Abstract
Importance, Objective
Studies on the relation between service attendance and mortality often have been limited by inadequate methodology for reverse causation, inability to assess effects over time, and limited information on mediators and cause-specific mortality.
Design, Setting, Participants, Main Outcomes and Measures
We evaluated associations between attendance and mortality in a prospective cohort, the Nurses’ Health Study (NHS), which included 74,534 women who were free of cardiovascular disease (CVD) and cancer at baseline. Religious service attendance was assessed by a self-reported question and was collected in 1992 and every four years subsequently. We used Cox proportional hazard model and marginal structural models with time-varying covariates to examine the association of religious service attendance with all-cause and cause-specific mortality. We adjusted for a wide range of demographic covariates, lifestyle factors and medical history measured repeatedly during the follow-up, and performed sensitivity analyses to examine the influence of potential unmeasured and residual confounding.
Results
During follow-up from 1996 until 2012, we identified 13,537 deaths, including 2,721 due to cardiovascular diseases and 4,479 due to cancer. After multivariate adjustment for major lifestyle, risk factors and attendance in 1992, attending religious service more than once/week was associated with 33% lower all-cause mortality, compared with women who had never attended religious services (Hazard Ratio [HR]=0.67, 95% confidence interval [CI]: 0.62–0.71, p for trend <0.0001). Comparing women who attended religious services more than once per week with those who never attend, the HR for cardiovascular mortality was 0.73 (0.62–0.85, p for trend <0.0001); and cancer mortality was 0.79 (0.70–0.89, p for trend <0.0001). Results were robust in sensitivity analysis. We found evidence that social support, depressive symptoms, smoking and optimism mediated the relationship between attendance and mortality.
Conclusions and Relevance
Frequent religious service attendance was associated with significantly lower risk of all-cause, cardiovascular and cancer mortality.
Keywords: Religious service attendance, mortality, causal model
Background
The World Health Organization defines health as “a state of complete physical, mental, and social well-being”1. Certain religious groups and others likewise view health holistically and emphasize the unity of body, mind, and spirit2–4. Health is often viewed as an inseparable component of spiritual well-being within some religious understandings5,6. Religious participation and beliefs can affect individual behavior, shift cognition and emotion, promote compassion, shape communities and public life, and may otherwise promote well-being and health/wholeness, but religion can also promote guilt, anxiety, violence and intolerance. A priori its effects on health are not thus immediately clear. Religious practice is common in America: Approximately 65% of Americans consider religion to be an important part of life, 83% report praying to God in the last week and 43% report having attended a religious service in the past week7,8.
A meta-analysis of studies related to the connection between religious service attendance and mortality between 1994 and 2009 concluded that “religious service attendance helped reduce mortality by 18% in healthy populations”9–12. Research on religion and health has led to some controversy. Sloan et al. questioned the validity of these studies and argued that the evidence is often weak and unconvincing with poor methodology and study design13,14. Denberg et al. criticized this kind of “research” as “simply reporting an association and then calling for more future research” arguing it was “trivial and unworthy of publication”15. Koenig et al. responded that Sloan et al.’s review was highly selective and biased with a misunderstanding of the epidemiological method16.
Much of the debate concerned major methodological limitations in previous studies9,17 that it was difficult to infer causality and that the observed association could be due to reverse causation if only healthy participants are able to attend services. Some stronger longitudinal studies have been published18–20.
However, to the best of our knowledge, no previous study has used methodology for repeated measures and time-dependent confounding that handles potential reverse causation between service attendance and health and evaluates “incident” rather than “prevalent” religious service attendance with mortality. We propose to address these issues using the Nurses’ Health Study, a large prospective cohort study among U.S. women with repeated measurements of religious service attendance, including detailed information on dietary, lifestyle, medical history and long-term follow-up. In addition, we could assess interactions with race, time-varying effects, and cause-specific mortality.
Methods
Study design
The Nurses’ Health study (NHS) began in 1976 and included 121,700 nurses aged 30–55 years from across the United States21. Information on lifestyle and medical history was collected using a self-administered questionnaire at baseline and every 2 years thereafter. Religious service attendance information was self-reported first in 1992, and every four years subsequently, in response to the question: “How often do you go to religious meetings or services? Response categories include “more than once a week, once a week, 1–3 times per month, less than once per month, never or almost never”. We defined baseline for this analysis as attendance as assessed in 1996; we used attendance in 1992 as an additional covariate. Follow-up for mortality continued until 2012. Participants who died before the baseline 1996, or did not reply to the 1996 questionnaire (n=27,122), who had 1996 religious service attendance missing (n=7,246), or had a diagnosis of cardiovascular disease (n=4,362) or cancer (n=8,457, except non-melanoma skin cancer) before 1996 were excluded. Participants were followed up from the return of the 1996 questionnaire until death, loss of follow-up, or the end of follow-up at June 2012, whichever came first. Our study includes 74,534 participants with 1,104,175, person years. We identified 13,537 total deaths, 2,721 cardiovascular deaths and 4,479 cancer deaths during follow up. The study protocol was approved by the institutional review boards of Brigham and Women’s Hospital and Harvard T. H. Chan School of Public Health.
Outcome
All-cause and cause-specific mortality was assessed between the return of the 1996 questionnaire and the end of follow-up (June 2012). Death events were identified through reports from next of kin and the National Death Index. We identified causes of death based on family reports, death certificates, and medical record. We searched in the National Death Index for names of non-responders and this has been shown to have good sensitivity and specificity22. We used International Classification of Diseases code, 8th revision (ICD-8) to define cancer related deaths (ICD:140–207), and cardiovascular disease related deaths (ICD: 390–459 and 795). We used the following ICD codes to identify detailed subcategories of cardiovascular disease and cancer: ischaemic heart disease (IHD; ICD codes 410–414), cerebrovascular disease (430–438), and any other CVD (ICD codes 390–459 and 795 excluding 410–414 and 430–438); cancers of the lung (ICD code 162), breast (174), ovaries (183), pancreas (157), colon or rectum (153), non-Hodgkin’s lymphoma (200, 202, 204), and cancer of other sites.
Covariates
We adjusted the analyses for the following known predictors of mortality in this cohort: age (continuous, years), alcohol consumption (none, 0.1–4.9, 5.0–14.9, ≥15.0 g/d), physical exercise (metabolic equivalent hours per week; quintiles), multivitamin use (yes, no), hypertension (yes, no), hypercholesterolemia (yes, no), type 2 diabetes (yes, no), menopausal status (premenopausal, postmenopausal) and post-menopausal hormone use (never, past and current), physical exam in the past 2 years (no, yes for symptoms and yes for screenings), Alternative Healthy Eating Index 2010 score (quintiles)23, smoking status (never, former, current), pack-years (<10, 10–19, 20–39, ≥40 pack-years for former smokers; <25, 25–44, 45–64, ≥65 pack-years for current smokers), BMI (kg/m2; <21, 21–22.9, 23–24.9, 25–27.4, 27.5–29.9, 30–34.9, ≥35), husband’s education (less than high school, some high school, high school graduate, college, graduate school), good physical function (defined as absence of limitations in moderate activities or moderate limitations in demanding activities, yes, no24,25), social integration score (social integration was derived included the following 6 components: Marital status, other group participation, number of close friends, number of close relatives, number of close friends see at least once per month, number of close relatives seen at least once per month26, quartiles), living alone (yes, no), median income of the family (dollars per year, quintiles), geographic region (north, south, middle, other), depression in 1992 (yes, no), and religious service attendance in 1992 (never, < 1/week, ≥ 1/week). Indicator variables were used for any missing covariate information for categorical variables and median imputation was used for missing continuous covariates.
For mediation analysis, covariate measurements prior to the religious attendance exposure were taken as potential confounders and those subsequent to religious attendance exposures were taken as potential mediators. For mediators, we considered the first measure available subsequent to 1996 which included depressive symptoms in 2000 measured using the Center for Epidemiologic Studies Depression-10 (CESD-10)27, smoking, alcohol consumption, and diet quality in 1998, number of close friends and have someone close to talk to in 2000, and optimism and phobic anxiety in 2004 measured using the Crown-Crisp Index (CCI)28.
Statistical analyses
We examined the association of religious service attendance with all-cause and cause-specific mortality using various analytic strategies including Cox proportional hazard models and marginal structural models with weights accounting for missing data and censoring. The marginal structural models account for reverse causation and time-varying confounding by weighting and are described at length elsewhere, and also in the online supplement29,30. Person time was accrued from baseline (return of the 1996 questionnaire) until the date of death, loss to follow up, or June 2012, whichever came first. We calculated hazard ratios and its 95% confidence interval comparing frequency of religious services attendance (more than, or equal to, or less than once per week) vs. never attend, for all-cause mortality and cause-specific mortality. For cause-specific mortality, we also further adjusted for cause-specific risk factors. Linear trends across categories of religious service attendance were tested by modeling attendance frequency as a continuous variable. Confounders were adjusted for in 1992 in the proportional hazards models; confounders were updated over time in the marginal structural model. We examined the joint effect of religious service attendance in 1996 and 2000 with all-cause mortality. We further stratified the analysis by race/ethnic groups (among Caucasians and African Americans only), and religious group (among Catholic and Protestant only). Likelihood ratio tests were used to assess the significance of the interaction. The relative excess risk due to interaction (RERI) and its 95% confidence interval were calculated31,32.
We applied mediation analysis methods33,34 to examine proportions of the association between religious service attendance in 1996 and mortality in 2012 that was mediated by the following factors: current smoking, alcohol intake, and diet quality in 1998, social support and depressive symptoms in 2000, phobic anxiety in 2004, optimism in 2004, and components of social integration in 2000 (including currently married, number of close friends, number of close relatives, seen close friends at least once per month, seen close relatives at least once per month, and hours of social group participation). For the mediation analysis, we further excluded participants who had mediator information missing, or who died between baseline and the mediator measurement. These mediators were selected a priori based on subject knowledge and assessed using multivariate logistic regression and linear regression models of the outcome and of the potential mediator, the results of which are then combined to estimate direct and indirect effects33,34. Methods for mediation assume baseline covariates suffice to control for exposure-outcome, mediator-outcome, and exposure-mediator confounding. Proportion mediated on a risk difference scale was calculated as the indirect effect divided by total effect and tests were conducted for evidence of mediation.
We conducted several sensitivity analyses to test the robustness of our results. To minimize the influence of reverse causation, we additionally performed subgroup analyses among participants who were free living (not living in a nursing home), never smokers, with no physical or functional limitations, no major medical comorbidities (such as depression), and exclusion of death events in the first 4 years of follow up. We compared effects sizes of religious service attendance with other components of social integration and with other covariates. We also updated covariates, modeled service attendance as time varying exposure, compared hazard ratios over different specific time frames of follow-up, and with different analytic strategies as sensitivity analyses. We examined the change of service attendance over time, and also calculated years of live saved35. We further assessed how substantial residual unmeasured confounding would need to be to explain away the observed associations36,37.
Results
Among 74,534 women at 1996 baseline with reported religious service attendance, 14,158 women attended more than once per week, 30,401 attended once per week, 12,103 attended less than once per week, and 17,872 never attended (Table 1). A majority of our study participants were Catholic or Protestant. Women who attended religious services more frequently tended to have fewer depressive symptoms; were less likely to be current smokers; and more likely to be married (Table 1). During follow up, a large majority of participants maintained their levels of service attendance but there was also considerable movement across all categories (eTable 1).
Table 1.
Age-adjusted baseline characteristics of study participants by frequency of religious service attendance in 1996
| Religious service attendance in 1996 | ||||
|---|---|---|---|---|
| Almost never (n=17872) |
Less than once/week (n=12103) |
Once/week (n=30401) |
More than once/week (n=14158) |
|
| Age at 1996,yeara | 61.1(7.1) | 60.8(7.2) | 62.1(7.1) | 63.2(6.9) |
| Religious service attendance in 1992 | ||||
| Almost never,% | 78.6 | 19.1 | 3.0 | 1.1 |
| Less than once/week,% | 18.4 | 67.4 | 15.8 | 4.5 |
| Once or more than once/week, % | 3 | 13.5 | 81.2 | 94.4 |
| Caucasians, % | 98 | 97 | 98 | 97 |
| Religious group | ||||
| Catholic, % | 29 | 28 | 54 | 41 |
| Protestant, % | 62 | 62 | 43 | 52 |
| Other Christian, % | 2 | 2 | 2 | 6 |
| Ashkenazi Jewish, % | 4 | 6 | 1 | 0 |
| Sephardic Jewish, % | 0 | 0 | 0 | 0 |
| Eastern (e.g. Buddhist, Hindu), % | 0 | 0 | 0 | 0 |
| Muslim, % | 0 | 0 | 0 | 0 |
| Other religious heritage | 2 | 1 | 1 | 1 |
| Pass through | 1 | 1 | 0 | 0 |
| College and graduate school, % | 56 | 57 | 54 | 54 |
| Diabetes, % | 6 | 7 | 6 | 6 |
| Hypertension, % | 40 | 41 | 39 | 38 |
| Hypercholesterolemia, % | 52 | 53 | 53 | 53 |
| Physical exam in past two years, % | 87 | 90 | 91 | 91 |
| Current hormone use, % | 49 | 51 | 48 | 50 |
| Geographic region, % | ||||
| North | 37 | 37 | 36 | 33 |
| West | 13 | 11 | 9 | 13 |
| Middle | 40 | 42 | 45 | 44 |
| Other | 10 | 10 | 10 | 10 |
| Body mass index, kg/m2 | 26.5(5.5) | 26.6(5.3) | 26.5(5.1) | 26.5(5.1) |
| Physical activity, METs-hrs/wk | 17.7(22.9) | 18.2(21.6) | 17.7(22.0) | 17.8(20.5) |
| Current smokers, % | 20 | 14 | 10 | 5 |
| Age at first birth, years | 24.7(3.9) | 24.8(3.8) | 24.8(3.7) | 24.8(3.9) |
| Parity | 2.9(1.6) | 2.9(1.6) | 2.9(1.6) | 2.9(1.6) |
| No physical function limitation, % | 48 | 49 | 52 | 51 |
| Depression in 1996, % | 8 | 7 | 6 | 5 |
| Multiple vitamin use, % | 51 | 55 | 52 | 56 |
| Alcohol consumption, g/day | 6.8(11.2) | 5.4(9.0) | 4.6(8.3) | 3.4(7.2) |
| Live alone, % | 17 | 16 | 14 | 15 |
| Not employed in last 2 years, % | 40 | 37 | 39 | 43 |
| Alternative Healthy Eating Index 2010 | ||||
| Quintile 5 (best diet quality), % | 19 | 20 | 20 | 21 |
| Current smoking in 1998 | 6.6 (9) | 5.4(9.2) | 4.6(8.4) | 3.4(7.3) |
| Alcohol consumption in 1998, g/day | 6.6(10.9) | 5.4(9.2) | 4.6(8.4) | 3.4(7.3) |
| Depressive symptoms in 2000 | 79.3(14.4) | 80.1(13.4) | 80.9(12.9) | 82.3(12.2) |
| Social Integration score in 2000 | 4.2(2.6) | 4.9(2.8) | 5.4(2.7) | 5.9(2.8) |
| Currently married in 2000, % | 70 | 72 | 76 | 77 |
| Number of close relatives seen monthly 2000 | 1.9(1.1) | 2.2(1.2) | 2.3(1.2) | 2.4(1.3) |
| Number of close friends seen monthly 2000 | 2.7(1.1) | 2.9(1.1) | 2.9(1.1) | 3.2(1.1) |
| Relatives you feel close to 2000 | 3.0(1.5) | 3.2(1.5) | 3.4(1.5) | 3.5(1.5) |
| Number of close friends 2000 | 3.2(1.2) | 3.4(1.1) | 3.5(1.2) | 3.6(1.2) |
| Hours/week in social groups 2000 | 1.9(1.4) | 2.0(1.4) | 2.3(1.3) | 2.9(1.3) |
| Optimism score in 2004 | 24.1(4.9) | 24.4(4.8) | 24.5(4.8) | 25.2(4.4) |
| Phobic Anxiety score in 2004 | 2.9(2.4) | 2.9(2.4) | 3.0(2.5) | 2.8(2.4) |
Values are means(SD) or percentages and are standardized to the age distribution of the study population.
Value is not age adjusted
Covariates were taken from 1996 questionnaire
Using a Cox proportional hazard model, compared with women who never attended religious services, women who attended regularly had lower mortality in follow-up (Figure 1) with multivariate adjusted HR=0.67 (95%CI: 0.62–0.71) for those attending more than once per week in 1996; HR=0.74 (95%CI: 0.70–0.78) for those attending weekly and HR=0.87 (95%CI: 0.81–0.92) for those attending less than weekly (p for trend <0.0001). Those who attended regularly in both 2000 and 1996 had even lower mortality rates with multivariate adjusted HR=0.55 (95%CI: 0.52–0.59) (Table 2). When using marginal structural models to better address potential feedback and reverse causation, the effect sizes were similar (Table 2). Results were also similar in analyses among participants who were free living, never smokers, with no physical or functional limitations, no major medical comorbidities (such as depression), and exclusion of death events in the first 4 years of follow up (eTable2, 3). Effect size of religious service attendance was comparable to physical activity and BMI (eTable 4). The inverse association between service attendance and mortality were consistent over time (eTable5). Religious service attendance was associated with 0.43 (95%CI: −0.09 −1.54) years longer survival for women who regularly attend services once per week or more (eTable 6).
Figure 1. Cumulative incidence for all-cause mortality and religious services attendance in the Nurses’ Health Study, 1996–2012.
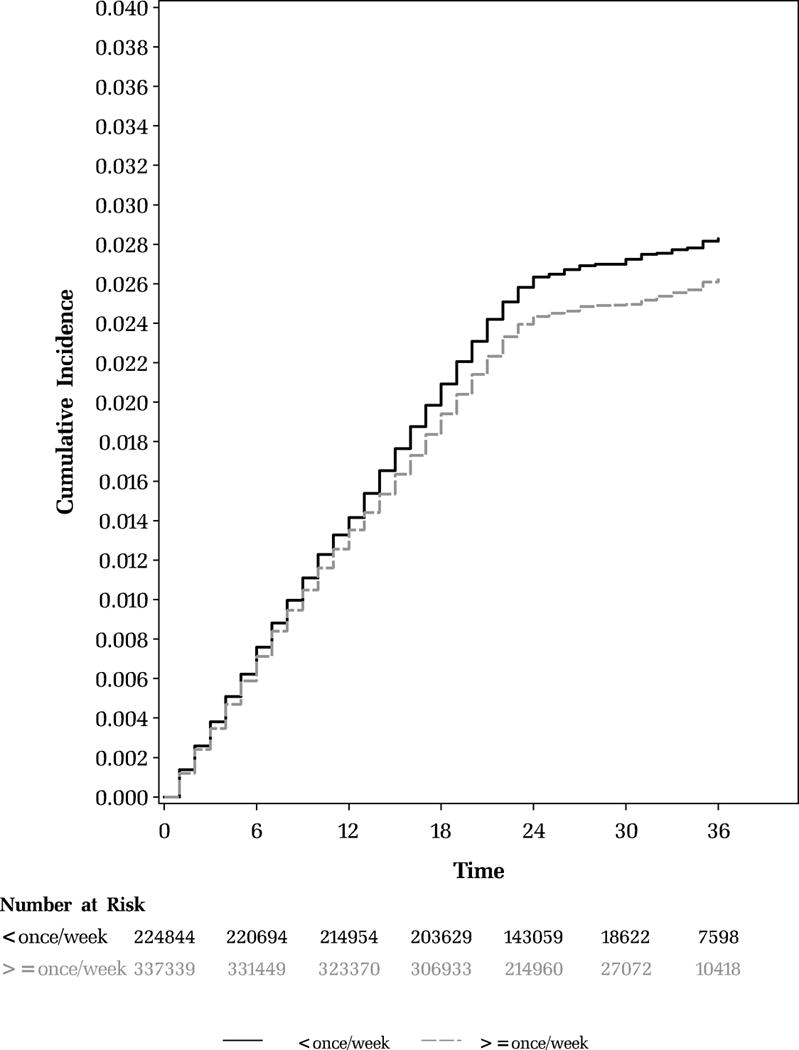
Hazard ratio = 0.67 (95% CI: 0.62–0.71)
Multivariable model adjusted for age (continuous), alcohol consumption (none, 0.1–4.9, 5.0–14.9, ≥15.0 g/d), physical exercise (metabolic equivalent hours per week; quintiles), multivitamin use (yes, no), hypertension (yes, no), hypercholesterolemia (yes, no), type 2 diabetes (yes, no), depression (yes, no), menopausal status (premenopausal, postmenopausal) and post-menopausal hormone use (never, past and current), physical exam in the past 2 years (no, yes for symptoms and yes for screenings), healthy eating score (quintiles), smoking status (never, former, current), pack-years (<10, 10–19, 20–39, ≥40 pack-years for former smokers; <25, 25–44, 45–64, ≥65 pack-years for current smokers), and BMI (kg/m2; <21, 21–22.9, 23–24.9, 25–27.4, 27.5–29.9, 30–34.9, ≥35), husband’s education (less than high school, some high school, high school graduate, college, graduate school), good physical or function (yes, no), social integration score (quartiles), live alone (yes, no), median family income (continuous, dollars per year), geographic region (north, south, west, other), and religious service attendance in 1992 (never, < 1/week, ≥ 1/week). Social integration score, including score and frequency of relatives and friends were derived based on the definition from Am J Epidemiol 1979;109:186–204. For adjustment, we derived social integration score without religious service attendance components.
P trend <0.0001 for Cox model
Table 2.
Joint effects of religious services attendance in 1996 and 2000 with all-cause mortality in the Nurses’ Health Study, 2000–2012
| Religious Service Attendance | Case No./person years | All-cause mortality Cox model Multivariable HR (95% CI) |
All-cause mortality MSM model Multivariable HR (95% CI) |
|
|---|---|---|---|---|
| 1996 | 2000 | |||
| < once/week | Never | 5897/322052 | 1.00 (reference) | 1.00 (reference) |
| < once/week | < once/week | 1140/132130 | 0.71(0.66, 0.76) | 0.45(0.40, 0.50) |
| < once/week | once/week | 425/40790 | 0.76(0.68, 0.84) | 0.48(0.41, 0.58) |
| < once/week | > once/week | 73/6535 | 0.85(0.67, 1.07) | 0.54(0.35, 0.83) |
| ≥ once/week | never | 157/7828 | 0.90(0.77, 1.07) | 1.13(0.93, 1.36) |
| ≥ once/week | < once/week | 526/53736 | 0.71(0.65, 0.78) | 0.46(0.40, 0.54) |
| ≥ once/week | once/week | 3517/348329 | 0.61(0.58, 0.64) | 0.52(0.48, 0.56) |
| ≥ once/week | > once/week | 1802/192776 | 0.55(0.52, 0.59) | 0.50(0.46, 0.54) |
HR: hazard ratio; CI: confidence interval
Multivariable model adjusted for age (continuous), alcohol consumption (none, 0.1–4.9, 5.0–14.9, ≥15.0 g/d), physical exercise (metabolic equivalent hours per week; quintiles), multivitamin use (yes, no), hypertension (yes, no), hypercholesterolemia (yes, no), type 2 diabetes (yes, no), depression (yes, no), menopausal status (premenopausal, postmenopausal) and post-menopausal hormone use (never, past and current), physical exam in the past 2 years (no, yes for symptoms and yes for screenings), healthy eating score (quintiles), smoking status (never, former, current), pack-years (<10, 10–19, 20–39, ≥40 pack-years for former smokers; <25, 25–44, 45–64, ≥65 pack-years for current smokers), and BMI (kg/m2; <21, 21–22.9, 23–24.9, 25–27.4, 27.5–29.9, 30–34.9, ≥35) and husband’s education (less than high school, some high school, high school graduate, college, graduate school), good physical or function (yes, no), live alone (yes, no), median family income (continuous, dollars per year), geographic region (north, south, west, other), social integration score without religious service attendance component (quartiles), and religious service attendance in 1992 (never, < 1/week, ≥ 1/week).
In the Cox model, for an unmeasured confounder to explain away the hazard ratio estimate of 0.67, the unmeasured confounder would have to both increase the likelihood of service attendance and decrease the likelihood of mortality by 2.35-fold, above and beyond the measured confounders. For an unmeasured confounder to bring the upper confidence limit of 0.71 for this estimate above 1, the unmeasured confounder would still have to both increase the likelihood of service attendance and decrease the likelihood of mortality by 2.16-fold. Similar substantial confounding would be needed to explain away the other estimates.
For cause-specific mortality, frequent religious service attendance was also inversely associated with cardiovascular mortality and cancer mortality, with HR=0.73 (0.62–0.85, p for trend<0.0001), and 0.79 (0.70–0.89, p for trend<0.0001) respectively (Table 3). Attendance was associated with lower cerebrovascular disease and other cardiovascular diseases mortality, but not ischemic heart disease (eTable 7). For site specific cancer mortality, frequent religious service attendance is associated with significantly lower risk of breast cancer mortality and colorectal cancer mortality, but not for other sites of cancer (eTable 8). Although attendance was associated with lower cardiovascular mortality and cancer mortality, attendance was not associated with breast cancer incidence (eTable 9) and only weakly associated with incidence of cardiovascular disease (eTable 10).
Table 3.
Multivariate adjusted hazard ratios between religious services attending and cardiovascular disease and cancer mortality in the Nurses’ Health Study, 1996–2012
| Mortality | Religious service attendance
|
P for trend | |||
|---|---|---|---|---|---|
| Never | Less than once/week | Once/week | More than once/week | ||
| All cardiovascular disease (2,721) | |||||
| Cases No. | 670 | 378 | 1116 | 557 | |
| Age-adjusted HR (95% CI) | 1.00 (ref) | 0.86(0.74, 0.99) | 0.74(0.66, 0.82) | 0.62(0.54, 0.71) | <0.0001 |
| Multivariable HR (95% CI) | 1.00 (ref) | 0.92(0.79, 1.06) | 0.80(0.70, 0.91) | 0.73(0.62, 0.85) | <0.0001 |
| All cancer (4,479) | |||||
| Cases No. | 1255 | 692 | 1752 | 780 | |
| Age-adjusted HR (95% CI) | 1.00 (ref) | 0.78(0.70, 0.87) | 0.71(0.66, 0.77) | 0.59(0.54, 0.66) | <0.0001 |
| Multivariable HR (95% CI) | 1.00 (ref) | 0.91(0.81, 1.01) | 0.86(0.78, 0.95) | 0.79(0.70, 0.89) | <0.0001 |
HR: hazard ratio; CI: confidence interval
Multivariable model adjusted for age (continuous), alcohol consumption (none, 0.1–4.9, 5.0–14.9, ≥15.0 g/d), physical exercise (metabolic equivalent hours per week; quintiles), multivitamin use (yes, no), hypertension (yes, no), hypercholesterolemia (yes, no), type 2 diabetes (yes, no), depression (yes, no), menopausal status (premenopausal, postmenopausal) and post-menopausal hormone use (never, past and current), physical exam in the past 2 years (no, yes for symptoms and yes for screenings), healthy eating score (quintiles), smoking status (never, former, current), pack-years (<10, 10–19, 20–39, ≥40 pack-years for former smokers; <25, 25–44, 45–64, ≥65 pack-years for current smokers), and BMI (kg/m2; <21, 21–22.9, 23–24.9, 25–27.4, 27.5–29.9, 30–34.9, ≥35), husband’s education (less than high school, some high school, high school graduate, college, graduate school), good physical or function (yes, no), live alone (yes, no), median family income (continuous, dollars per year), geographic region (north, south, west, other), social integration score without religious service attendance component (quartiles), and religious service attendance in 1992 (never, < 1/week, ≥ 1/week).
Comparing Caucasians and African Americans, the hazard ratio comparing those attending more than once per week to not at all was 0.88 (0.85–0.92) for Caucasians and 0.64 (0.46–0.90) for African Americans, though multiplicative interaction between the effect of attendance on mortality by race was not statistically significant (p for interaction =0.08, eTable 11). The hazard ratios for service attendance were comparable for Protestants and Catholics; for each level of service attendance, Catholics had slightly lower mortality than Protestants (eTable 12). We further compared the magnitude of the association of religious service attendance with other aspects of social integration and found that the inverse association with mortality was strongest for religious service attendance (eTable 13).
We used mediation analysis to estimate the proportion of the association that was mediated through each mediator. Depressive symptoms, smoking, social support and optimism were potentially important mediators, though the overall proportion of the association that was mediated through each mediator was moderate e.g. smoking explained about 22% of the effect, social support 23% etc. (Table 4).
Table 4.
Mediation analysis between religious service attendance in 1996 and all-cause mortality in 2012
| Mediator | Proportion Mediated | P value for Indirect Effect |
|---|---|---|
| Depressive Symptomsa | 11% | <0.001 |
| Current smoking b | 22% | <0.001 |
| Alcohol c | 0.2% | 0.76 |
| Diet quality d | −0.03% | 0.94 |
| Phobic Anxiety e | −1% | 0.65 |
| Optimism f | 9% | <0.001 |
| Social Integration Score derived without religious service attendance | 23% | 0.003 |
Depressive symptoms: continuous score in 2000; Depressive symptoms was measured using the Center for Epidemiologic Studies Depression-10 (CESD-10)26
Smoking: Current smoking vs. Past or Never smoking in 1998
Alcohol: defined as a binary variable, heavy drinker (>50g/d) vs. moderate or never drinker in 1998
Diet quality: defined as AHEI 2010 score51, continuous in 1998
Phobic Anxiety: Continuous score measured in 2004. Phobic Anxiety was measured using the Crown-Crisp Index (CCI)
Optimism: Continuous score, measured in 2004
Discussion
In this large prospective cohort of U.S. nurses, we found a consistent inverse association between frequent religious service attendance and all-cause mortality, cardiovascular mortality and cancer mortality. Compared with women who never attended religious services, women who attended more than once per week had 33% lower mortality risk; results were robust across different race/ethnicity groups, different analytic strategies and in sensitivity analyses.
In examining the potential pathways from religious service to all-cause mortality, we found that depressive symptoms, smoking, social support and optimism were potentially important mediators. No single mediator explained more than about 25% of the effect. There may be many pathways from religious service attendance to health. However, the proportion of effects mediated may be underestimated as mediators were considered only at a single point in time, and are measured imperfectly. Moreover, some individuals died before the mediators occurred and were excluded further which may affect our results. Future studies implementing causal mediation analysis with time-varying religious service attendance, time-varying mediators, and confounders are warranted. Other mechanisms that have been proposed that were not assessed here include increasing psychosocial resilience, religious coping mechanisms, purpose in life, and improving self-discipline38.
Our findings were consistent with previous study findings and the effect sizes were similar or somewhat larger, especially when examining associations with consistent pattern of service attendance. Literature supports the notion that religious service attendance is associated with better health and reduced mortality14,39–44. In our study, we were able to account for time-dependent confounding and examined the association between repeated measures of religious service attendance with long-term all-cause and cause-specific mortality. Although our study was not targeted to a particular religious group, the study in fact consists mainly of Caucasian Christians. Our results might not be generalizable to the general population, or to other countries, or to areas with limited religious freedom. Our study moreover consists of U.S. nurses with similar socioeconomic status who tend to be more health conscious. Our analysis is also restricted to the specific time period under consideration and the effects of service attendance may vary over time as the nature of attendance itself changes. Although frequency of service attendance did not substantially change in our study, it is possible that the content of the services themselves changed and this needs to be taken into account in interpretation. Further research could examine other religious practices, mindfulness practices, other aspects of spirituality and religiosity, other race/ethnicity and demographic groups, and could also further investigate the potential underlying mechanisms45,46. Our results do not imply that health care providers should prescribe religious service attendance, but for those who do already hold religious beliefs, service attendance could be encouraged as a form of meaningful social participation.
One limitation of our study is that we only have one single domain measure of religiosity or spirituality, namely, service attendance. This captures only one aspect of religiosity and may be subject to measurement error and over-reporting47–49, though with over-reporting the relative ordering of frequency might still be preserved. There is no reason to think that individual over-reporting would be related to mortality, and such non-differential misclassification in fact tends to yield conservative effect estimates50. Our finding of substantially lower breast cancer mortality in frequent attenders, despite no association for breast cancer incidence, lends support to an effect of social participation, and enhances the plausibility of our results. Religious service attendance may be highly correlated with other measures of social engagement, such as number of close friends and having someone close to talk to, which are significant predictors for lower mortality and thus may serve as important mechanisms. However, a number of studies of the health effects of religious attendance4,51 have examined the role of other measures of social engagement and find that religious attendance has robust effects even after the inclusion of these measures. In our study, this was also the case, and we moreover found that the inverse association with mortality was driven substantially by religious service attendance.
Clearly a randomized trial of religious service attendance is neither ethical nor feasible. Our study is an observational study. Although we adjusted for major confounders for the association between religious service attendance and mortality, the results may still be subject to unmeasured confounders and residual confounding. Personal, social, psychological, and socio-economic characteristics that may confound service attendance could be a potentially plausible explanation for the association. Some of the mediators are also potential confounders, which we adjusted at baseline. However, we performed sensitivity analyses techniques to assess how strong unmeasured confounding would need to be to explain away the observed association. For an unmeasured confounder to explain away the association of service attendance and mortality it would have to both increase the likelihood of service attendance and decrease the likelihood of mortality by 2.35-fold, above and beyond the measured covariates. Such substantial confounding by unmeasured factors seems unlikely given adjustment for an extensive set of covariates. We also performed subgroup analyses among participants who were free living, never smokers, no physical or functional limitations, no major medical comorbidities (such as depression), and exclusion of death events in the first 4 years of follow up, and estimates were similar.
Strengths of our study include a large sample size, long duration of follow-up, prospective cohort study design, and repeated measures of religious service attendance, analytic methods for feedback and reverse causation, and extensive confounding control. We have clear temporality of the exposure, covariates and outcome, and also have been able to adjust for baseline religious service attendance, baseline confounders, and account for time-dependent confounding. Our results were robust to methodology to address potential reverse causation.
Conclusion
In this large prospective long-term cohort study of US women, frequent religious service attendance, particularly recent service attendance, was associated with lower all-cause mortality, cardiovascular and cancer mortality.
Supplementary Material
Acknowledgments
Shanshan Li and Tyler J. VanderWeele had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Shanshan Li and Tyler J. VanderWeele from Harvard T. H. Chan School of Public Health have conducted and are responsible for the data analysis. The authors have no disclosures. The funding organization played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding: The Nurses’ Health Study was funded by U.S. National Institutes of Health (NIH) UM1 CA186107. The analysis and paper was supported by a research grant from the Templeton Foundation.
This study was approved by the institutional review boards at Harvard T. H. Chan School of Public Health. All authors have made (a) substantial contributions to the conception and design; or the acquisition, analysis, or interpretation of the data, (b) the drafting of the article or critical revision for important intellectual content, (c) final approval of the version to be published, and (d) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Footnotes
Conflict of Interest: None.
References
- 1.World Health Organization. http://www.who.int/mediacentre/factsheets/fs369/en/ Accessed March 10, 2016.
- 2.Balboni MJ, Puchalski CM, Peteet JR. The relationship between medicine, spirituality and religion: Three models for integration. Journal of Religion and Health. 2014;53(5):1586–1598. doi: 10.1007/s10943-014-9901-8. [DOI] [PubMed] [Google Scholar]
- 3.Koenig HG. Faith & Mental Health. Philadelphia, PA, USA: Templeton Foundation Press; 2005. [Google Scholar]
- 4.Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. Oxford: New York Oxford University Press; 2001. [Google Scholar]
- 5.Puchalski CM, Blatt B, Kogan M, Butler A. Spirituality and health: the development of a field. Academic Medicine: Journal of the Association of American Medical Colleges. 2014;89(1):10–16. doi: 10.1097/ACM.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 6.Puchalski CM, Vitillo R, Hull SK, Reller N. Improving the spiritual dimension of whole person care: reaching national and international consensus. Journal of Palliative Medicine. 2014;17(6):642–656. doi: 10.1089/jpm.2014.9427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crabtree S, Pelham B. What Alabamians and Iranians have in common; A global perspective on Americans’ religiosity offers a few surprises. Gallup Poll News Service. 2009 [Google Scholar]
- 8.Franck R, Iannaccone L. Religious decline in the 20th century West: testing alternative explanations. Public Choice. 2014;159(3):385–414. [Google Scholar]
- 9.McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: a meta-analytic review. Health Psychology: official journal of the Division of Health Psychology, American Psychological Association. 2000;19(3):211–222. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 10.Lucchetti G, Lucchetti AL, Koenig HG. Impact of spirituality/religiosity on mortality: comparison with other health interventions. Explore. 2011;7(4):234–238. doi: 10.1016/j.explore.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Hall DE. Religious attendance: more cost-effective than lipitor? Journal of the American Board of Family Medicine: JABFM. 2006;19(2):103–109. doi: 10.3122/jabfm.19.2.103. [DOI] [PubMed] [Google Scholar]
- 12.Larson DB, Larson SS, Koenig HG. Mortality and religion/spirituality: A brief review of the research. Annals of Pharmacotherapy. 2002;36(6):1090–1098. doi: 10.1345/aph.1A438. [DOI] [PubMed] [Google Scholar]
- 13.Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? The New England Journal of Medicine. 2000;342(25):1913–1916. doi: 10.1056/NEJM200006223422513. [DOI] [PubMed] [Google Scholar]
- 14.Sloan RP, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet. 1999;353(9153):664–667. doi: 10.1016/s0140-6736(98)07376-0. [DOI] [PubMed] [Google Scholar]
- 15.Denberg T. Religious attendance: More cost-effective than lipitor? The Journal of the American Board of Family Medicine. 2006;19(4):430. doi: 10.3122/jabfm.19.4.430. [DOI] [PubMed] [Google Scholar]
- 16.Koenig H, Idler E, Kasl S, et al. Religion, spirituality, and medicine: A rebuttal to skeptics. International Journal of Psychiatry In Medicine. 1999;29(2):123–131. doi: 10.2190/C2FB-95VW-FKYD-C8RV. [DOI] [PubMed] [Google Scholar]
- 17.VanderWeele T. Unmeasured confounding and hazard scales: sensitivity analysis for total, direct, and indirect effects. Eur J Epidemiol. 2013;28(2):113–117. doi: 10.1007/s10654-013-9770-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dupre M, Franzese A, Parrado E. Religious attendance and mortality: Implications for the black-white mortality crossover. Demography. 2006;43(1):141–164. doi: 10.1353/dem.2006.0004. [DOI] [PubMed] [Google Scholar]
- 19.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. American Journal of Public Health. 1997;87(6):957. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellison CG, Hummer RA, Cormier S, Rogers RG. Religious involvement and mortality risk among African American adults. (Age and health in a multiethnic society: Patterns and methods) Research on Aging. 2000;22(6):630. [Google Scholar]
- 21.Colditz GA, Hankinson SE. The Nurses’ Health Study: lifestyle and health among women. Nature Reviews Cancer. 2005;5(5):388–396. doi: 10.1038/nrc1608. [DOI] [PubMed] [Google Scholar]
- 22.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the national death index and equifax nationwide death search. Am J Epidemiol. 1994;140(11):1016–1019. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 23.Chiuve SE, Sampson L, Willett WC. The association between a nutritional quality index and risk of chronic disease. American Journal of Preventive Medicine. 2011;40(5):505–513. doi: 10.1016/j.amepre.2010.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun Q, Townsend MK, Okereke OI, et al. Alcohol consumption at midlife and successful ageing in women: A prospective cohort analysis in the Nurses’ Health Study. PLoS Medicine. 2011;8(9) doi: 10.1371/journal.pmed.1001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30(6):473. [PubMed] [Google Scholar]
- 26.Berkman L, Syme S. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda county residents. American Journal of Epidemiology. 1979;109(2):186. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 27.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 28.Burgess PM, Mazzocco L, Campbell IM. Discriminant validity of the Crown-Crisp Experiential Index. The British Journal of Medical Psychology. 1987;60(Pt 1):61–69. [PubMed] [Google Scholar]
- 29.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561. doi: 10.1097/00001648-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Robins JM, Hernán MÁ, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Knol MJ, VanderWeele TJ, Groenwold RH, Klungel OH, Rovers MM, Grobbee DE. Estimating measures of interaction on an additive scale for preventive exposures. European Journal of Epidemiology. 2011;26(6):433–438. doi: 10.1007/s10654-011-9554-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.VanderWeele TJ, Vansteelandt S. Invited commentary: Some advantages of the relative excess risk due to interaction (RERI)–towards better estimators of additive interaction. Am J Epidemiol. 2014;179(6):670–671. doi: 10.1093/aje/kwt316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.VanderWeele T. Explanation in causal inference: methods for mediation and interaction. Oxford University Press; 2015. [Google Scholar]
- 34.Valeri JL, Vanderweele JT. SAS Macro for causal mediation analysis with survival data. Epidemiology. 2015;26(2):e23–e24. doi: 10.1097/EDE.0000000000000253. [DOI] [PubMed] [Google Scholar]
- 35.Zucker D. Restricted mean life with covariates: Modification and extension of a useful survival analysis method. Journal of the American Statistical Association. 1998;93(442):702–709. [Google Scholar]
- 36.VanderWeele TJ. Unmeasured confounding and hazard scales: sensitivity analysis for total, direct, and indirect effects. European Journal of Epidemiology. 2013;28(2):113–117. doi: 10.1007/s10654-013-9770-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ding P, VanderWeele T. Sensitivity analysis without assumptions. Epidemiology. 2016 doi: 10.1097/EDE.0000000000000457. http://arxiv.org/abs/1507.03984. [DOI] [PMC free article] [PubMed]
- 38.Hill PL, Turiano NA. Purpose in life as a predictor of mortality across adulthood. Psychological Science. 2014;25(7):1482–1486. doi: 10.1177/0956797614531799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levin JS, Larson DB, Puchalski CM. Religion and spirituality in medicine: research and education. JAMA. 1997;278(9):792–793. doi: 10.1001/jama.278.9.792. [DOI] [PubMed] [Google Scholar]
- 40.Matthews DA, McCullough ME, Larson DB, Koenig HG, Swyers JP, Milano MG. Religious commitment and health status: a review of the research and implications for family medicine. Archives of Family Medicine. 1998;7(2):118–124. doi: 10.1001/archfami.7.2.118. [DOI] [PubMed] [Google Scholar]
- 41.Koenig HG. Medicine, religion, and health: where science & spirituality meet. West Conshohocken, PA: Templeton Foundation Press; 2008. [Google Scholar]
- 42.Levin JS. Religion and health: is there an association, is it valid, and is it causal? Social Science & Medicine (1982) 1994;38(11):1475–1482. doi: 10.1016/0277-9536(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 43.Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and U.S. adult mortality. Demography. 1999;36(2):273–285. [PubMed] [Google Scholar]
- 44.Oman D, Reed D. Religion and mortality among the community-dwelling elderly. Am J Public Health. 1998;88(10):1469–1475. doi: 10.2105/ajph.88.10.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Idler E, Musick MA, Ellison CG, et al. Measuring multiple dimensions of religion and spirituality or health research - Conceptual background and findings from the 1998 General Social Survey. Research On Aging. 2003;25(4):327–365. [Google Scholar]
- 46.Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality. American Psychologist. 2003;58(1):64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- 47.Hadaway CK, Marler PL, Chaves M. What the polls don’t show: A closer look at U.S. church attendance. American Sociological Review. 1993;58(6):741–752. [Google Scholar]
- 48.Presser S, Stinson L. Data collection mode and social desirability bias in self-reported religious attendance. American Sociological Review. 1998;63(1):137–145. [Google Scholar]
- 49.Chaves M. American Religion: Contemporary Trends. Princeton, N.J: Princeton University Press; 2011. [Google Scholar]
- 50.Rothman KJ. Modern Epidemiology. 3rd Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 51.Musick MA, House JS, Williams DR. Attendance at religious services and mortality in a national sample. Journal of Health and Social Behavior. 2004;45(2):198–213. doi: 10.1177/002214650404500206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


