To the Editor
Psychosocial stress among asthmatic children and/or their caregivers is an important variable affecting childhood asthma morbidity(1) but few studies have examined stress among caregivers of inner-city asthmatic children. The 4-item perceived stress scale [PSS-4] is a validated measure of the degree to which situations in a person’s life are perceived as stressful.(2) It is scored from 0–16, with higher scores indicating higher degrees of stress. To our knowledge, there is no well-established cutoff in the PSS-4 score to define high stress among caregivers of asthmatic children, making it challenging to compare stress across study populations. We sought to assess PSS-4 scores among caregivers of inner-city children with asthma by considering scores in relation to published normative data. Additionally, we aimed to determine whether caregiver stress was related to asthma morbidity.
The School Inner City Asthma Study [SICAS] was conducted between 2008–2013. We recruited school-aged students with physician-diagnosed asthma from schools in a northeastern US city and followed through an academic year. Detailed methods have been described elsewhere(3). At the baseline visit, caregiver stress was assessed using the PSS-4. To define stress levels, we used the mean PSS-4 score of 4.49 and standard deviation [SD] of 2.96 from a publication that validated the PSS-4 in a large population-based sample of the US.(2) We defined “normal”, “high”, and “very high” stress in our cohort as less than 1 SD, more than 1 SD, and more than 2 SD above this mean, respectively. Asthma morbidity was measured as two week symptom recall at baseline followed by quarterly telephone survey at 3, 6, 9, and 12 months. The primary morbidity outcome, maximum symptom days over the last 2 weeks, was defined as the largest value among (1) number of days participant experienced wheeze, cough, or chest tightness, or (2) number of nights participant awoke due to asthma, or (3) number of days participant slowed down or discontinued activities because of asthma. Secondary outcomes included individual measures of poor asthma control, based on symptoms in the last 4 weeks. Categories included dyspnea, night-time symptoms, decreased daytime activity, and rescue medication use. For each category, caregiver responses were categorized as “well controlled” or “not well controlled” asthma, based on the National Asthma Education and Prevention Program guidelines.(4) The online supplement contains variable definitions and statistical methods.
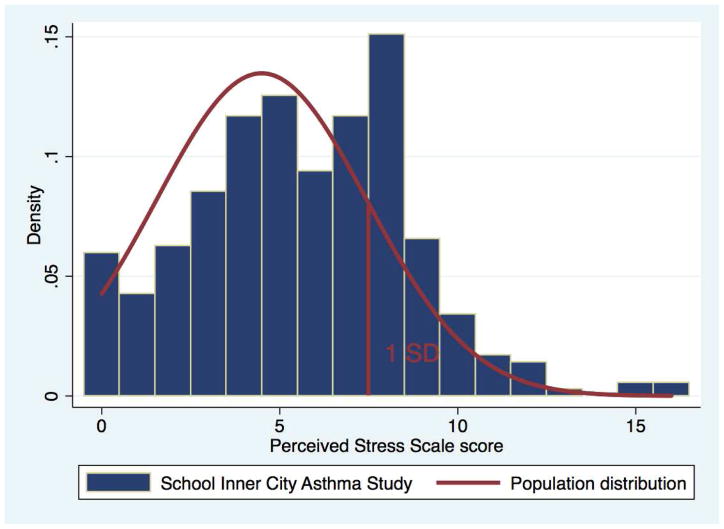
There were 247 caregivers (70.4%) in the “normal stress” group (PSS-4 score ≤ 7), 88 (25.1%) in the “high stress” group (PSS-4 score 8–10), and 16 (4.6%) in the “very high stress” group (PSS-4 score ≥11). These findings demonstrate that 29.6% of caregivers in our study had stress levels greater than 1 SD above the population mean, compared with an estimated 15.9% in the general U.S. population(2) (p < 0.001) (see Figure 1). PSS-4 scores in SICAS are also higher (mean (SD) 5.6 (3.1)) than those reported by Islam et al(5) (mean (SD) 3.9 (2.8)), which may be due to inherent differences in the populations studied.
Figure 1.
Distribution of PSS-4 scores among the SICAS cohort compared to expected PSS-4 scores from a published validation sample(2). Bars represent distribution of stress scores in the SICAS cohort. Line represents the normal population distribution of PSS scores(2).
There is no single, broadly accepted definition of high stress among caregivers of asthmatic children using the PSS-4. Islam et al(5) defined “high stress” as above the median PSS-4 score within their sample, which was 4. In contrast, using our method, our cohort’s “high stress” group had a PSS-4 score of ≥ 8. Wright et al. examined PSS-4 scores in tertiles in their study of caregivers of infants at risk for asthma.(1) In that cohort, the mean (SD) PSS-4 scores in the “low”, “intermediate”, and “high” stress groups were 1.1 (0.8), 4.1 (0.8), and 7.4 (1.7) respectively, compared to our “normal”, “high”, and “very high” stress groups in which means (SD) are 4.1 (2.1), 8.5 (0.7), and 12.6 (1.9) respectively. The examples above demonstrate that the definition of high stress varies between studies, making comparison difficult. Therefore, rather than confining the gauge of stress to the distribution contained within our own study population, we defined stress groups using population-based normative data,(2) which allows for both characterization of the overall stress level in our own cohort, and ability to compare stress levels across studies.
Consistent with the validation cohort,(2) we found higher degrees of stress were more likely to come from lower income households, and with higher rates of household unemployment (supplementary table E1).
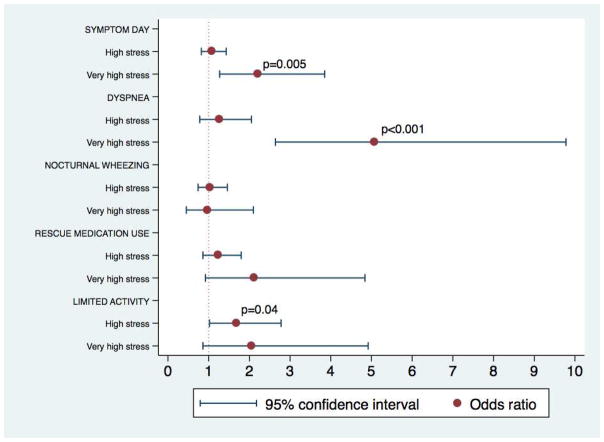
Participants whose caregivers had very high stress had more than two-fold odds of having a symptom day (odds ratio [OR] =2.21, 95% confidence interval [CI] = [1.27, 3.85], p=0.005, Figure 2). They had 5.0 symptom days per two-week period compared to 2.9 symptom days for participants whose caregivers had normal stress. Similarly, very high stress was associated with greater dyspnea (OR 5.08, CI = [2.64–9.78], p< 0.001) and high stress was associated with greater activity limitation (OR 1.68, CI = [1.02–2.78], p = 0.04) compared to normal stress. These findings are consistent with previous studies which examined populations with different socio-demographics from the SICAS population (such as age and SES)(1) or which used tools other than the PSS-4 to measure stress,(6) or which reported on different outcomes(6) from SICAS.
Figure 2.
Asthma morbidity outcomes in high stress group and very high stress group, compared to normal stress group. Dotted vertical line represents normal stress (reference) group.
It has been speculated that caregiver stress may lead to asthma morbidity by intermediaries such as tobacco smoking,(7) child anxiety, disorganized home conditions, or may affect the child’s perception of control and self-efficacy, asthma management skills, or the family’s problem-solving abilities,(8) which may in turn affect medication adherence. However, we found no associations between caregiver stress and any of these factors (table E1).
We acknowledge that subjects’ symptoms were reported by caregivers. However, we have previously demonstrated good caregiver-subject agreement on screening surveys in this cohort.(9) Prior studies have also used caregiver responses to predict childhood outcomes.(1, 5). Additionally, measuring PSS-4 at multiple time points, instead of a single measure, may have offered a more robust exposure metric, however, we would expect this limitation to bias toward the null hypothesis. Therefore, we deem our results as likely being conservative.
In conclusion, we used a method to define caregiver stress which may allow for easier comparison across different study populations. This method may even have applications in the clinical setting, allowing pediatric health care providers to measure stress among caregivers in a standardized fashion. We found that psychosocial stress is high among caregivers of inner-city children with asthma, and is independently associated with childhood asthma morbidity. Further study is needed to elucidate mechanisms underlying this association so that interventions can be considered.
Supplementary Material
Clinical Implications.
Our novel method of defining high stress among caregivers of asthmatic children considers PSS-4 scores in relation to normative data, allowing for comparison across study populations. When applied to inner-city caregivers, stress was associated with worsened asthma morbidity among children.
Acknowledgments
Funding: This study was supported by grants K23 AI 106945 (PI Gaffin), K23 AI104780 (PI Sheehan), R01 AI 073964, K24 AI 106822, U01 AI 110397 from the National Institutes of Health (PI Phipatanakul) and by Aerocrine, Inc (Kopel, 2012 Fellows Program Award in Asthma/Allergy/Immunology/Pulmonary/Critical Care), and the American Lung Association/American Academy of Allergy, Asthma, and Immunology Respiratory Diseases Award (Phipatanakul).
The work was conducted with support from Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences), National Institutes of Health Award UL1 TR001102, and financial contributions from Harvard University and its affiliated academic healthcare centers.
We would like to acknowledge Ann Bailey, and the community of parents, nurses, research staff, teachers, school administrators, and children who have contributed to this work. We would also like to acknowledge the following organizations that funded or supported this research: National Institutes of Health, Aerocrine, Inc, American Lung Association/American Academy of Allergy, Asthma, and Immunology, Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences), Harvard University and its affiliated academic healthcare centers.
Abbreviations
- PSS-4
4-item perceived stress scale
- SES
socioeconomic status
- SICAS
School Inner City Asthma Study
Footnotes
Statement of Authors’ Contributions: All authors made significant contributions to the conception of the study, data acquisition and analysis, and data interpretation, drafting of the manuscript and/or critical revision of the manuscript. All authors also gave approval of the final version of the manuscript for publication. All authors agree to be accountable for all aspects of the work, including the accuracy and integrity of the work.
Disclaimer: The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Clinical Trial Registration: NCT01756391
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wright RJ, Cohen S, Carey V, Weiss ST, Gold DR. Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. American Journal of Respiratory and Critical Care Medicine. 2002;165(3):358–65. doi: 10.1164/ajrccm.165.3.2102016. Epub 2002/01/31. [DOI] [PubMed] [Google Scholar]
- 2.Cohen S, Williamson GM. Perceived Stress in a Probability Sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park: Sage; 1988. pp. 31–67. [Google Scholar]
- 3.Phipatanakul W, Bailey A, Hoffman EB, Sheehan WJ, Lane JP, Baxi S, et al. The school inner-city asthma study: design, methods, and lessons learned. The Journal of asthma: official journal of the Association for the Care of Asthma. 2011;48(10):1007–14. doi: 10.3109/02770903.2011.624235. Epub 2011/10/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. Journal of Allergy and Clinical Immunology. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. Epub 2007/12/06 S0091-6749(07)01823-4 [pii] [DOI] [PubMed] [Google Scholar]
- 5.Islam T, Urman R, Gauderman WJ, Milam J, Lurmann F, Shankardass K, et al. Parental stress increases the detrimental effect of traffic exposure on children’s lung function. American Journal of Respiratory and Critical Care Medicine. 2011;184(7):822–7. doi: 10.1164/rccm.201104-0720OC. Epub 2011/06/28 201104-0720OC [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104(6):1274–80. doi: 10.1542/peds.104.6.1274. Epub 1999/12/10. [DOI] [PubMed] [Google Scholar]
- 7.Evatt DP, Kassel JD. Smoking, arousal, and affect: the role of anxiety sensitivity. Journal of anxiety disorders. 2010;24(1):114–23. doi: 10.1016/j.janxdis.2009.09.006. Epub 2009/10/13. [DOI] [PubMed] [Google Scholar]
- 8.Wolf JM, Miller GE, Chen E. Parent psychological states predict changes in inflammatory markers in children with asthma and healthy children. Brain, behavior, and immunity. 2008;22(4):433–41. doi: 10.1016/j.bbi.2007.10.016. Epub 2007/12/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baxi SN, Sheehan WJ, Gaffin JM, Yodying J, Panupattanapong S, Lane JP, et al. Agreement between parent and student responses to an asthma and allergy questionnaire in a diverse, inner-city elementary school population. Ann Allergy Asthma Immunol. 2011;107(4):371–3. doi: 10.1016/j.anai.2011.08.007. Epub 2011/10/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.