Abstract
Background
The purpose of the present study was to analyse the impact of patient-related risk factors and medication drugs on haemorrhagic complications following cholecystectomy.
Methods
All cholecystectomies registered in the Swedish population-based Register for Gallstone Surgery and ERCP (GallRiks) were identified. Risk factors for bleeding were assessed by linking data in the GallRiks to the National Patient Register and the Prescribed Drug Register, respectively. The risk of haemorrhage leading to intervention was determined by variable regression, and Kaplan–Meier analysis assessed survival rate following perioperative haemorrhage.
Results
A total of 94,557 patients were included between 2005 and 2015, of which 799 (0.8%) and 1192 (1.3%) patients were registered as having perioperative and post-operative haemorrhage, respectively. In multivariable analysis, an increased risk of haemorrhagic complications was seen in patients with cerebrovascular disease (p = 0.001), previous myocardial infarction (p = 0.001), kidney disease (p = 0.001), heart failure (p = 0.001), diabetes (p = 0.001), peripheral vascular disease (p = 0.004), and obesity (p = 0.005). Prescription of tricyclic antidepressant (p = 0.018) or dipyridamole (p = 0.047) was associated with a significantly increased risk of perioperative haemorrhage. However, this increase in risk did not remain significant following Bonferroni correction for mass significance. Perioperative haemorrhage increased the risk of death occurring within the first post-operative year [Hazard Ratio, (HR) 4.9, CI 3.52–6.93] as well as bile duct injury (OR 2.45, CI 1.79–3.37).
Conclusion
The increased risk of haemorrhage associated with comorbidity must be taken into account when assessing patients prior to cholecystectomy. Perioperative bleeding increases post-operative mortality and is associated with an increased risk of bile duct injury.
Introduction
Laparoscopic cholecystectomy (LC) has since its introduction in the 1990s become the golden standard for the surgical treatment of symptomatic gallstone disease. In Sweden, about 13,000 cholecystectomies are performed each year of which 90% are performed with laparoscopic technique [1]. In LC, bile duct injuries and haemorrhage are the most feared complications. However, major haemorrhage is a rare event (0.08–0.25%) and is most often caused by injury to the right hepatic artery or inadvertent placement of a trocar in the aorta or vena cava [2–4]. More frequently occurring are minor bleeds arising from the abdominal wall and the liver bed following cholecystectomy (2.0–4.1%) [5, 6]. Haemorrhage from small vessels complicates the surgical procedure, increases the risk of conversion [7], and in some cases requires reoperation and/or blood transfusion [5].
Risk scoring systems based on comorbidity has been developed in order to predict bleeding risk. Furthermore, conditions such as renal and heart failure have been found to be associated with increased risk of haemorrhagic complications [8, 9]. In order to minimize the risk of procedure-related bleeding, drugs with anticoagulant or antiaggregant effects are usually discontinued. However, not often considered there are other drugs with side effects that might inadvertently affect platelet function and/or coagulation factors leading to impaired clotting ability [10, 11].
The influence of patient comorbidity and drugs on haemorrhagic complications in cholecystectomy is insufficiently known. We therefore undertook a population-based study to assess comorbidity as an independent risk factor for haemorrhagic complications. Furthermore, in the context of reducing haemorrhagic complications, a second part of the study aimed to investigate the need for the discontinuation of prescription drugs prior to cholecystectomy.
Methods
Study design
All laparoscopic and open cholecystectomy procedures registered between 2006 and 2015 in the Swedish Register for Gallstone Surgery and ERCP (GallRiks) [12] were included in the study. Every Swedish citizen has a unique National Registration Number (NRN) [13]. In order to assess the impact of prescribed drugs on risk of haemorrhage, the NRN was used as an aid in cross-matching the GallRiks with the Swedish Prescribed Drug Register (PDR; Swedish: Läkemedelsregistret) [14]. Only drugs prescribed to patients within 90 days prior to surgery were included in the analysis. The association of comorbidity with risk of bleeding was studied by comparing data from the GallRiks with the National Patient Register (NPR; Swedish: Patientregistret). Data in GallRiks were linked to the Swedish Death Register to obtain ICD codes indicating cause of death. Mortality was only considered to be procedure-related if a complication was registered on the death certificate as primary or contributing diagnosis.
Definitions
Data regarding perioperative haemorrhage were obtained from the GallRiks. Perioperative haemorrhage was defined as blood loss during the procedure that led to conversion to open surgery, blood transfusion, or other intervention not routinely applied in gallstone surgery. A post-operative haemorrhage was defined as bleeding within 30 days after cholecystectomy that necessitated reoperation, blood transfusion, or resulted in prolonged hospital stay (>1 day longer than the median stay). The post-operative incidence was based on those patients registered in the GallRiks and/or PAR as having had a post-operative haemorrhage. The occurrence of haemorrhage in the peri- and/or post-operative period within 30 days following cholecystectomy was given the term “total bleed”. Bile duct injury was defined as injury and/or clinically significant leakage detected in the peri- and/or post-operative period.
Data sources
The main purpose of the GallRiks is to assemble information, serve as a base for quality assurance, and facilitate research regarding gallstone surgery and ERCP. The register was started in 2005 and has today reached full national coverage (>90%). There are currently 79 hospitals/units in Sweden enrolled in the GallRiks. Repeated annual validation assures high-quality data with correctness in 97.2–98.2% of all registrations [15]. Data assembly in the GallRiks have previously been described in detail [16].
The population-based PDR has registered dispensed medication in Sweden since July 2005. All drugs prescribed are classified according to the Anatomical Therapeutic Chemical (ATC) classification system. Information on dose and date of dispensing of all prescribed drugs dispensed at Swedish pharmacies is registered in the PDR. However, the register contains no information regarding drugs administered during in-hospital treatment, over-the-counter (OTC) drugs (without prescription), or drugs administered in day care. In July–December 2005, the PDR registered 84% of the nation’s total consumption of drugs and 77% of the total expenditure [17].
The NPR was founded in 1964 and provides information and discharge diagnosis for all hospital admissions and outpatients in Sweden. With nationwide coverage, the NPR contains information on over 50 million patients since its inception. Diagnoses in the NPR are coded according the ICD system and currently over 99% of all discharges are covered [18]. The validity of the register has been tested by Ludwigsson et al. [19] showing a high accuracy (85–95%) for most diagnoses.
Statistical analysis
The Chi-square test was used to compare patient characteristics. Univariate analysis was undertaken in order to identify predictors of haemorrhage with estimates of odds ratio (OR) and 95 per cent confidence intervals. In order to restrict confounding to a minimum, all variables in the multivariate regression analyses of patient characteristics were adjusted for gender, age, ASA, surgical indication, operative approach, thromboembolism prophylaxis, operation time, and prescribed anticoagulant medication.
The impact of prescribed drugs on bleeding was assessed by univariate regression.
In this analysis, mass significance was managed by Bonferroni correction [20], where data were considered significant at the 95% level if the p value divided by the number of drugs in the analysis (n = 28) was less than p = 0.05/28 = 0.002. Kaplan–Meier analysis assessed the overall survival following a registered haemorrhagic complication. Hazard ratios (HRs) were estimated using the Cox regression model. Gender, age, indication, operative approach, and ASA classification were added as covariables in the calculation of adjusted HR. All statistical analyses were performed using SPSS, IBM® (version 23.0.0.0).
Results
Incidence
Altogether 94,557 patients registered in the GallRIks undergoing cholecystectomy (laparoscopic as well as open) 2005–2015 were included in the study. The total incidence of post-operative complications was 8.4% (7975 patients). Perioperative haemorrhage was registered in 799 (0.8%). The incidence of post-operative haemorrhage was 1.3% (1192 patients). There was 46.8% agreement in frequency of post-operative haemorrhage between the registers. The majority of post-operative complications registered in the GallRiks occurred within 30 days after surgery (n = 779, 97%). Bleeding was also registered between 30 and 60 days (n = 18, 2.25%) and between 60 and 90 days (n = 6, 0.75%). In total, 1867 patients were registered with a peri- and/or post-operative intervention due to haemorrhage, resulting in a total bleeding incidence of 2.0%. Haemorrhagic shock was registered in 10 patients (0.01%).
Risk factors
Risk factors for haemorrhage in univariate regression (Table 1) were: male gender; high age; ASA > I; gallstone complications; conversion to open surgery; open cholecystectomy; thromboembolism prophylaxis; and long operation time. A subgroup analysis was conducted on 36,797 patients for whom BMI was registered (missing = 57,760). There were 12,334 patients (33.5%) with BMI < 18.5 (underweight), 13,776 patients (37.4%) with BMI 18.5–24.9 (normal weight), 9702 (26.4%) patients with BMI 25–29.9 (overweight), and 985 patients (2.7%) with BMI > 30 (obesity). The odds ratio for BMI ≥ 25 and bleeding was 1.04, (CI 0.89–1.23, data not shown). However, in the multivariate analysis, obesity was a significant risk factor for bleeding (OR = 1.3, CI 1.10–1.56).
Table 1.
Patient characteristics as described by Chi-square test and risk of haemorrhage assessed by univariate regression
| M | N (%) | Periop bleed (%) | OR CI | Postop bleed (%) | OR CI | Total bleed1 (%) | OR CI | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1 | ||||||||||
| Female | 63,488 (67.1) | 408 (0.62) | 1 | Ref | 697 (1.10) | 1 | Ref | 1036 (1.63) | 1 | Ref | |
| Male | 31,068 (32.9) | 391 (1.31) | 2.15 | 1.87–2.47 | 495 (1.59) | 1.46 | 1.30–1.64 | 831 (2.67) | 1.66 | 1.51–1.82 | |
| Age | 1 | ||||||||||
| ≤40 | 28,457 (30.1) | 117 (0.41) | 1 | Ref | 273 (0.96) | 1 | Ref | 378 (1.33) | 1 | Ref | |
| 41–60 | 37,252 (39.4) | 243 (0.65) | 1.59 | 1.28–1.98 | 383 (1.03) | 1.07 | 0.92–1.25 | 590 (1.58) | 1.20 | 1.05–1.36 | |
| >60 | 28,847 (30.5) | 439 (1.52) | 3.74 | 3.05–4.59 | 536 (1.86) | 1.95 | 1.69–2.26 | 899 (3.12) | 2.39 | 2.12–2.70 | |
| ASA | 0 | ||||||||||
| I | 49,172 (52.0) | 258 (0.52) | 1 | Ref | 434 (0.88) | 1 | Ref | 660 (1.34) | 1 | Ref | |
| II | 38,094 (40.3) | 390 (1.02) | 1.59 | 1.28–1.98 | 534 (1.40) | 1.07 | 0.92–1.25 | 871 (2.29) | 1.20 | 1.05–1.36 | |
| ≥III | 7291 (7.71) | 151 (2.07) | 3.74 | 3.05–4.59 | 224 (3.07) | 1.95 | 1.69–2.26 | 336 (4.61) | 2.39 | 2.12–2.70 | |
| Indication | 0 | ||||||||||
| Gallstone colic | 54,681 (57.8) | 312 (0.57) | 1 | Ref | 518 (0.95) | 1 | Ref | 791 (1.45) | 1 | Ref | |
| Gallstone complications2 | 36,659 (38.8) | 454 (1.24) | 2.19 | 1.89–2.53 | 606 (1.65) | 1.76 | 1.56–1.98 | 986 (2.69) | 1.88 | 1.71–2.07 | |
| Acalculous cholecystitis |
648 (0.70) | 4 (0.62) | 1.08 | 0.40–2.91 | 25 (3.90) | 4.20 | 2.79–6.32 | 28 (4.32) | 3.08 | 2.09–4.52 | |
| Other | 2569 (2.70) | 29 (1.13) | 1.99 | 1.36–2.92 | 43 (1.67) | 1.78 | 1.30–2.44 | 62 (2.41) | 1.69 | 1.30–2.19 | |
| Op approach | 2293 | ||||||||||
| Lap | 78,814 (85.4) | 356 (0.45) | 1 | Ref | 746 (0.95) | 1 | Ref | 1066 (1.35) | 1 | Ref | |
| Converted to open surgery | 6593 (7.20) | 272 (4.13) | 9.48 | 8.08–11.13 | 214 (3.25) | 3.51 | 3.01–4.10 | 433 (6.57) | 5.13 | 4.57–5.75 | |
| Open | 6857 (7.40) | 155 (2.26) | 5.10 | 4.21–6.17 | 187 (2.73) | 2.93 | 2.50–3.45 | 307 (4.48) | 3.42 | 3.00–3.89 | |
| Thromboembolism prophylaxis | 289 | ||||||||||
| No | 57,696 (61.2) | 273 (0.47) | 1 | Ref | 534 (0.93) | 1 | Ref | 758 (1.31) | 1 | Ref | |
| Yes | 36,572 (38.8) | 526 (1.44) | 3.07 | 2.65–3.56 | 643 (1.76) | 1.92 | 1.71–2.15 | 1094 (3.0) | 2.32 | 2.11–2.54 | |
| Op time | 290 | ||||||||||
| <120 | 71,552 (75.9) | 288 (0.40) | 1 | Ref | 750 (1.05) | 1 | Ref | 1001 (1.40) | 1 | Ref | |
| >120 | 22,715 (24.1) | 511 (2.25) | 5.62 | 4.86–6.50 | 428 (1.88) | 1.85 | 1.64–2.08 | 852 (3.75) | 2.76 | 2.51–3.02 | |
1Total bleed perioperative and/or post-operative haemorrhage and/or haemorrhagic shock)
2Cholecystitis and/or gallstone pancreatitis
M missing data, N number of patients, OR odds ratio, CI 95% confidence interval, Ref reference
In Table 2, 28 prescription drugs with known anticoagulant or antiplatelet effect were tested for association with bleeding. In the univariate analysis, dipyridamole (n = 252, OR = 2.39, CI 0.98–5.81) and tricyclic antidepressants (TCA, n = 1151. OR = 1.78, CI 1.10–2.89) had a significantly elevated risk of perioperative haemorrhage. This increase in risk, however, did not remain significant in a Bonferroni correction.
Table 2.
Prescribed drugs1 and haemorrhagic complications
| Drug | N (%) | Periop bleed (%) | p | Postop bleed | p | Total bleed2 (%) | p |
|---|---|---|---|---|---|---|---|
| Acetysalicylic acid | 7443 (8.75) | 61 (8.5) | 0.81 | 106 (9.68) | 0.27 | 159 (9.36) | 0.36 |
| ACE inhibitor | 6575 (7.73) | 53 (7.38) | 0.73 | 80 (7.31) | 0.60 | 126 (7.42) | 0.63 |
| Apixaban | 11 (0.01) | 0 (0) | n.s | 0 (0) | n.s | 0 (0) | n.s |
| Azathioprin | 179 (0.21) | 0 (0) | n.s | 0 (0) | n.s | 0 (0) | n.s |
| Acyclovir | 198 (0.23) | 2 (0.28) | 0.80 | 2 (0.18) | 0.22 | 4 (0.24) | 0.98 |
| Beta-lactam antibiotics | 4790 (5.63) | 51 (7.10) | 0.09 | 63 (5.75) | 0.86 | 101 (5.95) | 0.56 |
| Calcium channel inhibitor | 6146 (7.22) | 60 (8.40) | 0.24 | 76 (6.94) | 0.72 | 130 (7.66) | 0.49 |
| Carboxamide | 361 (0.42) | 1 (0.14) | 0.24 | 2 (0.18) | 0.22 | 3 (0.18) | 0.11 |
| Cephalosporin | 31 (0.04) | 0 (0) | n.s | 1 (0.10) | 0.34 | 1 (0.06) | 0.62 |
| Clopidogrel | 565 (0.66) | 7 (0.97) | 0.30 | 4 (0.37) | 0.22 | 11 (0.65) | 0.93 |
| Cytostatic agents | 238 (0.28) | 3 (0.42) | 0.48 | 6 (0.55) | 0.09 | 7 (0.41) | 0.30 |
| Dabigatran | 37 (0.04) | 1 (0.14) | 0.22 | 0 (0) | n.s | 1 (0.06) | 0.76 |
| Dipyridamole | 252 (0.30) | 5 (0.70) | 0.05* | 1 (0.10) | 0.21 | 6 (0.35) | 0.66 |
| Heparin | 838 (0.98) | 7 (0.97) | 0.98 | 11 (1.0) | 0.95 | 15 (0.88) | 0.67 |
| Kinin | 58 (0.07) | 0 (0) | n.s | 0 (0) | n.s | 0 (0) | n.s |
| NSAID | 7932 (9.32) | 73 (10.2) | 0.43 | 102 (9.32) | 1.0 | 163 (9.60) | 0.69 |
| Phenytoin | 77 (0.09) | 0 (0) | n.s | 2 (0.18) | 0.31 | 2 (0.12) | 0.71 |
| Prasugrel | 5 (0.01) | 0 (0) | n.s | 0 (0) | n.s | 0 (0) | n.s |
| Rifampicin | 16 (0.02) | 0 (0) | n.s | 1 (0.10) | 0.08 | 1 (0.06) | 0.22 |
| Rivaroxaban | 23 (0.03) | 0 (0) | n.s | 0 (0) | n.s | 0 (0) | n.s |
| SSRI | 5203 (6.11) | 45 (6.27) | 0.86 | 67 (6.12) | 0.99 | 106 (6.24) | 0.82 |
| Statin | 7377 (8.67) | 58 (8.10) | 0.57 | 108 (9.86) | 0.16 | 157 (9.25) | 0.39 |
| Thiazide | 2355 (2.77) | 25 (3.48) | 0.24 | 31 (2.83) | 0.90 | 55 (3.24) | 0.23 |
| Ticagrelor | 32 (0.04) | 0 (0) | n.s | 1 (0.10) | 0.36 | 1 (0.06) | 0.65 |
| Tricyclic antidepressant | 1151 (1.35) | 17 (2.37) | 0.02* | 18 (1.64) | 0.40 | 32 (1.88) | 0.055 |
| Trimethoprim/sulphamethoxazole | 255 (0.30) | 4 (0.56) | 0.21 | 4 (0.37) | 0.69 | 6 (0.35) | 0.68 |
| Valproate | 210 (0.25) | 2 (0.28) | 0.86 | 0 (0) | n.s | 2 (0.12) | 0.28 |
| Warfarin | 1818 (2.14) | 21 (2.92) | 0.14 | 27 (2.47) | 0.45 | 45 (2.70) | 0.14 |
Table 2: Pearson´s Chi-Square test
* Significant within 95% confidence interval
1Drugs prescribed within 90 days prior to surgery
2Total haemorrhage (peri- and/or post-operative) for each drug
Cerebrovascular disease (OR = 1.96; CI 1.64–2.34), previous myocardial infarction (OR = 1.94, CI 1.56–2.40), kidney disease (OR = 1.93; CI 1.41–2.63), heart failure (OR = 1.73, CI 1.37–2.18), diabetes (OR = 1.49, CI 1.27–1.74), peripheral vascular disease (OR = 1.49, CI 1.13–1.95), and obesity (OR = 1.27, CI 1.08–1.51) were all found to be associated with a significantly increased risk of haemorrhagic complications (Table 3).
Table 3.
Comorbidity and haemorrhagic complications1
| Condition | N (%) | Bleed (%) | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|
| p | OR | CI | p | OR | CI | |||
| Cerebrovascular disease | 3283 (3.48) | 151 (4.60) | 0.001 | 2.52 | 2.12–2.98 | 0.001 | 1.96 | 1.64–2.34 |
| Diabetes | 5396 (5.71) | 197 (3.65) | 0.001 | 1.99 | 1.71–2.31 | 0.001 | 1.49 | 1.27–1.74 |
| Heart failure | 1797 (1.90) | 103 (5.73) | 0.001 | 3.14 | 2.56–3.85 | 0.001 | 1.73 | 1.37–2.18 |
| Kidney disease | 788 (0.83) | 48 (6.10) | 0.001 | 3.28 | 2.44–4.41 | 0.001 | 1.93 | 1.41–2.63 |
| Liver cirrhosis | 345 (0.37) | 14 (4.10) | 0.005 | 2.11 | 1.23–3.61 | 0.053 | 1.71 | 0.99–2.94 |
| Lung disease | 8750 (9.27) | 181 (2.10) | 0.51 | 1.05 | 0.90–1.23 | 0.363 | 0.930 | 0.79–1.09 |
| Obesity | 6173 (6.54) | 157 (2.54) | 0.01 | 1.32 | 1.12–1.56 | 0.005 | 1.27 | 1.08–1.51 |
| Peripheral vascular disease | 1314 (1.40) | 64 (4.87) | 0.001 | 2.60 | 2.01–3.35 | 0.004 | 1.49 | 1.13–1.95 |
1Peri- and/or post-operative haemorrhagic complications
Bile duct injury
By including perioperative iatrogenic bile duct injury and/or post-operative bile leakage, the overall incidence of bile duct injury was 1.6%. For patients with perioperative haemorrhage, the incidence of bile duct injury was significantly higher (5.4%, p < 0.05). Adjusting for gender, age, indication, operative approach, and ASA classification, perioperative bleeding was found to be a risk factor for bile duct injury (OR = 2.45, CI 1.79–3.37).
Mortality
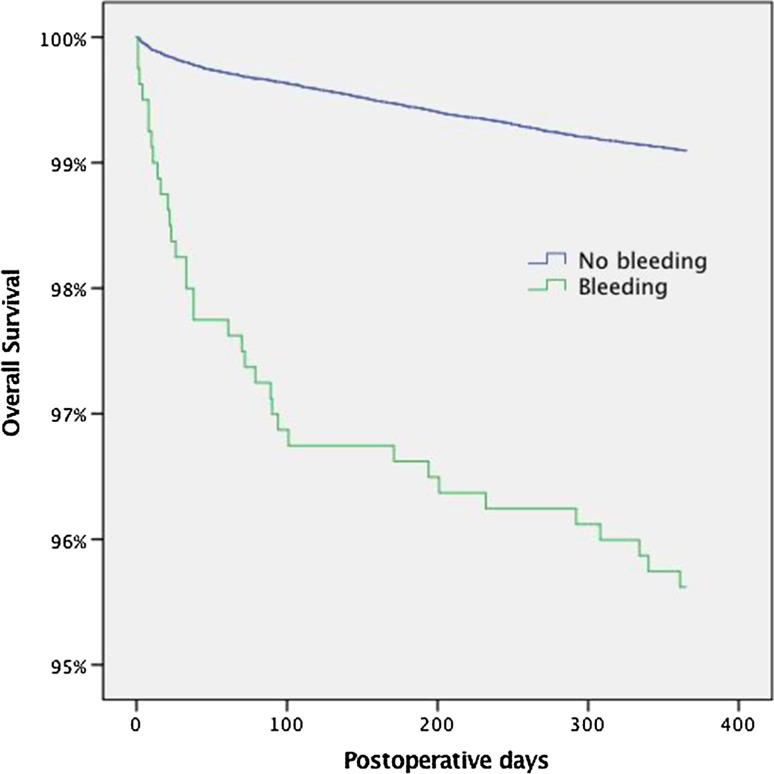
In total, 223 (0.24%) patients died within 30 days after cholecystectomy. The cause of death was procedure-related in 25 (0.03%). In patients with perioperative, post-operative, and total bleeding, 16 patients (2.0%), 25 patients (11.2%), and 34 patients (15.2%) died, respectively. Almost half of patients (48%) with a procedure-related cause of death had a haemorrhage registered prior to death. Patients that had a perioperative haemorrhage had a significantly increased mortality during the first post-operative year (Fig. 1). The increased hazard of death (HR) associated with perioperative bleeding was estimated to be 4.9 (CI 3.52–6.93) with an adjusted HR of 1.8 (CI 1.28–2.53). The increased mortality in patients with a perioperative haemorrhage remained when performing a subgroup analysis where death within thirty days was excluded (p < 0.05).
Fig. 1.
Kaplan-Meier plot of survival following peri-operative haemorrhage in cholecystectomy
Discussion
In this population-based study, cerebrovascular disease, previous myocardial infarction, kidney disease, heart failure, diabetes, peripheral vascular disease, and obesity were all found to be independent risk factors for haemorrhagic complications in cholecystectomy. Furthermore, patients with perioperative haemorrhage had a fivefold increase in hazard ratio for post-operative death. Perioperative bleeding significantly increased the risk of bile duct injury.
Strength and weakness
The strength that this study presents is the population-based design, with data retrieved from three validated Swedish quality registers. Other strengths are that haemorrhage was presented as perioperative, post-operative as well as total. Our definition of haemorrhage in this study was a bleed that mandated intervention. It could be argued, however, that a more stringent way of defining a haemorrhage would be a minimum volume of blood loss.
There are some potential weaknesses with the present study. Data on prescribed drugs did not provide information on if, or for how long the drug was discontinued prior to surgery. In this study, the assessment of potent anticoagulants such as Warfarin and new oral anticoagulants (NOACs) was difficult since it was unlikely to believe that these drugs would have been continued during surgery. Furthermore, the timing of surgery after interrupting the anticoagulant treatment may also affect the risk of bleeding. Since we do not have any data on this, we are not able to determine the optimal interval to perform surgery after anticoagulant cessation.
Another weakness was the lack of precision in comorbidity diagnoses. For instance, “kidney disease” is a group diagnosis made up from a number of kidney disorders. Furthermore, registers on surgical procedures that are based on self-reported adverse events are inevitably subject to selection bias since it is more likely that a positive outcome of surgery is reported. This effect is lessened by repeated validation. Surgical units enrolled in GallRiks are continuously visited by appointed inspectors, and during these validations, data from medical journals are scrutinized and compared with those entered in the register. Previous cross-check control of data has found less than 2% error [15].
Comparison with other studies
The overall incidence of haemorrhage during and within 30 days after cholecystectomy was 2.0%. Due to differences in criteria, the comparison of haemorrhage rates between different studies must be interpreted with caution. Shea et al. [21] reported in a meta-analysis a bleeding complication rate of 10.5% and Z´graggen reported a perioperative haemorrhage incidence of 1.97% [7]. In a study by Ercan et al., patients taking oral anticoagulants (OACs) were taken off their medication prior to cholecystectomy and given enoxaparin (low molecular heparin) bridging therapy and compared to a control group. In the OAC group, the post-operative bleeding rate was 25% compared to 1.5% in the control group [22].
In accordance with previous studies [7, 21, 23, 24], we found that the overall 30-day mortality following cholecystectomy is low (0.24%). However, haemorrhage leading to intervention increased mortality by over 60 times compared to patients without bleeding complications. Furthermore, half of all patients that died in the post-operative period from procedure-related causes were registered as having a haemorrhage prior to death. A Kaplan–Meier estimate also showed that survival of patients who had a perioperative haemorrhage continued to decline beyond the 30-day post-operative interval.
Serotonin plays an important role in the process of platelet aggregation and vasoconstriction during primary haemostasis [25]. Indeed, by reducing the re-uptake of serotonin, TCA inhibits platelet aggregation [26] and has been associated with an elevated bleeding risk [27, 28]. In our study, tricyclic antidepressants (TCA) significantly increased the risk of perioperative haemorrhage. However, the correlation did not tolerate a Bonferroni correction, indicating that the result could be an artefact of mass significance. Nevertheless, TCA may have a clinically relevant impact on the risk of haemorrhage that should be evaluated in future studies.
Following cholecystectomy, it has been shown that a significant number of patients with bile duct injuries have an associated vascular injury [29, 30]. These “vasculobiliary” injuries are often managed at tertiary care facilities [30]. Risk factors for biliary injury during cholecystectomy have previously been described in detail [31]. However, to the best of our knowledge, perioperative bleeding has not been defined as a significant risk factor for bile duct injury. As previously reported, bile duct injuries may occur as a consequence of a bleeding-impaired exposure and visualization during dissection in cholecystectomy [32].
It is reasonable to believe that a perioperative haemorrhage distorts anatomical landmarks, resulting in an increased risk of iatrogenic bile duct injury or misplacement of clips. In order to account for all possible injuries to the bile ducts, we chose a broader definition for bile duct injury including both iatrogenic injuries detected during the operation and/or bile leaks in the post-operative phase. This resulted in a higher incidence of bile duct injuries than previously reported [4, 7]. In the present study, perioperative bleeding was associated with an increased incidence of injury and/or bile leakage. Moreover, in a multivariable regression model, perioperative bleeding was a strong predictor of bile duct injury.
Conclusion
Patient comorbidity needs to be taken into account when assessing the risk of haemorrhage and peri-operative bleeding increases the risk of death following cholecystectomy. However, our results suggest that commonly prescribed medication does not need to be discontinued in order to reduce haemorrhagic complications. Finally, surgeons need to be aware of the increased risk of biliary duct injury following haemorrhage and should consider converting to open surgery if visualization and exposure is inadequate.
Acknowledgement
This study was made possible by a research grant from the Olle Engqvist Research Foundation.
References
- 1.http://www.ucr.uu.se/gallriks/fou/arsrapporter
- 2.Usal H, Sayad P, Hayek N, et al. Major vascular injuries during laparoscopic cholecystectomy. An institutional review of experience with 2589 procedures and literature review. Surg Endosc. 1998;12:960–962. doi: 10.1007/s004649900756. [DOI] [PubMed] [Google Scholar]
- 3.Mechchat A, Bagan P. Management of major vascular complications of laparoscopic surgery. J Visc Surg. 2010;147:e145–e153. doi: 10.1016/j.jviscsurg.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Deziel DJ, Millikan KW, Economou SG, et al. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/S0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 5.Persson G, Strömberg J, Svennblad B, et al. Risk of bleeding associated with use of systemic thromboembolic prophylaxis during laparoscopic cholecystectomy. Br J Surg. 2012;99:979–986. doi: 10.1002/bjs.8786. [DOI] [PubMed] [Google Scholar]
- 6.Schafer M, Lauper M, Krahenbuhl L. A nation’s experience of bleeding complications during laparoscopy. Am J Surg. 2000;180:73–77. doi: 10.1016/S0002-9610(00)00416-5. [DOI] [PubMed] [Google Scholar]
- 7.Z’Graggen K, Wehrli H, Metzger A, et al. Complications of laparoscopic cholecystectomy in Switzerland. A prospective 3-year study of 10,174 patients. Swiss Association of Laparoscopic and Thoracoscopic Surgery. Surg Endosc. 1998;12:1303–1310. doi: 10.1007/s004649900846. [DOI] [PubMed] [Google Scholar]
- 8.Decousus H, Tapson VF, Bergmann JF, et al. Factors at admission associated with bleeding risk in medical patients: findings from the IMPROVE investigators. Chest. 2011;139:69–79. doi: 10.1378/chest.09-3081. [DOI] [PubMed] [Google Scholar]
- 9.Kuijer PM, Hutten BA, Prins MH, et al. Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med. 1999;159:457–460. doi: 10.1001/archinte.159.5.457. [DOI] [PubMed] [Google Scholar]
- 10.Kenney B, Stack G. Drug-induced thrombocytopenia. Arch Pathol Lab Med. 2009;133:309–314. doi: 10.5858/133.2.309. [DOI] [PubMed] [Google Scholar]
- 11.Scharf RE. Drugs that affect platelet function. Semin Thromb Hemost. 2012;38:865–883. doi: 10.1055/s-0032-1328881. [DOI] [PubMed] [Google Scholar]
- 12.GallRiks—Swedish national register for gallstone surgery and ERCP. http://www.ucr.uu.se/gallriks
- 13.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, et al. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–667. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swedish Prescribed Drug Register (PDR). http://www.socialstyrelsen.se/register/halsodataregister/lakemedelsregistret
- 15.Rystedt J, Montgomery A, Persson G. Completeness and correctness of cholecystectomy data in a national register—GallRiks. Scand J Surg. 2014;103:237–244. doi: 10.1177/1457496914523412. [DOI] [PubMed] [Google Scholar]
- 16.Enochsson L, Thulin A, Osterberg J, et al. The Swedish Registry of Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks): a nationwide registry for quality assurance of gallstone surgery. JAMA Surg. 2013;148:471–478. doi: 10.1001/jamasurg.2013.1221. [DOI] [PubMed] [Google Scholar]
- 17.Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–735. doi: 10.1002/pds.1294. [DOI] [PubMed] [Google Scholar]
- 18.Swedish Patient Register. http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish
- 19.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haynes W. Bonferroni correction. In: Dubitzky W, Wolkenhauer O, Cho K-H, Yokota H, editors. Encyclopedia of systems biology. New York: Springer; 2013. p. 154. [Google Scholar]
- 21.Shea JA, Healey MJ, Berlin JA, et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996;224:609–620. doi: 10.1097/00000658-199611000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ercan M, Bostanci EB, Ozer I, et al. Postoperative hemorrhagic complications after elective laparoscopic cholecystectomy in patients receiving long-term anticoagulant therapy. Langenbecks Arch Surg. 2010;395:247–253. doi: 10.1007/s00423-009-0483-y. [DOI] [PubMed] [Google Scholar]
- 23.Rosenmuller M, Haapamaki MM, Nordin P, et al. Cholecystectomy in Sweden 2000-2003: a nationwide study on procedures, patient characteristics, and mortality. BMC Gastroenterol. 2007;7:35. doi: 10.1186/1471-230X-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McMahon AJ, Fischbacher CM, Frame SH, et al. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000;356:1632–1637. doi: 10.1016/S0140-6736(00)03156-1. [DOI] [PubMed] [Google Scholar]
- 25.Berger M, Gray JA, Roth BL. The expanded biology of serotonin. Annu Rev Med. 2009;60:355–366. doi: 10.1146/annurev.med.60.042307.110802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohammad SF, Mason RG. Inhibition of human platelet-collagen adhesion reaction by amitriptyline and imipramine. Proc Soc Exp Biol Med. 1974;145:1106–1113. doi: 10.3181/00379727-145-37962. [DOI] [PubMed] [Google Scholar]
- 27.Lee YC, Shau WY, Chang CH, et al. Antidepressant use and the risk of upper gastrointestinal bleeding in psychiatric patients: a nationwide cohort study in Taiwan. J Clin Psychopharmacol. 2012;32:518–524. doi: 10.1097/JCP.0b013e31825ccd5a. [DOI] [PubMed] [Google Scholar]
- 28.Lupattelli A, Spigset O, Koren G, et al. Risk of vaginal bleeding and postpartum hemorrhage after use of antidepressants in pregnancy: a study from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2014;34:143–148. doi: 10.1097/JCP.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 29.Buell JF, Cronin DC, Funaki B, et al. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–708. doi: 10.1001/archsurg.137.6.703. [DOI] [PubMed] [Google Scholar]
- 30.Keleman AM, Imagawa DK, Findeiss L, et al. Associated vascular injury in patients with bile duct injury during cholecystectomy. Am Surg. 2011;77:1330–1333. [PubMed] [Google Scholar]
- 31.Tornqvist B, Stromberg C, Akre O, et al. Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy. Br J Surg. 2015;102:952–958. doi: 10.1002/bjs.9832. [DOI] [PubMed] [Google Scholar]
- 32.Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–469. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]