Abstract
Long-term acute care hospitals (LTACs) are an increasingly common discharge destination for patients recovering from intensive care. In this article the authors use U.S. Medicare claims data to examine regional- and hospital-level variation in LTAC utilization after intensive care to determine factors associated with their use. Using hierarchical regression models to control for patient characteristics, this study found wide variation in LTAC utilization across hospitals, even controlling for LTAC access within a region. Several hospital characteristics were independently associated with increasing LTAC utilization, including increasing hospital size, for-profit ownership, academic teaching status, and colocation of the LTAC within an acute care hospital. These findings highlight the need for research into LTAC admission criteria and the incentives driving variation in LTAC utilization across hospitals.
Keywords: mechanical ventilation, intensive care, long-term acute care, post-acute care utilization, practice variation
Introduction
Long-term acute care hospitals (LTACs) provide inpatient services for patients with complex medical problems requiring extended hospital stays (Liu et al., 2001). Defined by the Centers for Medicare and Medicaid Services (CMS) as acute care hospitals with average lengths of stay exceeding 25 days, LTACs typically admit hospitalized patients in the recovery phase after severe acute illness (Scheinhorn et al., 2007a, 2007b). LTACs are among the fastest growing segments of acute care in the United States—from 1997 to 2006 the number of LTACs in the United States increased from 192 to 408, for an average annual increase of 8.8% (Kahn, Benson, Appleby, Carson, & Iwashyna, 2010). LTAC spending has grown at a comparable rate—in 2008 Medicare reimbursement for LTACs was $4.6 billion, up from $398 million in 1993 (Medicare Payment Advisory Commission, 2010).
Despite such growth, LTACs remain a poorly understood segment of the health system. LTACs are defined by their average duration of stay, not by the type of patients admitted or the services provided. Consequently, there is little consensus about when and why patients should be transferred to an LTAC. There is also substantial regional variation in LTAC penetration—some states have many LTACs while others have none (Medicare Payment Advisory Commission, 2004). Little is known about how hospitals may vary in the degree they use LTACs, or the degree in which utilization is driven by patient characteristics, regional variation in LTAC penetration, or other hospital factors. In this data trends analysis, we use Medicare data to examine hospital-level variation in LTAC utilization and the relationship between hospital utilization and LTAC market penetration.
New Contribution
LTACs have only recently emerged as a prominent part of the post–acute care landscape, and to this point no studies have systematically evaluated regional and hospital patterns of use. Reports by the Medicare Payment Advisory Commission and the peer reviewed literature (Kahn et al., 2010) demonstrate regional variation in LTAC penetration and increasing utilization over time, but have not examined hospital-level variation in utilization or the hospital factors associated with increasing use. This study helps frame future LTAC research by providing novel empiric data on LTAC transfer patterns and the ways in which hospitals differentially use them for patients recovering from severe acute illness. Understanding existing patterns of and variations in care is an essential first step for future research on the policy implications of these patterns.
Method
Study Design and Data Sources
We examined LTAC utilization after critical illness using the 100% Medicare Provider Analysis and Review File (MedPAR) from 2006. MedPAR contains patient-level demographic data, diagnosis codes, and resource utilization codes from hospitalizations for fee-for-service Medicare beneficiaries. We supplemented the MedPAR data with hospital-level characteristics from the 2006 Centers for Medicare and Medicaid Health Cost Report Information System, population estimates from the Centers for Disease Control and Prevention’s National Center for Health Statistics (www.cdc.gov/nchs), and data on state certificate of need laws for LTACs from the National Conference on State Legislators (www.ncsl.org).
Patients and Variables
We examined all Medicare hospitalizations in the continental United States involving an intensive care unit (ICU) stay for beneficiaries 65 years or older, identified using ICU-specific resource utilization codes. We limited the analysis to ICU hospitalizations since these patients have high LTAC utilization rates compared with other hospitalized patients (Kahn et al., 2010). We identified LTACs using CMS hospital identifiers as previously described (Kahn & Iwashyna, 2010). LTAC transfers were defined as temporally adjacent hospitalizations (i.e., discharge from the first hospital on day n and admission to the second hospital on day n or n + 1), in which the first hospitalization is in a short stay hospital and the second hospitalization is in an LTAC (Iwashyna, Christie, Moody, Kahn, & Asch, 2009). We defined hospital-level LTAC transfer rates as the percentage of hospitalizations involving an ICU stay that ended in a transfer to an LTAC. To ensure that observed differences in transfer rates were not attributable to differences in case-mix between hospitals, we used a patient-level multivariate hierarchical logistic regression model to create hospital-specific adjusted transfer rates, a method analogous to indirect standardization. These adjusted transfer rates were used in all subsequent analyses.
Analysis
We examined variation in adjusted LTAC utilization between hospitals using summary statistics and histograms. To determine the relationship between hospital characteristics and adjusted LTAC utilization, we first categorized hospitals as either nonutilizers (adjusted transfer rate = 0%), lowutilizers (adjusted transfer rate between 0% and 2.5%), and high utilizers (adjusted transfer rate ≥2.5%). We then tested the association between LTAC utilization and selected hospital characteristics. We restricted this analysis to hospitals within Dartmouth Atlas hospital referral regions (HRRs) that contained at least one LTAC (Dartmouth Medical School, 1999). Hospital characteristics of interest included the annual number of ICU admissions, hospital bed size, hospital ownership, hospital teaching status (defined using the resident-to-bed ratio), the size of the hospital’s metropolitan statistical area, the presence of an LTAC colocated within the hospital, the linear arc distance from each hospital to the nearest LTAC, and whether or not the LTAC is located in a state with certificate of need laws for LTACs, and LTAC market penetration defined as the number of LTAC beds per capita in the hospital’s HRR.
Univariate analyses were performed using a chi-squared test or analysis of variance, as appropriate. We also performed a hospital-level multivariate analysis using random-effects negative binomial regression, in which the dependent variable was a count of each hospital’s ICU patients transferred to an LTAC, accounting for the total number of patients at risk. We included all hospital- and region-level factors as fixed effects and specified a HRR-level random effect. The exponentiated regression coefficients are interpreted as hospital-specific incidence rate ratios controlling for the other covariates in the model. Data management was performed using SAS 9.0 (Cary, NC) and statistical analyses were performed using Stata 11.0 (College Station, TX). Additional methodological details regarding model specification and variable definitions are available from the authors. This project was approved by the University of Pennsylvania Institutional Review Board.
Results
LTAC Characteristics and Market Penetration
In 2006 there were 408 LTACs in the United States. The median bed size was 43 (interquartile range = 31–72), and 283 (69.4%) were for-profit institutions. Approximately half of all LTACs (198, 48.5%) were colocated within an acute-care hospital. LTACs were heterogeneously distributed throughout the country (Figure 1). Of the 304 HRRs in the continental United States, 134 (44.1%) contained no LTACs, 86 (28.3%) contained one LTAC, 43 (14.1%) contained two LTACs, and 41 (13.5%) contained three or more LTACs. The number of LTACs per million adults in each HRR ranged from 0 to 17.0 (median = 0.95, interquartile range = 0–2.6).
Figure 1.
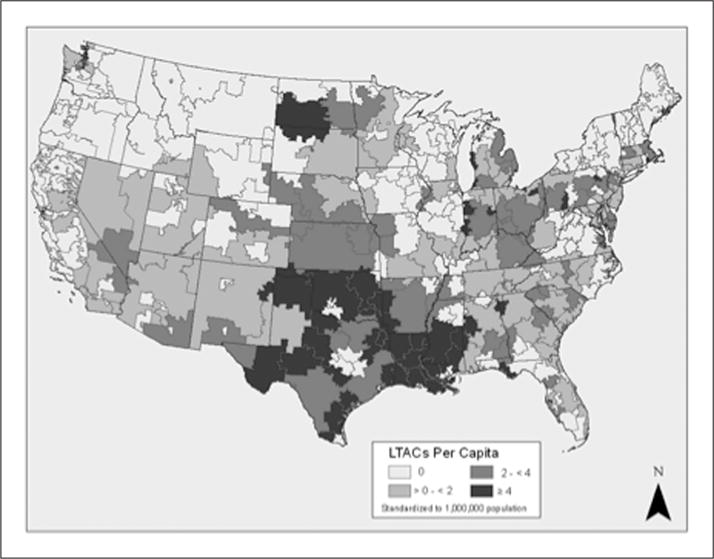
Regional variation in long-term acute care hospital (LTAC) penetration by Dartmouth Atlas hospital referral region
Hospital Variation in LTAC Utilization
Of 3,763 acute care hospitals with ICUs, 2,225 (59.1%) transferred at least one patient to an LTAC after intensive care. We found substantial variation in both unadjusted and adjusted transfer rates between hospitals. Unadjusted transfer rates ranged from 0% to 38.7% (median = 0.4%, interquartile range = 0% to 2.3%). Adjusted transfer rates ranged from 0% to 23.3% (median = 0.7%; interquartile range = 0.0% to 2.0%).
The number of hospitals transferring patients to LTACs increased with increasing LTAC bed availability. Yet sizable variation persisted even when stratifying by LTAC bed availability (Figure 2). In HRRs without LTACs, adjusted transfer rates ranged from 0% to 4.8%. In HRRs with 1 to 100 LTAC beds, adjusted transfer rates ranged from 0% to 10.5%; in HRRs with 101 to 200 LTAC beds, adjusted transfer rates ranged from 0% to 10.5%; while in HRRs with >200 LTAC beds adjusted transfer rates ranged from 0% to 23.3%. Even in high penetrance HRRs with a large number of LTACs (i.e., >200 LTAC beds), 195 hospitals (20.4%) transferred no critically ill patients to LTACs.
Figure 2.
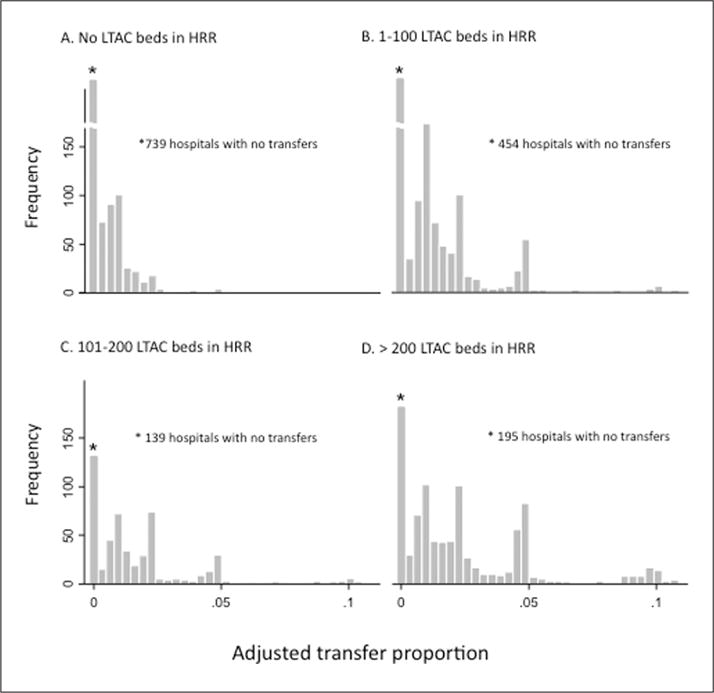
Hospital-level variation in LTAC utilization after critical illness, by population-adjusted LTAC penetration
Note: LTAC = long-term acute care hospital; HRR = hospital referral region.
Hospital Factors Associated With Increasing Transfer Rates
A total of 2,670 hospitals were located in HRRs with at least one LTAC. Of these, 798 hospitals (29.9%) were nonutilizers of LTACs (adjusted transfer rate = 0%), 1,307 hospitals (49.0%) were low utilizers (adjusted transfer rate 0% to 2.5%), and 564 hospitals (21.1%) were high utilizers (adjusted transfer rate ≥2.5%). Increasing hospital size, for-profit ownership, academic status, and colocation with an LTAC were all associated with higher utilization (Table 1). Physical proximity to an LTAC (even if not colocated) and increasing numbers of LTAC beds in the HRR were also associated with increased LTAC use. State certificate of need laws were associated with lower LTAC use. These associations persisted after simultaneously adjusting for patient-, hospital- and region-level factors (Table 2).
Table 1.
Hospital Characteristics by Increasing Adjusted LTAC Utilization After Critical Illness for Hospitals With at Least One LTAC in the HRR
| Variable | No LTAC Utilization (n = 798) | Low LTAC Utilization; <2.5% Utilization; (n = 1,307) | High LTAC ≥2.5% (n = 564) | P |
|---|---|---|---|---|
| Critical care admissions | 94 (23–201) | 417 (234–788) | 385 (202–748) | <.001 |
| Bed size | 40 (25–84) | 167 (102–296) | 195 (113–316) | <.001 |
| Ownership | ||||
| Nonprofit | 409 (51.2) | 843 (64.5) | 300 (53.2) | <.001 |
| For-profit | 122 (14.3) | 274 (21.0) | 185 (32.8) | |
| Government | 267 (33.5) | 190 (14.5) | 79 (14.0) | |
| Teaching statusa | ||||
| Nonteaching | 726 (90.1) | 832 (63.7) | 333 (59.0) | <.001 |
| Small teaching | 51 (6.4) | 317 (24.3) | 165 (29.3) | |
| Large teaching | 21 (2.6) | 158 (12.1) | 66 (11.7) | |
| MSA size | ||||
| <100,000 | 505 (63.3) | 299 (22.9) | 63 (11.2) | <.001 |
| 100,000 to 1 million | 126 (15.8) | 363 (27.8) | 175 (31.0) | |
| >1 million | 167 (20.9) | 645 (49.4) | 326 (57.8) | |
| LTAC in hospital | 0 (0.0) | 65 (5.0) | 141 (25.0) | <.001 |
| Distance to nearest LTAC | 42.9 (23.9–72.4) | 13.0 (4.2–30.4) | 2.5 (0.1–7.4) | <.001 |
| Certificate of need law in state | 324 (40.6) | 713 (54.6) | 169 (30.0) | <.001 |
| Per capita LTAC beds in HRR | ||||
| 1–<200 | 685 (85.8) | 1094 (83.7) | 90 (51.4) | <.001 |
| 200–400 | 90 (11.3) | 156 (11.9) | 146 (25.9) | |
| >400 | 23 (2.9) | 57 (4.4) | 128 (22.7) |
Note: All values are given as median (interquartile range) or frequency (percentage). Utilization rates are adjusted for case-mix. LTAC = long-term acute care hospital; MSA = metropolitan statistical area size; HRR = Dartmouth Atlas hospital referral region.
Teaching status categorized by resident-to-bed ratio (nonteaching = 0, small teaching = >0 and <0.25, large teaching = ≥0.25).
Table 2.
Negative Binomial Regression Analysis Examining Independent Factors Associated With Increasing Hospital LTAC Utilization After Critical Illnessa
| Variable | IRR | P |
|---|---|---|
| Bed size | ||
| <100 | Referent | |
| 100–200 | 1.23 (1.11–1.36) | <.001 |
| >200 | 1.18 (1.06–1.31) | .003 |
| Ownership | ||
| Nonprofit | Referent | |
| For-profit | 1.25 (1.16–1.34) | <.001 |
| Government | 1.06 (0.97–1.15) | .21 |
| Teaching status | ||
| Nonteaching | Referent | |
| Small teaching | 1.01 (0.94–1.08) | .88 |
| Large teaching | 1.11 (1.01–1.22) | .03 |
| MSA size | ||
| <100,000 | Referent | |
| 100,000 to 1 million | 1.08 (0.97–1.21) | .17 |
| >1 million | 1.13 (1.00–1.28) | .05 |
| Distance to nearest LTAC (miles) | ||
| >50 | Referent | |
| >25–50 | 1.40 (1.18–1.65) | <.001 |
| >15–25 | 1.70 (1.42–2.04) | <.001 |
| >5–15 | 2.44 (2.06–2.89) | <.001 |
| >0–5 | 3.25 (2.74–3.85) | <.001 |
| 0 (HWH) | 4.13 (3.47–4.91) | <.001 |
| State with certificate of need law | 0.69 (0.59–0.79) | <.001 |
| Census region | ||
| Northeast | Referent | |
| Southeast | 1.75 (1.46–2.10) | <.001 |
| Midwest | 1.35 (1.12–1.63) | .002 |
| West | 1.40 (1.14–1.70) | .001 |
| Per capita LTAC beds in HRR | ||
| 1–200 | Referent | |
| 201–400 | 1.31 (1.13–1.53) | <.001 |
| >400 | 1.34 (1.10–1.63) | <.003 |
Note: LTAC = long-term acute care hospital; IRR = incidence rate ratio; MSA = metropolitan statistical area; HWH = hospital within a hospital; HRR = Dartmouth Atlas hospital referral region
Utilization rates are adjusted for differences in case mix across hospitals.
Discussion
In a national study of LTAC utilization after critical illness, we found wide variation between hospitals in the utilization of LTACs after critical care, even after accounting for differences in patient characteristics. The major driver of utilization was access to LTACs—LTACs tend to be clustered in some regions of the United States, and we found greater utilization among hospitals in close proximity to an LTAC. However, we observed substantial variation in utilization rates even within HRRs, indicating that LTACs are used differently even by hospitals with equivalent LTAC access. Controlling for other hospital characteristics, colocated hospitals, large hospitals, for-profit hospitals, and academic hospitals had relatively high utilization rates.
The variation in LTAC utilization we observe highlights in the need for future research into the role that LTACs play in the U.S. health system. LTACs function as dedicated weaning centers for patients requiring prolonged mechanical ventilation and as long-stay hospitals for other types of patients recovering from severe acute illness (Carson, 2007). Yet there are several alternative sites of care for these types of patients. Patients requiring prolonged mechanical ventilation can continue to receive care in a short-stay hospital, either in the ICU or in a step-down unit specially designed for ventilator weaning (Subbe, Criner, & Baudouin, 2007). Less severely ill patients can receive care in skilled nursing facilities, inpatient rehabilitation hospitals, or acute care hospital wards. Research is needed into the comparative effectiveness of these different models of care for patients with chronic critical illness.
There are reasons why LTACs might either be beneficial or harmful for patients recovering from critical illness. LTACs might improve quality by providing specialized expertise and protocols for the care of complex patients (Girard et al., 2008; Kahn et al., 2006). LTACs could also decrease costs by taking advantage of economies of scale, shortening overall length of stay, or reducing readmission rates (Jacobs, Rapoport, & Edbrooke, 2004; Lellouche et al., 2006). On the other hand, there are reasons to hypothesize that LTACs might worsen quality and costs. LTACs typically provide less intense nurse and physician staffing, and may not have all the resources of an acute care hospital (Nayar, 2008), which may worsen outcomes and increase medical errors. LTAC transfer might also increase overall length of stay by disrupting communication and fragmenting the episode of acute care, with concomitant increases in costs (Coleman, Min, Chomiak, & Kramer, 2004). Comparative effectiveness research examining these mechanisms will help both clinical decisions regarding transfer to an LTAC and policy decisions about whether LTACs should be incentivized in the health system. Such research will help define which types of patients may most benefit from LTACs, evaluate tools for identifying these patients, and determine the optimal timing of transfer.
Research is also needed into the role of different types of LTACs. Currently LTACs operate as either free-standing facilities or as facilities colocated with general acute care hospitals. Colocated LTACs, also called “hospitals-within-a-hospital,” are financially independent from their host hospital but share many of the same services. We found that approximately half the LTACs in the United States are colocated in an acute care hospital, and the highest LTAC utilization rates are in hospitals that contain an LTAC. Medicare recognizes that colocation may decrease the barriers to LTAC transfer, and in 2005 implemented the “25% rule,” which states that colocated LTACs may not admit more than 25% of their patients from single hospital (Medicare Payment Advisory Commission, 2010). In 2007 Medicare extended this rule to all LTACs.
The goal of the 25% rule is to prevent host hospitals from overutilizing the colocated LTAC. Yet, colocation may provide clinical benefit to patients, since colocated LTACs can more easily avail themselves of the resources of acute care hospitals, potentially preventing the need for hospital readmission in the event of clinical decompensation. Colocation may also be beneficial for patient families, who can avoid the emotional trauma that may be associated with interhospital transfer of a critically ill loved one (Happ et al., 2007). Future research should evaluate whether or not LTAC colocation has clinical and financial benefits for patients and society. This research will help inform Medicare payment policy for LTACs, which can either encourage or discourage the colocated model.
Finally, our study highlights the need for research into the external incentives surrounding LTAC utilization, especially financial incentives and external incentives for quality such as value-based purchasing. We found that for-profit hospitals are more likely to use LTACs than nonprofit hospitals, even after controlling for patient characteristics and geographic access. This finding suggests that profit-seeking firms may attempt to increase LTAC transfers in order to maximize payments under Medicare’s prospective payment system. Moreover, LTAC transfers might artificially improve quality metrics such as in-hospital mortality for ICU patients (Kahn, Kramer, & Rubenfeld, 2007; Vasilevskis et al., 2009). Given the wide variation in LTAC utilization we observe, research designed to inform policy initiatives geared toward ICU quality should consider LTAC transfer rates as possible explanatory factors for variation in quality.
Study Limitations
Our study has several limitations. We used a patient-level hierarchical multivariate model to create standardized LTAC transfer rates that take into account differences in patient characteristics across hospitals. Although this approach greatly minimizes the chance of bias, we cannot rule out the possibility that some of the hospital-variation we observe is due to residual variation in case mix. Additionally, MedPAR contains data only on fee-for-service Medicare beneficiaries. Our analysis does not include individuals enrolled in Medicare Advantage programs or patients not eligible for Medicare. We might observe different transfer patterns in an all-pay or data set, where incentives to transfer patients to LTAC might be higher. However, MedPAR Medicare pays for nearly 70% of LTAC discharges, and MedPAR is the only national data source for studying LTAC hospitalizations, enabling us to study the entirety of the United States rather than just a small region.
We were unable to look at determinants of LTAC utilization at the physician level, such as might occur when physicians provide services at both an acute care hospital and an LTAC. Future studies should examine physician-level financial incentives for LTAC utilization. Finally, our analysis does not account for overlap of services between LTACs and other post–acute care facilities such as skilled nursing facilities or rehabilitation hospitals. These hospitals may provide similar services as LTACs for some patients and therefore impact overall utilization rates. We address this limitation in part by focusing on ICU patients, which are more homogeneous and have higher LTAC utilization rates than the general population.
Conclusions
LTACs are a rapidly expanding model of care for patients recovering from severe acute illness, but little research has evaluated their effectiveness. In a national study of LTAC utilization after critical illness, we observe wide variation in the proportion of patients transferred to LTAC after critical illness, highlighting their uncertain role in the health care system. We found relatively high utilization among large hospitals, for-profit hospitals, academic hospitals, and hospitals in close proximity to an LTAC. This variation persisted even after adjusting for LTAC bed availability within regions. Health policy for LTACs is still in evolution. Our findings elucidate the hospital-level factors associated with LTAC use and demonstrate the need for critical evaluation of LTACs as a model of care for patients in the post-ICU period.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
This work was funded by the United States National Institutes of Health (R01HL096651).
Footnotes
Reprints and permission: http://www.sagepub.com/journalsPermissions.nav
Authors’ Note
Dr. Kahn has received speaking honoraria from the National Association of Long Term Acute Care Hospitals.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Carson SS. Know your long-term care hospital. Chest. 2007;131:2–5. doi: 10.1378/chest.06-2513. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: Patterns, complications, and risk identification. Health Services Research. 2004;39:1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartmouth Medical School. The Dartmouth atlas of health care. Chicago, IL: American Hospital Association; 1999. [Google Scholar]
- Girard TD, Kress JP, Fuchs BD, Thomason JW, Schweickert WD, Pun BT, Ely EW. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): A randomised controlled trial. Lancet. 2008;371:126–134. doi: 10.1016/S0140-6736(08)60105-1. [DOI] [PubMed] [Google Scholar]
- Happ MB, Swigart VA, Tate JA, Arnold RM, Sereika SM, Hoffman LA. Family presence and surveillance during weaning from prolonged mechanical ventilation. Heart & Lung. 2007;36:47–57. doi: 10.1016/j.hrtlng.2006.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Medical Care. 2009;47:787–793. doi: 10.1097/MLR.0b013e318197b1f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs P, Rapoport J, Edbrooke D. Economies of scale in British intensive care units and combined intensive care/high dependency units. Intensive Care Medicine. 2004;30:660–664. doi: 10.1007/s00134-003-2123-2. [DOI] [PubMed] [Google Scholar]
- Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. Journal of the American Medical Association. 2010;303:2253–2259. doi: 10.1001/jama.2010.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. New England Journal of Medicine. 2006;355:41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- Kahn JM, Iwashyna TJ. Accuracy of the discharge destination field in administrative data for identifying transfer to a long-term acute care hospital. BMC Research Notes. 2010;3:205. doi: 10.1186/1756-0500-3-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: A simulation study. Chest. 2007;131:68–75. doi: 10.1378/chest.06-0741. [DOI] [PubMed] [Google Scholar]
- Lellouche F, Mancebo J, Jolliet P, Roeseler J, Schortgen F, Dojat M, Brochard L. A multicenter randomized trial of computer-driven protocolized weaning from mechanical ventilation. American Journal of Respiratory and Critical Care Medicine. 2006;174:894–900. doi: 10.1164/rccm.200511-1780OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Baseggio C, Wissoker D, Maxwell S, Haley J, Long S. Long-term care hospitals under Medicare: Facility-level characteristics. Health Care Financing Review. 2001;23(2):1–18. [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Defining long term acute care hospitals. Report to the Congress: New approaches in Medicare. Washington, DC: Author; 2004. [Google Scholar]
- Medicare Payment Advisory Commission. Medicare Payment Policy. Washington, DC: Author; 2010. [Google Scholar]
- Nayar P. The impact of Medicare’s Prospective Payment System on staffing of long-term acute care hospitals: The early evidence. Health Care Management Review. 2008;33:264–273. doi: 10.1097/01.HMR.0000324911.26896.d8. [DOI] [PubMed] [Google Scholar]
- Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, Petrak RA. Post-ICU mechanical ventilation at 23 long-term care hospitals: A multicenter outcomes study. Chest. 2007a;131:85–93. doi: 10.1378/chest.06-1081. [DOI] [PubMed] [Google Scholar]
- Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, Petrak RA. Ventilator-dependent survivors of catastrophic illness transferred to 23 long-term care hospitals for weaning from prolonged mechanical ventilation. Chest. 2007b;131:76–84. doi: 10.1378/chest.06-1079. [DOI] [PubMed] [Google Scholar]
- Subbe CP, Criner GJ, Baudouin SV. Weaning units: Lessons from North America? Anaesthesia. 2007;62:374–380. doi: 10.1111/j.1365-2044.2007.04984.x. [DOI] [PubMed] [Google Scholar]
- Vasilevskis EE, Kuzniewicz MW, Dean ML, Clay T, Vittinghoff E, Rennie DJ, Dudley RA. Relationship between discharge practices and intensive care unit in-hospital mortality performance: Evidence of a discharge bias. Medical Care. 2009;47:803–812. doi: 10.1097/MLR.0b013e3181a39454. [DOI] [PubMed] [Google Scholar]


