017/S0033291708004534 [DOI] [PubMed] [Google Scholar]
- 50.de Wit MA, Tuinebreijer WC, Dekker J, Beekman AJ, Gorissen WH, Schrier AC, et al. Depressive and anxiety disorders in different ethnic groups: a population based study among native Dutch, and Turkish, Moroccan and Surinamese migrants in Amsterdam. Soc Psychiatry Psychiatr Epidemiol. 2008;43: 905–912. doi: 10.1007/s00127-008-0382-5 [DOI] [PubMed] [Google Scholar]
- 51.Johns LC, Cannon M, Singleton N, Murray RM, Farrell M, Brugha T, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185: 298–305. doi: 10.1192/bjp.185.4.298 [DOI] [PubMed] [Google Scholar]
- 52.Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med. 2008;66: 1334–1345. [DOI] [PubMed] [Google Scholar]
- 53.Van ‘t Land H, Grolleman J, Mutsaers K, Smits C. Trendrapportage GGZ 2008 [Internet]. Utrecht; 2008. http://www.nvag.nl/afbeeldingen/Bibliotheek/OGGZAlgemeen/trendrapportggzdeel2toegangenzorggebruik.pdf
- 54.Fassaert T, de Wit MA, Tuinebreijer WC, Verhoeff AP, Beekman AT, Dekker J. Perceived need for mental health care among non-western labour migrants. Soc Psychiatry Psychiatr Epidemiol. 2009;44: 208–216. doi: 10.1007/s00127-008-0418-x [DOI] [PubMed] [Google Scholar]
- 55.Latzer Y. Traditional versus Western perceptions of mental illness: women of Moroccan origin treated in an Israeli mental health center. J Soc Work Pract. 2003;17: 77–94. [Google Scholar]
- 56.van de Beek MH, van der Krieke L, Schoevers RA. Online mental health platform for Moroccan-Dutch in the Netherlands. Psychiatr Serv. 2013;64: 1178 doi: 10.1176/appi.ps.6401102 [DOI] [PubMed] [Google Scholar]
- 57.Andersson G, Cuijpers P. Internet-Based and Other Computerized Psychological Treatments for Adult Depression: A Meta-Analysis. Cogn Behav Ther. 2009;38: 196–205. doi: 10.1080/16506070903318960 [DOI] [PubMed] [Google Scholar]
- 58.Johansson R, Andersson G. Expert Review of Neurotherapeutics Internet-based psychological treatments for depression. Expert Rev Neurother. 2012;127: 861–870. [DOI] [PubMed] [Google Scholar]
- 59.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: Is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011;31: 89–103. doi: 10.1016/j.cpr.2010.09.008 [DOI] [PubMed] [Google Scholar]
- 60.Buntrock C, Ebert DD, Lehr D, Smit F, Riper H, Berking M, et al. Effect of a Web-Based Guided Self-help Intervention for Prevention of Major Depression in Adults With Subthreshold Depression: A Randomized Clinical Trial. Jama. 2016;315: 1854–1863. doi: 10.1001/jama.2016.4326 [DOI] [PubMed] [Google Scholar]
- 61.Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2016;45: 102–114. doi: 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 62.Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA psychiatry. 2014;71: 573–581. doi: 10.1001/jamapsychiatry.2014.16 [DOI] [PubMed] [Google Scholar]
- 63.Lara DR, Ottoni GL, Brunstein MG, Frozi J, De Carvalho HW, Bisol LW. Development and validity data of the Brazilian Internet Study on Temperament and Psychopathology (BRAINSTEP). J Affect Disord. Elsevier B.V.; 2012;141: 390–398. doi: 10.1016/j.jad.2012.03.011 [DOI] [PubMed] [Google Scholar]
- 64.Brouwer W, Kroeze W, Crutzen R, de Nooijer J, de Vries NK, Brug J, et al. Which Intervention Characteristics are Related to More Exposure to Internet-Delivered Healthy Lifestyle Promotion Interventions? A Systematic Review. J Med Internet Res. Journal of Medical Internet Research; 2011;13: e2 doi: 10.2196/jmir.1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Van ‘t Riet J, Crutzen R, De Vries H. Investigating Predictors of Visiting, Using, and Revisiting an Online Health-Communication Program: A Longitudinal Study. J Med Internet Res. Journal of Medical Internet Research; 2010;12: e37 doi: 10.2196/jmir.1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rice RE. Influences, usage, and outcomes of Internet health information searching: Multivariate results from the Pew surveys. Int J Med Inform. 2006;75: 8–28. doi: 10.1016/j.ijmedinf.2005.07.032 [DOI] [PubMed] [Google Scholar]
- 67.Veling W, Selten JP, Veen N, Laan W, Blom JD, Hoek HW. Incidence of schizophrenia among ethnic minorities in the Netherlands: a four-year first-contact study. Schizophr Res. 2006;86: 189–193. doi: 10.1016/j.schres.2006.06.010 [DOI] [PubMed] [Google Scholar]
- 68.Van Selm M, Jankowski N. Conducting Online Surveys. Quality & Quantity. 2006. pp. 435–456. [Google Scholar]
- 69.Pavalko EK, Mossakowski KN, Hamilton VJ. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women’s physical and emotional health. J Health Soc Behav. 2003;44: 18–33. Available: http://www.ncbi.nlm.nih.gov/pubmed/12751308 [PubMed] [Google Scholar]
- 70.Brown TN, Williams DR, Jackson JS, Neighbors HW, Torres M, Sellers SL, et al. “Being black and feeling blue”: the mental health consequences of racial discrimination. Race Soc. 2000;2: 117–131. doi: 10.1016/S1090-9524(00)00010-3 [Google Scholar]
- 71.Gee G, Walsemann K. Does health predict the reporting of racial discrimination or do reports of discrimination predict health? Findings from the National Longitudinal Study of Youth. Soc Sci Med. Elsevier Ltd; 2009;68: 1676–1684. doi: 10.1016/j.socscimed.2009.02.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(PDF)
(DOCX)
Data Availability Statement
Privacy restrictions prevent us from publicly sharing the raw dataset. Data are available upon request for other researchers by contacting the corresponding author or at the following institutional address: Commission scientific research, Dimence Groep; Tav Diana Westerkamp; Burg. Roelenweg 9; Postbus 473; 8000 AL Zwolle; The Netherlands; onderzoek@dimencegroep.nl.