Abstract
Vasectomy is the most effective form of sterilization for men. With approximately 500,000 vasectomies performed each year in the United States, 1–2% of these patients will experience chronic testicular pain for greater than three months after the procedure. Post-vasectomy pain syndrome (PVPS) is diagnosis of exclusion, and may be caused by direct damage to spermatic cord structures, compression of nerves in the spermatic cord via inflammation, back pressure from epididymal congestion, and perineural fibrosis. Treatment should begin with the most noninvasive options and progress towards surgical management if symptoms persist. Noninvasive therapies include acupuncture, pelvic floor therapy and pharmacologic options. Ultimately, management of PVPS requires a multimodal approach. Thorough understanding of the potential etiologies of PVPS along with the therapeutic options currently available is important to improve quality of life.
Keywords: Post-vasectomy pain, post-vasectomy pain syndrome (PVPS), orchalgia, testicular pain, epididymectomy, microdenervation of spermatic cord, vasectomy reversal, vasovasostomy
Background
Approximately 500,000 vasectomies are performed each year in the United States (1). With a success rate of 98%, vasectomy serves as the most effective form of sterilization for men. In an outpatient setting under local anesthesia, the vas deferens are severed, thereby preventing sperm from entering the ejaculate (2). Some of the techniques used additionally to prevent re-canalization include, excision of a segment of the vas deferens, fulgurating both ends with electrocautery, fascial interposition, suturing or clipping both stumps (3).
Following vasectomy, a small fraction of patients experience chronic pain. Post-vasectomy pain syndrome (PVPS) is widely known as either constant or intermittent testicular pain for greater than three months (4). This pain interferes with quality of life and requires some degree of medical treatment in approximately 1–2% of men who undergo vasectomy (5). However, the incidence of PVPS is difficult to estimate due to the lack of prospective studies. One prospective study cites up to 15% of men suffering from PVPS after vasectomy, although the estimate appears much higher than any of the other series (6). As a complication following one of the most common urologic procedures, understanding the etiology and diagnosis of PVPS as well as the potential treatment options is crucial.
Etiology
The pathophysiology of this condition is somewhat uncertain. The similar histologic findings in many PVPS patients, including thickened basement membranes, spermatid degeneration and testicular interstitial fibrosis, support a pathologic, not psychologic, etiology for this diagnosis (7).
Some of the proposed mechanisms thought to cause PVPS include direct damage to spermatic cord structures, compression of nerves in the spermatic cord via inflammation, back pressure from epididymal congestion, and perineural fibrosis (6). Unalleviated back pressure on the proximal stump of the vas deferens may cause sperm granulomas or epididymal blowout (8). There may also be an immunological component to the etiology of PVPS via the formation of antisperm antibodies. Following the disruption of the blood-testes barrier during vasectomy, 60–80% of men have detectable levels of serum antisperm antibodies. These antibodies have been shown to trigger organized immune responses in animal models (9). These potential mechanisms, either isolated or jointly, may ultimately lead to prolonged testicular or epididymal pain post-vasectomy.
Diagnosis
It is crucial to differentiate acute post-operative pain from PVPS. The most common symptom of PVPS is persistent orchalgia greater than three months after surgery, however, some patients present with pain with ejaculation, intercourse or erection. The differential diagnoses for these patients include neuropathic pain, infection, hydrocele, varicocele, inguinal hernia, intermittent testicular torsion, prostatitis, and psychogenic causes. Patients with PVPS often have a tender and/or full epididymis, tender proximal vas deferens, or palpable granuloma (10). With a detailed history and physical exam serially for several months following vasectomy, a diagnosis of PVPS can be safely made.
Ultimately, the diagnosis of PVPS is most safely made as a diagnosis of exclusion. A thorough history and physical is required at least three months after surgery. All patients with chronic testicular pain should undergo scrotal ultrasound with Doppler color-flow. Routine urinalysis, urine culture and semen culture should be obtained to rule out infection. In cases of concomitant neurological symptoms, MRI is recommended to rule out nerve impingement. To isolate the scrotum as the origin for pain, a spermatic cord block may be performed. This entails injecting 10 cc of 1% lidocaine without epinephrine into the cord at its location 1cm medial to the pubic tubercle and injecting 0.9% normal saline as a placebo injection. If pain subsides after injection of lidocaine up to 1–2 days, then cord block can serve as a diagnostic test in confirming that the pain is referred to the scrotum via nerves within the spermatic cord and predict response to spermatic cord denervation. Thus, a comprehensive evaluation is warranted to best establish a diagnosis in patients with chronic testicular pain.
Management and treatment
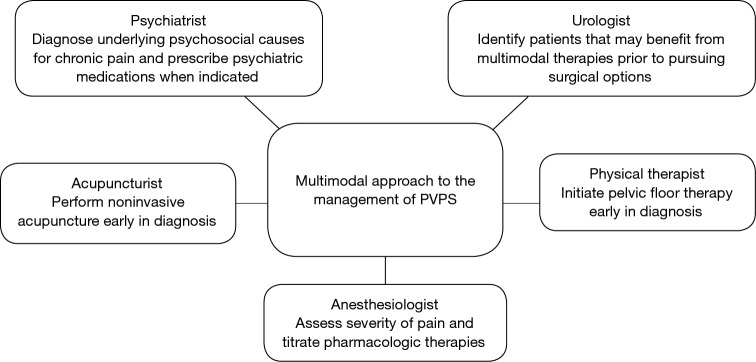
Management of PVPS can be frustrating for both the clinician and the patient. Treatment should begin with the most noninvasive options and progress towards surgical management if symptoms persist (Figure 1).
Figure 1.
Multimodal approach to the management of PVPS. PVPS, post-vasectomy pain syndrome.
Nonsurgical treatments include both pharmacotherapy and nonsurgical modalities to alleviate pain. Medical treatment usually begins with scheduled non-steroidal anti-inflammatory drugs (NSAIDs) for 4–6 weeks. If NSAIDs do not improve testicular pain, the second line medication recommended is a tricyclic antidepressant (TCA) or gabapentin. Some small retrospective studies have shown some improvement in patients with PVPS. TCAs have been proven to decrease neuropathic pain in other pathologies, including diabetic neuropathy and post herpetic neuralgia, by inhibiting the channels that link the neuronal synapses necessary in generating pain (11). Anticonvulsants such as gabapentin have been recommended for relief from PVPS. However, most studies exhibit success with anticonvulsants in patients with idiopathic testicular pain rather than pain from PVPS (12). Long-term use of narcotic pain medication is not recommended as a sustainable treatment option for patients with chronic PVPS.
Either exclusively or in combination with pharmacotherapy, pelvic floor therapy and/or acupuncture may be offered to patients with PVPS. Although there are no clinical trials proving the effectiveness of these modalities in PVPS, they are noninvasive and safe options to offer patients early in their diagnosis. Additionally, psychiatric evaluation may be warranted to rule out any mood disorder.
These nonsurgical treatment options are typically not long-lasting. Failed pharmacotherapy and noninvasive modalities should trigger surgical intervention. Surgical options include excision of sperm granuloma, microdenervation of spermatic cord, epididymectomy, vasovasostomy and in severe cases, orchiectomy. Of note, it is crucial to counsel patients that surgical interventions are not guaranteed to completely relieve pain and symptoms of the PVPS may continue or even worsen after surgery. This risk is particularly essential to document in all surgical informed consents (Table 1).
Table 1. Ideal patient selection for each surgical treatment option for PVPS.
| Surgical treatment option | Patient selection |
|---|---|
| Excision of sperm granuloma | Palpable sperm granuloma on physical exam |
| Microdenervation of the spermatic cord | Successful temporary relief with spermatic cord block |
| Epididymectomy | Pain localized to epididymis and not cord and/or testicle |
| Vasovasostomy | No concern for possibility for future fertility |
| Orchiectomy | Failed all other medical and surgical treatment options |
PVPS, post-vasectomy pain syndrome.
Microdenervation of the spermatic cord (MDSC) is the precise transection of all nerves within the spermatic cord. Care is taken to avoid all vasculature and lymphatic drainage. MDSC is useful in identifying intra-scrotal pathology as the etiology for scrotal pain. Patients who had effective temporary relief with spermatic cord block predicted a successful MDSC. One study specifically evaluated the use of MDSC in patients with PVPS. This study by Ahmed et al. performed MDSC on 17 patients with PVPS, and 76.5% of patients had complete resolution of pain at first follow-up visit (13). Several other studies have proven the effectiveness of MDSC in patients with various etiologies for chronic orchalgia (14,15).
Epididymectomy is most effective when pain is localized to the epididymis and not diffused around the entire cord or testicle. Several studies have been conducted to demonstrate the role of epididymectomy in treating PVPS. One study by Chung et al performed epididymectomy with simultaneous injection of hyaluronic acid and carboxymethyl cellulose to prevent fibrosis in PVPS patients, and this resulted in even better pain relief results (16).
Vasectomy reversal, or vasovasostomy, has been shown to significantly improve pain in patients with PVPS. This method directly alleviates the back pressure caused by obstruction at the proximal stump of the vas deferens. Many single-center studies demonstrate the high effectiveness of vasovasostomy, with up to 93% of patients reporting improvement of pain (17). The obvious downside of this treatment option is the return of initially unwanted fertility. Additionally, this option may not be covered by health insurance, thus making it cost prohibitive for patients with PVPS.
Orchiectomy serves as a last resort for relief of PVPS if all other surgical options have failed in resolving symptoms. Inguinal orchiectomy is preferred over scrotal orchiectomy due to higher likelihood of complete resolution of pain post-operatively (18). Although effective, the hormonal effects of this radical therapy make this an option only after exhausting all other medical and surgical options.
Conclusions
Vasectomy is one of the most common procedures for elective male sterilization in the United States. As the number of vasectomies performed climbs, PVPS is becoming more prevalent. Because the pathophysiology of PVPS can be difficult to pinpoint, the diagnosis and treatment of this disorder can become equally challenging. Patients with PVPS are significantly affected by their symptoms. As a diagnosis of exclusion, patients often go through a rigorous work up and are eager to start treatment once their diagnosis is established. PVPS treatments range from noninvasive therapies and pharmacologic treatments, to surgical interventions. Thorough understanding of the potential etiologies of PVPS along with the therapeutic options currently available is important to improve quality of life.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Barone MA, Hutchinson PL, Johnson CH, et al. Vasectomy in the United States, 2002. J Urol 2006;176:232-6. 10.1016/S0022-5347(06)00507-6 [DOI] [PubMed] [Google Scholar]
- 2.Jamieson DJ, Costello C, Trussell J, et al. US collaborative review of sterilization working group. The risk of pregnancy after vasectomy. Obstet Gynecol 2004;103:848-50. 10.1097/01.AOG.0000123246.11511.e4 [DOI] [PubMed] [Google Scholar]
- 3.Cook LA, Van Vliet HA, Lopez LM, et al. Vasectomy occlusion techniques for male sterilization. Cochrane Database Syst Rev 2014;(3):CD003991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan WP, Levine LA. An overview of the management of post-vasectomy pain syndrome. Asian J Androl 2016;18:332-7. 10.4103/1008-682X.175090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharlip ID, Belker AM, Honig S, et al. American urological association. Vasectomy: AUA guideline. J Urol 2012;188:2482-91. 10.1016/j.juro.2012.09.080 [DOI] [PubMed] [Google Scholar]
- 6.Leslie TA, Illing RO, Cranston DW, et al. The incidence of chronic scrotal pain after vasectomy: a prospective audit. BJU Int 2007;100:1330-3. 10.1111/j.1464-410X.2007.07128.x [DOI] [PubMed] [Google Scholar]
- 7.Whyte J, Sarrat R, Cisneros AI, et al. The vasectomized testis. Int Surg 2000;85:167-74. [PubMed] [Google Scholar]
- 8.Kathrins M. Techniques and complications of elective vasectomy: the role of spermatic granuloma in spontaneous recanalization. Fertil Steril 2016;106:68-9. 10.1016/j.fertnstert.2016.04.030 [DOI] [PubMed] [Google Scholar]
- 9.Linnet L, Hjort T. Sperm agglutinins in seminal plasma and serum after vasectomy: correlation between immunological and clinical findings. Clin Exp Immunol 1977;30:413-20. [PMC free article] [PubMed] [Google Scholar]
- 10.Nangia AK, Myles JL, Thomas AJ. Vasectomy reversal for the post-vasectomy pain syndrome: a clinical and histological evaluation. J Urol 2000;164:1939-42. 10.1016/S0022-5347(05)66923-6 [DOI] [PubMed] [Google Scholar]
- 11.Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 2010;85:S3-14. 10.4065/mcp.2009.0649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinclair AM, Miller B, Lee LK. Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. Int J Urol 2007;14:622-5. 10.1111/j.1442-2042.2007.01745.x [DOI] [PubMed] [Google Scholar]
- 13.Ahmed I, Rasheed S, White C, Shaikh NA. The incidence of post-vasectomy testicular pain and the role of nerve stripping (denervation) of the spermatic cord in its management. Br J Urol 1997;79:269-70. 10.1046/j.1464-410X.1997.32221.x [DOI] [PubMed] [Google Scholar]
- 14.Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol 2008;180:949-53. 10.1016/j.juro.2008.05.018 [DOI] [PubMed] [Google Scholar]
- 15.Levine LA, Matkov TG. Microsurgical denervation of the spermatic cord as primary surgical treatment of chronic orchalgia. J Urol 2001;165:1927-9. 10.1016/S0022-5347(05)66244-1 [DOI] [PubMed] [Google Scholar]
- 16.Chung JH, Moon HS, Choi HY, et al. Inhibition of adhesion and fibrosis improves the outcome of epididymectomy as a treatment for chronic epididymitis: a multicenter, randomized controlled, single-blind study. J Urol 2013;189:1730-4. 10.1016/j.juro.2012.11.168 [DOI] [PubMed] [Google Scholar]
- 17.Horovitz D, Tjong V, Domes T, et al. Vasectomy reversal provides long-term pain relief for men with the post-vasectomy pain syndrome. J Urol 2012;187:613-7. 10.1016/j.juro.2011.10.023 [DOI] [PubMed] [Google Scholar]
- 18.Davis BE, Noble MJ, Weigel JW, et al. Analysis and management of chronic testicular pain. J Urol 1990;143:936-9. [DOI] [PubMed] [Google Scholar]