Abstract
Chronic orchialgia is a vexing condition defined as chronic or intermittent scrotal pain lasting at least three months that significantly interferes with daily activities. There are currently no guidelines regarding the diagnosis and management of this condition despite it being the cause of 2.5–4.8% of urologic clinic visits. Men often present with chronic orchialgia in their mid to late 30s, although the condition can present at any age. A broad differential diagnosis of chronic orchialgia includes epididymitis, testicular torsion, tumors, obstruction, varicocele, epididymal cysts, hydrocele, iatrogenic injury following vasectomy or hernia repair, and referred pain from a variety of sources including mid-ureteral stone, indirect inguinal hernia, aortic or common iliac artery aneurysms, lower back disorders, interstitial cystitis, and nerve entrapment due to perineural fibrosis; approximately 25–50% of chronic orchialgia is idiopathic in nature. In such cases, it is reasonable to consider psychological and psychosocial factors that may be contributing to chronic pain. Invasive testing is not recommended in the work-up of chronic orchialgia.
Keywords: Chronic orchialgia, testicular pain, scrotal pain
Introduction and epidemiology of chronic orchialgia
Chronic orchialgia is one of the most vexing urologic complaints due to the relative dearth of information regarding proper evaluation and management of many of its causes. Currently, the American Urological Association (AUA) and European Urological Association (EAU) provide no formal guidelines for the diagnosis, evaluation, and management of chronic orchialgia.
Chronic pelvic pain syndromes more generally have been better characterized and studied in women than in men (1). Chronic pelvic pain affects approximately 15% of women 18–50 years old (2). In contrast, a recent study of 900 Swedish men estimated that chronic pelvic pain only affects 3–5% of men 40–69 years old (3). The differential diagnosis of chronic pelvic pain includes scrotal and testicular pain. Zermann observed that 38.8% of cases of chronic pelvic pain in men localize to the scrotum (4). A Swedish study that surveyed how urologists treat chronic scrotal pain estimated that 2.5% of visits are for chronic scrotal pain, given that urologists on average self-reported 6.5 new patient visits with a primary diagnosis of chronic scrotal pain monthly (5). A more recent study observed chronic scrotal pain in 4.8% (113/2,375) of men who presented to an outpatient urologist (6). Yet, before management and treatment can be pursued to help men suffering from this condition, a thorough understanding of its etiologies, evaluation and management are needed. In this review, we present a contemporary understanding of the epidemiology, diagnosis, and evaluation of chronic orchialgia.
Etiologies of chronic orchialgia
Chronic orchialgia is defined as chronic or intermittent scrotal pain lasting at least three months that significantly interferes with the patient’s daily activities (7). Of note, more recent definitions state that chronic ochialgia encompasses not just pain localized to the testicle, but also pain localizing to the epididymis, paratesticular structures, and spermatic cord (8). A broad differential diagnosis for chronic orchialgia includes both chronic and unresolved acute etiologies of testicular pain including epididymitis, testicular torsion, tumors, obstruction, varicocele, epididymal cysts, hydrocele, iatrogenic injury following vasectomy or hernia repair, and referred pain from a variety of sources such as a mid-ureteral stone, indirect inguinal hernia, aortic or common iliac artery aneurysms, lower back disorders, interstitial cystitis and nerve entrapment due to perineural fibrosis (8) (Table 1). Psychological factors contributing to genital pain should also be considered as a possible etiology for chronic orchialgia (32). Schover observed that in 48 men with no defined organic etiology for their scrotal pain, many had psychological symptoms including somatization disorder (56%), non-genital chronic pain syndromes (50%), major depression (27%), and chemical dependency (27%). These men also reported low levels of social support mechanisms, with 33% feeling isolated and only 50% having a spouse (33).
Table 1. Differential diagnosis of scrotal pain.
| Etiology | Epidemiology | History | Physical exam | Labs/imaging |
|---|---|---|---|---|
| Acute | ||||
| Epididymitis (9) | 600,000 cases in United States with bimodal distribution in men 16–30 and 51–70 years old with highest incidence | Gradual onset of unilateral pain with symptoms of urinary tract infection and history of sexual activity | Swelling of epididymis with exquisite tenderness; normal cremasteric reflex and pain relief with scrotal elevation | urinalysis and urethral culture along with Doppler U/S showing increased blood flow |
| Testicular torsion (10,11) | Bimodal peak in adolescence and in neonatale period | Acute onset of unilateral testicular pain | High riding testis with abnormal cremasteric reflex; pain with testis elevation | Doppler U/S showing decreased blood flow |
| Chronic | ||||
| Testicular mass (12) | Most common in young males average age 32 years old | Range from painless to dull ache, acute pain possible but uncommon | Mass palpated on exam | U/S to determine intra vs. extra-testicular mass |
| Varicocele (13) | 2-10% prevalence in the general population of adult men | Dull aching, throbbing pain worsened by standing, straining, or increased activity | “Bag of worms” on palpation | Color Doppler showing spermatic vein diameter >3.0–3.5 mm in diameter with demonstration of retrograde flow with Valsalva |
| Spermatocele (14,15) | Increased frequency observed in sons of mothers who used DES and in patients with VHL | Usually asymptomatic | Smooth, round and usually small transilluminating mass on the epididymis | U/S can be helpful if not clear on physical exam |
| Hydrocele (14,15) | 1–2% of neonates | Swelling of scrotal sac often bilateral, usually non painful although pain may occur with distention | Transilluminating mass | U/S helpful is testes not palpable |
| Post-vasectomy pain (16,17) | 6% of men seek medical advice within 3–4 years post vasectomy for chronic testicular pain | Scrotal discomfort, history of vasectomy | Tender full epididymitis and tender vasectomy sites with palpable nodule | None |
| Post-hernia repair pain (18,19) | roughly equal amount of patients (~15%) with testicular pain at 5-year follow-up regardless of surgical approach | Burning or stabbing pain with changes in sensation, worsened by activity | Normal genital exam | None |
| Interstitial cystitis (20) | Self-report studies estimate 60 cases per 100,000 men; Medical billing data describe 41 cases per 100,000 men |
Suprapubic pain, pain may include lower back | Variable tenderness of the abdominal wall, hip girdle, pelvic floor, bladder base, and urethra | Urinalysis, urine culture, and post void residual volume |
| Pelvic floor dysfunction (21-23) | 4.4% of men with urinary symptoms of dysfunction and up to 6.8% with defecation symptoms | Complaints of micturition, defecation, sexual function, and pelvic floor pain | Tenderness of pelvic floor in rectal exam | urine analysis and urine culture |
| Pain referred from | ||||
| Mid-ureteral stone (24,25) | Unusual presentation presented in case reports | Colicky unilateral pain | Normal genital exam | Urinalysis to assess for blood, abdominal X-ray |
| Indirect inguinal hernia (19,26,27) | Unusual presentation presented in case reports | Severe unilateral pain | Hernia noted on exam | Ultrasound to assess for decreased blood flow to testicle |
| Aortic or common iliac artery aneurysms (28,29) | Unusual presentation presented in case reports | Abdominal crampy pain radiating to testicle; may be constant or intermittent | Normal genital exam | CT or U/S to reveal aneurysm |
| Lower back disorders (30,31) | Unusual presentation presented in case reports | Unilateral scrotal pain worsened with coughing and leaning forward | Normal genital exam, straight leg raise aggravates pain, normal neuro exam | MRI spine |
Despite the numerous possible causes of chronic orchialgia, 25–50% of chronic orchialgia is currently considered idiopathic (7). It has been hypothesized that neurogenic inflammation elicited by activation of unmyelinated sensory neurons through noxious stimuli resulting in release of neuropeptides such as substance P and calcitonin gene related peptide (CGRP) are related to the pain. Specifically, this inflammation may be mediated by changes in alpha-2 receptors, given that such receptors with a lower response to alpha-2 antagonists have been identified in men with chronic scrotal pain (34). Most men with chronic orchialgia are in their mid to late 30s, although the condition can occur from adolescence to old age (7,35,36). Conditions associated with chronic orchialgia include infertility (9.7%), varicocele (8.8%), mid and distal ureteral stones (7.1%), chronic prostatitis (5.3%), lumber pain (4.4%), stress (4.4%), epididymal cysts (4.4%), irritable bowel (4.4%), infection (3.5%), previous operation (2.7%), driving (2.7%), hernia (2.7%), and hydrocele (1.8%) according to a study of 2,375 men meeting criteria for chronic scrotal pain (6).
Diagnosis and evaluation
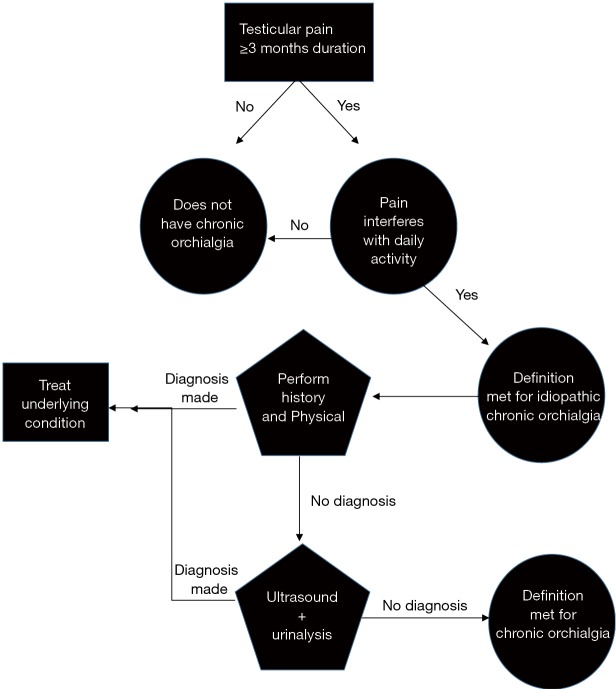
Diagnosis and evaluation of chronic orchialgia should be directed towards the differential diagnosis of acute testicular pain, with chronic orchialgia considered a diagnosis of exclusion (16). The initial workup consists of a thorough history and physical exam to rule out other possible causes of testicular pain of prolonged duration (Figure 1). The physician should consider intermittent torsion, infection, masses, varicocele, other comorbidities and past surgical history in establishing a definitive cause for the patient’s chronic pain.
Figure 1.
Diagnosis and work-up algorithm.
The patient history should also elicit details of the pain including acuity of onset, severity, location, quality, timing, and radiation to other locations. Aggravating and alleviating factors should be discussed as well, with emphasis on urinary habits, bowel movements, and sexual and physical activities (8,16). For example, acuity of pain onset may help differentiate between acute pathology such as testicular torsion or infection and more chronic pathology such as testicular mass or painful varicocele. Asking about other locations where pain may be present and radiation of the pain can also be useful, given that lower back disorders, mid-ureteral stones, aortic aneurysms, and indirect inguinal hernias can all contribute to scrotal pain. In men with interstitial cystitis, location of pain is of importance as suprapubic pain is usually present. Also, relief of pain with voiding and discomfort with bladder filling would be characteristic and the history should elucidate this relationship (20).
Recent studies suggest that referred pelvic floor pain that may be due to a painful condition or pelvic floor weakness may play a role in chronic orchialgia. In 2010, 41 men with chronic testicular pain were evaluated by Planken et al. for pelvic floor dysfunction. The authors found 93% of the 41 men had at least 1 symptom of pelvic floor dysfunction. In subsequent pelvic floor testing using electromyography registration, 88% of patients had increased resting pelvic floor muscle tone with mean of 6.7 mV (normal <3.0 mV) (21). Men with a normal resting pelvic floor tone were significantly older than those with an increased resting tone (65.6 vs. 45.6 years, P=0.0001) which supported the possibility of pelvic floor dysfunction in younger men with chronic orchialgia (21). A 2016 study by Farrell et al. further supported these findings by showing that men with chronic scrotal pain who also had pelvic floor pain and/or tightness on digital rectal examination could have improvement in scrotal pain with physical therapy of the pelvic floor muscles. Thirty patients were followed for a median of 13 months (range, 3-48 months). Median pre-physical therapy pain score was 6/10. After a mean of 12 [interquartile range (IQR), 6–16] sessions, the median decrease in pain score was 4.5/10. Further, fewer men required analgesic medication after physical therapy (44.0% vs. 73.3%, P=0.03) (22).
Chronic orchialgia can therefore be classified as part of the spectrum of chronic pelvic pain syndromes in men, and specific questions about sexual health and abuse are important given that men with chronic pelvic pain have an increased risk [odds ratio (OR) of 1.7–3.3] of having experienced psychological, physical, and sexual abuse (37). A thorough sexual history and history of abuse may also help identify risk factors for epididymitis in addition to psychological factors that may play into chronic pain. If a psychological component to the pain is suspected the history should include assessment of psychiatric history, substance use and/or abuse, and support structures, as men with idiopathic chronic scrotal pain often have numerous psychological risk factors that may contribute to a psychological etiology (33).
A thorough physical examination of the genitalia, with emphasis on the scrotal contents including the epididymides and vasa deferentia, and a rectal exam should be performed with the goal of ruling out all potential sources of pain (8).
Laboratory examinations include urinalysis and possibly semen culture if an infectious etiology is suspected (8). A duplex Doppler scrotal ultrasound should be performed to rule out structural abnormalities (8,38). Costabile examined 48 patients with chronic orchialgia and found ultrasound to be the only diagnostic test with a significant rate of abnormal findings, with 22 normal ultrasounds and 8 of 30 patients having incidental abnormal findings, defined as an anatomical or congenital abnormality that should be observed rather than treated. Other evaluation modalities including computed tomography (CT) scan, cystoscopy, urinalysis and culture, urodynamics, and excretory urography, which were normal in more than 91% of cases for each of these modalities (35). Compared to ultrasound, physical exam remains useful in patients with chronic pain without associated swelling. A study by Lau et al. examining the utility of physical exam to identify scrotal pathology in comparison with ultrasound in patients with chronic scrotal pain and without scrotal swelling yielded a sensitivity of 71.4% for physical exam in identifying pathology (39). Specificity of physical exam was 90.9%, with a positive predictive value of 76.9%, and a negative predictive value of 88.2% (39). These data show that while an ultrasound is highly useful in the setting of chronic orchialgia, its utility is rivaled by a good physical exam in patients with chronic testicular pain without obvious scrotal swelling. Therefore, idiopathic chronic orchialgia should be high on the differential diagnosis in a patient with a history that is negative for other possible causes of orchialgia and a benign physical exam.
Invasive testing and other imaging modalities including CT scan, intravenous pyelogram (IVP), retrograde pyelography, voiding cystourethrogram (VCUG) and cystoscopy are not helpful in working up chronic orchialgia and are not currently recommended as a part of the work-up (8,38). When initial work-up for chronic orchialgia results in no organic etiology a reasonable next step is spermatic cord nerve block with bupivacaine. Successful pain relief with spermatic cord blockade is helpful in both diagnosis of chronic orchialgia and in determining whether microsurgical spermatic cord denervation will be effective as a treatment (8,40-42).
Conclusions
Chronic orchialgia is a condition with a multitude of potential etiologies that include genitourinary and non-genitourinary conditions. Despite having a broad differential diagnosis, chronic orchialgia is classified as idiopathic in 25–50% of cases. In the absence of clear guidelines for the workup and treatment of chronic orchialgia, relying on a thorough history and physical exam to rule out all possible causes of chronic orchialgia is essential. The use of adjunct imaging modalities, in particular scrotal ultrasonography, can also facilitate a definitive diagnosis in the setting of an equivocal physical exam. Further invasive testing in the form of CT scan, IVP, retrograde pyelography, and VCUG is not recommended in the work-up of chronic orchialgia.
Acknowledgements
Funding: AW Pastuszak is a K12 scholar supported by a Male Reproductive Health Research (MRHR) Career Development Physician-Scientist Award (Grant # HD073917-01) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Program.
Footnotes
Conflicts of Interest: Dr. Pastuszak reports the following potential conflicts: Endo Pharmaceuticals—speaker and advisor and Boston Scientific/AMS—research support. The other author has no conflicts of interest to declare.
References
- 1.Hakenberg OW, Wirth MP. Chronic pelvic pain in men. Urol Int 2002;68:138-43. 10.1159/000048438 [DOI] [PubMed] [Google Scholar]
- 2.Mathias SD, Kuppermann M, Liberman RF, et al. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet Gynecol 1996;87:321-7. 10.1016/0029-7844(95)00458-0 [DOI] [PubMed] [Google Scholar]
- 3.Hedelin H, Johannisson H, Welin L. Prevalence of the chronic prostatitis/chronic pelvic pain syndrome among 40-69-year-old men residing in a temperate climate. Scand J Urol 2013;47:390-2. 10.3109/00365599.2012.756930 [DOI] [PubMed] [Google Scholar]
- 4.Zermann DH, Ishigooka M, Doggweiler R, et al. Neurourological insights into the etiology of genitourinary pain in men. J Urol 1999;161:903-8. 10.1016/S0022-5347(01)61802-0 [DOI] [PubMed] [Google Scholar]
- 5.Strebel RT, Leippold T, Luginbuehl T, et al. Chronic scrotal pain syndrome: management among urologists in Switzerland. Eur Urol 2005;47:812-6. 10.1016/j.eururo.2005.01.003 [DOI] [PubMed] [Google Scholar]
- 6.Ciftci H, Savas M, Yeni E, et al. Chronic orchialgia and associated diseases. Curr Urol 2010;4:67-70. 10.1159/000253415 [DOI] [Google Scholar]
- 7.Davis BE, Noble MJ, Weigel JW, et al. Analysis and management of chronic testicular pain. J Urol 1990;143:936-9. [DOI] [PubMed] [Google Scholar]
- 8.Levine L. Chronic orchialgia: evaluation and discussion of treatment options. Ther Adv Urol 2010;2:209-14. 10.1177/1756287210390409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician 2009;79:583-7. [PubMed] [Google Scholar]
- 10.Pentyala S, Lee J, Yalamanchili P, et al. Testicular torsion: a review. J Low Genit Tract Dis 2001;5:38-47. [DOI] [PubMed] [Google Scholar]
- 11.Ta A, D'Arcy FT, Hoag N, et al. Testicular torsion and the acute scrotum: current emergency management. Eur J Emerg Med 2016;23:160-5. 10.1097/MEJ.0000000000000303 [DOI] [PubMed] [Google Scholar]
- 12.Junnila J, Lassen P. Testicular masses. Am Fam Physician 1998;57:685-92. [PubMed] [Google Scholar]
- 13.Shridharani A, Lockwood G, Sandlow J. Varicocelectomy in the treatment of testicular pain: a review. Curr Opin Urol 2012;22:499-506. 10.1097/MOU.0b013e328358f69f [DOI] [PubMed] [Google Scholar]
- 14.Hagerty JA, Yerkes EB. Pediatric scrotal masses. Clin Pediatr Emerg Med 2009;10:50-5. 10.1016/j.cpem.2009.01.008 [DOI] [Google Scholar]
- 15.Eyre RC, O'Leary MP, Eamranond P. Evaluation of nonacute scrotal pathology in adult men. Available online: http://www.uptodate.com/contents/evaluation-of-nonacute-scrotal-pathology-in-adult-men?selectedTitle=1
- 16.Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol 2015;56:3-11. 10.4111/kju.2015.56.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris C, Mishra K, Kirkman RJ. A study to assess the prevalence of chronic testicular pain in post-vasectomy men compared to non-vasectomised men. J Fam Plann Reprod Health Care 2002;28:142-4. 10.1783/147118902101196298 [DOI] [PubMed] [Google Scholar]
- 18.Grant AM, Scott N, O'Dwyer P. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. British journal of surgery 2004;91:1570-4. 10.1002/bjs.4799 [DOI] [PubMed] [Google Scholar]
- 19.Brooks DC, Obeid A, Hawn M. Classification, clinical features and diagnosis of inguinal and femoral hernias in adults. Available online: https://www.uptodate.com/contents/classification-clinical-features-and-diagnosis-of-inguinal-and-femoral-hernias-in-adults
- 20.Clemens JQ. Pathogenesis, clinical features, and diagnosis of interstitial cystitis/bladder pain syndrome. Available online: http://www.uptodate.com/contents/pathogenesis-clinical-features-and-diagnosis-of-interstitial-cystitis-bladder-pain-syndrome
- 21.Planken E, Voorham-van der Zalm PJ, Lycklama ANAA, et al. Chronic testicular pain as a symptom of pelvic floor dysfunction. J Urol 2010;183:177-81. 10.1016/j.juro.2009.08.147 [DOI] [PubMed] [Google Scholar]
- 22.Farrell MR, Dugan SA, Levine LA. Physical therapy for chronic scrotal content pain with associated pelvic floor pain on digital rectal exam. Can J Urol 2016;23:8546-50. [PubMed] [Google Scholar]
- 23.MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG: An International Journal of Obstetrics & Gynaecology 2000;107:1460-70. 10.1111/j.1471-0528.2000.tb11669.x [DOI] [PubMed] [Google Scholar]
- 24.Holland JM, Feldman JL, Gilbert HC. Phantom orchalgia. J Urol 1994;152:2291-3. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg SD, Witchell SJ. Right testicular pain: unusual presentation of obstruction of the ureteropelvic junction. Can J Surg 1988;31:246-7. [PubMed] [Google Scholar]
- 26.Yeates WK. Pain in the scrotum. Br J Hosp Med 1985;33:101-4. [PubMed] [Google Scholar]
- 27.Desai Y, Tollefson B, Mills L, et al. Testicle ischemia resulting from an inguinal hernia. J Emerg Med 2012;43:e299-301. 10.1016/j.jemermed.2010.06.010 [DOI] [PubMed] [Google Scholar]
- 28.Ali MS. Testicular pain in a patient with aneurysm of the common iliac artery. Br J Urol 1983;55:447-8. [PubMed] [Google Scholar]
- 29.McGee SR. Referred scrotal pain: case reports and review. J Gen Intern Med 1993;8:694-701. 10.1007/BF02598293 [DOI] [PubMed] [Google Scholar]
- 30.White SH, Leslie IJ. Pain in scrotum due to intervertebral disc protrusion. Lancet 1986;1:504. 10.1016/S0140-6736(86)92963-6 [DOI] [PubMed] [Google Scholar]
- 31.Wouda EJ, Leenstra S, Vanneste JA. Scrotal pain as the presenting symptom of lumbar disc herniation: a report of 2 cases. Spine (Phila Pa 1976) 2005;30:E47-9. 10.1097/01.brs.0000150633.36777.c8 [DOI] [PubMed] [Google Scholar]
- 32.Hong MK, Corcoran NM, Adams SJ. Understanding chronic testicular pain: a psychiatric perspective. ANZ J Surg 2009;79:676-7. 10.1111/j.1445-2197.2009.05049.x [DOI] [PubMed] [Google Scholar]
- 33.Schover LR. Psychological factors in men with genital pain. Cleve Clin J Med 1990;57:697-700. 10.3949/ccjm.57.8.697 [DOI] [PubMed] [Google Scholar]
- 34.Singh V, Sinha RJ. Idiopathic chronic orchialgia - a frustrating issue for the clinician and the patient. Indian J Surg 2008;70:107-10. 10.1007/s12262-008-0032-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Costabile RA, Hahn M, McLeod DG. Chronic orchialgia in the pain prone patient: the clinical perspective. J Urol 1991;146:1571-4. [DOI] [PubMed] [Google Scholar]
- 36.Wesselmann U, Burnett AL, Heinberg LJ. The urogenital and rectal pain syndromes. Pain 1997;73:269-94. 10.1016/S0304-3959(97)00076-6 [DOI] [PubMed] [Google Scholar]
- 37.Hu JC, Link CL, McNaughton-Collins M, et al. The association of abuse and symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome: results from the Boston Area Community Health survey. J Gen Intern Med 2007;22:1532-7. 10.1007/s11606-007-0341-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Granitsiotis P, Kirk D. Chronic testicular pain: an overview. Eur Urol 2004;45:430-6. 10.1016/j.eururo.2003.11.004 [DOI] [PubMed] [Google Scholar]
- 39.Lau MW, Taylor PM, Payne SR. The indications for scrotal ultrasound. Br J Radiol 1999;72:833-7. 10.1259/bjr.72.861.10645188 [DOI] [PubMed] [Google Scholar]
- 40.Benson JS, Abern MR, Larsen S, et al. Does a positive response to spermatic cord block predict response to microdenervation of the spermatic cord for chronic scrotal content pain? J Sex Med 2013;10:876-82. 10.1111/j.1743-6109.2012.02937.x [DOI] [PubMed] [Google Scholar]
- 41.Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol 1996;155:1005-7. 10.1016/S0022-5347(01)66369-9 [DOI] [PubMed] [Google Scholar]
- 42.Heidenreich A, Olbert P, Engelmann UH. Management of chronic testalgia by microsurgical testicular denervation. Eur Urol 2002;41:392-7. 10.1016/S0302-2838(02)00023-4 [DOI] [PubMed] [Google Scholar]