Abstract
Introduction
Shock wave lithotripsy (SWL) is a well – established treatment option for urolithiasis. The technology of SWL has undergone significant changes in an attempt to better optimize the results while reducing failure rates. There are some important limitations that restrict the use of SWL. In this review, we aim to place these advantages and limitations in perspective, assess the current role of SWL, and discuss recent advances in lithotripsy technology and treatment strategies.
Methods
A comprehensive review was conducted to identify studies reporting outcomes on ESWL. We searched for literature (PubMed, Embase, Medline) that focused on the physics of shock waves, theories of stone disintegration, and studies on optimising shock wave application. Relevant articles in English published since 1980 were selected for inclusion.
Results
Efficacy has been shown to vary between lithotripters. To maximize stone fragmentation and reduce failure rates, many factors can be optimized. Factors to consider in proper patient selection include skin – to – stone distance and stone size. Careful attention to the rate of shock wave administration, proper coupling of the treatment head to the patient have important influences on the success of lithotripsy.
Conclusion
Proper selection of patients who are expected to respond well to SWL, as well as attention to the technical aspects of the procedure are the keys to SWL success. Studies aiming to determine the mechanisms of shock wave action in stone breakage have begun to suggest new treatment strategies to improve success rates and safety.
Keywords: Lithotripsy, Lithotripter, Shock wave generation, Urolithiasis
1. Introduction
The introduction of shock wave lithotripsy (SWL) in 1980 revolutionized the management of kidney stones. Within ten years, it became the most common intervention for patients [1] suffering from renal or ureteral calculi. The changes in SWL technology over the past 3 decades have resulted in varied success rates. Accordingly, researchers have developed a well defined range of uses for SWL to better – optimize results and reduced retreatment rates. Although ureteroscopy is gaining popularity with its recent advances, SWL remains a commonly used treatment option [2].
2. Shock wave generation
The Dornier HM3 was the first lithotripter to be widely utilized in clinical practice. It is a device that features a large water bath for optimum shock wave coupling, fluoroscopic imaging, an ellipsoid reflector with a small aperture and an electrohydraulic shockwave generator [3]. Shock wave sources have evolved over time. There are currently three types of shock wave generators: electrohydraulic, electromagnetic, and piezoelectric.
Electrohydraulic generators are based on spark – gap technology that produces a vaporization bubble. The bubble expands and immediately collapses, producing a high – energy pressure wave. The shock wave then encounters an ellipsoid reflector that focuses the wave [4].
Electromagnetic generators produce a magnetic field. The coil, which is basis of this technology, is located in one of two places: around a cylinder, on the inside plane of a spherical cap, or on a flat exterior with an overlying conductive membrane. A shock wave is produced when the magnetic field causes repulsion of the membrane. It is focused with a parabolic reflector or acoustic lens [5,6]. Unlike electrohydraulic technology, which requires electrode replacement every several thousand shockwaves, electromagnetic generators last for millions of shock waves.
Piezoelectric generators result in the generation of a shockwave by non – linear propagation [7].
A capacitor is fired through a collection of hundreds of piezoceramic elements positioned on a reflector. Each element is focused on the same location (F2) much like a satellite dish.
3. Clinical parameters that may affect outcome of SWL
The outcomes of SWL can be enhanced in many ways. Patient selection plays an important role, and factors to consider include body habitus, stone burden, anatomical location, stone density measured by non – contrast CT, and for renal stone cases, stone to skin distance.
4. Body habitus
Poor outcomes for SWL have been attributed to obesity. Appropriately positioning patients with high body mass index (BMI) to target the stone can be challenging as the focal length of most lithotripters is in the 15 cm range. Furthermore, excess adipose tissue dampens the energy from the shock wave as it travels to F2 [8]. Ackermann and colleagues’ multivariate analysis reported finding that BMI was a significant negative predictor of a stone – free outcome following SWL [9]. Portis et al. have also reported similar findings [10].
Morbid obesity may render SWL impractical or technically impossible for various reasons. Firstly, there are weight limitations on the lithotripter table or gantry. Furthermore, it may be impossible to radio – graphically target the stone. Most often, the skin – to – stone distance (SSD) often exceeds the maximum allowable focal distance of the lithotripter. In such circumstances, a blast path technique that relies on high pressures generated at a point located co – axially beyond second focus (F2) may be considered [11]. The skin – to – stone distance (SSD), as measured by computed tomography, may actually be a more important outcome predictor than BMI.
A recent study combined two parameters: SSD with a measure of stone density (Hounsfield units). The results revealed that patients with both favourable parameters had a 91% stone – free rate, while those with both unfavourable parameters had a 41% stone – free rate (Fig. 1) [12].
Fig. 1.

Influence of stone density (HU) and SSD. HU, Hounsfield units; SSD, skin-to-stone distance.
5. Stone burden
Stone burden plays a significant role in predicting the outcome of SWL (even for patients with non – staghorn calculi). As stone size increases, the likelihood of a successful outcome decreases. EAU and AUA guidelines do not recommend SWL as primary treatment for stones larger than 2 cm in size [13,14]. These calculi are unlikely to respond well to SWL treatment, and are best managed using an alternative method, such as percutaneous nephrolithotomy (PCNL) [15].
6. Stone composition
Stones of differing composition vary widely with regard to their fragility. Similarly, stones of the same composition may respond differently to shockwaves [16]. For example, when SWL is unselectively used to treat patients with cystine stones, poor results can be expected.
Hockley and collaborators reported on 43 cystinuric patients treated with SWL and PCNL. The stone – free rates with SWL were 70.5% for calculi 20 mm or less; meanwhile, stones greater than 20 mm had stone free rates of 41% [17]. Similarly, Kachel et al. reviewed 18 patients with cystine stones and recommended SWL monotherapy for cystine stones smaller than 15 mm [18]. Chow and Streem also studied SWL treatment outcomes in 31 cystinuric patients and found an overall stone – free rate of 86.9% [19]. Hence, SWL for cystine stones should be reserved for patients with a small stone burden.
Brushite calculi also respond poorly to SWL. Klee et al. reported on 30 patients with a total of 46 brushite stones [20]. Success was defined as fragments less than 4 mm. The overall success rate for patients treated by SWL monotherapy was 65%. Hence, a reasonable treatment paradigm would recommend SWL only for patients with known brushite stones of a small size.
Poor response to SWL is not only limited to stones commonly thought of as exceptionally hard or dense. In fact, very soft matrix calculi, composed of as much as 65% organic matter (in comparison to 2% or 3% organic matter in most non – infected urinary calculi), also respond poorly to SWL [21]. When stone composition is unknown, the density of the calculus (as measured by hounsefield unit) on preoperative axial imaging can predict stone fragility and response to SWL [22].
Joseph and colleagues reported a significantly reduced stone free rate of 54.5% with SWL for calculi greater than 1000 HU [23]. In contrast, they found a 100% success rate if stones were less than 500 HU. For stones between 500 and 1000 HU, the clearance rate was 85.7%. Gupta and associates found that HU predicted stone clearance by SWL better than stone size alone [24]. The authors reported that patients with stone density over 750 HU needed 3 or more SWL sessions to achieve a 65% clearance rate; whereas, if the stone was less than 750 HU, 80% of patients needed 3 or fewer treatments. Recently, Pareek and colleagues developed CT – based metrics as a scoring system. The Triple D Score incorporates three metrics (stone density, stone volume/dimensions, and skin – to – stone distance (SSD), to augment the prediction of SWL treatment outcome. They established cutoffs of <150 μL for ellipsoid stone volume, <12 cm for SSD, and <600HU for stone density. A Triple D Score of 0,1, 2, and 3 correlated with SWL success rates of 21.4%, 41.3%, 78.7%, and 96.1%, respectively [25].
7. Stone location
Stone location is an influential factor for the outcome of SWL. Attaining a stone – free status with lower pole calculi (even if fragmentation occurs) can be challenging. Albala and collaborators’ prospective, multicenter, randomized – controlled trial, Lower Pole I, compared success rates for lower pole calculi treated with SWL in comparison to PCNL [26]. At 3 months postoperatively, they noted an overall stone free rate of 95% for PCNL versus 37% using SWL for lower pole stones. The stone free rate for lower pole calculi less than 1 cm was 63%, meanwhile, stones greater than 2 cm had a stone free rate of only 14% [26].
The follow – up study, Lower Pole II was also a prospective, multicenter, randomized – controlled trial comparing ureteroscopy to SWL for lower pole stones less than 1 cm [27]. The authors reported that although there was a trend favoring ureteroscopy, there was no statistically significant difference between the 2 techniques.
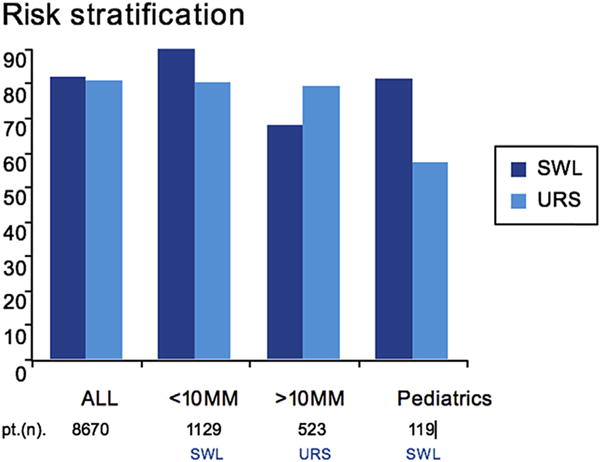
In addition to being contraindicated in young females of childbearing age, SWL of distal ureteral calculi, is associated with lower success rates. The 2007 meta – analysis of EAU/AUA offered guidelines for the management of ureteral calculi and pooled data on SWL outcomes. They noted an 82% stone free rate in the proximal ureter on 41 studies with 6428 patients, 73% stone free rate in the mid – ureter reporting on 31 studies in 1607 patients, and 74% stone free rate in the distal ureter reporting on 50 studies in 6981 patients. (Fig. 2) [28]. When stone size was less than 1 cm, the stone free rates were higher for each location.
Fig. 2.
Stone-free rates for proximal ureteral calculi from the EAU/AUA Guideline.
Infundibulopelvic angle plus infundibular width and length are anatomical factors that can alter the success rate for treatment of lower pole calculi with SWL. Elbahnasy and associates evaluated intrinsic renal anatomy using intravenous pyelogram features [29]. They found that, regardless of the angle, a wide angle or short length with a broad width was associated with a higher success rate for SWL. When evaluating location, upper pole, renal pelvic, and ureteropelvic junction stones have the highest success rates among calculi treated with SWL [30].
The unique clinical scenario of calyceal diverticula is a controversial topic when discussing appropriateness of SWL. The neck of the diverticulum is classically quite narrow; consequently, it can be quite challenging to fragment the stone enough to get clearance of all or any of the pieces. One study revealed a stone free rate of only 21% [31]. Remarkably, despite the low clearance rate, many patients (60%) were still symptom – free. The duration of follow – up in this study was only 3 months.
Patient selection may play a significant role in this subgroup. If there was adequate visualization of the ostium on pre – operative imaging, with the diverticula filling with contrast, and if stone size was small. Streem and Yost demonstrated stone clearance rates of 58% for calyceal diverticular stones [32]. Caution should be exercised when using SWL as monotherapy for calyceal diverticular stones. SWL may be more beneficial when used following ureteroscopy with dilation of the diverticular neck.
8. Treatment strategies with the potential to improve SWL
Case selection, surgeon technique, and modifiable parameters play a role in enhancing safety and maximizing successful outcomes of SWL.
9. Rate
Improved stone fragmentation and reduced tissue damage can be achieved with an optimal rate of shock wave application. Numerous randomized trials have indicated that decreasing shock wave rate can improve stone fragmentation, especially for stones larger than 1 cm [33–37]. Slowing treatment rate results in longer treatment times.
The optimal treatment rate is not clear. Studies suggest that SWL at 60 to 90 shocks/min results in better fragmentation when compared to 120 shocks/min (particularly for larger stones) [38]. Most studies were performed with renal calculi, however, improved outcomes have been demonstrated for upper ureteric stones as well.
10. Energy ramping
Ramping up the energy voltage of the device (rather than beginning at maximum energy) is one way to minimize the risk of tissue injury and potentially improve stone breakage. Ramping also allows for better patient accommodation to the sensation of treatment [39,40]. One in vitro study that had superior fragmentation compared to serially decreasing voltages started with 100 shocks at 12.3 kV, then escalated to 14.8 kV for 400 shocks, followed by 15.8 kV for 1600 shocks [41].
Recently, Lingeman and colleagues discovered that the administration of 300 pretreatment SWs can initiate a protective response in the majority of treated kidneys. Their findings can serve as a guide for minimizing tissue injury while simultaneously decreasing treatment time. This can be attained by selecting 300 or more pretreatment SWs as part of a pause – less treatment protocol; thus, avoiding an extended time pause between initial pretreatment SWs and the main body of treatment shocks [42].
11. Coupling
Maximizing energy delivery to the stone can be achieved by proper coupling of the SWL generator head to the patient in an air – tight manner, with minimization of gas bubbles in the coupling media. Failure to recognize breaks in coupling can result in unsuccessful stone fragmentation [43].
Advances in lithotripter design have led to a shift from water bath coupling (as was seen with the original HM3 design) to the use of a smaller coupling interface. Coupling is influenced by numerous factors: the type of SWL machine, gel used at the patient – generator interface (preferably, a greater volume of lower – viscosity), method of gel application (best to apply to shock head first), and patient factors (i.e. patient movement during treatment, decoupling caused by lifting of the back off the generator and introducing air bubbles into the coupling interface) [44].
12. Targeting
Proper stone targeting is fundamental to SWL success. An ongoing debate exists regarding the superiority of fluoroscopic or ultrasound targeting. Success rates vary based on urologist expertise, SWL machine type, and stone composition [45]. Throughout treatment, targeting should be confirmed at regular intervals. Improved outcomes have been documented with greater use of fluoroscopy time [46].
13. Recent technical innovations
13.1. Wide focal zone shock wave generators
Lithotripters differ based on their acoustic output (i.e. the dimensions and pressures of the focal zone (F2). In cases with multiple renal stones, the efficacy was reduced when compared to the former gold standard, Dornier HM3 [47]. Currently, the evidence indicates that a wide focal zone provides more efficient fragmentation [48,49], while high peak pressures (i.e. high energy flux densities) result in increased tissue injury [50]. Improvements to the design of the acoustic lens of a contemporary Electromagnetic Lithotripter (EML) resulted in the enlargement of the focal zone and significantly less trauma and superior fragmentation (89% stone comminution versus 54%) in a in vivo porcine model [51].
13.2. Dual pulse lithotripter
Distributing the shockwave energy on two applicators is the basis for the dual – EHL system (Direx Duet, Direx Corp, Israel). As shock waves can be delivered along separate paths, the use of dual shock sources has the potential advantage of reducing treatment time. Twin sources can be operated so that shockwaves are fired simultaneously (synchronous or simultaneous mode) or in sequence (alternating mode). Since this method can manipulate the acoustic field, it also has the potential to improve stone breakage [52]. The limited clinical data available indicates safe application with no advantage over single – source SWL. The main challenge with this approach is creating adequate coupling to the stone [53].
13.3. Future ideas
Recognition of the role of cavitation in stone fragmentation has resulted in increased efforts to enhance the action of cavitation bubbles. One such example is tandem shockwaves generated utilizing a piezoelectric source fitted to an electrohydraulic system with an additional discharge circuit to produce the piezoelectric second pulse [54]. Recently, a similar concept utilizing high – intensity focused ultrasound (histotripsy) with an electrohydraulic lithotripter demonstrated a significant reduction in fragmentation time in vitro [55].
On the other hand, cavitation can be detrimental to stone fragmentation. The process results in the production of gas bubbles that last for hundreds of micro seconds, thereby blocking subsequent impulses [56]. Harper and associates developed an innovative technique that utilizes short bursts of focused ultrasonic pulses to transcutaneously reposition stones within the renal collecting system and ureter. Future applications include repositioning stones prior to treatment, expediting the expulsion of residual fragments following ureteroscopy or SWL, and moving obstructing ureteropelvic junction (UPJ) stones into the kidney (to alleviate acute renal colic). The technology is currently being enhanced, and future directions include fusion of the technology with burst wave lithotripsy and stone – specific ultrasound imaging algorithms [57].
Future studies should aim to improve clinical outcomes while simultaneously minimizing complications. The key to achieving better results involves focusing on modifiable factors including shockwave source, focal zone, acoustic output, voltage used, imaging modalities, focusing techniques, and coupling. Lastly, operator or technician experience is critical to success.
14. Conclusion
For the properly selected patients, SWL is a well – tolerated, noninvasive procedure that produces reasonable stone clearance of upper urinary tract calculi while offering low morbidity rates. Recent advances in SWL have produced significant improvements in its safety and efficacy. A drawback to SWL is that retreatments may be necessary.
Ureteroscopy has undergone remarkable advancements in the last 30 years. With the introduction of modern semi – rigid and flexible devices, stones that would have traditionally been considered for SWL, can now be managed via ureteroscopy. In fact, the application of ureteroscopic procedures for upper urinary tract calculi now surpasses that of SWL around the world.
It would be erroneous to conclude that SWL is ineffective or is being replaced. SWL continues to have an important role. Proper selection of patients that are expected to respond well the procedure, as well as consideration of the technical aspects of SWL are key to it success.
Although the features discussed serve as general guidelines for the use of SWL and help predict outcomes, the non – invasive nature of SWL has made it a desirable choice for patients. Many patients that are not ideal candidates for SWL, willingly accept the risk of a failed treatment (and the subsequent need for a secondary procedure) knowing no instrumentation will be necessary with the first attempt.
HIGHLIGHTS.
The key to SWL success lies in the proper selection of patients and attention to SWL technique.
The three modes of SW generation vary in their efficiency.
New treatment strategies to improve success rates and safety.
Current evidence indicates that a wide focal zone provides more efficient fragmentation.
Acknowledgments
Funding
None.
Abbreviations
- SWL
Shock wave lithotripsy
- CT
Computed Tomography
- BMI
Body Mass Index
- F2
Second Focus
- SSD
Skin to Stone Distance
- PCNL
Percutanous nephrolithotomy
- HU
Hounsefield Unit
- UPJ
Ureteropelvic junction
- EML
Electromagnetic lithotripter
Footnotes
Ethical approval
Not applicable.
Author contribution
James Lingeman and H E Elmansy.
Conflicts of interest
None.
Guarantor
James Lingeman.
References
- 1.Chaussy CG, Fuchs GJ. Current state and future developments of noninvasive treatment of human urinary stones with extracorporeal shock wave lithotripsy. J Urol. 1989;141:782–789. doi: 10.1016/s0022-5347(17)41010-x. [DOI] [PubMed] [Google Scholar]
- 2.Scales CD, Jr, Krupski TL, Curtis LH, et al. Practice variation the surgical management of urinary lithiasis. J Urol. 2011;186:146–150. doi: 10.1016/j.juro.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaussy C, Schmiedt E, Jocham D, et al. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982;127:417–420. doi: 10.1016/s0022-5347(17)53841-0. [DOI] [PubMed] [Google Scholar]
- 4.Rassweiler JJ, Knoll T, Kshrmann KU, et al. Shock wave technology and application – an update. Eur Urol. 2011;59:784–796. doi: 10.1016/j.eururo.2011.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pishchalnikov YA, McAteer R, VonderHaar J, et al. Detection of significant variation in acoustic output of an electromagnetic lithotripter. J Urol. 2006;176:2294–2298. doi: 10.1016/j.juro.2006.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lingeman JE, McAteer JA, Gnessin E, et al. Shock wave lithotripsy: advances in technology and technique. Nat Rev Urol. 2009;6:660–670. doi: 10.1038/nrurol.2009.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng CF, Mclornan L, Thompson TJ, et al. Comparison of 2 generations of piezoelectric lithotripters using matched pair analysis. J Urol. 2004;172:1887–1891. doi: 10.1097/01.ju.0000142730.60583.7a. [DOI] [PubMed] [Google Scholar]
- 8.Pareek G, Armenakas NA, Panagopoulos G, et al. Extracorporeal shock wave lithotripsy success based on body mass index and Hounsfield units. Urology. 2005;651:33–36. doi: 10.1016/j.urology.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Ackermann DK, Fuhrimann R, Pfluger D, et al. Prognosis after extracorporeal shock wave lithotripsy of radiopaque renal calculi: a multivariate analysis. Eur Urol. 1994;25:105–109. doi: 10.1159/000475261. [DOI] [PubMed] [Google Scholar]
- 10.Portis AJ, Yan Y, Pattaras JG, et al. Matched pair analysis of shock wave lithotripsy effectiveness for comparison of lithotriptors. J Urol. 2003;169:58–62. doi: 10.1016/S0022-5347(05)64034-7. [DOI] [PubMed] [Google Scholar]
- 11.Locke DR, Newman RC, Steinbock GS, et al. Extracorporeal shock wave lithotripsy in horseshoe kidneys. Urology. 1990;35:407–411. doi: 10.1016/0090-4295(90)80082-x. [DOI] [PubMed] [Google Scholar]
- 12.Perks AE, Schuler TD, Lee J, et al. Stone attenuation and skin – to – stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology. 2008;72:765–769. doi: 10.1016/j.urology.2008.05.046. [DOI] [PubMed] [Google Scholar]
- 13.Turk C, Petrik A, Sarica A, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69(3):475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 14.Preminger GM, Assimos DG, Lingeman JE, et al. AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 15.Galvin DJ, Pearle MS. The contemporary management of renal and ureteric calculi. BJU Int. 2006;98:1283–1288. doi: 10.1111/j.1464-410X.2006.06514.x. [DOI] [PubMed] [Google Scholar]
- 16.Williams JC, Jr, Saw KC, Paterson RF, et al. Variability of renal stone fragility in shock wave lithotripsy. Urology. 2003;61:1092–1097. doi: 10.1016/s0090-4295(03)00349-2. [DOI] [PubMed] [Google Scholar]
- 17.Hockley NM, Lingeman JE, Hutchinson CL. Relative efficacy of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy in the management of cystine calculi. J Endourol. 1989;2:273–285. [Google Scholar]
- 18.Kachel TA, Vijan SR, Dretler SP. Endourological experience with cystine calculi and a treatment algorithm. J Urol. 1991;145:25–28. doi: 10.1016/s0022-5347(17)38237-x. [DOI] [PubMed] [Google Scholar]
- 19.Chow GK, Streem SB. Contemporary urological intervention for cystinuric patients: immediate and long – term impact and implications. J Urol. 1998;160:341–344. doi: 10.1016/s0022-5347(01)62889-1. [DOI] [PubMed] [Google Scholar]
- 20.Klee LW, Brito CG, Lingeman JE. The clinical implications of brushite calculi. J Urol. 1991;145:715–718. doi: 10.1016/s0022-5347(17)38432-x. [DOI] [PubMed] [Google Scholar]
- 21.Bani-Hani AH, Segura JW, Leroy AJ. Urinary matrix calculi: our experience at a single institution. J Urol. 2005;173:120–123. doi: 10.1097/01.ju.0000145868.18824.25. [DOI] [PubMed] [Google Scholar]
- 22.Saw KC, McAteer JA, Fineberg NS, et al. Calcium stone fragility is predicted by helical CT attenuation values. J Endourol. 2000;14:471–474. doi: 10.1089/end.2000.14.471. [DOI] [PubMed] [Google Scholar]
- 23.Joseph P, Mandal AK, Singh SK, et al. Computerized tomography attenuation value of renal calculus: can it predict successful fragmentation of the calculus by extracorporeal shock wave lithotripsy. A preliminary study. J Urol. 2002;167:1968–1971. doi: 10.1016/s0022-5347(05)65064-1. [DOI] [PubMed] [Google Scholar]
- 24.Gupta NP, Ansari MS, Kesarvani P, et al. Role of computed tomography with no contrast medium enhancement in predicting the outcome of extracorporeal shock wave lithotripsy for urinary calculi. BJU Int. 2005;95:1285–1288. doi: 10.1111/j.1464-410X.2005.05520.x. [DOI] [PubMed] [Google Scholar]
- 25.Tran TY, McGillen K, Cone EB, et al. Triple D Score is a reportable predictor of shockwave lithotripsy stone – free rates. J Endourol. 2015;2:226–230. doi: 10.1089/end.2014.0212. [DOI] [PubMed] [Google Scholar]
- 26.Albala DM, Assimos DG, Clayman RV, et al. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotrispsy and percutaneous nephrolithotomy for lower pole nephrolithiasis–initial results. J Urol. 2001;166:2072–2080. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 27.Pearle MS, Lingeman JE, Leveillee R, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol. 2005;173:2005–2009. doi: 10.1097/01.ju.0000158458.51706.56. [DOI] [PubMed] [Google Scholar]
- 28.Preminger GM, Tiselius HG, Assimos DG, et al. Guidelines for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 29.Elbahnasy AM, Shalhav AL, Hoenig DM, et al. Lower caliceal stone clearance after shock wave lithotripsy or ureteroscopy: the impact of lower pole radiographic anatomy. J Urol. 1998;159:676–682. [PubMed] [Google Scholar]
- 30.Weld KJ, Montiglio C, Morris MS, et al. Shock wave lithotripsy success for renal stones based on patient and stone computed tomography characteristics. Urology. 2007;706:1043–1046. doi: 10.1016/j.urology.2007.07.074. [DOI] [PubMed] [Google Scholar]
- 31.Turna B, Raza A, Moussa SA, et al. Management of calyceal diverticular stones with extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy: long–term outcome. BJU Int. 2007;100:151–156. doi: 10.1111/j.1464-410X.2007.06911.x. [DOI] [PubMed] [Google Scholar]
- 32.Streem SB, Yost A. Treatment of caliceal diverticular calculi with extracorporeal shock wave lithotripsy: patient selection and extended followup. J Urol. 1992;148:1043–1046. doi: 10.1016/s0022-5347(17)36812-x. [DOI] [PubMed] [Google Scholar]
- 33.Pace KT, Ghiculete D, Harju M, et al. Shock wave lithotripsy at 60 or 120 shocks per minute: a randomized, double–blind trial. J Urol. 2005;174:595–599. doi: 10.1097/01.ju.0000165156.90011.95. [DOI] [PubMed] [Google Scholar]
- 34.Honey RJ, Schuler TD, Ghiculete D, et al. A randomized, double–blind trial to compare shock wave frequencies of 60 and 120 shocks per minute for upper ureteral stones. J Urol. 2009;182:1418–1423. doi: 10.1016/j.juro.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 35.Davenport K, Minervini A, Keoghane S, et al. Does rate matter? The results of a randomized controlled trial of 60 versus 120 shocks per minute for shock wave lithotripsy of renal calculi. J Urol. 2006;176:2055–2058. doi: 10.1016/j.juro.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 36.Madbouly K, El–Tiraifi AM, Seida M, et al. Slow versus fast shock wave lithotripsy rate for urolithiasis: a prospective randomized study. J Urol. 2005;173:127–130. doi: 10.1097/01.ju.0000147820.36996.86. [DOI] [PubMed] [Google Scholar]
- 37.Yilmaz E, Batislam E, Basar M, et al. Optimal frequency in extracorporeal shock wave lithotripsy: prospective randomized study. Urology. 2005;66:1160–1164. doi: 10.1016/j.urology.2005.06.111. [DOI] [PubMed] [Google Scholar]
- 38.Li K, Lin T, Zhang C, et al. Optimal frequency of shock wave lithotripsy in urolithiasis treatment: a systematic review and meta–analysis of randomized controlled trials. J Urol. 2013;190:1260–1267. doi: 10.1016/j.juro.2013.03.075. [DOI] [PubMed] [Google Scholar]
- 39.McAteer JA, Evan AP, Williams JC, et al. Treatment protocols to reduce renal injury during shock wave lithotripsy. Curr Opin Urol. 2009;19:192–195. doi: 10.1097/mou.0b013e32831e16e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lambert EH, Walsh R, Moreno MW, et al. Effect of escalating versus fixed voltage treatment on stone comminution and renal injury during extracorporeal shock wave lithotripsy: a prospective randomized trial. J Urol. 2010;183:580–584. doi: 10.1016/j.juro.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 41.Yong DZ, Lipkin ME, Simmons WN, et al. Optimization of treatment strategy used during shockwave lithotripsy to maximize stone fragmentation efficiency. J Endourol. 2011;25:1507–1511. doi: 10.1089/end.2010.0732. [DOI] [PubMed] [Google Scholar]
- 42.Connors BA, Evan AP, Handa RK, et al. Using 300 pretreatment shock waves in a voltage ramping protocol can significantly reduce tissue injury during extracorporeal shock wave lithotripsy. J Endourol. 2016;9:1004–1008. doi: 10.1089/end.2016.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pishchalnikov YA, Neucks JS, VonDerHaar RJ, et al. Air pockets trapped during routine coupling in dry head lithotripsy can significantly decrease the delivery of shock wave energy. J Urol. 2006;176:2706–2710. doi: 10.1016/j.juro.2006.07.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jain A, Shah TK. Effect of air bubbles in the coupling medium on efficacy of extracorporeal shock wave lithotripsy. Eur Urol. 2007;51:1680–1686. doi: 10.1016/j.eururo.2006.10.049. [DOI] [PubMed] [Google Scholar]
- 45.Bohris C, Bayer T, Gumpinger R. Ultrasound monitoring of kidney stone extracorporeal shockwave lithotripsy with an external transducer: does fatty tissue cause image distortions that affect stone comminution? J Endourol. 2010;24:81–88. doi: 10.1089/end.2009.0158. [DOI] [PubMed] [Google Scholar]
- 46.Logarakis NF, Jewett MA, Luymes J, et al. Variation in clinical outcome following shock wave lithotripsy. J Urol. 2000;163:721–725. [PubMed] [Google Scholar]
- 47.Zehnder P, Roth B, BirkhŠuser F, et al. A prospective randomized trial comparing the modified HM3 with the Modulith SLX–F2 lithotripter. Eur Urol. 2011;59:637–644. doi: 10.1016/j.eururo.2011.01.026. [DOI] [PubMed] [Google Scholar]
- 48.Granz B, Kšhler G. What makes a shock wave efficient in lithotripsy. J Stone Dis. 1992;4:123–128. [PubMed] [Google Scholar]
- 49.Eisenmenger W. The mechanisms of stone fragmentation in ESWL. Ultrasound Med Biol. 2001;27:683–693. doi: 10.1016/s0301-5629(01)00345-3. [DOI] [PubMed] [Google Scholar]
- 50.Bergsdorf T, ThŸroff S, Chaussy C. The isolated perfused kidney: an in vitro test system for evaluation of renal tissue by high–energy shockwave sources. J Endourol. 2005;19:883–888. doi: 10.1089/end.2005.19.883. [DOI] [PubMed] [Google Scholar]
- 51.Neisius A, Smith NB, Sankin G, et al. Improving the lens design and performance of a contemporary electromagnetic shock wave lithotripter. Proc Natl Acad Sci U S A. 2014;111(13):1167–1175. doi: 10.1073/pnas.1319203111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sokolov DL, Bailey MR, Crum LA. Use of a dual–pulse lithotripter to generate a localized and intensified cavitation field. J Acoust Soc Am. 2001;110:1685–1695. doi: 10.1121/1.1394221. [DOI] [PubMed] [Google Scholar]
- 53.Sheir KZ, El–Diasty TA, Ismail AM. Evaluation of a synchronous twin–pulse technique for shock wave lithotripsy: the first prospective clinical study. BJU Int. 2005;95:389–393. doi: 10.1111/j.1464-410X.2005.05306.x. [DOI] [PubMed] [Google Scholar]
- 54.Zhou Y, Cocks FH, Preminger GM, et al. Innovation in shock wave lithotripsy technology: updates in experimental studies. J Urol. 2004;172:1892–1898. doi: 10.1097/01.ju.0000142827.41910.a2. [DOI] [PubMed] [Google Scholar]
- 55.Duryea AP, Hall TL, Maxwell AD, et al. Histotripsy erosion of model urinary calculi. J Endourol. 2011;25:341–344. doi: 10.1089/end.2010.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pishalnikov YA, Sapozhnikov OA, Williams JC, Jr, et al. Cavitation bubble cluster activity in the breakage of kidney stones by lithotripter shock waves. J Endourol. 2003;17:435–446. doi: 10.1089/089277903769013568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.May PC, Bailey MR, Harper JD. Ultrasonic propulsion of kidney stones. Curr Opin Urol. 2016;26(3):264–270. doi: 10.1097/MOU.0000000000000276. [DOI] [PMC free article] [PubMed] [Google Scholar]


