Abstract
Background/Aims
Gastric motility abnormalities have been considered to be pathophysiological features of functional dyspepsia (FD) that are closely related to dyspepsia symptoms, especially postprandial distress syndrome (PDS). The aims of this study are to (1) investigate the prevalence of gastric motility disorders and (2) evaluate the association between gastric motility abnormalities and dyspeptic symptoms using gastric scintigraphy in the PDS type of FD.
Methods
Forty healthy subjects and 94 PDS type FD patients were enrolled in the study. The volunteers and patients ingested a radiolabeled (technetium-99m) solid test meal, and scintigraphic images were recorded. Gastric accommodation and emptying were assessed by scintigraphic imaging. The patients’ dyspeptic symptoms were also explored using self-completed symptom questionnaires with 10 variables (4 scales, 0–3 points) at the same time.
Results
In 94 Japanese FD patients, the prevalence of impaired gastric accommodation and delayed emptying were 14.9% (14/94) and 10.6% (10/94), respectively. Gastric motility abnormalities were seen in 25.5% (24/94) of FD patients. There was no association between gastric motility abnormalities and dyspeptic symptoms.
Conclusions
Gastric motility abnormalities were seen in 25.5% of Japanese PDS type FD patients. However, there was no association between gastric motility abnormalities and dyspeptic symptoms on gastric scintigraphy.
Keywords: Dyspepsia, Motility, Prevalence, Stomach
Introduction
Functional dyspepsia (FD) is a non-organic disease that is nonetheless accompanied by chronic upper gastrointestinal symptoms, including indigestion and stomach pain. FD is classified into 2 types depending on the association of upper gastrointestinal symptoms with dietary intake: (1) postprandial distress syndrome (PDS), which is seen in those who experience indigestion after meals and early satiety, and (2) epigastric pain syndrome (EPS), which is seen in those who experience epigastric pain and epigastric burning. PDS is a commonly reported type of FD in Asia.1–3
PDS is reported to be associated with gastric motility abnormalities, and reports to date have described a gastric emptying disorder in about 20–50% and an adaptive relaxation disorder in about 40% of FD patients.4,5
The association between the prevalence of gastric motility abnormalities and upper gastrointestinal symptoms currently remains unclear in many Asian PDS patients. In this study, the gastric scintigraphic images of 94 Japanese PDS type FD patients diagnosed by the Rome III criteria were used to clarify the association between the prevalence of gastric motility abnormalities, including impaired gastric accommodation and delayed emptying and the patients’ dyspeptic symptoms.6
Materials and Methods
Study design
This study was a prospective observational study at a single facility. Ninety-four PDS type FD patients diagnosed by the Rome III criteria as having chronic “indigestion” and “early satiety” following a visit to our outpatient clinic between February 2013 and June 2015 were enrolled as subjects. Forty healthy individuals without any upper gastrointestinal symptoms were recruited as the control group, and only patients who gave their full informed consent to participate were included in this study. The enrolled patients were evaluated for gastric motility (gastric accommodation and gastric emptying) and gastrointestinal symptoms. The range of the mean ± 2SD of the control group was defined as the normal range for gastric motility. Approval to conduct this clinical study was obtained from the Institutional Review Board of Hyogo College of Medicine on January 9th, 2008 (approval number: 536).
Functional Dyspepsia Subjects
Criteria for inclusion in this study were: (1) outpatients of at least 20 years of age; (2) patients who had undergone upper gastrointestinal endoscopy within 1 year of their visit and were not suffering from any organic diseases (malignant tumors, peptic ulcers, esophagitis, etc) that could be the cause of upper gastrointestinal symptoms; (3) patients not taking any drugs to improve gastrointestinal motility, gastric acid secretion inhibitors (histamine H2 receptor antagonists, proton pump inhibitors), gastric mucosal protectants, prostaglandin analogs, antidepressants, anti-anxiety drugs, sleep-inducing drugs, or antipsychotics (any patients taking these drugs must have stopped taking them for at least 2 weeks before taking the test meal); (4) patients expected to comply with the medication; and (5) patients who gave their written, informed consent to participate in this study. Criteria for exclusion were: (1) patients with a history of surgery of the upper gastrointestinal tract including the stomach and esophagus; (2) patients with severe liver dysfunction and/or kidney dysfunction; (3) patients with concomitant or suspected concomitant mental illness; (4) pregnant and breastfeeding patients or patients wishing to become pregnant during the study period; and (5) patients who had undergone Helicobacter pylori eradication therapy within the 6 months prior to their visit or patients currently undergoing eradication therapy.
Assessment
FD was diagnosed using the Japanese version of the Rome III criteria,6 and the gastric motility (gastric accommodation and gastric emptying) of each patient was evaluated by gastric scintigraphy.7 Upper gastrointestinal symptoms were evaluated by a questionnaire containing 10 items on gastrointestinal symptoms, and the association between the presence or absence of a gastric motility disorder and the strength of upper gastrointestinal symptoms was investigated.
Gastric Motility (Scintigraphic Procedure)
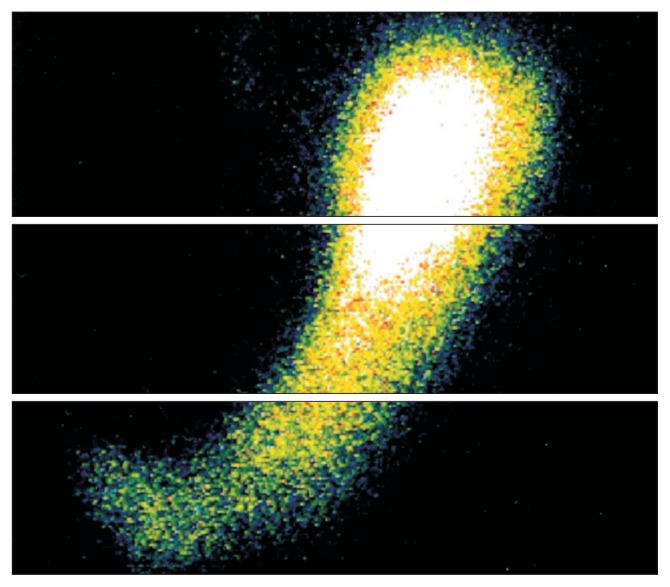
The subjects fasted for at least 6 hours before undergoing gastric scintigraphy. In the sitting position, the subjects consumed a test meal containing technetium-99m-labeled tin colloid (37 MBq) within 5 minutes. The composition of the test meal (retort curry, rice, and processed pork loin; total caloric content, 270.9 kcal; carbohydrate, 45.4 g; protein, 8.8 g; fat, 6.0 g) was almost the same as that of the standard meal recommended by the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine in 2008.8 During scintigraphy, the subjects remained in the sitting position. Using a gamma camera (RC2600i; HITACHI, Tokyo, Japan), scintigraphic images of the entire stomach were obtained in the anteroposterior and posteroanterior positions for 3 minutes each immediately after consumption of the meal, and at 15, 30, 45, 60, 90, and 120 minutes after the meal. Gastric accommodation and gastric emptying were measured simultaneously. In order to evaluate gastric accommodation, the radioactivity levels of the upper one-third of the stomach were measured just after meal intake, and this was regarded as a marker of gastric accommodation (Fig. 1). The region of interest was determined semi-automatically. Attenuation of the radioactivity was calculated automatically. Gastric emptying time was determined as the time required for radioactivity in the entire stomach to reach one-half of the initial level, which is called T half.7
Figure 1.
Representative image of gastric scintigraphy. Regarding the evaluation of gastric accommodation, the radioactivity levels of the upper one-third of the stomach when the stomach was divided into 3 equal parts along its long axis were measured just after meal intake, and this was regarded as a marker of gastric accommodation. Region of interest was determined semi-automatically. Attenuation of the radioactivity was calculated automatically.
Gastrointestinal Symptoms
Before undergoing gastric scintigraphy, patients were asked to rate the following 10 items of a questionnaire on gastrointestinal symptoms on a 4-point scale (0–3 points: 0, no symptoms; 1, mild symptoms; 2, moderate symptoms; 3, strong and/or painful symptoms). The 10 items were: (1) upper abdominal pain (pain around the pit of the stomach or stomach pain); (2) upper abdominal discomfort (discomfort or feeling of heaviness around the pit of the stomach); (3) upper abdominal bloating (feeling of distension around the pit of the stomach); (4) postprandial fullness (constant feeling of food remaining in the stomach or feeling of indigestion); (5) early satiety (feeling satiated despite eating only a little); (6) nausea (feeling sick or queasy); (7) vomiting (stronger feeling of sickness, regurgitating the contents of the stomach); (8) anorexia (decreased appetite or loss of appetite); (9) belching (gas that has accumulated in the esophagus and stomach is regurgitated and discharged from the mouth); and (10) heartburn (symptoms accompanied by a burning sensation from the pit of the stomach to the chest).
Statistical Methods
Statistical analyses were performed with GraphPad Prism5 (GraphPad Software, La Jolla, CA, USA). All results are expressed as mean ± SD. Characteristics of enrolled patients were analyzed by Fisher’s exact test, and only sex was analyzed by the Chi-square test. Regarding the correlation between gastric motility and dyspeptic symptoms, the unpaired t test was used. The effect of age on gastric motility was analyzed by the Spearman correlation test. Statistical significance was defined as a value of P < 0.05.
Results
Characteristics of Enrolled Patients
Ninety-four PDS type FD patients (29 men and 65 women, aged 21–84 [mean age: 54.3 ± 17.3] years) who gave their consent to participate were enrolled in this study. The characteristics of the FD patients are presented in Table 1. With respect to background factors, the age of patients in the FD group was significantly older than those in the healthy subjects group (P = 0.004).
Table 1.
Characteristics of the Subjects and Patients
| Characteristics | Healthy subjects | FD patients (PDS) | P-value |
|---|---|---|---|
| Patients (n) | 40 | 94 | |
| Age (mean ± SD, yr) | 44.7 ± 18.0 | 54.3 ± 17.3 | 0.004 |
| Sex (n [%]) | |||
| Male | 27 (67.5) | 29 (30.9) | |
| Female | 13 (32.5) | 65 (69.1) | |
FD, functional dyspepsia; PDS, postprandial distress syndrome.
Normal Gastric Motility in Healthy Controls
The 40 healthy subjects (27 men and 13 women, aged 23–76 years [mean age: 44.7 ± 18.0 years]) had gastric accommodation of 38.1 ± 9.8% (range: 21.6–57.0%) and gastric emptying of 53.0 ± 14.7 (range: 29.1–82.1) minutes. Impaired gastric accommodation was defined as an accommodation of 18.5% or less, delayed gastric emptying was defined as emptying in 82.4 minutes or more, and accelerated gastric emptying was defined as emptying in 23.6 minutes or less.
Prevalence of Impaired Gastric Accommodation and Gastric Emptying in Japanese Functional Dyspepsia Patients
Impaired gastric accommodation was seen in 14.9% (14/94), delayed gastric emptying was seen in 10.6% (10/94), accelerated gastric emptying was seen in 0.0% (0/94), and normal emptying was seen in 89.4% (84/94) of the 94 Japanese FD patients. None of the patients had both impaired gastric accommodation and delayed gastric emptying. Some form of gastric motility dysfunction was seen in 25.5% (24/94) of Japanese FD patients (Table 2).
Table 2.
Abnormalities of Gastric Motility in Japanese Functional Dyspepsia Patients
Impaired gastric accommodation.
Delayed gastric emptying.
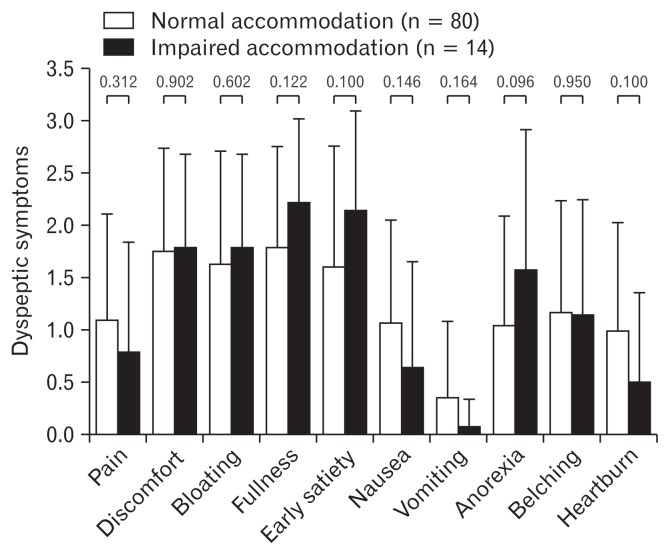
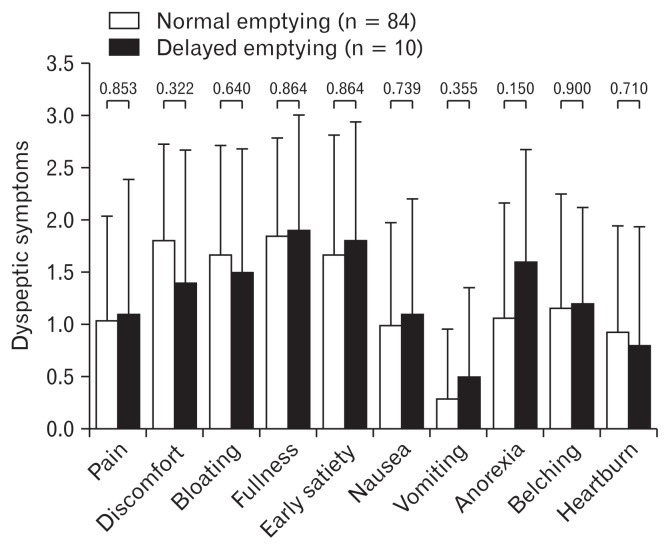
Association Between Gastric Motility Abnormalities and Dyspeptic Symptoms
The gastrointestinal symptoms on the 10-item questionnaire were not significantly different between the group with and the group without a gastric motility disorder. However, symptoms of early satiety and anorexia tended to manifest in the group with impaired gastric accommodation than in the group without impaired gastric accommodation (early satiety: P = 0.100, anorexia: P = 0.096) (Fig. 2). No significant difference was seen in any of the 10 items for the association between the presence or absence of impaired gastric emptying and gastrointestinal symptoms (Fig. 3).
Figure 2.
Association between gastric accommodation abnormality and dyspeptic symptoms. There was no significant differences in any of the 10 items between the group with and the group without impaired accommodation.
Figure 3.
Association between gastric emptying abnormality and dyspeptic symptoms. There was no significant difference in any of the 10 items for the association between the presence or absence of delayed gastric emptying and dyspeptic symptoms.
Effect of Age on Gastric Motility in Functional Dyspepsia Patients
We investigated the effect of age on gastric motility in FD patients, and we found that there was no correlation (r = 0.042, P = 0.683) between age and gastric delayed emptying time in FD patients. Regarding the impaired accommodation, there was no correlation (r = 0.174, P = 0.094).
Discussion
Many FD patients in Asia are of the PDS type,1–3 and gastric motility abnormalities are reported as the main pathology; however, few reports have investigated the prevalence of gastric motility abnormalities in a large sample. When the prevalence of gastric motility abnormalities was investigated in Japanese PDS type FD patients in this study, approximately 25% of PDS patients had some kind of gastric motility abnormality, such as impaired gastric accommodation or delayed gastric emptying. However, there was no association between the presence or absence of a gastric motility disorder and gastrointestinal symptoms.
The results of recent studies have drawn attention to visceral hypersensitivity9–16 and gastric motility abnormalities5,17–29 as important factors that have a direct impact on the occurrence of upper gastrointestinal symptoms. Moreover, the results of many previous studies in gastric motility abnormalities have identified a variety of abnormalities, including delayed gastric emptying,4,17,18 adaptive relaxation disorder,5 intragastric food distribution abnormalities,19–21 postprandial antral dysmotility,22 gastric electrical activity abnormalities,23–25 decreased interdigestive migrating contractions,26,27 and postprandial hypercontraction of the gastric fundus.29 According to reports, adaptive relaxation disorders and delayed gastric emptying are particularly associated with upper gastrointestinal symptoms.4,5,30–33 It is therefore important to simultaneously evaluate both gastric accommodation and gastric emptying when assessing gastric motility abnormalities.
Reports emerging primarily from the West have identified delayed gastric emptying in about 20% to 50% of FD patients, adaptive relaxation disorders in about 40% of FD patients, and visceral hypersensitivity to extension stimuli in 34% of FD patients.4,5,16 However, typical gastric motility evaluations only assess one of these functions. Differences in testing methods, test meals, and other parameters also have a large impact on test results, which makes it difficult to compare results with those of past studies. Moreover, no normal reference values are defined in actual evaluations of gastric motility, which makes deciding which criteria to use in the evaluation of gastric motility abnormalities difficult.
In the present study, gastric scintigraphy was used to simultaneously evaluate 2 important aspects of gastric motility in Japanese FD patients, particularly those with PDS. We have previously focused on gastric scintigraphy, which is considered the gold standard for examination of gastric emptying, and have previously reported that gastric scintigraphy is a useful modality to assess not only gastric emptying but also gastric accommodation.7 Regarding the evaluation of gastric accommodation, we had found positive correlation between gastric scintigraphy and barostat in a previous study.7 The results showed gastric motility abnormalities in approximately 30% of these Japanese PDS patients. In the present study, normal values were calculated from the reference values of a control group of 40 volunteers without any gastrointestinal symptoms to accurately evaluate the gastric motility of FD patients. The prevalence of gastric motility abnormalities was also examined in FD patients using strict criteria based on the reference values of the control group, which fell within the range of the mean ± 2SD. In addition, scintigraphic images were recorded for 2 hours. Generally, long time measurement is important for the evaluate the gastric delayed emptying.34,35 In the present study, delayed gastric emptying was defined as emptying in about 80 minutes or more. However, there was just 1 case (total: 94 cases) in which the emptying time was over 2 hours. Accordingly, we believe that the results in the present study are acceptable. The results showed impaired gastric accommodation in about 15% of FD patients, and delayed gastric emptying in about 10%. The results of the present study showed a lower prevalence of gastric motility abnormalities than reports to date, particularly overseas reports. The reason for this lower prevalence of gastric abnormalities may be that normal cut-off values were evaluated based on a stricter range of values, within a mean ± 2SD, than in earlier reports.
Furthermore, the test meal for the gastric scintigraphy that was performed contained semi-solid food that was ingested and imaged from the sitting position, which is relatively similar to dietary intake conditions in daily life.30,36,37 In light of this fact, gastric scintigraphy is a valid test method for evaluating the presence of gastric motility abnormalities in the pathology of FD. The results of the present study showed some kind of gastric motility abnormality in about 30% of Japanese FD patients, particularly PDS patients, which once again suggested the possibility that the pathology of PDS and the appearance of upper gastrointestinal symptoms have some association. Moreover, regarding the background factors, the age of patients in the FD group were significantly older than those in the healthy subjects group (P = 0.004). However, there were no correlation between age and gastric motility abnormalities results in FD patients. Accordingly, these results are considered to be reliable.
Next, the association between gastric motility abnormalities and upper gastrointestinal symptoms was investigated in the present study. Various previous reports have examined the association between gastric motility abnormalities and gastrointestinal symptoms. Of particular note are reports that described an association between early satiety and weight loss in those with impaired gastric accommodation,5,30,31 while other reports claimed no association between impaired gastric accommodation and dyspepsia symptoms.38 Meanwhile, some reports described an association between postprandial fullness and nausea and vomiting in gastric emptying disorders and gastrointestinal symptoms;4,32,33 however, many recent reports completely ruled out an association with gastrointestinal symptoms.18,39,40 In any case, differences in past testing methods, body positions during testing, and test meals have a major impact on past study results and are highly likely to produce variations in the results. In general, meta-analyses of gastric motility abnormalities in FD patients have found that approximately 40% of FD patients have delayed gastric emptying,41 suggesting that the gastric emptying of these patients is likely more delayed than that of healthy individuals. However, no reports have described a correlation between the extent of delayed gastric emptying and the extent of gastrointestinal symptoms. Moreover, delayed gastric emptying is often transient, which suggests that it is difficult to find a correlation between gastrointestinal symptoms and delayed gastric emptying. In the present study, the association between gastric motility abnormalities and dyspepsia symptoms was actually investigated by examining the association of 10 gastrointestinal symptoms with the presence or absence of impaired gastric accommodation and a gastric emptying disorder. However, no significant difference was seen in the presence or absence of gastric motility disorder and gastrointestinal symptoms. Nonetheless, the same fixed trend as that seen in past studies was observed, despite the lack of significant differences in impaired accommodation, early satiety, and anorexia.
Most reports regarding gastric motility in FD to date have been articles published by researchers in the West with Westerners as subjects. Gastric scintigraphy in particular is regarded as the gold standard for measurement of gastric emptying; however, recent reports have described its usefulness as a method for measuring gastric accommodation, as well as gastric emptying. The fact that it was possible to produce data supporting an association between gastric motility and gastrointestinal symptoms in Asians using gastric scintigraphy is significant.
Nonetheless, the present study was limited by the fact that it was a study at a single facility. Furthermore, the FD patients were limited to those who visited or were referred to our university hospital, which may have resulted in patient selection bias. In particular, the lack of a significant association between gastrointestinal symptoms and gastric motility abnormalities strongly indicates that many patients who come to our university hospitals have strong psychological factors.
In the present study, the association between the prevalence of gastric motility abnormalities and gastrointestinal symptoms was investigated in Japanese FD patients, particularly PDS patients, by using gastric scintigraphy. Gastric motility abnormalities were seen in approximately 25% of Japanese FD, particularly PDS, patients, but no association was seen with gastrointestinal symptoms. Further studies will be needed that take into account the difficulty in directly evaluating the association between gastrointestinal symptoms and gastric motility.
Footnotes
Conflicts of interest: None.
Author contributions: Haruki Asano and Toshihiko Tomita contributed to the concept and design of the study; Kumiko Nakamura, Takahisa Yamasaki, Takuya Okugawa, Takashi Kondo, Tomoaki Kono, Katsuyuki Tozawa, Yoshio Ohda, Hirokazu Fukui, Kazuhito Fukushima, and Shozo Hiroto were involved in data acquisition and analysis; Tadayuki Oshima provided statistical design; Jiro Watari and Hiroto Miwa coordinated acquisition of data and trial supervision; and all authors contributed to data interpretation, critically reviewed the manuscript for important intellectual contents, and approved final version of the manuscript.
Financial support: None.
References
- 1.Mak AD, Wu JC, Chan Y, Chan FK, Sung JJ, Lee S. Dyspepsia is strongly associated with major depression and generalised anxiety disorder - a community study. Aliment Pharmacol Ther. 2012;36:800–810. doi: 10.1111/apt.12036. [DOI] [PubMed] [Google Scholar]
- 2.Kim SE, Park HK, Kim N, et al. Prevalence and risk factors of functional dyspepsia: a nationwide multicenter prospective study in Korea. J Clin Gastroenterol. 2014;48:e12–e18. doi: 10.1097/MCG.0b013e31828f4bc9. [DOI] [PubMed] [Google Scholar]
- 3.Matsuzaki J, Suzuki H, Asakura K, et al. Classification of functional dyspepsia based on concomitant bowel symptoms. Neurogastroenterol Motil. 2012;24:325–e164. doi: 10.1111/j.1365-2982.2011.01859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarnelli G, Caenepeel P, Geypens B, Janssens J, Track J. Symptoms associated with impaired gastric emptying of solids and liquids in functional dyspepsia. Am J Gastroenterol. 2003;98:783–788. doi: 10.1111/j.1572-0241.2003.07389.x. [DOI] [PubMed] [Google Scholar]
- 5.Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi: 10.1016/S0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- 6.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 7.Tomita T, Okugawa T, Yamasaki T, et al. Use of scintigraphy to evaluate gastric accommodation and emptying: comparison with barostat. J Gastroenterol Hepatol. 2013;28:106–111. doi: 10.1111/j.1440-1746.2012.07261.x. [DOI] [PubMed] [Google Scholar]
- 8.Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008;36:44–54. doi: 10.2967/jnmt.107.048116. [DOI] [PubMed] [Google Scholar]
- 9.Lémann M, Dederding JP, Flourié B, Franchisseur C, Rambaud JC, Jian R. Abnormal perception of visceral pain in response to gastric distension in chronic idiopathic dyspepsia. The irritable stomach syndrome. Dig Dis Sci. 1991;36:1249–1254. doi: 10.1007/BF01307517. [DOI] [PubMed] [Google Scholar]
- 10.Rhee PL, Kim YH, Son HJ, et al. Evaluation of individual symptoms cannot predict presence of gastric hypersensitivity in functional dyspepsia. Dig Dis Sci. 2000;45:1680–1684. doi: 10.1023/A:1005550019308. [DOI] [PubMed] [Google Scholar]
- 11.Samsom M, Verhagen MA, vanBerge Henegouwen GP, Smout AJ. Abnormal clearance of exogenous acid and increased acid sensitivity of the proximal duodenum in dyspeptic patients. Gastroenterology. 1999;116:515–520. doi: 10.1016/S0016-5085(99)70171-X. [DOI] [PubMed] [Google Scholar]
- 12.Björnsson E, Sjöberg J, Ringström G, Norström M, Simrén M, Abrahamsson H. Effects of duodenal lipids on gastric sensitivity and relaxation in patients with ulcer-like and dysmotility-like dyspepsia. Digestion. 2003;67:209–217. doi: 10.1159/000072059. [DOI] [PubMed] [Google Scholar]
- 13.Oshima T, Okugawa T, Tomita T, et al. Generation of dyspeptic symptoms by direct acid and water infusion into the stomachs of functional dyspepsia patients and healthy subjects. Aliment Pharmacol Ther. 2012;35:175–182. doi: 10.1111/j.1365-2036.2011.04918.x. [DOI] [PubMed] [Google Scholar]
- 14.Miwa H, Nakajima K, Yamaguchi K, et al. Generation of dyspeptic symptoms by direct acid infusion into the stomach of healthy Japanese subjects. Aliment Pharmacol Ther. 2007;26:257–264. doi: 10.1111/j.1365-2036.2007.03367.x. [DOI] [PubMed] [Google Scholar]
- 15.Farré R, Vanheel H, Vanuytsel T, et al. In functional dyspepsia, hypersensitivity to postprandial distention correlates with meal-related symptom severity. Gastroenterology. 2013;145:566–573. doi: 10.1053/j.gastro.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 16.Tack J, Caenepeel P, Fischler B, Piessevaux H, Jassens J. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001;121:526–535. doi: 10.1053/gast.2001.27180. [DOI] [PubMed] [Google Scholar]
- 17.Stanghellini V, Tosetti C, Paternico A, et al. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996;110:1036–1042. doi: 10.1053/gast.1996.v110.pm8612991. [DOI] [PubMed] [Google Scholar]
- 18.Talley NJ, Verlinden M, Jones M. Can symptoms discriminate among those with delayed or normal gastric emptying in dysmotility-like dyspepsia? Am J Gastroenterol. 2001;96:1422–1428. doi: 10.1111/j.1572-0241.2001.03683.x. [DOI] [PubMed] [Google Scholar]
- 19.Gilja OH, Hausken T, Wilhelmsen I, Berstad A. Impaired accommodation of proximal stomach to a meal in functional dyspepsia. Dig Dis Sci. 1996;41:689–696. doi: 10.1007/BF02213124. [DOI] [PubMed] [Google Scholar]
- 20.Troncon LE, Herculano JR, Jr, Savoldelli RD, Moraes ER, Secaf M, Oliveira RB. Relationships between intragastric food maldistribution, disturbances of antral contractility, and symptoms in functional dyspepsia. Dig Dis Sci. 2006;51:517–526. doi: 10.1007/s10620-006-3164-5. [DOI] [PubMed] [Google Scholar]
- 21.Lorena SL, Tinois E, Brunetto SQ, Camargo EE, Mesqita MA. Gastric emptying and intragastric distribution of a solid meal in functional dyspepsia: influence of gender and anxiety. J Clin Gastroenterol. 2004;38:230–236. doi: 10.1097/00004836-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Camilleri M, Brown ML, Malagelada JR. Relationship between impaired gastric emptying and abnormal gastrointestinal motility. Gastroenterology. 1986;91:94–99. doi: 10.1016/0016-5085(86)90444-0. [DOI] [PubMed] [Google Scholar]
- 23.Lin Z, Eaker EY, Sarosiek I, McCallum RW. Gastric myoelectrical activity and gastric emptying in patients with functional dyspepsia. Am J Gastroenterol. 1999;94:2384–2389. doi: 10.1111/j.1572-0241.1999.01362.x. [DOI] [PubMed] [Google Scholar]
- 24.Parkman HP, Miller MA, Trate D, et al. Electrogastrography and gastric emptying scintigraphy are complementary for assessment of dyspepsia. J Clin Gastroenterol. 1997;24:214–219. doi: 10.1097/00004836-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Leahy A, Besherdas K, Clayman C, Mason I, Epstein O. Abnormalities of the electrogastrogram in functional gastrointestinal disorders. Am J Gastroenterol. 1999;94:1023–1028. doi: 10.1111/j.1572-0241.1999.01007.x. [DOI] [PubMed] [Google Scholar]
- 26.Labò G, Bortolotti M, Vezzadini P, Bonora G, Bersani G. Interdigestive gastroduodenal motility and serum motilin levels in patients with idiopathic delay in gastric emptying. Gastroenterology. 1986;90:20–26. doi: 10.1016/0016-5085(86)90069-7. [DOI] [PubMed] [Google Scholar]
- 27.Kusano M, Sekiguchi T, Kawamura O, et al. Further classification of dysmotility-like dyspepsia by interdigestive gastroduodenal manometry and plasma motilin level. Am J Gastroenterol. 1997;92:481–484. [PubMed] [Google Scholar]
- 28.Takahashi T. Interdigestive migrating motor complex -its mechanism and clinical importance. J Smooth Muscle Res. 2013;49:99–111. doi: 10.1540/jsmr.49.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simrén M, Vos R, Janssens J, Tack J. Unsuppressed postprandial phasic contractility in the proximal stomach in functional dyspepsia: relevance to symptoms. Am J Gastroenterol. 2003;98:2169–2175. doi: 10.1111/j.1572-0241.2003.07663.x. [DOI] [PubMed] [Google Scholar]
- 30.Piessevaux H, Tack J, Walrand S, Pauwels S, Geubel A. Intragastric distribution of a standardized meal in health and functional dyspepsia: correlation with specific symptoms. Neurogastroenterol Motil. 2003;15:447–455. doi: 10.1046/j.1365-2982.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 31.Kim DY, Delgado-Aros S, Camilleri M, et al. Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol. 2001;96:3099–3105. doi: 10.1111/j.1572-0241.2001.05264.x. [DOI] [PubMed] [Google Scholar]
- 32.Perri F, Clemente R, Festa V, et al. Patterns of symptoms in functional dyspepsia: role of Helicobacter pylori infection and delayed gastric emptying. Am J Gastroenterol. 1998;93:2082–2088. doi: 10.1111/j.1572-0241.1998.00597.x. [DOI] [PubMed] [Google Scholar]
- 33.Pasricha PJ, Colvin R, Yates K, et al. Characteristics of patients with chronic unexplained nausea and vomiting and normal gastric emptying. Clin Gastroenterol Hepatol. 2011;9:567–576. e1–e4. doi: 10.1016/j.cgh.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24–29. doi: 10.1023/A:1005697422454. [DOI] [PubMed] [Google Scholar]
- 35.Ziessman HA, Bonta DV, Goetze S, Ravich WJ. Experience with a simplified, standardized 4-hour gastric-emptying protocol. J Nucl Med. 2007;48:568–572. doi: 10.2967/jnumed.106.036616. [DOI] [PubMed] [Google Scholar]
- 36.Talley NJ, Shuter B, McCrudden G, Jones M, Hoschl R, Piper DW. Lack of association between gastric emptying of solids and symptoms in nonulcer dyspepsia. J Clin Gastroenterol. 1989;11:625–630. doi: 10.1097/00004836-198912000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Tominaga K, Higuchi K, Ochi M, et al. Concurrent assessment of reservoir and emptying of the stomach for dyspepsia patients. Hepatogastroenterology. 2008;55:744–749. [PubMed] [Google Scholar]
- 38.Boeckxstaens GE, Hirsch DP, Kuiken SD, Heisterkamp SH, Tytgat GN. The proximal stomach and postprandial symptoms in functional dyspeptics. Am J Gastroenterol. 2002;97:40–48. doi: 10.1111/j.1572-0241.2002.05421.x. [DOI] [PubMed] [Google Scholar]
- 39.Scott AM, Kellow JE, Shuter B, et al. Intragastric distribution and gastric emptying of solids and liquids in functional dyspepsia. Lack of influence of symptom subgroups and H. pylori-associated gastritis. Dig Dis Sci. 1993;38:2247–2254. doi: 10.1007/BF01299904. [DOI] [PubMed] [Google Scholar]
- 40.Janssen P, Harris MS, Jones M, et al. The relation between symptom improvement and gastric emptying in the treatment of diabetic and idiopathic gastroparesis. Am J Gastroenterol. 2013;108:1382–1391. doi: 10.1038/ajg.2013.118. [DOI] [PubMed] [Google Scholar]
- 41.Quartero AO, de Wit NJ, Lodder AC, Numans ME, Smout AJ, Hoes AW. Disturbed solid-phase gastric emptying in functional dyspepsia: a meta-analysis. Dig Dis Sci. 1998;43:2028–2033. doi: 10.1023/A:1018803129779. [DOI] [PubMed] [Google Scholar]